Dyspepsia
1/12
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
What is dyspepsia?
disregulation of acid production within the gastric system
Who does peptic ulcer disease affect? (population groups)
children but rare, gastric ulcers peak population 55-65, duodenal ulcers 25-75, male risk is twice female risk, women commonly gastrc rather than duodenal
What are some of the risk factors associated with peptic ulcers?
genetic factors and family hstory as could be down to increased acid production, weaker mucosa, abnormal mucus production
caffeine, smoking, alcohol, NSAIDs (partcularly high dose, long term), Stress

How can you tell where peptc ulcer is based on symptoms?
poorly, gastric made worse by food and more likely than duodenal to be associated with weight loss, anorexia and nausea
When do you need to be worried about gastric cancer?
anyone over 45 with peptic ulcer disease as it can be be a precurcer
Why do you increase acid production durng stress?
flight or fight, need more nutrition so the ACh triggers secretion of acid
What is the aetiology of peptic ulceration?
not presisely known but many contibutary factors, excessive acid production or intrinsic defect in the mucosal barrier
gastric ulcers normally due to inflammatory response of parietal cells due to damage to underlying mucosa
duodenal ulcers normallt associated with high acid/low bicarbonate
infection with H. Pylori
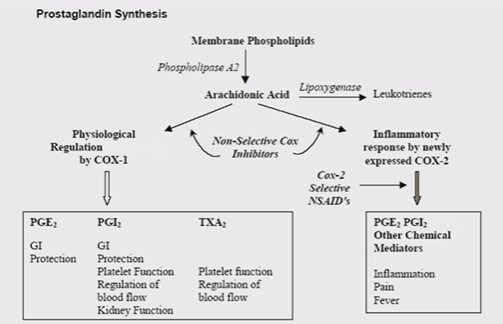
long term use of NSAIDs as block COX enzymes decreasing prostaglandn production
errosion eventually reaches the muscularis layer, gastric pain is triggered due to the nerve complexes underneath, if not treated this leads to a chronic ulcer which can perferate the gastric system and can be life threatening
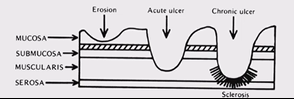
How does a gastric ulcer develop?
assocated with normal or decreased acid secreation, due to damage to parietal cells that normal produce the acid, causes atrophic gastritis
How does a duodenal ulcer develop?
associated with increased acid secretion, gastric inflammation elevated in antral/pyloric region, killing off D cells but not parietal cells, so acid production is the same and somatastatin production is reduced so it can’t switch acid production off, this means more acid goes into the duodenum causes issues as its not protected, increased gastrin release
What is H.Pylori?
Helicobacter Pylori , damages the mucosa, secretes urase which nutralises the acid, causes more damage to the mucosa (urea), acid then causes futher damage, can treat and reduce it but can’t eliminate it completly
How can NSAIDs cause Gastric ulcers?
If on NSAIDs for a long period of time causes thining of the mucosa so the underlying mucosa is suseptible to damage, this is due to them reducing prostaglandin formation as they inhibit COX 1 as well as COX 2, causes gastric ulceraton and bleeding, can be prevented with a stable PG₁ analogue
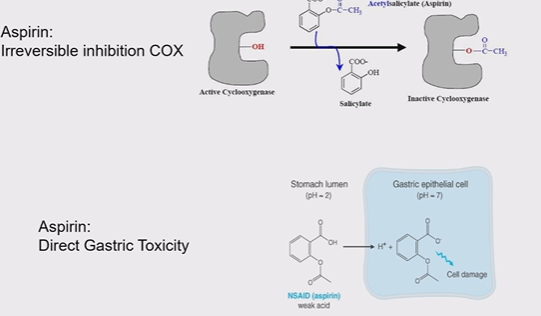
Why is asprin in partcular bad for the gastic mucosa
it irriversibly covently blocks COX 1 receptors, asprin become ionised in the stomach mucosa as it is a weak acid, directly damaging it, this is why asprin is enteric coated
What are the effects of switching off the COX enzymes?
mucus secretion decreases, loose cell regenaration ability, decrease HCO₃⁻ release, increases H⁺, and decreases blood flow