Week 8 - Membranes, Temperature
1/102
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
103 Terms
What is the difference between the terms "mucous" and "mucus"?
- Mucous = adjective
- Mucus = noun
What do mucous membranes do?
- Mucous membranes line the cavities of the body which are contiguous with the skin and exposed to the external environment, providing secretions to keep the body structures moist
What are some examples of body systems where mucous membranes can be found?
- Respiratory tract
- GIT
- Urinary tract
- Reproductive tract
What are some mucous membranes which can be easily assessed on physical exam?
- Oral cavity (tongue, inner lip, gums)
- Vulva/prepuce
- Conjunctiva
- Rectoanal
On a physical exam, what factors should be assessed regarding mucous membranes?
- Color
- Feel
- CRT
How can the "feel" of mucous membranes be assessed?
- Using your bare finger, gently touch the mucous membrane
What do the following "feelings" of mucous membranes indicate?
A. Moist
B. Dry and tacky
C. Signs of hypersalivation
A. Normal
B. Dehydrated, potentially excess panting
C. Nausea, nervous, pain, hepatic encephalopathy
What physical exam findings would be associated with the following states?
A. Euhydrated
B. Mild (~5% dehydrated)
C. Moderate (~8% dehydrated)
D. Severe (>10% dehydrated)
A. Normal
B. Minimal loss of skin turgor, semi-dry mucous membranes, normal eye
C. Moderate loss of skin turgor, dry mucous membranes, weak rapid pulses, enophthalmos
D. Considerable loss of skin turgor, severe enophthalmos, tachycardia, extremely dry mucous membranes, weak/thready pulses, hypotension, altered level of consciousness
How is CRT assessed?
- Lightly compress the mucosa by transiently arresting capillary flow and observing how many seconds it takes for color to return
What does a prolonged CRT indicate (>2 s)?
- Poor tissue perfusion (Decreased CO vs. severe dehydration)
How sensitive./specific is CRT?
- Highly subjective and insensitive
What is mucous membrane color determined by?
- Amount of oxygenated hemoglobin in the blood
- Degree of tissue blood flow
- Presence of other pigments (hemoglobin, myoglobin, bilirubin
What is pallor?
- Paleness of tissue
What are the 2 major causes of pallor?
1) Lack of oxygenated hemoglobin (anemia)
2) Poor tissue perfusion (shock, vasoconstriction)
What is a normal HCT for a....
A. Cat
B. Dog
C. Puppy (6-8 weeks old)
A. 30-45%
B. 35-55%
C. 27-36%
What evidence of poor perfusion can be found on a physical exam?
- Prolonged CRT
- Weak peripheral pulses
- Arrhythmias
What evidence of anemia can be found on a physical exam?
- CRT usually normal
- Bounding peripheral pulses
- Evidence of blood loss
By what mechanism does tachycardia result in pallor?
- Both mechanisms (Lack of oxygenated hemoglobin (anemia), Poor tissue perfusion (shock, vasoconstriction))
What laboratory tests can be used to work-up pallor in an emergency setting? What about if there is more time?
- Emergency: PCV/TS, BP
- Additional: EKG to assess for arrhythmia causing poor perfusion, coagulation tests, abdominal/thoracic imaging, CBC with reticulocytes
What is hyperemia?
- Increased arterial blood (pre-capillary) flow to a tissue
What are some causes of hyperemia
- Physiologic (Secondary to excitement, exercise, heat)
- Pathologic (Response to inflammation, heatstroke, sepsis)
What would one expect the CRT to be in a hyperemic patient?
- Delayed to shortened
What are some things to rule out when hyperemia is suspected?
- Gingivitis
- Erythrocytosis
- CO poisoning
- CN intoxication
What is cyanosis?
- Blue discoloration of mucous membranes
What causes cyanosis?
- Presence of large amounts of deoxygenated hemoglobin
What are the two types of cyanosis? Briefly describe them.
1) Central cyanosis - Global deoxygenation of arterial blood
2) Peripheral cyanosis - Local reduction in oxygenated hemoglobin
What are some causes of central cyanosis?
