Respiratory Handout
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Type I pneumocytes:
A. Cover less than 10% of the alveolar surface area.
B. Account for about 60% of alveolar epithelial cells.
C. Produce and secrete of surfactant.
D. Can replicate to replace damaged Type II pneumocytes.
E. Are responsible for gas exchange in the alveoli.
E. Are responsible for gas exchange in the alveoli.
In normal pulmonary circulation,
A. Blood flow is directly proportional to the overall resistance of the pulmonary vasculature.
B. Blood flow is lower than in systemic circulation.
C. Resistance to blood flow is higher than in systemic circulation.
D. Driving pressure for blood flow is higher than in systemic circulation.
E. Blood flow is about the same as in systemic circulation.
E. Blood flow is about the same as in systemic circulation.
Which of the following structures form part of the conducting zone?
A. Alveolar ducts
B. Alveolar sacs
C. Respiratory bronchioles
D. Trachea
E. Alveolar fluid with surfactant
D. Trachea
Lecture 2:
Transmural Pressures (Pressures across a Wall):
Transpulmonary and Trans-Chest-Wall Pressures.
For lungs to function normally and to prevent lungs from collapsing,
For lungs to function normally and to prevent lungs from collapsing:
The intrapleural pressure must be lower than alveolar pressure!
Normal FEV1/FVC ratio:
Normal FEV1/FVC ratio = 0.7 to 0.8
Below are NOT highlighted:
meaning that about 70-80% of the vital capacity can be expired in the first second of forced expiration.
Younger and taller people tend to have higher normal FEV1/FVC ratio.
✅FEV₁ = Forced Expiratory Volume in 1 second
How much air you can forcibly blow out in the first second of exhalation.
✅FVC = Forced Vital Capacity
The total amount of air you can forcibly exhale after a full inhalation.
In obstructive diseases such as asthma:
In obstructive diseases such as asthma:
both FVC and FEV1 are decreased, FEV1/FVC is also decreased
Below are NOT Highlighted:
Because decrease in FEV1 is often more pronounced than that in FVC
Changes in pulmonary arteriolar resistance and blood flow are controlled by:
Changes in pulmonary arteriolar resistance and blood flow are controlled by:
mainly by local factors, primarily PA(O2)
The normal overall ratio of alveolar ventilation (Va, L/min, normally 4 L/min) to pulmonary blood flow (Q, L/min, normally 5L/min) is approximately
The normal overall ratio of alveolar ventilation (Va, L/min, normally 4 L/min) to pulmonary blood flow (Q, L/min, normally 5L/min) is approximately:
4/5=0.8
What is the largest lung volume or capacity that can be inspired above FRC?
A. Inspiratory reserve volume
B. Inspiratory capacity
C. Vital capacity
D. Total lung capacity
E. Residual volume
B. Inspiratory capacity
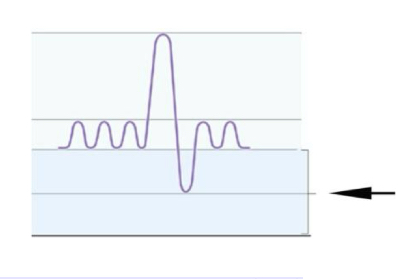
The lung volume or capacity indicated by the arrow in the following figure is
A. Inspiratory reserve volume (IRV)
B. Expiratory reserve volume (ERV)
C. Residual volume (RV)
D. Vital capacity (VC)
E. Functional residual capacity (FRC)
E. Functional residual capacity (FRC)
If ventilation/perfusion (V/Q) ratio of a lung region decreases, how will the Po2 and Pco2 in the blood in that region change?
A. Pco2 is decreased and Po2 is increased
B. Po2 is decreased and Pco2 is unchanged
C. Po2 is decreased and Pco2 is increased
D. Po2 is unchanged and Pco2 is increased
E. Both Po2 and Pco2 are decreased
C. Po2 is decreased and Pco2 is increased
Which of the following is/are often decreased in both restrictive and obstructive lung diseases?
A. Vital capacity
B. FEV1
C. FEV1/FVC
D. Both A and B
E. Both B and C
D. Both A and B
In dead space associated with pulmonary embolism,
A. V/Q ratio = 0
B. PAO2 is 40 mm Hg and PACO2 is 46 mm Hg
C. V/Q ratio = ∞
D. PAO2 is approximately 150 mmHg
E. Both C and D
E. Both C and D
Lecture 3:
Emphysema is associated with:
Emphysema is associated with:
loss of elastic fibers in the lungs.
