6. Diseases of the Episclera and sclera (with bits of 5)
1/127
Earn XP
Description and Tags
Since didn't finish all of 5 for exam, some remaining is on this 2nd miterm.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
128 Terms
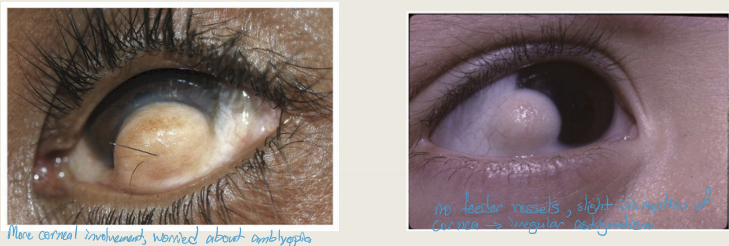
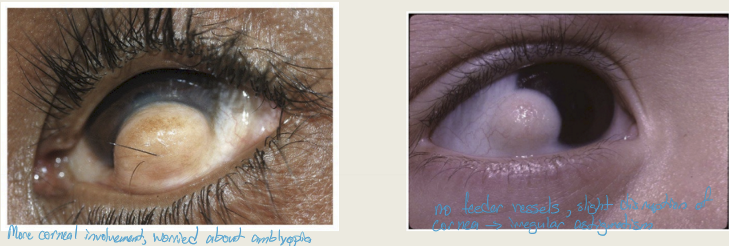
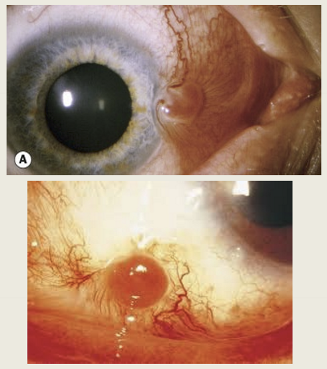
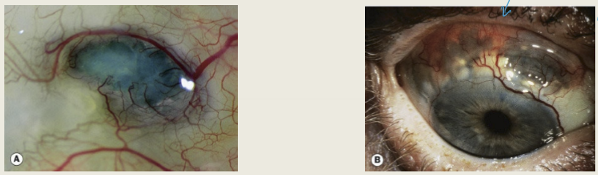
What is limbal dermoid?
A mass of normal tissue in an abnormal position (choristoma)
Who does limbal dermoid typically affect?
More common in children
What are systemic associations of limbal dermoid?
Goldenhar syndrome
Treacher Collins syndrome
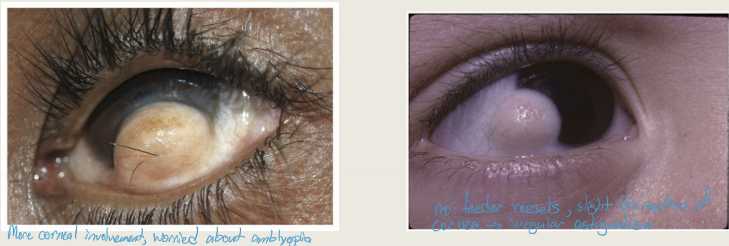
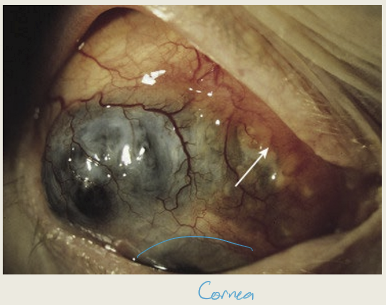
What are the presentations of Limbal dermoid?
Smooth yellow soft subconjunctival mass
Typically located inferior temporal
May have protruding hair
Will disrupt corneal architecture to differing degrees: superficial involvement to invasion into anterior chamber; extensive corneal involvement can lead to astigmatism and amblyopia
What are the treatments for limbal dermoid?
Surgical-simple excision for small lesions to corneal transplants for lesions with extensive corneal involvement
What is dermolipoma?
A mass of fatty tissue in an abnormal position, similar to limbal dermoid.

Who is typically affected by dermolipoma?
Adults are typically affected.

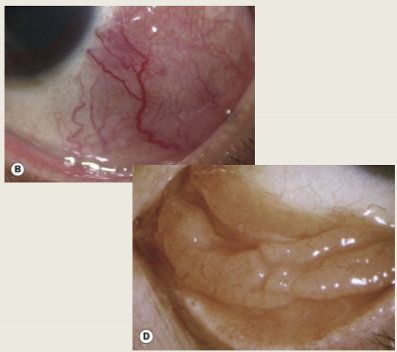
What are the presentations of dermolipoma?
Yellow subconjuctival mass near outer canthus
Surface of mass will be keratinized
may contain hairs

What are the treatments for dermolipoma?
Debulking the mass
Surgery is rarely performed due to complications

What is pyogenic granuloma?
A fibrovascular lesion that is the result of a surgery or injury
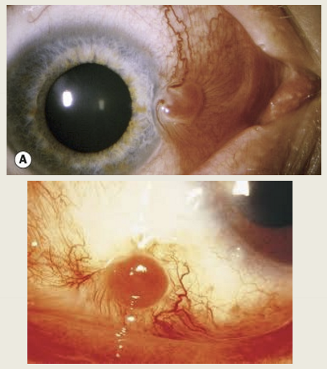
Where is pyogenic granuloma found?
On the lid or conjunctiva
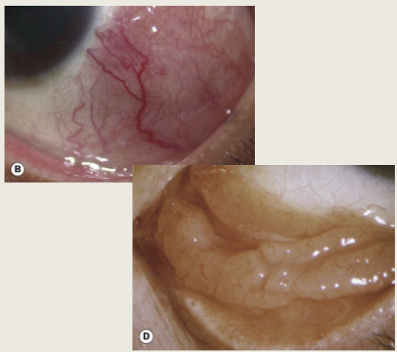
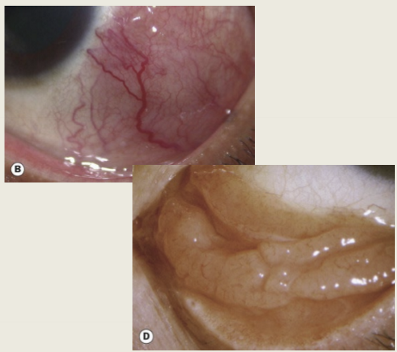
What are the presentations of pyogenic granuloma?
Dark pink fleshy conjunctival mass
mass tends to be rapidly trowing
has more BV than pterygium
What are the treatments for pyogenic granuloma?
Topical steriod
excision
Education pt, what causes it, and to not rub the eye
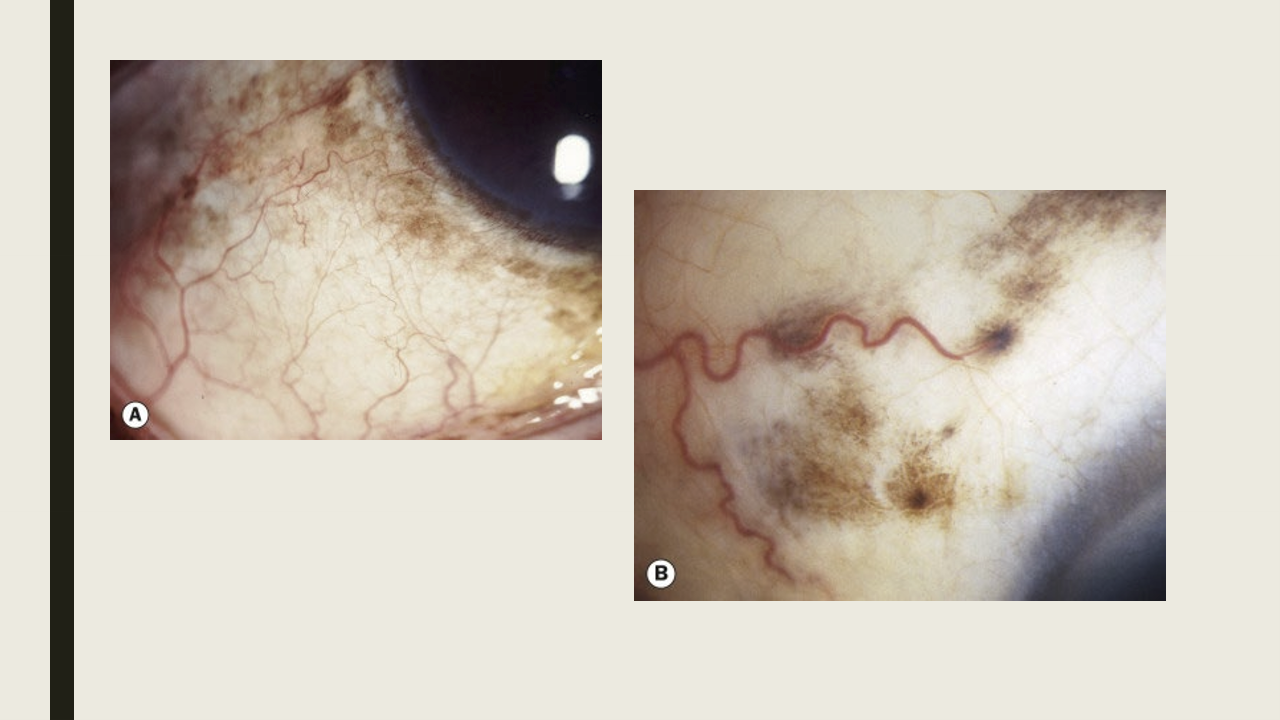
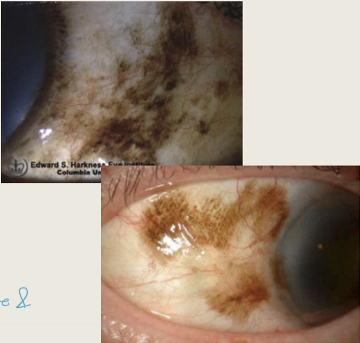
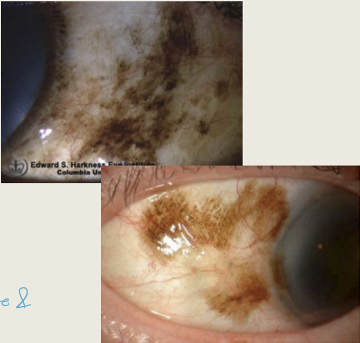
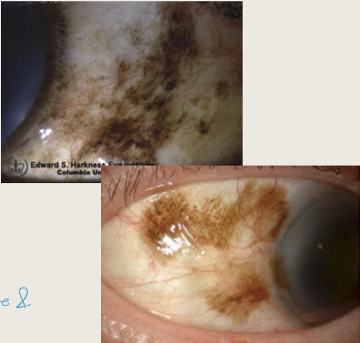
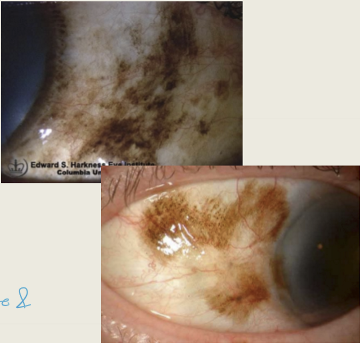
What is racial melanosis (conj epithelial melanosis)?