- Pulmonary disease
- Cardiovascular disease
- Diseases preventing hemoglobin from carrying oxygen (methemoglobin)
What are some causes of peripheral cyanosis?
- Obstruction of blood flow
- Vasoconstriction
Cyanosis occurs when deoxygenated hemoglobin is over _________________ within the capillary bed. In animals with normal hemoglobin levels, oxygen saturation must fall below ______________ for visible cyanosis to occur.
- Over 5g/100 mL
- 80%
Why is cyanosis rare in anemic animals, even though they may be hypoxemic?
- There is not enough hemoglobin present to allow visible cyanosis
What are causes of central cyanosis?
- Hypoxemia (usually the cause - V/Q mismatch)
- Hypoventilation
- Macroscopic venous to arterial shunting
- Methemoglobinemia
Explain what occurs with a V/Q mismatch leading to hypoxemia.
- Oxygen exchange impaired at the level of the alveolus
- Perfusion without ventilation: blood flowing to alveolus becomes inadequately oxygenated
- Ventilation without perfusion: oxygenate alveolus has inadequate blood flow
What are some causes of hypoxemia and subsequent central cyanosis?
- Pulmonary infiltration (pulmonary edema, pneumonia, neoplasia, acute respiratory distress syndrome, pulmonary fibrosis, pulmonary contusions, pulmonary hemorrhage)
- Pulmonary thromboembolism
Describe how hypoventilation results in central cyanosis.
- There is no V/Q mismatch, but the delivery of oxygen to the alveolus is impaired
What are some causes of hypoventilation?
- Elevated pleural pressure (pleural effusion, pneumothorax)
- Depressed respiratory drive (neurologic disease, drug overdose)
- Obstruction (laryngeal paralysis, tracheal foreign body, mass in large airway)
- Inadequate oxygenation of inspired gas (high altitude, anesthetic accident)
What is macroscopic venous to arterial shunting?
- Shunting of blood due to changes in pressure gradient causes mixing of deoxygenated with oxygenated blood
What are causes of macroscopic venous to arterial shunting?
- Cardiac causes (uncommon) including Tetralogy of Fallot, ASD or VSD with pulmonic stenosis, tricuspid valve dysplasia, or pulmonary hypertension, and R to L PDA
- Extra-cardiac causes (pulmonary arterivenous fistula)
Describe the pathophysiology of methemoglobinemia.
- Methemoglobin is a product of hemoglobin oxidation, normally maintained in low levels by methemoglobin reductase. If methemoglobin reductase is absent or overwhelmed, methemoglobin levels rise
What are some causes of methemoglobinemia?
- Acquired (acetaminophen, topical benzocaine products, skunk musk, hydroxyurea, nitrates/nitrites, fermented bok chou/brassica spp.)
- Congenital (lack of methemoglobin reductase (rare) or NADH-cytochrome b5 reductase deficiency)
If > ___________% of total Hb is methemoglobin, muddy mucous membranes will be seen.
- 10
_____________ causes of cyanosis may be more common in a young animal while ____________ causes may be more common in an older animal.
- Congenital
- Acquired
Polycythemia can indicate chronic ________________.
- Hypoxia
How is cyanosis treated?
- Oxygen (if obstruction or hypoventilation are present, these must be addressed before oxygen therapy will be beneficial)
- Thoracocentesis
- Treat underlying cause
What is icterus?
- Jaundice, Yellow color to the mucous membranes due to hyperbilirubinemia
Describe the normal metabolism of hemoglobin.
- Senescent RBCs are removed from circulation by mononuclear phagocytic system in the spleen, liver, and bone marrow. Heme is metabolized to bilirubin in mononuclear cells and bilirubin is released into the bloodstream. It is then absorbed in the liver. In the liver, bilirubin is processed, excreted into the bile, enters the GIT, and is reabsorbed in the ileum or undergoes further processing to stercobilin to be excreted in the feces or urobilinogen to be taken up in the blood and excreted into the urine
What are causes of pre-hepatic icterus?