As a result, the compliance of the lungs increases (↑)
In pulmonary fibrosis, the compliance of the lungs decreases (↓)
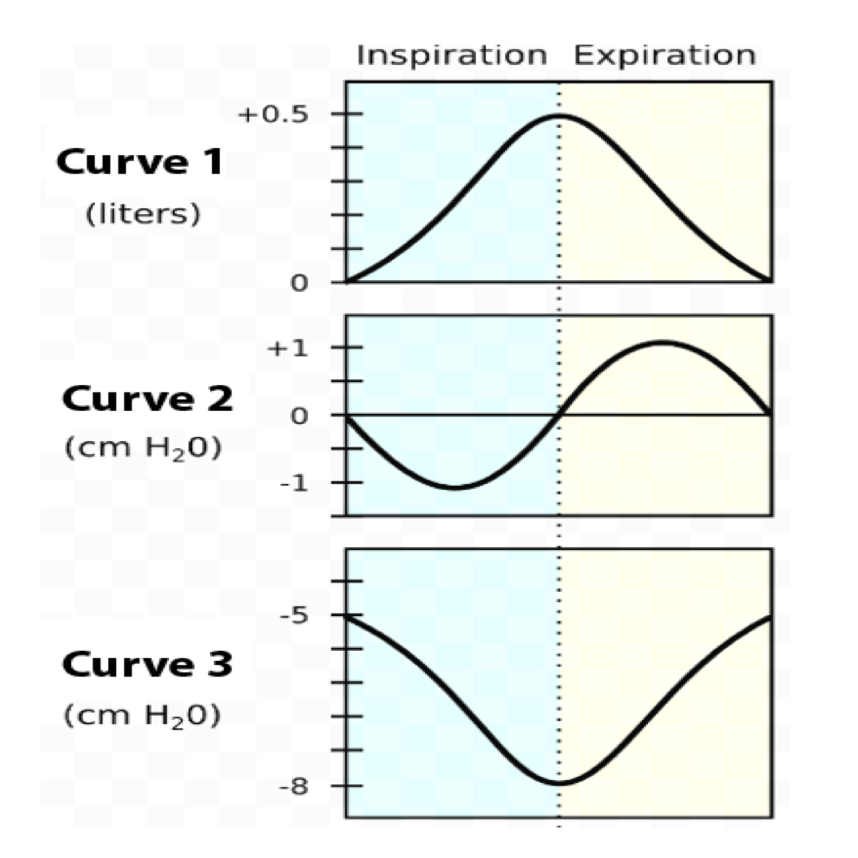
In the following figure, which curve most accurately reflects changes in intra-alveolar pressure during the breath cycle?
A. Curve 1
B. Curve 2
C. Curve 3
D. Both Curve 2 and 3
E. Both Curve 1 and 3
B. Curve 2
Which of the following statements about respiratory airflow is NOT TRUE?
A. The driving force for air flow is the pressure gradient ∆P in the airways.
B. According to the Law of Laplace, smaller spherical alveoli have higher collapsing pressure than the larger alveoli.
C. If the radius of an airway decreases by a factor of 2, resistance will increase by 16-fold.
D. The smallest airways are the sites of highest resistance due to their small radius.
E. Airflow is inversely proportional to the resistance of the airways.
D. The smallest airways are the sites of highest resistance due to their small radius.
Lecture 4:
Arterial oxygen saturation (SaO2):
Hemoglobin A is about:
Hemoglobin A is about 98% saturated at sea level when PaO2 = 100 mmHg in a normal adult.
Venous oxygen saturation (SvO2):
In normal mixed venous blood:
In normal mixed venous blood, hemoglobin is approximately 75% saturated.
Which of the following statements regarding gas exchange and transport is TRUE?
A. CO2 binds to hemoglobin to form carboxyhemoglobin in RBCs.
B. Carbonic anhydrase in the blood is predominantly located in plasma.
C. HCO3- is mostly transported inside red blood cells.
D. CO binds rapidly and irreversibly to hemoglobin.
E. HCO3- in plasma is quantitatively the major and most important form of CO2 transport in the blood.
E. HCO3- in plasma is quantitatively the major and most important form of CO2 transport in the blood.
Which of the following statements about chloride shift and CO2 transport is NOT true?