An excessive melanin within the basal layer of the conj epithelial melanocytes
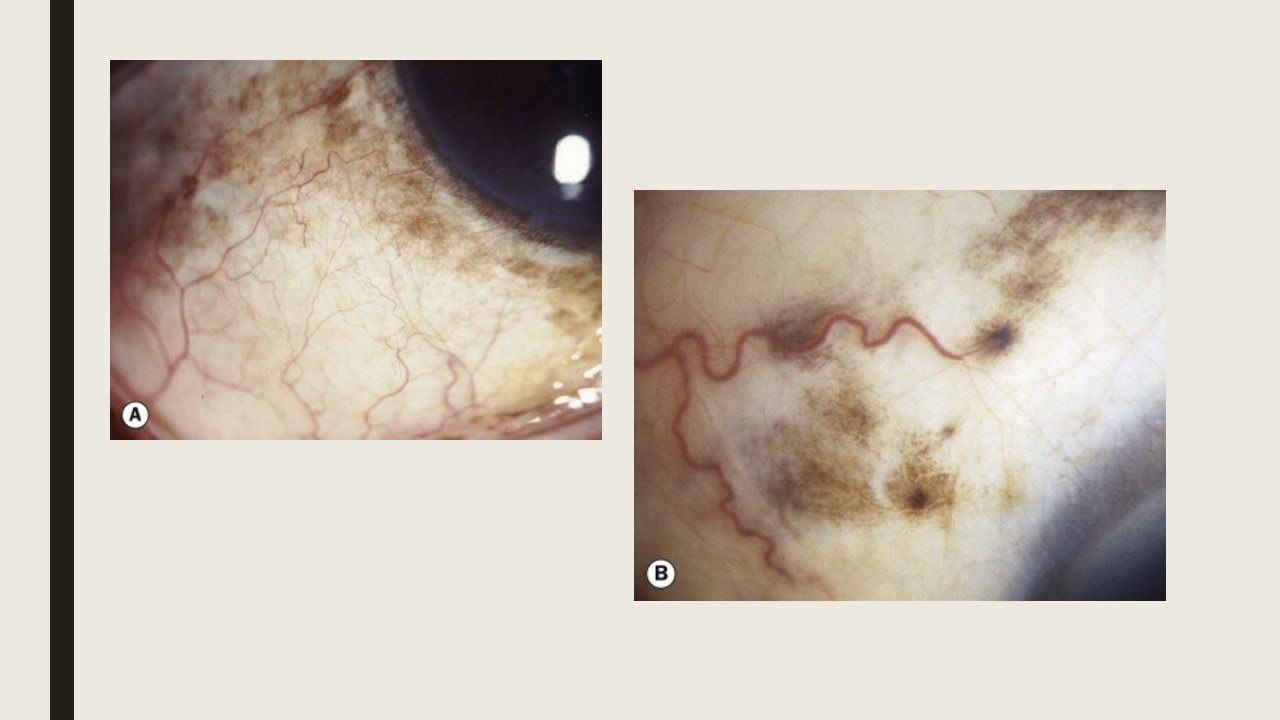
When is racial melanosis typically seen?
It presents during childhood and remains stable through adulthood. It is common in dark skinned individuals.
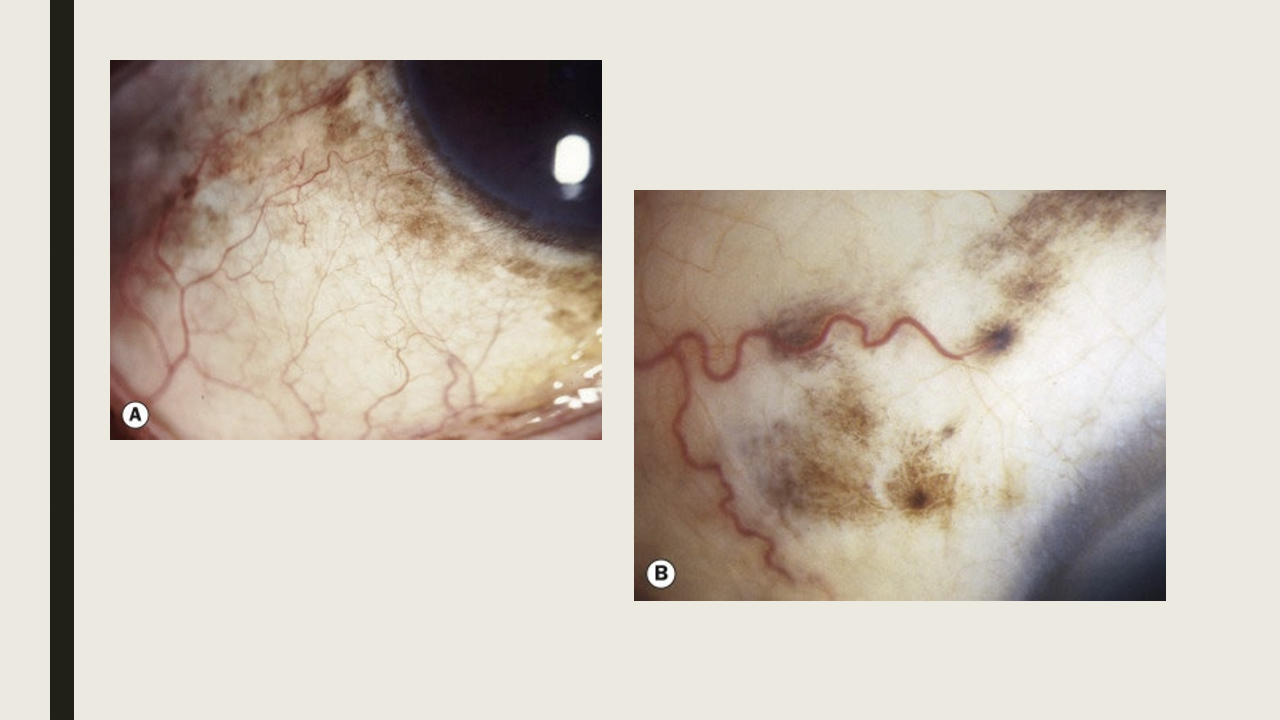
What are the presentations of racial melanosis?
Bilateral condition, but bay be asymmetric
Flat, patchy brown pigmentation
Can be found throughout the conj with a higher conc near the limbus
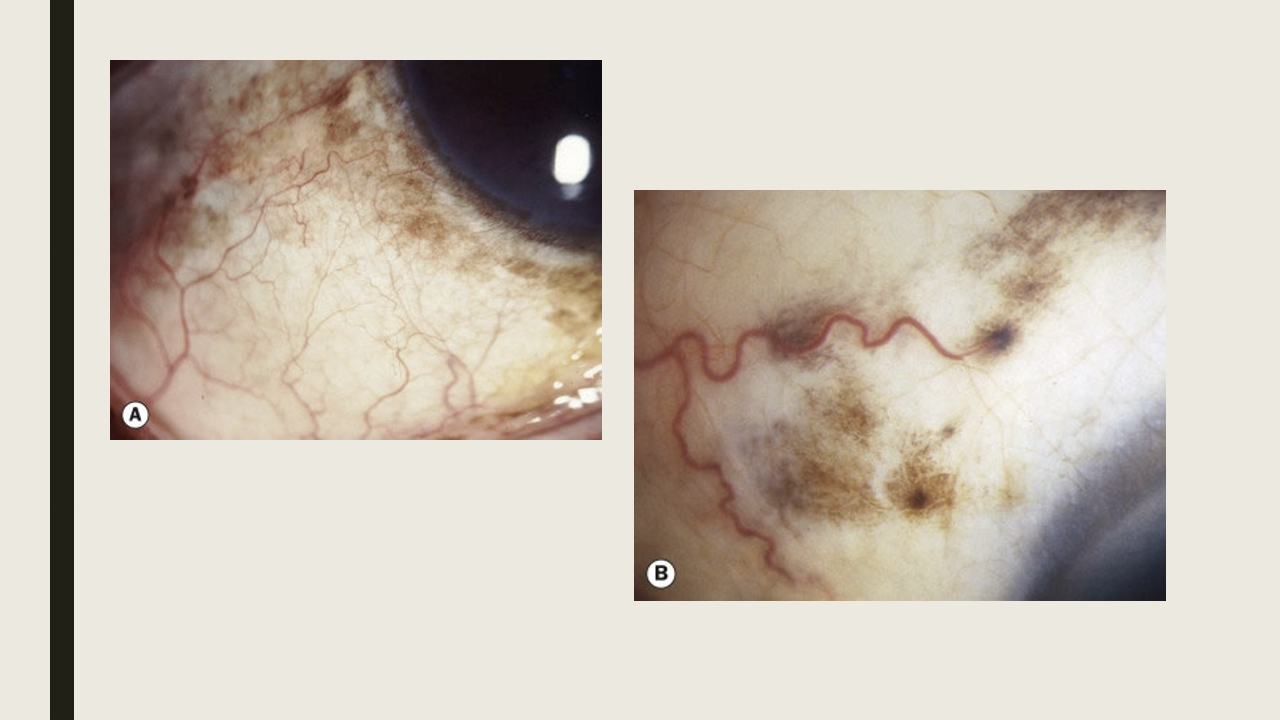
What are the treatments for racial melanosis?
None, just education patient that it is something fun to look at, but will not turn into anything bad.
What is primary acquired melanosis (PAM)?
PAM is a pigmented lesion of the conjunctival epithelium
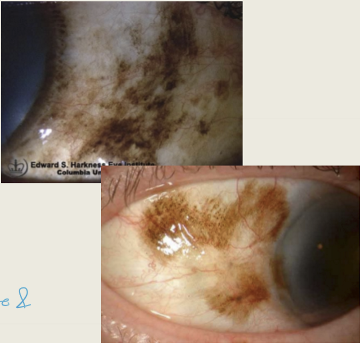
Who is mostly commonly affected by PAM?
Typically seen in fair-skinned, middle-aged to elderly individuals. It is usually unilateral and appears as a flat, brown patch.
What are the two histologic variants of PAM and their clinical significance?
PAM without atypia: Pigmentation of the conj epithelium with or without benign melanocyte hyperplasia; does not progress to melanoma.
PAM with atypia: Pigmentation of conj epithelium with atypical melanocyte hyperplasia; considered precancerous, high risk for melanoma.
Need biopsy to differentiate
What factor increases the risk of PAM transforming into melanoma?
Lesion size. The larger the lesion, the greater the risk of malignant transformation.
What are the typical symptoms of PAM?
Asymptomatic
What are the presentations of PAM?
Flat, irregular brown lesion of the conj epithelium
Unilateral condition
Located on palepbral, bulabar, and fornix
May be uni- or multifocal
What are the treatment for PAM?
Observation or excision. Assume cancer on fiar skinned people & refer out (can also observe)
How common is conjunctival melanoma and in which age group does it typically present?
It is uncommon, accounting for ~2% of all ocular tumors, and usually presents in the sixth decade of life.