- Breakdown of heme proteins (i.e., hemolysis and overactive monocular phagocyte system)
What are causes of hepatic icterus?
- Defective conjugation or uptake of bilirubin by the hepatocyte (i.e., liver failure)
What are causes of post-hepatic icterus?
- Problem occurs outside of the liver and affects bile flow (i.e., bile duct obstruction - stones, infection, inflammation, neoplasia, pancreatitis)
What two lab tests must be evaluated together to determine whether icterus is pre-hepatic, hepatic, or post-hepatic?
- CBC
- Serum chemistry
What are the liver enzymes and liver synthetic markers?
- Hepatocellular enzymes: ALT (cats/dogs only), SDH, GLDH
- Cholestatic: ALP (cats/dogs only), GGT - poor indicators of hepatic function
- Liver synthetic markers: BUN, glucose, albumin, cholesterol
How is an abdominal ultrasound used in the evaluate of icterus?
- Differentiate hepatic and post-hepatic icterus
True or false: Icterus will resolve as soon as hyperbilirubinemia resolves.
- False; Icterus may persist long after hyperbilirubinemia has resolved because bilirubin is bound to albumin and CT
What are petechiae?
- Small hemorrhages resulting from leakage of blood from capillaries
Petechiae are a characteristic of ___________________________________ disorders.
- Primary hemostatic
What are the causes of petechiation?
- Thrombocytopenia
- Thrombocytopathia
- Vasculitis
- Von Willebrand's Disease (rarely manifests with petechiation)
True or false: The degree of petechiation caused by thrombocytopenia always correlates with the degree of thrombocytopenia.
- False
What are causes of thrombocytopenia?
- Decreased production (toxins/drugs, infectious diseases)
- Increased destruction (IMTP)
- Consumption (DIC, hemorrhage)
- Sequestration (splenomegaly, hepatomegaly); This form of thrombocytopenia rarely causes petechiation
What are causes of thrombocytopathia?
- Inherited
- Acquired (Uremia, liver disease, dysproteinemia - lymphoma, multiple myeloma, drugs that inhibit platelet function like aspirin and clopidogrel)
What are causes of vasculitis?
- Infectious (tick-borne, streptococcus equi., BTV)
- Immune-mediated inflammation
- Neoplasia
- Drug reactions
What are some particular history questions to consider in regards to petechiation?
- Drug history
- Recent vaccinations?
- Tick-exposure history
- History of similar episodes in a family member (inherited)
What labwork may be useful in working up a patient with petechiation?
- CBC
- BMBT
- Genetic testing for inherited thrombocytopathies or vWD
- Coagulation testing (PT/PTT)
- Bone marrow aspirate/biopsy
- Infectious disease testing (tick borne disease, salmon poisoning disease)
- PFA 100
What happens when body temperatures fall below normal?
- Metabolic processes slow down, impairing body function
- If severe, cardiac fibrillation and death can occur
What happens when body temperatures rise above normal?
- Increased metabolic state and increased oxygen consumption
- Suppression of appetite center
- If severe, multiple organ dysfunction and death can occur
Describe poikilotherms. What types of animals are poikilotherms?
- Body temperature varies with environmental temperature; Behavior methods are used to prevent changes in body temperature
- Fish, reptiles, amphibians
Describe homeotherms. What types of animals are homeotherms?
- They maintain constant body temperature in presence of considerable changes in environmental temperature by maintained a high metabolic rate to provide heat needed to maintain body temperature within a normal range
- Mammals and birds
Control of core body temperature is a balance between which factors?
- Heat production
- Heat conservation
- Heat loss
Body heat is produced by what?
- Basal metabolic activity
- Muscle activity (movement and shivering)
- Digestion
- Thyroxine
- Sympathetic stimulation
How is body heat conserved?
- Autonomic stimulation (reduced peripheral circulation and heat loss through the skin, piloerection for increased insulation)
- Behavioral changes (huddling, grouping, seeking shelter)
What are the mechanisms of heat loss? Describe them briefly.