A. In systemic capillaries, bicarbonate moves into the red blood cells in exchange for chloride moving out.
B. Chloride shift is mediated by the anion transport protein Band 3.
C. Reverse chloride shift operates in pulmonary capillaries.
D. The major form of CO2 transport in the blood is carbaminohemoglobin.
E. Both A and D.
E. Both A and D.
Assuming the fractional concentration of O2 in inspired air is 0.21, and barometric pressure is 760 mm Hg,
The partial pressure of O2 (Po2) in dry inspired air will be:
A. 100 mm Hg
B. 150 mm Hg
C. 160 mm Hg
D. 180 mm Hg
E. 200 mm Hg
C. 160 mm Hg
Assuming the fractional concentration of O2 in inspired air is 0.21, and barometric pressure is 760 mm Hg,
If water vapor pressure at 37°C is 47 mm Hg, the Po2 in humidified tracheal air at 37°C will be:
A. 100 mm Hg
B. 110 mm Hg
C. 130 mm Hg
D. 150 mm Hg
E. 160 mm Hg
D. 150 mm Hg
Lecture 5:
Chloride Shift and Reverse Chloride Shift in Systemic and Pulmonary Capillaries:
Plasma bicarbonate HCO3- is:
Plasma bicarbonate HCO3- is quantitatively the major and most important form of CO2 transport in the blood.
pulmonary arterial blood has:
pulmonary arterial blood has: a higher bicarbonate ion concentration than systemic arterial blood.
Which of the following statements about oxygen transport in the blood is NOT TRUE?
A. Hemoglobin F has higher affinity for oxygen than adult hemoglobin A.
B. Methemoglobin does not bind oxygen.
C. 2,3-DPG interacts with the β chains of deoxyhemoglobin
D. Hemoglobin is normally 50% saturated when PaO2 is at 50 mmHg.
E. CO competes with oxygen at the same heme binding site in hemoglobin.
D. Hemoglobin is normally 50% saturated when PaO2 is at 50 mmHg.
Sickle-cell anemia is caused by
A. A missense mutation of the alpha chain of hemoglobin.
B. A deficiency in methemoglobin reductase.
C. Oxidation of Fe2+ to Fe3+ by nitrites and sulfonamides.
D. Increased binding affinity of hemoglobin S for oxygen.
E. A missense mutation of the beta chain of hemoglobin.
E. A missense mutation of the beta chain of hemoglobin.
Carbon monoxide
A. Binds irreversibly to hemoglobin A with high affinity.
B. Increases the saturation of hemoglobin by O2
C. Causes a right shift of the O2-hemoglobin dissociation curve.
D. Increases O2-binding capacity of blood.
E. None of the above.
E. None of the above.
Lecture 6:
No highlights
Central chemoreceptors
A. Are stimulated by a decrease in pH of the blood.
B. Are sensitive to a decrease in PaO2.
C. Detect changes in pH of the cerebrospinal fluid.
D. Are located close to the dorsal surface of the medulla.
E. Both C and D.
C. Detect changes in pH of the cerebrospinal fluid.
Peripheral chemoreceptors in the aortic body
A. Are significantly activated when PaO2 drops to 85 mmHg
B. Are highly sensitive to changes in pH in cerebrospinal fluid (CSF)
C. Produce hyperventilation when PaO2 is increased.
D. Are insensitive to changes in PaCO2
E. Produce a rapid increase in breathing rate when PaO2 is dropped to 55 mmHg.
E. Produce a rapid increase in breathing rate when PaO2 is dropped to 55 mmHg.
Which of the following is most likely to occur in a healthy visitor to high altitude?
A. Decrease in PaO2 directly activates central chemoreceptors.
B. Oxygen-hemoglobin dissociation curve shifts to left.
C. Metabolic acidosis develops.
D. Synthesis of erythropoietin is decreased.
E. Respiratory alkalosis may develop.
E. Respiratory alkalosis may develop.
Respiratory Physiology Review:
A case of CO poisoning:
A 55-year-old man decides to warm his car in the garage. While the car is warming, he waits in a workshop adjoining the garage. About 30 minutes later, his wife found him tinkering at his workbench, confused and breathing rapidly. He was taken to a nearby emergency department and immediately given 100% O2 to breathe. The following arterial blood values are then measured: PaO2: 660 mm Hg; PaCO2: 36 mmHg; pH: 7.43; Percent O2 saturation of hemoglobin: 60%. If the solubility of O2 in blood is 0.003 mL O2/100 mL blood/mm Hg, what is the expected dissolved O2 concentration in this patient’s blood?