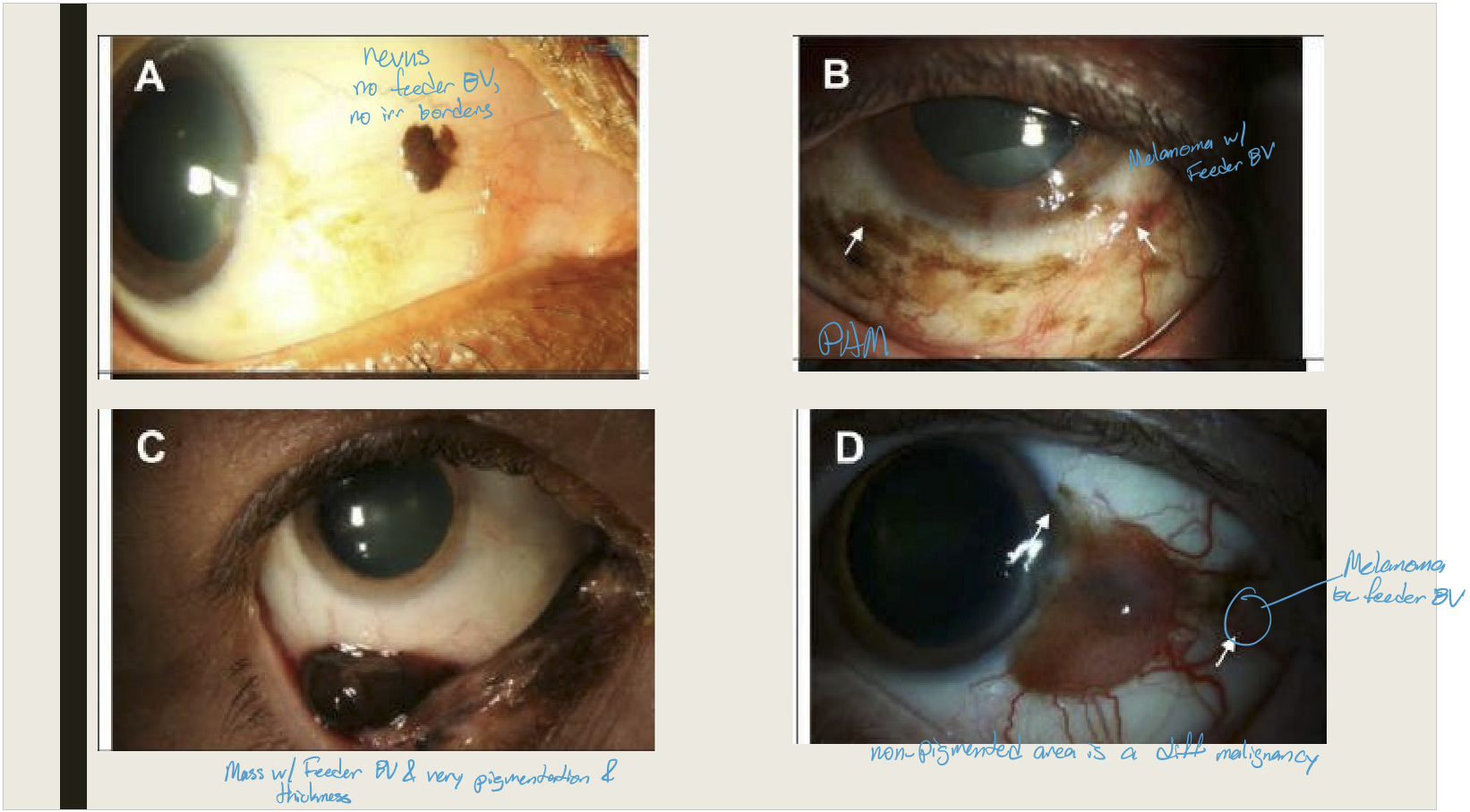
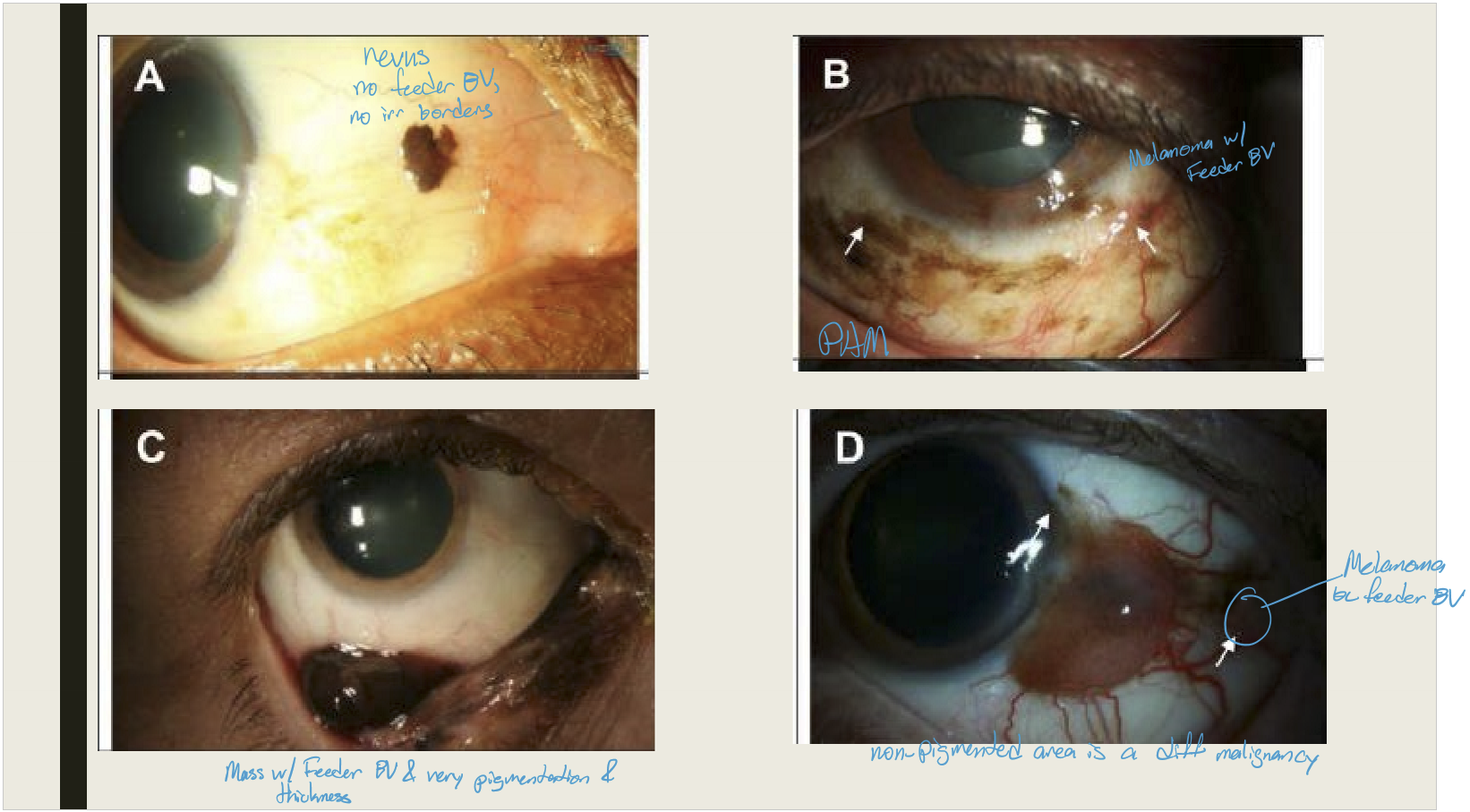
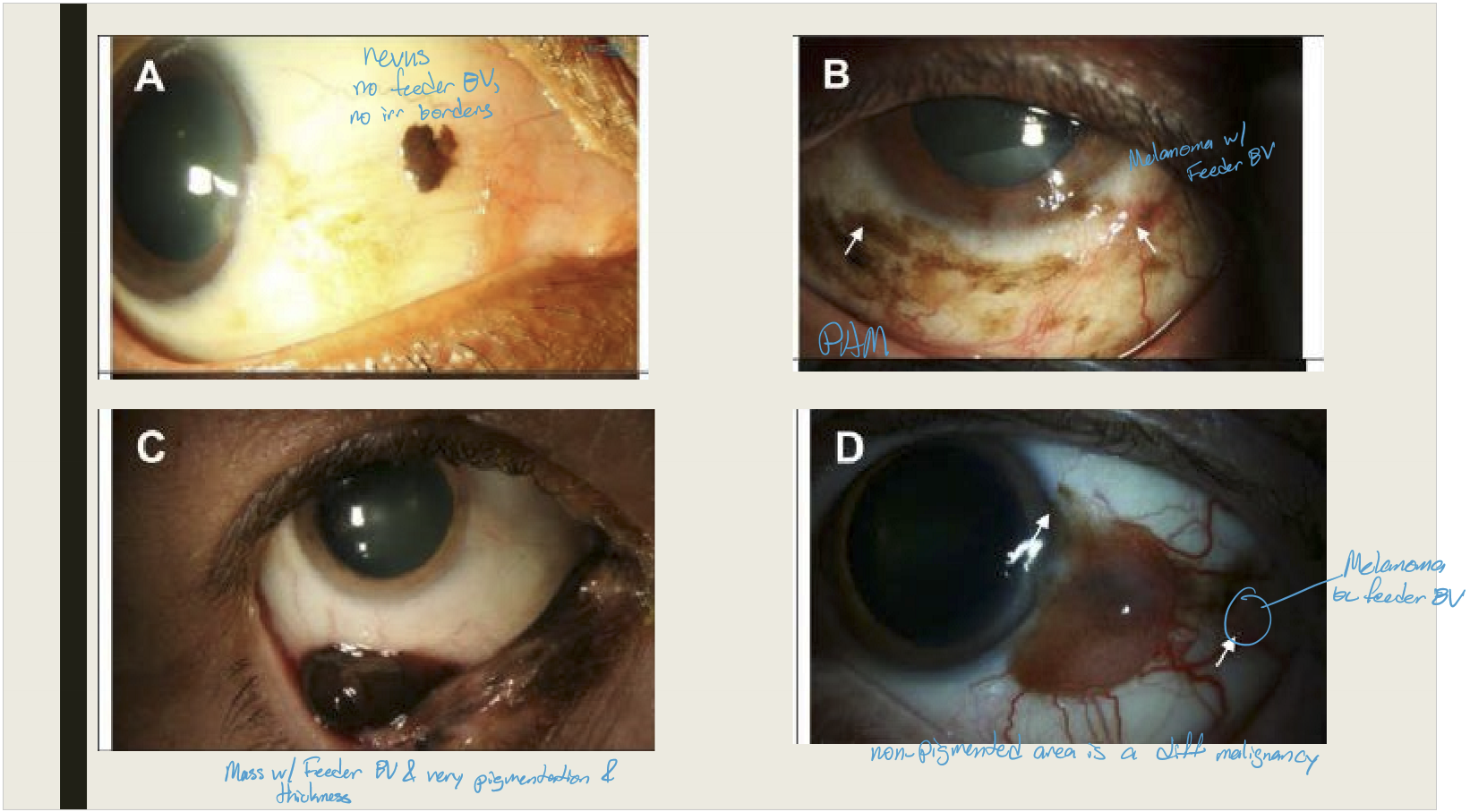
What are the main origins of conjunctival melanoma?
PAM with atypia (9–32%).
Conjunctival nevus (~1%).
Can also occur de novo (without prior lesion).
What are the typical clinical presentations of conjunctival melanoma?
Pigmented, elevated lesion with surrounding pigmentation.
Most commonly on bulbar conjunctiva and limbus; less often on palpebral conjunctiva or fornix.
Often associated with feeder vessels.
What is the treatment for conjunctival melanoma?
Excision combined with chemotherapy, cryotherapy, or radiotherapy
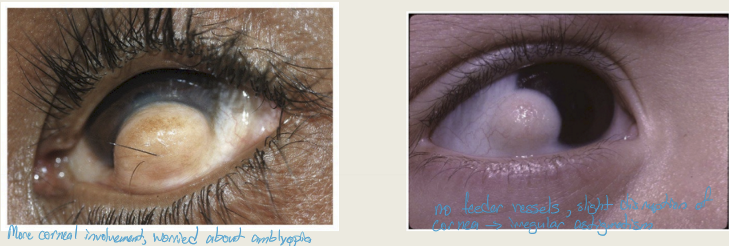
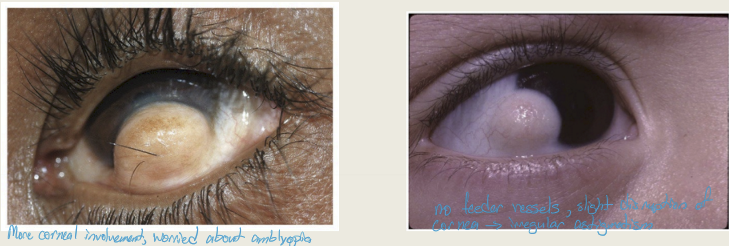
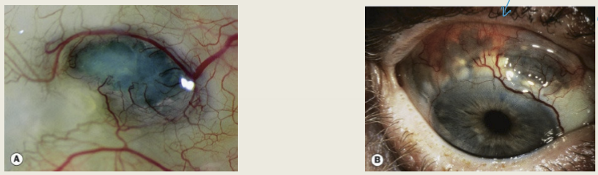
What is ocular surface squamous neoplasia (OSSN) and who is typically affected?