1) Conduction (transfer of heat to another substance (an object) - like a conduction stove in which the pan has to touch the stove)
2) Convection (transfer of heat to air or water - like an oven blowing hot air)
3) Radiation (heat lost from body surface by IR radiation)
4) Evaporation (heat lost when water in sweat, saliva, and respiratory secretions is converted to water vapor)
Which mechanism of heat loss predominantes as ambient temperatures rise?
- Evaporation (via respiratory tract in ruminants and dogs, via skin/sweat in horses in humans)
Heat in the body is primarily produced in the _____________ and ___________, and primarily eliminated through the ____________ and _________________________
- Muscles
- Liver
- Skin
- Respiratory tract
True or false: Tissues are excellent conductors of heat while the bloodstream is a poor conductor.
- False; Tissues are poor conductors while heat is most effective transferred through the blood stream (circulatory convection)
Do countercurrent exchange mechanisms conserve heat or contribute to heat loss?
- Can both conserve and lose heat
What is the function of the anterior hypothalamus in body temperature controle?
- Acts as a thermostat → 'set-point' at which the core body temperature will be maintained
- Transition of the core temperature below or above the set-point will alter behavioral and homeostatic responses to acquire or lose heat
Temperature sensitive neurons at which locations throughout the body send information to the anterior hypothalamus?
- Bran
- Core body/viscera
- Skin
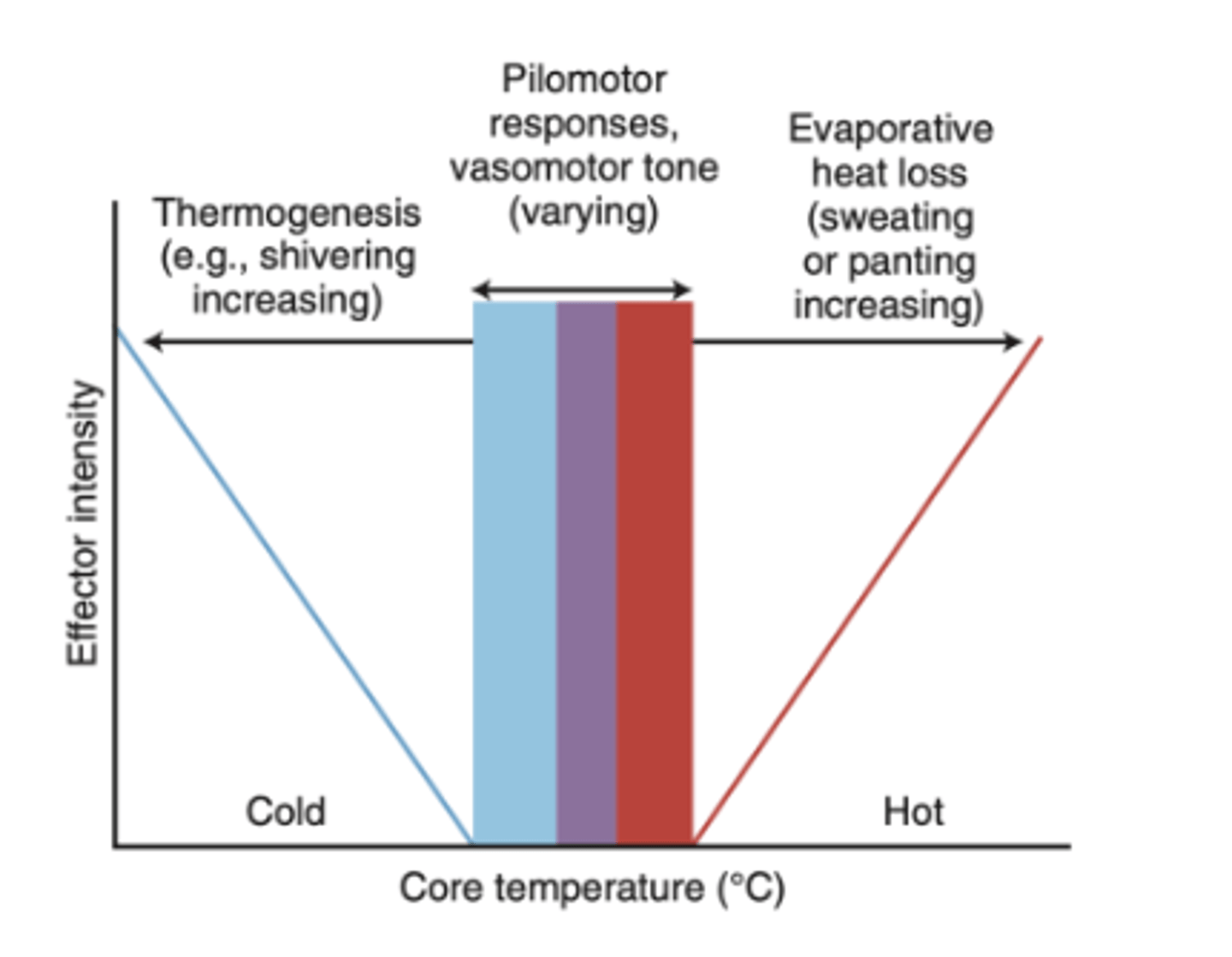
Describe the relationship between intensity of thermoregulatory responses and core body temperature.
- Effector intensity increases as deviation from core temperature increases
What are broad causes of hypothermia?
- Excessive heat loss
- Decreased heat production
- Impaired thermoregulatory functions
What are some causes of "primary" hypothermia?
- "Accidental" hypothermia (I.e., patient left outside too long)
- Exposure to low environmental temperatures with normal heat production
What are some causes of "secondary" hypothermia?
- Sequelae of disease, injury, surgery, drug-induced
- Examples: Hypothyroidism, sepsis, sedation/anesthesia, trauma and hypo-perfusion
What are some signs of hypothermia?