A. 0.98 mL O2/100 mL blood.
B. 1.98 mL O2/100 mL blood.
C. 2.98 mL O2/100 mL blood.
D. 3.98 mL O2/100 mL blood.
E. 4.98 mL O2/100 mL blood.
B. 1.98 mL O2/100 mL blood.
Which of the following is a structural characteristic of alveolar sacs?
A. The alveolar walls are consisted of ciliated epithelium.
B. The alveolar walls are rich in cartilage.
C. The alveolar walls are rich in smooth muscle cells.
D. Type I alveolar cells cover over 95% of the alveolar surface area.
E. Type I alveolar cells are primarily responsible for producing surfactant.
D. Type I alveolar cells cover over 95% of the alveolar surface area.
Which of the following is a common characteristic of chronic obstructive pulmonary disease
(COPD)?
A. CO poisoning is common
B. FEV1 is increased
C. FEV1/FVC ratio is decreased
D. Total lung capacity is reduced
E. Vital capacity is increased
C. FEV1/FVC ratio is decreased
Which of the following describes functional residual capacity (FRC)?
A. Tidal volume + residual volume
B. Vital capacity + residual volume
C. Inspiratory capacity + residual volume
D. Inspiratory reserve volume + residual volume
E. Expiratory reserve volume + residual volume
E. Expiratory reserve volume + residual volume
Which of the following is the principal muscle responsible for inspiration during quite
breathing?
A. The scalene muscles
B. Abdominal wall muscles
C. The diaphragm
D. The sternocleidomastoid muscles
E. Pectoralis Minor
C. The diaphragm
A 46-year-old woman at high altitude presents with respiratory alkalosis. Her arterial blood
pH is __________ due to ___________________.
A. decreased; CO2 retention
B. increased; CO2 retention
C. decreased; hypoventilation
D. increased; hyperventilation
E. decreased; increased PaO2
D. increased; hyperventilation
Which of the following respiratory regulatory component is mostly present on the medulla
oblongata?
A. Pneumotaxic center
B. Apneustic center
C. Peripheral chemoreceptors
D. Inspiratory center
E. Irritant receptors
D. Inspiratory center
Vital capacity
A. is the tidal volume plus the inspiratory reserve volume
B. includes all of the lung volumes
C. is composed of the inspiratory capacity plus the expiratory reserve volume
D. is the expiratory reserve volume (ERV) plus the residual volume
E. is approximately 1200 mL in normal human subjects.
C. is composed of the inspiratory capacity plus the expiratory reserve volume
Under normal physiological conditions, partial pressure of CO2 in arterial blood is
approximately
A. 64 mm Hg
B. 100 mm Hg
C. 46 mm Hg
D. 760 mm Hg
E. None of the above
E. None of the above
In case of acute mild CO poisoning,
A. P50 for oxygen binding to hemoglobin is increased.
B. O2 content of arterial blood is decreased.
C. SaO2 is increased.
D. PaO2 is normal.
E. Both B and D.
E. Both B and D.
Which of the following typically can NOT cross the blood–brain barrier by diffusion?
A. H+
B. HCO3-
C. CO2
D. Both A and B
E. Both B and C
D. Both A and B
Hyperventilation
A. Increases the oxygen supply to brain
B. Decreases PaCO2
C. Decreases the pH of systemic arterial blood
D. Decreases binding affinity of hemoglobin for O2
E. Both A and B
B. Decreases PaCO2
At which of the following sites is the partial pressure of oxygen (PO2) the highest?
A. Exhaled gas
B. Anatomical dead space at the end of expiration
C. Anatomical dead space at the end of inspiration
D. Alveolar gas
E. About the same PO2 in all of the above.
C. Anatomical dead space at the end of inspiration
The stretch receptors for the Hering-Breuer reflex are primarily found in
A. Aortic bodies
B. Carotid sinus
C. The ventral surface of medulla
D. The smooth muscle of the airways
E. The joints and muscles of limbs
D. The smooth muscle of the airways
In an average sized person with no lung pathology, the normal FRC is approximately
A. the same as FVC
B. 2400 mL
C. 1200 mL
D. 3000 mL
E. 500 mL
B. 2400 mL
The sites of highest airway resistance are found in
A. The smallest airways
B. The medium-sized bronchi
C. The largest airways
D. Alveoli
E. Terminal bronchioles
B. The medium-sized bronchi
Residual volume (RV)