OSSN is a slowly progressive lesion of the conjunctiva/cornea that may be benign, premalignant, or malignant. It typically affects males more in US and Europe and women in Africa
What are the risk factors for OSSN?
UV exposure
Fair skin
Smoking
Xeroderma pigmentosum
HIV infection
Human papillomavirus (HPV)
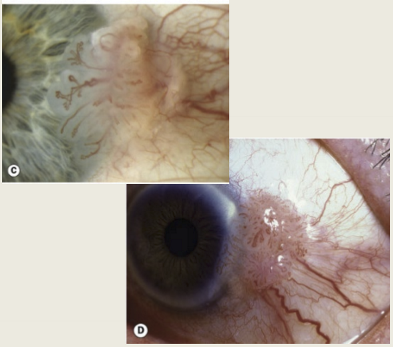
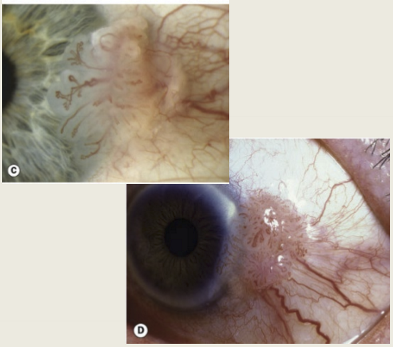
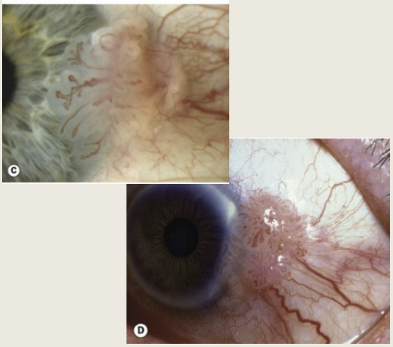
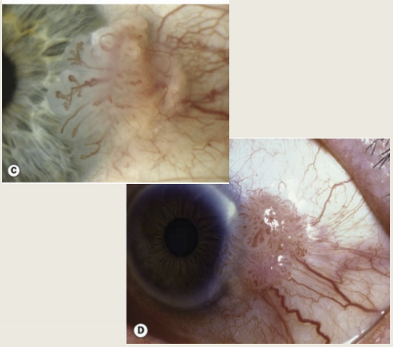
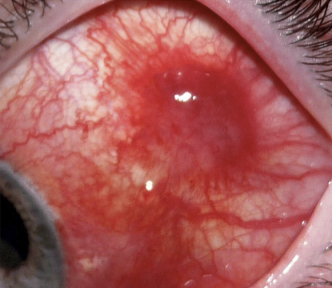
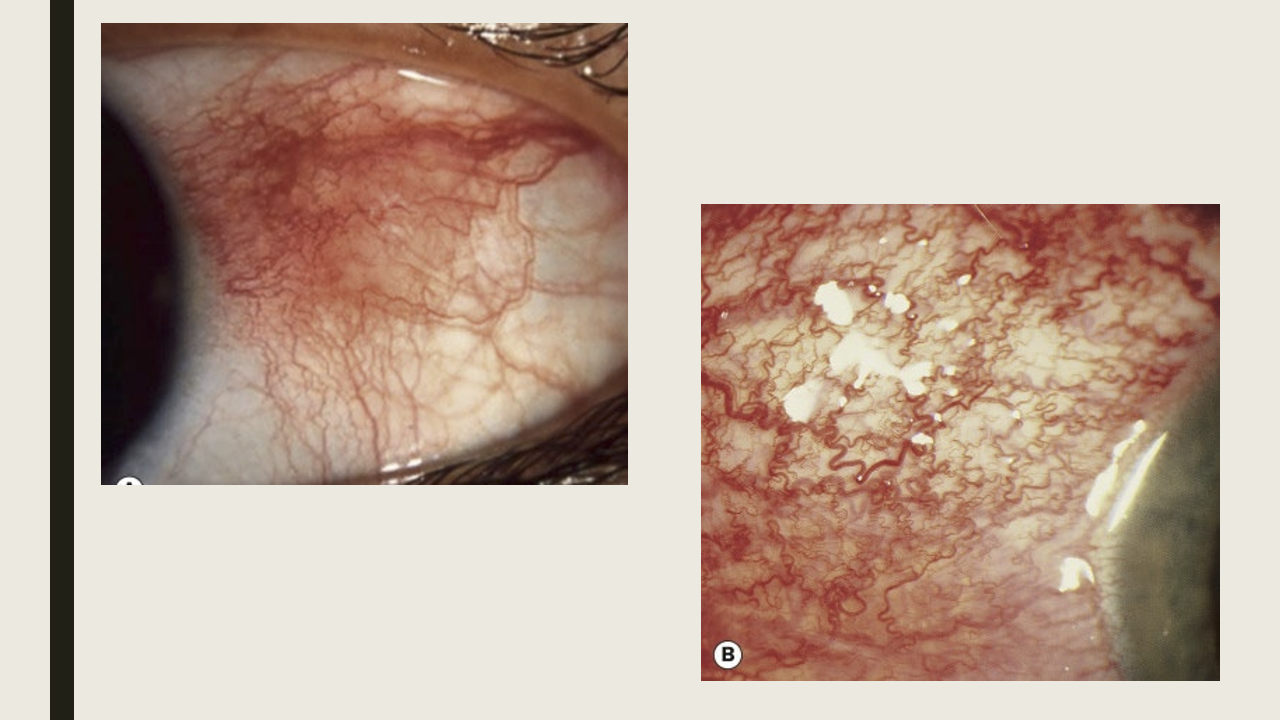
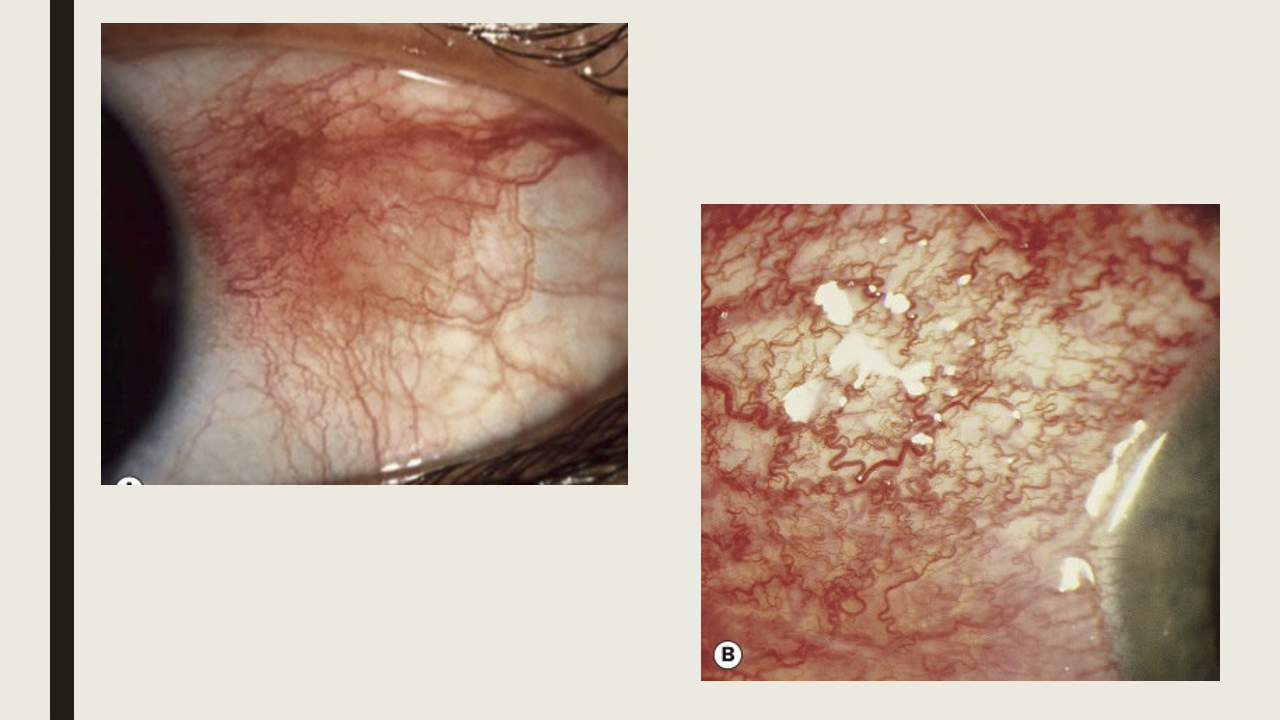
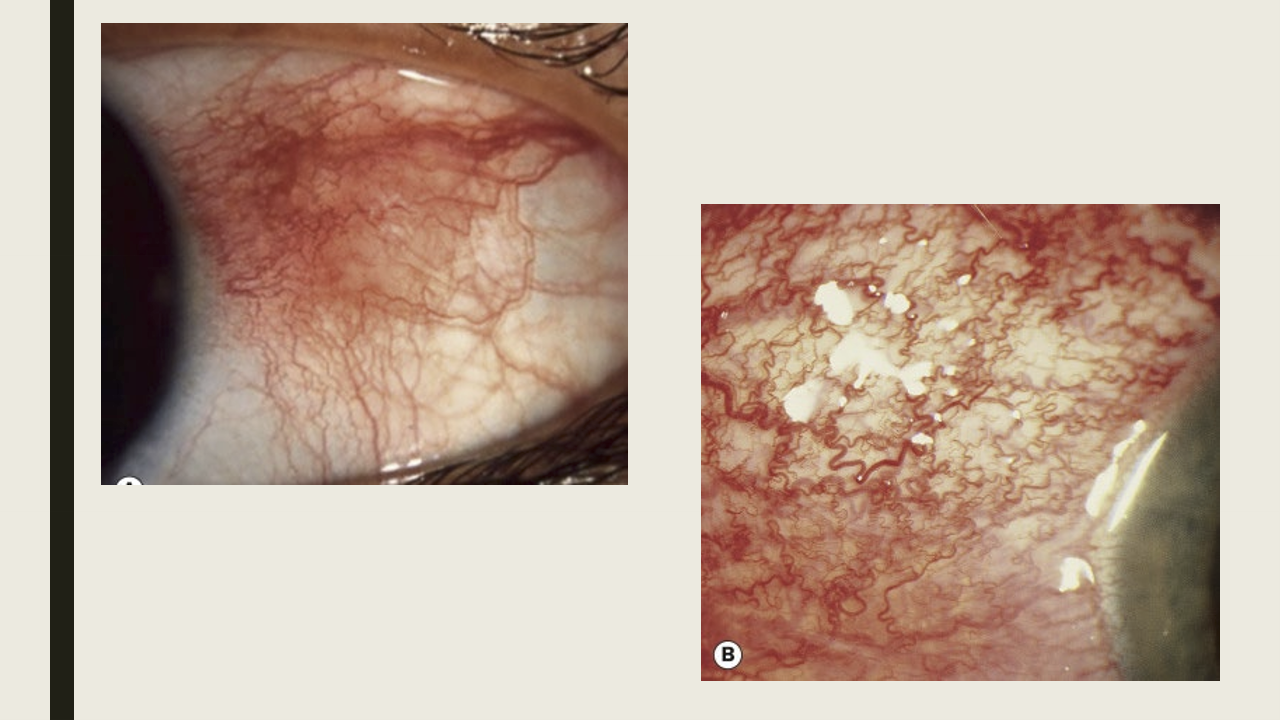
What are the symptoms and presentations of OSSN?
Visible mass with occasional conjunctivitis
Fleshy gelatinous mass
May have papillomatous appearance
feeder vessels will be visible
typically located within interpalpebral fissure,particularly at the limbus
What are the treatments for OSSN?
Excision
What is the typical demographic of malignant conjunctival lymphoproliferative lesions?
Occurs in late adulthood
What are the presentations of malignant conjunctival lymphoproliferative lesions?
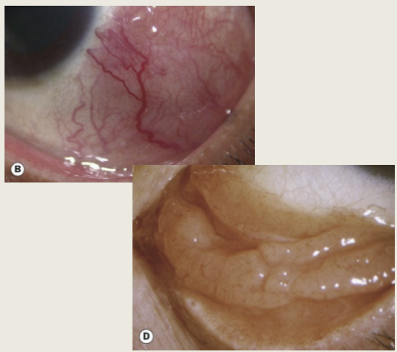
Painless irritation with swelling (can be bilateral) and flesh-colored infiltrate on the bulbar surface or fornix.
How can diffuse malignant conjunctival lymphoproliferative lesions mimic another condition?
When diffuse (rarely), they resemble chronic conjunctivitis but remain mobile on examination.
What are the main treatment options for malignant conjunctival lymphoproliferative lesions?
Radiotherapy, chemotherapy, surgical excision, and cryotherapy.
What is Kaposi sarcoma of the conjunctiva, and who is most commonly affected?
A rare malignant tumor of the conjunctiva primarily affecting patients with AIDS.
How does Kaposi sarcoma typically present on the conjunctiva?
As a flat, bright red lesion.
What are the main treatment options for conjunctival Kaposi sarcoma?
Focal radiotherapy and surgical excision (with or without adjacent cryotherapy).
What is the typical demographic for conjunctival trauma?
Most cases occur in late adolescence or adulthood (especially >70 years), with men affected more than women.
What are the most common causes of conjunctival trauma?
Sports-related injuries and motor vehicle accidents.
What is the most common cause of conjunctival laceration?
Fingernail injury
What are the key symptoms of conjunctival laceration?
Pain, redness, and foreign body sensation.
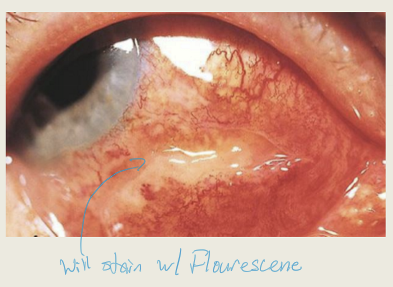
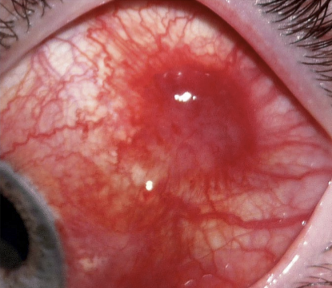
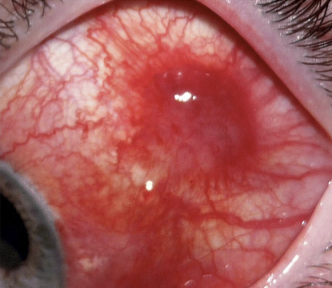
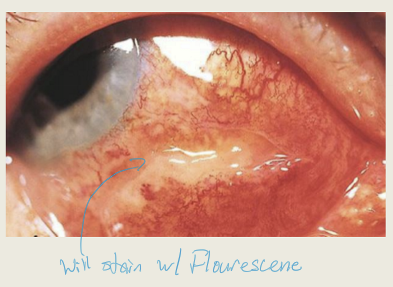
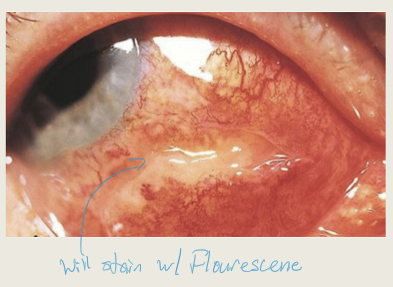
How does conjunctival laceration typically present on examination?
Rolled conjunctival tissue, conjunctival chemosis, and conjunctival hemorrhage. Will stain with fluoresce
How is treatment for conjunctival laceration determined?
Based on the size of the laceration.
What is the treatment for conjunctival lacerations under 10 mm?
Topical antibiotic ointment
What is the treatment for conjunctival lacerations over 10 mm?
Suture repair and topical antibiotic.
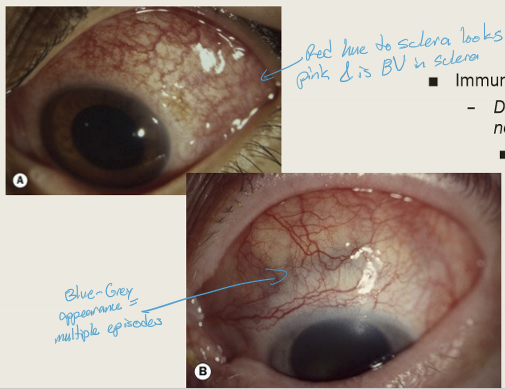
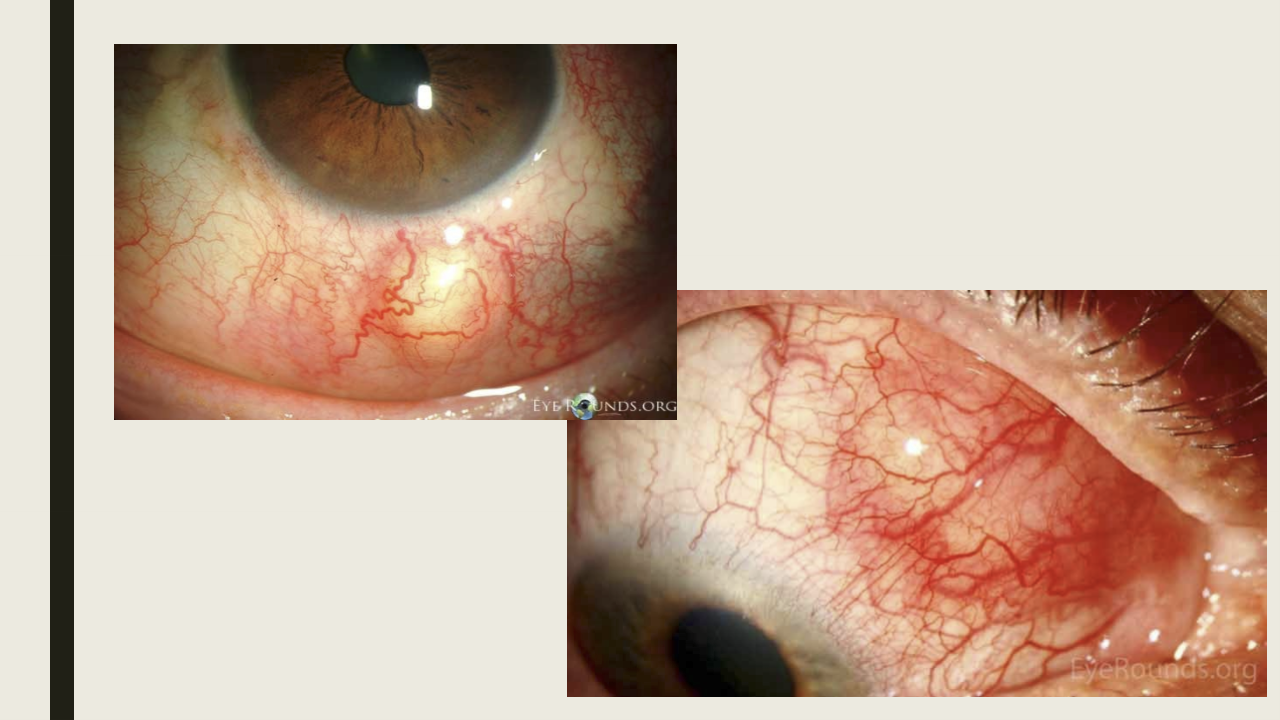
What is episcleritis and how does it typically behave clinically?
Inflammation of the episclera; usually benign, self-limiting, and an attack lasts for days.
What are the common characteristics of episcleritis?
Idiopathic, often bilateral and recurrent.
What are the two main types of episcleritis?
Simple and nodular
What proportion of episcleritis cases are simple episcleritis, and who is more commonly affected?
About 75% of cases; females are affected more than males.
How does simple episcleritis typically present?
Sectoral or diffuse interpalpebral redness that peaks about 12 hours after onset and lasts several days.
What is the treatment approach for simple episcleritis?
Mild cases: observation or artificial tears
Moderate/severe: topical steroids or oral NSAIDs
Who is most commonly affected by nodular episcleritis, and how does its duration compare to simple episcleritis?
Young females; nodular episcleritis lasts longer than simple episcleritis.
How does nodular episcleritis typically present?
Redness upon waking that worsens over 2–3 days, with a tender, movable nodule in the interpalpebral space; sclera remains flat under the nodule. Pt may have foreign body sensation
What is a key diagnostic feature of nodular episcleritis using phenylephrine?
Blood vessels blanch with instillation of 2.5% phenylephrine.
What is the treatment for nodular episcleritis?
Mild cases: observation or artificial tears
Moderate/severe: topical steroids or oral NSAIDs
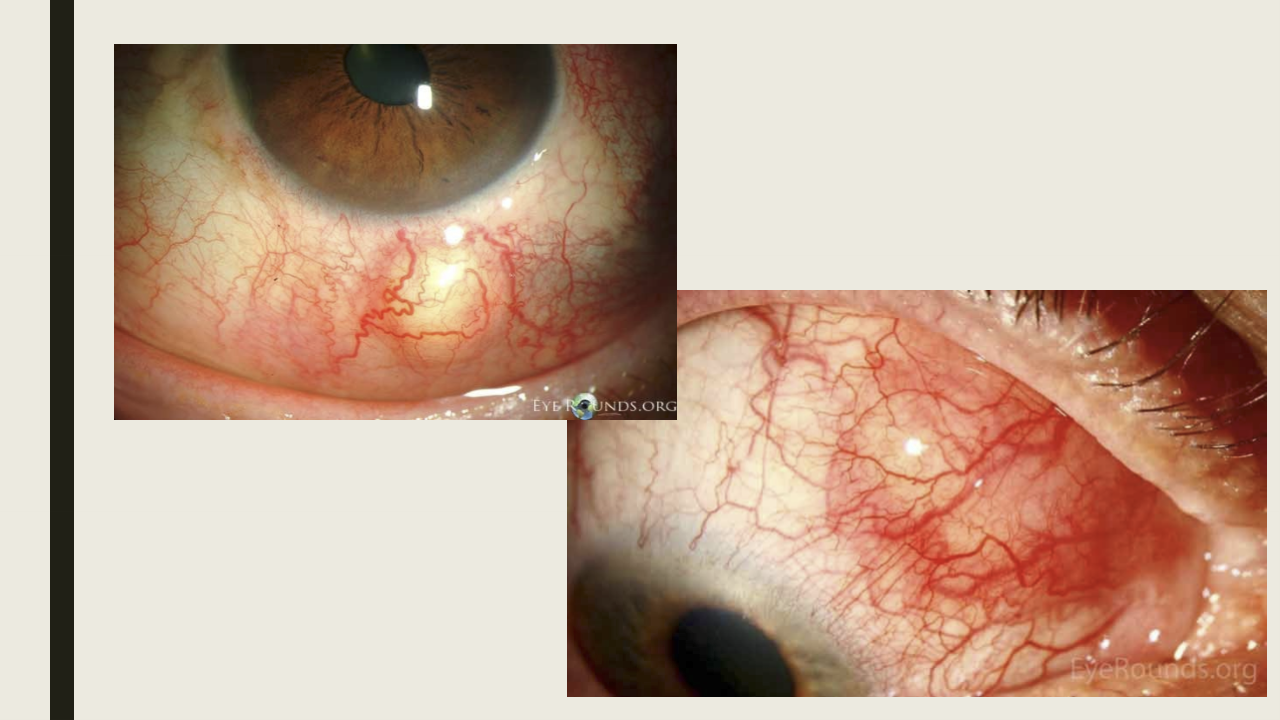
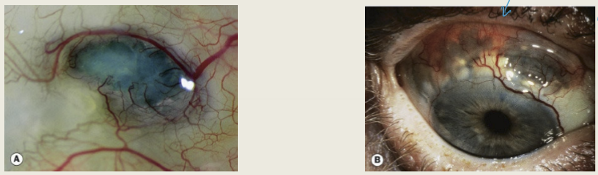
What is scleritis and how common is it?