A. Is the volume of gas remaining in the lungs after a maximal inspiration.
B. Is the residual volume that can be expired below tidal volume.
C. Is approximately 3000 mL in normal humans.
D. Can be measured directly by spirometry.
E. Is approximately 1200 mL in normal human subjects.
E. Is approximately 1200 mL in normal human subjects.
Physiologic dead space (VD)
A. Refers to the space of airways and lungs lined with dead alveolar cells.
B. Refers to the volume of the airways and lungs that participates in CO2 exchange only.
C. Is the total volume of the lungs that participate in O2 exchange only.
D. Includes the anatomic dead space plus a functional dead space in the alveoli.
E. Is approximately 350 mL under normal resting condition.
D. Includes the anatomic dead space plus a functional dead space in the alveoli.
Carbon monoxide is highly poisonous because
A. CO binds irreversibly to hemoglobin to form carboxyhemoglobin.
B. It causes a right shift of the O2-hemoglobin dissociation curve.
C. Binding of CO at one of O2-binding sites in hemoglobin decreases the oxygen affinity of the remaining sites.
D. CO binds to hemoglobin with an affinity that is 25 times that of O2
E. None of the above.
E. None of the above.
Which cause of hypoxemia is associated with increased A - a gradient?
A. High altitude
B. Hypoventilation
C. breathing 10% O2
D. V/Q defects and fibrosis
E. Left-to-right shunt
D. V/Q defects and fibrosis
Which of the following increases P50 in O2-hemoglobin dissociation curve?
A. CO poisoning
B. increased H+ concentration
C. decreased PCO2
D. decreased 2,3-diphosphoglycerate (DPG) concentration
E. decreased body temperature
B. increased H+ concentration
Which of the following statements about pulmonary blood flow is NOT true?
A. Cardiac output of the right heart is ejected from the right ventricle and is delivered to the lungs via the pulmonary artery.
B. When a person is standing, blood flow is lowest at the base (bottom) of the lungs and highest at the apex (top) of the lungs.
C. The blood that leaves the ventilated pulmonary capillaries is oxygenated.
D. Bronchial pulmonary circulation does not participate in gas exchange.
E. The pulmonary circulation is characterized by much lower pressure and resistance than the systemic circulation.
B. When a person is standing, blood flow is lowest at the base (bottom) of the lungs and highest at the apex (top) of the lungs.
Which of the following statements about physiologic shunt is NOT true?
A. It refers to a large fraction of pulmonary blood that flows directly to the alveoli
B. One source of physiologic shunt is bronchial pulmonary blood flow
C. Another source of physiologic shunt is a small portion of coronary venous blood that drains directly into the left heart.
D. In pathologic conditions involving ventilation/perfusion defect, the physiologic shunt may be increased.
E. Due to physiologic shunt, systemic arterial blood may have a slightly lower Po2 than alveolar air.
A. It refers to a large fraction of pulmonary blood that flows directly to the alveoli
A normal child with TLC of 2.5 liters, VC of 2.0 liters, and ERV of 0.5 liters would most likely have an FEV1 of approximately
A. 0.6 liters
B. 1.6 liters
C. 2.6 liters
D. 3.6 liter
E. 4.6 liters
B. 1.6 liters
What is the oxygen binding capacity of the blood when the hemoglobin count is 10g/dL?
A. 10.4 mL per deciliter.
B. 13.4 mL per deciliter.
C. 23.4 mL per deciliter.
D. 18.4 mL per deciliter
E. 25.4 mL per deciliter.
B. 13.4 mL per deciliter.
A man who has a tidal volume of 550 mL is breathing at a rate of 14 breaths/min. His estimated dead space is 138 mL.
What is his minute ventilation?
A. 3300 mL/min
B. 1200 mL/min
C. 7700 mL/min
D. 6500 mL/min
E. None of the above.
C. 7700 mL/min
A man who has a tidal volume of 550 mL is breathing at a rate of 14 breaths/min. His estimated dead space is 138 mL.
What is his alveolar ventilation?
A. 556 mL
B. 1235 mL
C. 3065 mL
D. 3568 mL
E. 5768 mL
E. 5768 mL
A man who has a tidal volume of 550 mL is breathing at a rate of 14 breaths/min. His estimated dead space is 138 mL.
What percentage of each tidal volume reaches functioning alveoli?
A. About 55%
B. About 65%
C. About 75%
D. About 85%
E. About 95%