Edema and cellular inflammation of the sclera; an uncommon condition.
What are the main etiologies of scleritis?
Often associated with autoimmune diseases; can also have bacterial causes.
What are the two major types of scleritis?
Anterior and posterior.
Who is most commonly affected by diffuse anterior non-necrotizing scleritis, and at what age?
More common in females; typically presents in the 5th decade.
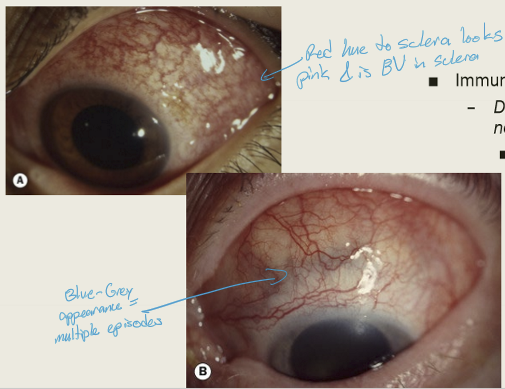
What is the hallmark symptom of diffuse anterior non-necrotizing scleritis?
Severe aching pain that radiates to the face and temple region.
How does diffuse anterior non-necrotizing scleritis present clinically?
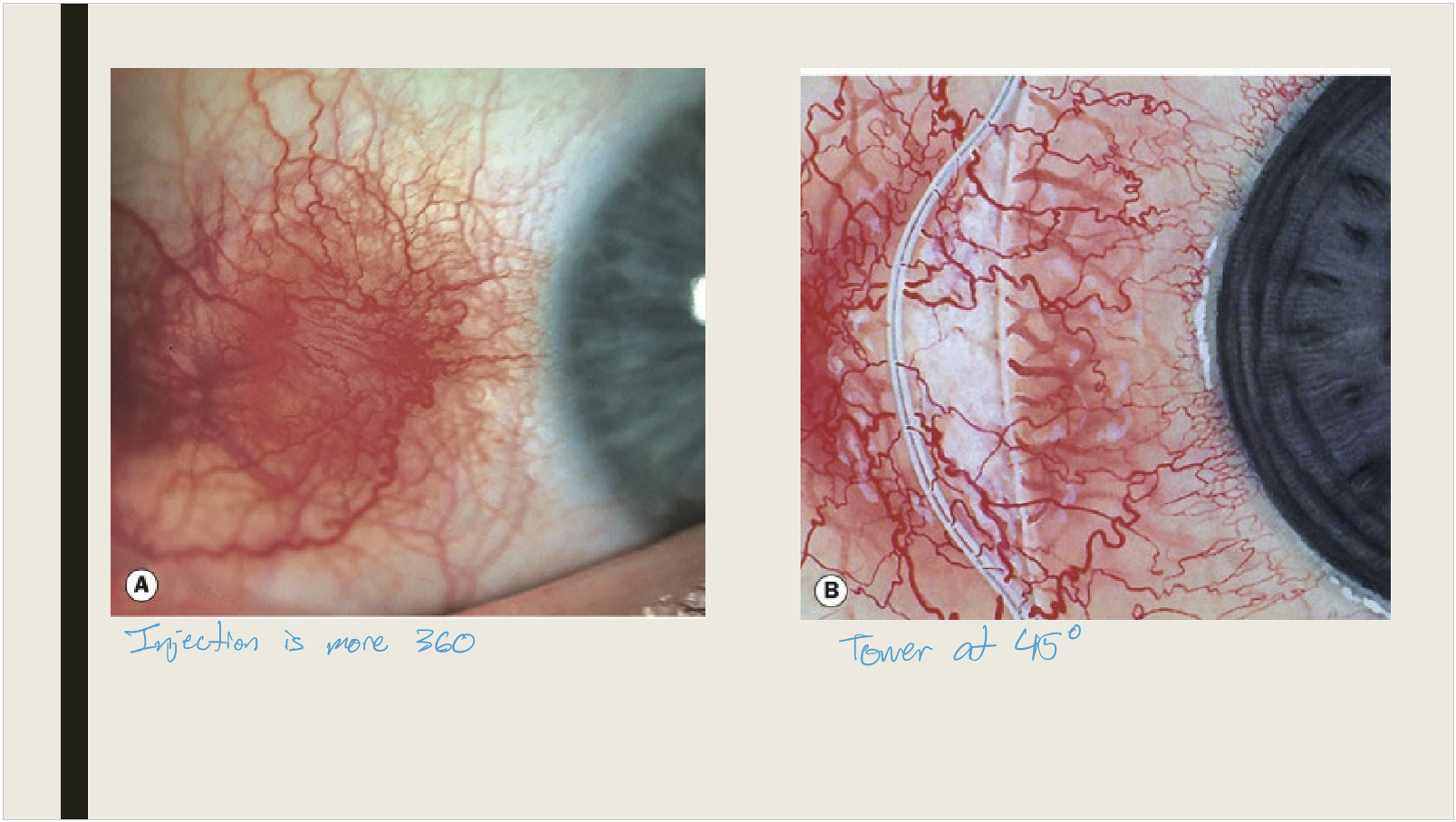
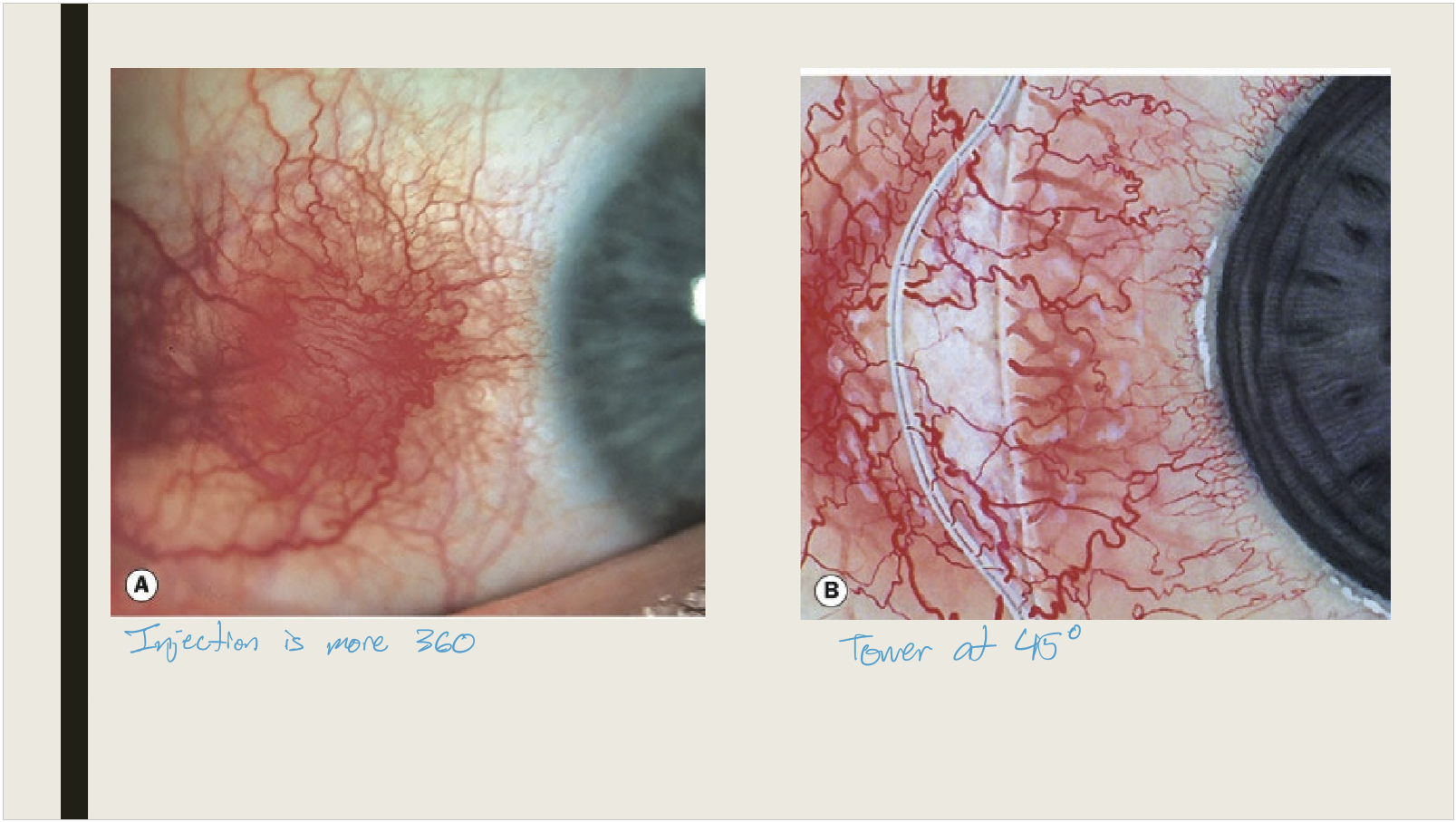
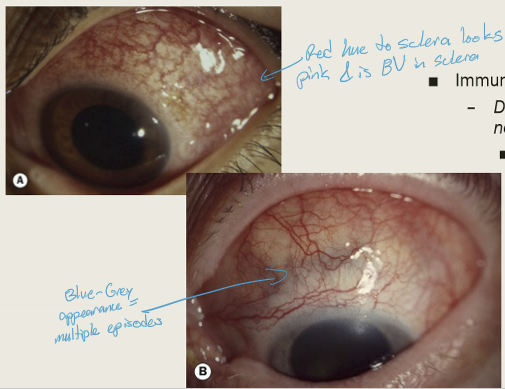
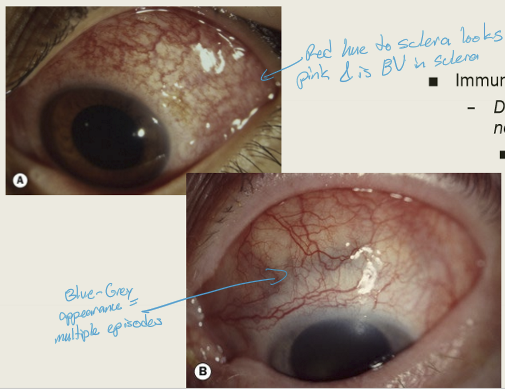
Vascular dilation and congestion with edema; sectoral or diffuse redness that does not blanch with 2.5% phenylephrine.
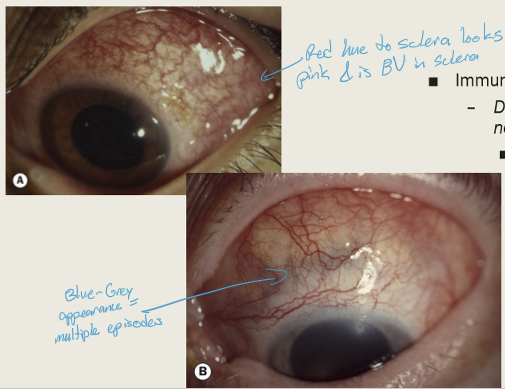
What happens to the sclera after resolution of diffuse anterior non-necrotizing scleritis?
It turns blue/grey.
What are the main treatment options for diffuse anterior non-necrotizing scleritis?
Oral NSAIDs, oral corticosteroids, and immunosuppressive agents.
Who is most commonly affected by nodular anterior scleritis, and at what age?
Females, typically in the 5th decade of life.
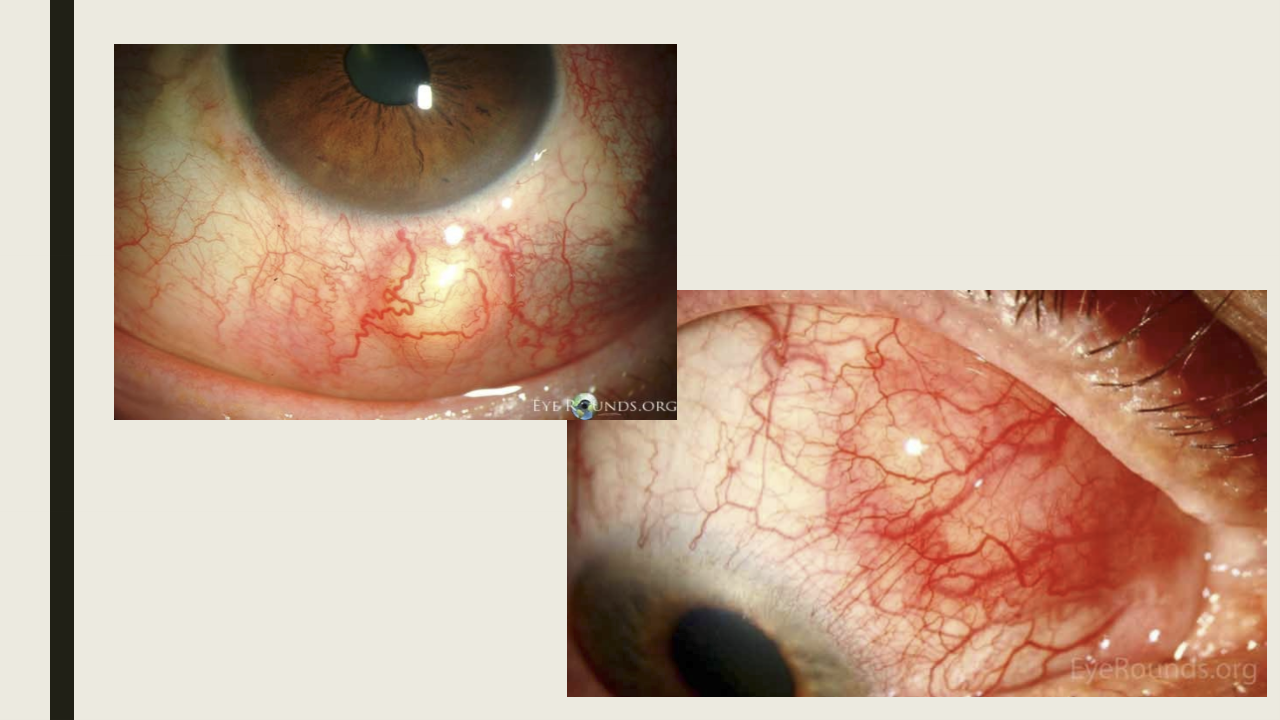
How does nodular anterior scleritis typically present?
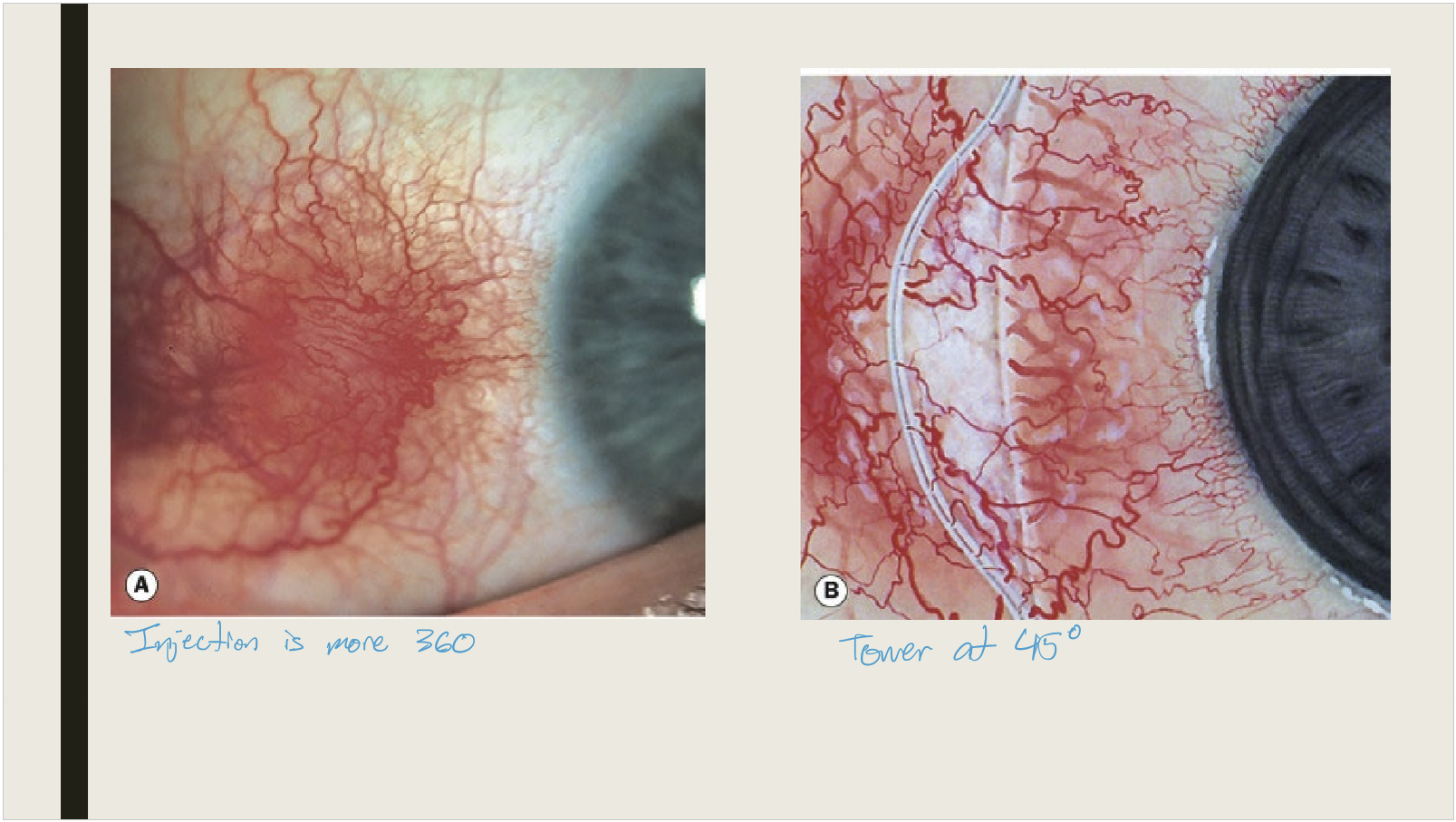
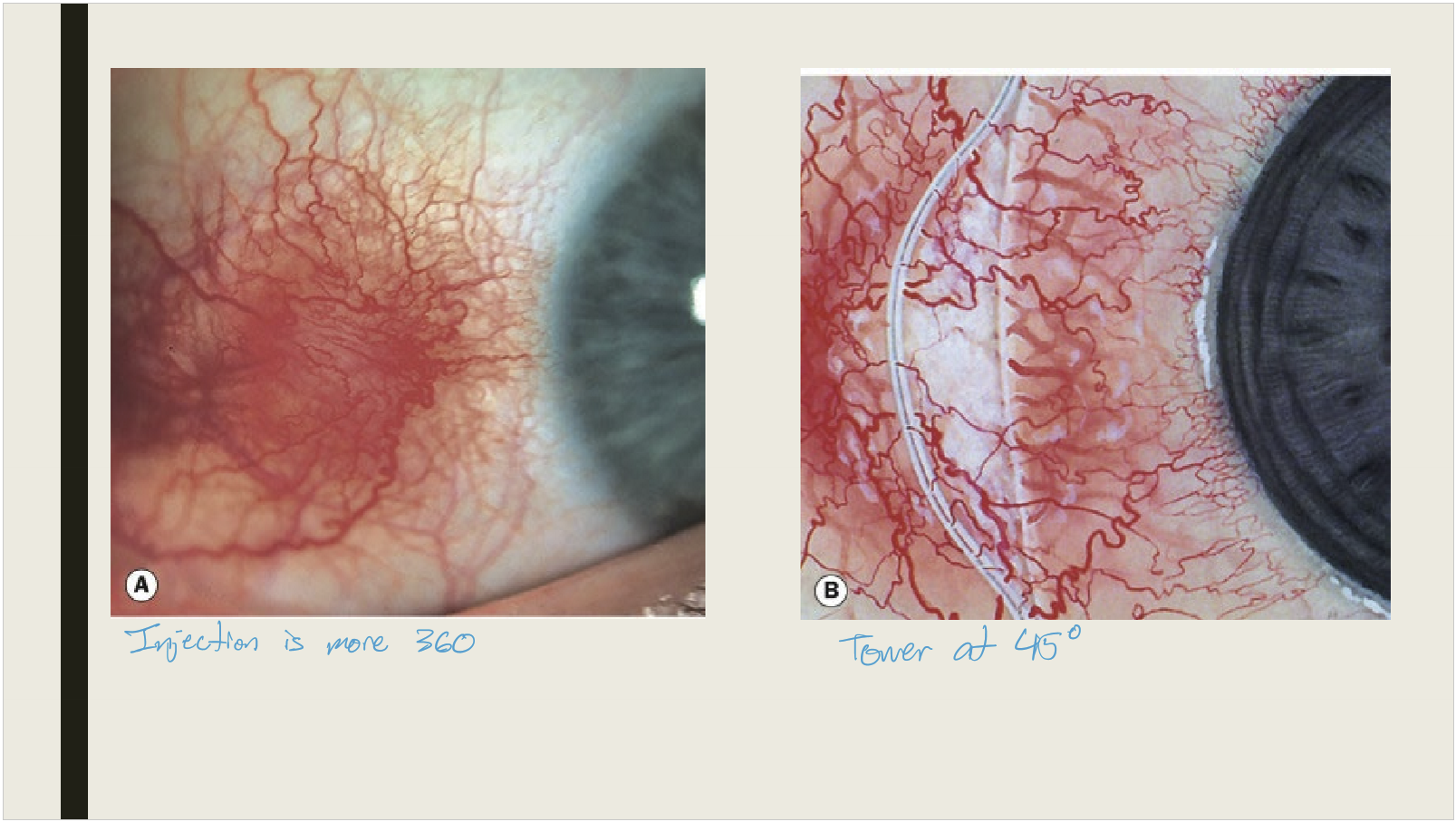
Sudden onset of severe pain
Ocular redness
One or more immobile nodules located in the interpalpebral space about 3 to 4 mm from the limbus
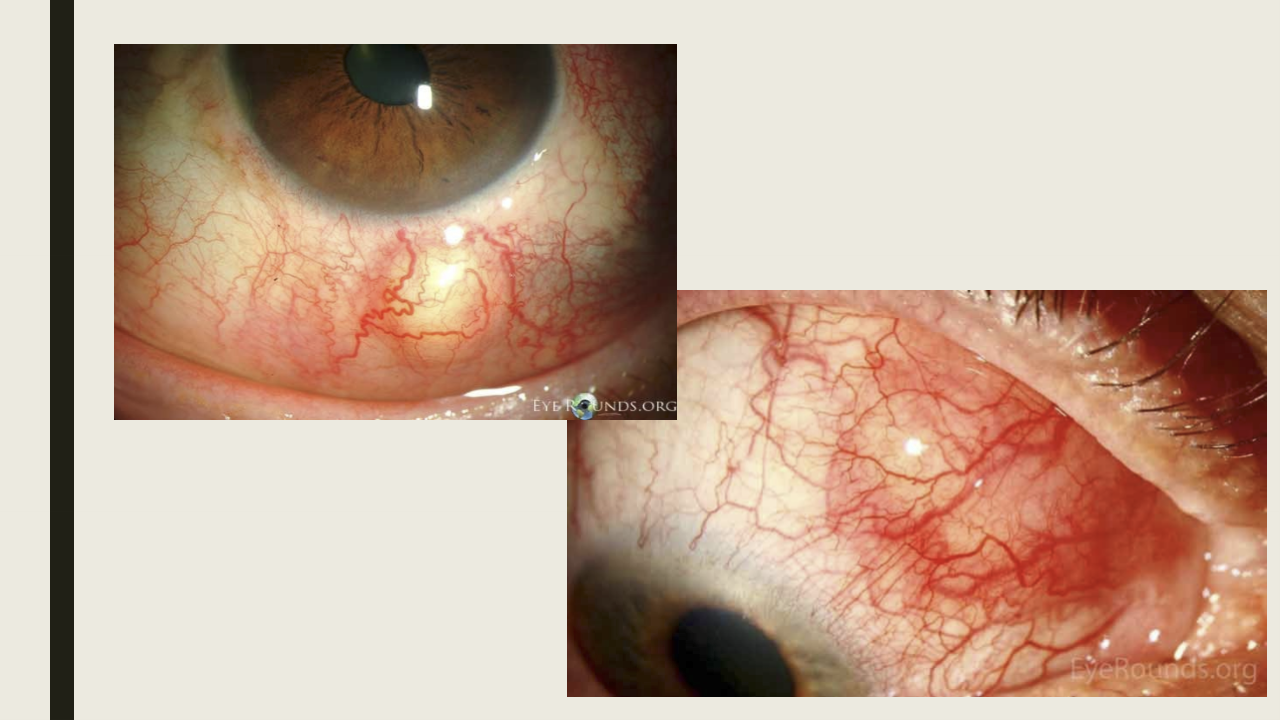
What is the characteristic appearance of nodules in nodular anterior scleritis?
Deep blue coloration; nodules are immobile.
What are the treatment options for nodular anterior scleritis?
Topical or systemic NSAIDs
Systemic corticosteroids
Systemic immunosuppressive medications (has lost of SE/last resort)
Conjunctival steroid injection for multiple episodes
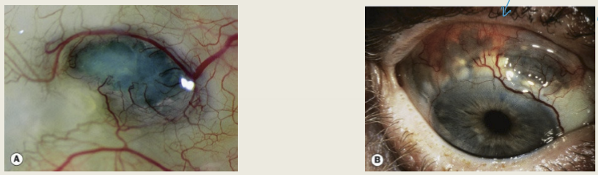
What is the most aggressive form of scleritis, and what is its consequence if untreated?
Anterior necrotizing scleritis with inflammation; can lead to severe visual morbidity and possible loss of the eye.
What is the typical age and laterality of anterior necrotizing scleritis with inflammation?
Usually presents around age 60 and is typically bilateral.
Describe the pain pattern in anterior necrotizing scleritis with inflammation.
Severe, persistent pain radiating to the temple, brow, or jaw; can interferes with sleep and does not respond to pain medication.
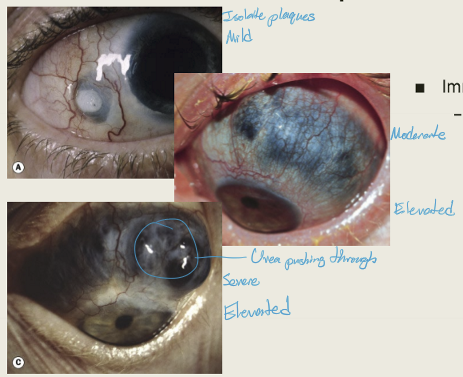
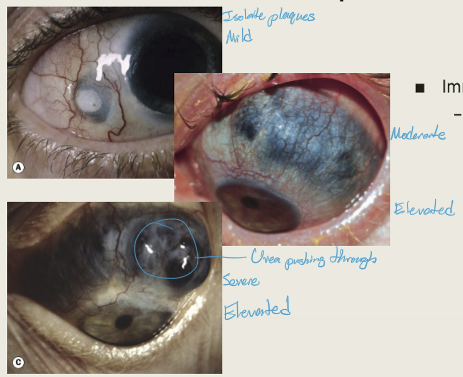
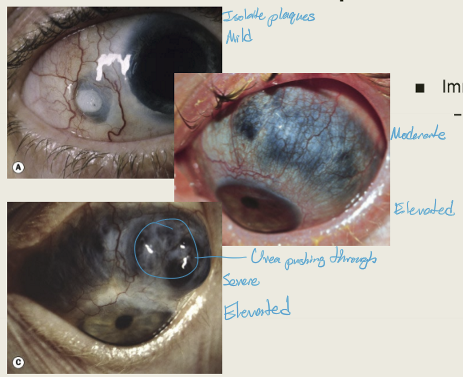
What are the three subtypes of anterior necrotizing scleritis with inflammation?
Vaso-occlusive, granulomatous, and surgically induced.
Which systemic condition is vaso-occlusive necrotizing scleritis often associated with?
Rheumatoid arthritis
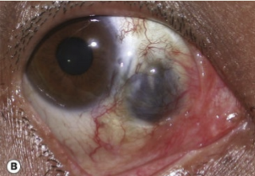
What is the characteristic ocular presentation of vaso-occlusive necrotizing scleritis?
Isolated patches of scleral edema with overlying areas of non-perfused episclera and conjunctiva.
Which systemic conditions are associated with granulomatous necrotizing scleritis?
Wegener granulomatosis and polyarteritis nodosa.
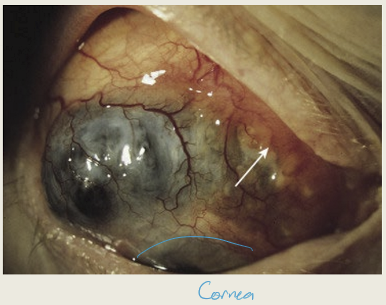
How does granulomatous necrotizing scleritis present clinically?
Edema of the sclera, episclera, conjunctiva, and cornea
Area becomes irregularly raised, starting at the limbus and extending posteriorly
When does surgically induced necrotizing scleritis typically occur, and after which procedures?
Usually within 3 weeks of surgery; associated with strabismus surgery, trabeculectomy, scleral buckle for retinal detachment, or pterygium excision with adjunctive mitomycin C.
What is the characteristic ocular finding in surgically induced necrotizing scleritis?
Scleral thinning begins at the surgical site and does not involve the entire eye.
What are the major complications of anterior necrotizing scleritis with inflammation?
Corneal complications: acute infiltrative stromal keratitis, sclerosing keratitis, peripheral ulcerative keratitis
Other ocular issues: uveitis, glaucoma, hypotony, and risk of perforation
Which laboratory tests help identify systemic associations in necrotizing scleritis?
RF: Rheumatoid arthritis
ANA: Autoimmune disorders
ANCA: Wegener granulomatosis
Antiphospholipid antibodies: Lupus and rheumatoid arthritis
What are the main treatment options for anterior necrotizing scleritis with inflammation?
Systemic corticosteroids
Periocular steroid injection
Immunosuppressive medications
Which systemic conditions are commonly associated with posterior scleritis?
Rheumatoid arthritis (most common), systemic lupus erythematosus, and granulomatosis with polyangiitis.
How is the pain of posterior scleritis typically described?
Moderate to severe, deep, dull, boring pain that interferes with sleep and worsens with eye movement.
What are the key clinical signs of posterior scleritis?
Pain and tenderness
Proptosis
Extraocular muscle restriction
Acute angle-closure glaucoma (due to anterior chamber changes)
Retinal findings: choroidal folds, exudative retinal detachment, papilledema
May coexist with anterior scleritis
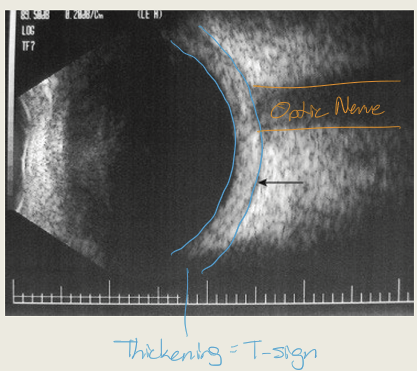
What is the most characteristic finding on B-scan ultrasonography in posterior scleritis?
The “T-sign”, caused by fluid in Tenon’s space; other findings include scleral thickening, nodules, separation of Tenon capsule, disc edema, choroidal folds, and retinal detachment.
What is the treatment for posterior scleritis?
Oral NSAIDs or oral corticosteroids or treat underlying infection
What is scleromalacia perforans and who is most commonly affected?
Necrotizing scleritis without inflammation; typically affects elderly women with rheumatoid arthritis.
How does scleromalacia perforans present clinically?
Pain: Absent
Findings: Necrotic scleral plaques near the limbus that coalesce and enlarge
Other: Vascular congestion absent; slow progression of scleral thinning
What are the treatments for scleromalacia perforans?
Systemic non-steroidal anti-inflammatory drugs
Systemic steroids
Immunosuppressive medication
What is rheumatoid arthritis and which demographic is most commonly affected?
An autoimmune, inflammatory condition primarily affecting joints; typically affects females over age 60.
Besides joints, which other tissues can rheumatoid arthritis affect?
Eyes, lungs, and heart.
How does rheumatoid arthritis typically present?
Joint pain, tenderness, swelling, or stiffness; often multiple joints on the same side of the body.
How is scleritis related to rheumatoid arthritis severity?
Mild RA is associated with non-necrotizing scleritis, while severe RA is linked to necrotizing scleritis.
What is Wegener granulomatosis and what type of vessels does it affect?
An inflammatory condition characterized by small-vessel vasculitis.
Which organs are commonly affected by Wegener granulomatosis?
Lungs, kidneys, and eyes.
Who is most commonly affected by Wegener granulomatosis?
Males in the fifth decade of life.
What are the key clinical features of Wegener granulomatosis?
Pulmonary symptoms with nodular lung lesions
Nasal deformities due to inflammation
Necrotizing glomerulonephritis (protein and blood in urine)
Necrotizing scleritis
What is relapsing polychondritis and what type of vessels does it involve?
An inflammatory condition of cartilage associated with small-vessel vasculitis.
Who is most commonly affected by relapsing polychondritis?
Equally affects males and females; usually diagnosed between the 4th and 6th decades.