- Low rectal temperature
- Depressed ventilation
- Absence of shivering
- Decreased reflexes
- Depressed cardiac function and decreased intravascular volume -> hypoxia, acidemia and abnormal cardiac rhythm
What is the difference between hyperthermia and fever?
- Fever is increased body temperature associated with a raised (and often variable) thermoregulatory set point in the anterior hypothalamus secondary to the release of pyrogens (e.g., IL-1, TNF-alpha, etc.)
- Hyperthermia is not associated with alterations in the "set point"
What is the difference between hyperthermia and fever in regards to how the animal responds?
- With fever, the cold seeking behavior threshold also varies, which is why you may not feel warm (body is trying to defend the NEW set point)
- With hyperthermia, the animal will make more behavioral and physiological efforts to cool itself
What are the broad categories of causes of hyperthermia?
- Increased heat production (exercise, malignant hyperthermia, prolonged seizures)
- Absorption of environmental heat (heat stroke)
- Impaired heat loss (heat stroke)
- Impaired ability to control core temperature (nervous system disease)
- Combination of factors
How does exercise result in increased heat production and hyperthermia? How can this be managed?
- Elevates core temp. when heat production exceeds heat loss in a manner proportional to exercise intensity and increases core temperature for several hours
- Training will improve thermoregulation
What is malignant hyperthermia?
- Hereditary defect of the ryanodine receptor (calcium conductance channel) affecting horses, pigs, dogs, and humans upon exposure to halogenated anesthetics or muscle relaxants
What animals are at risk of heat stroke?
- Dogs (large breed, obese, brachycephalic)
- Ruminants
- Horses
What are clinical signs of heat stroke?
- Lethargy
- Shock
- Multi-organ dysfunction
How is heat stroke treated?
- Whole body cooling
- Fluid therapy
- Oxygen
Damage to what part of the brain may result in impaired ability to control core temperature, often resulting in an increased temperature?
- Hypothalamus
What are characteristics of nervous system disease affecting the hypothalamus?
- Lack of diurnal variation
- Absence of sweating
- Resistant to anti-pyretics agents
- Excessive response to external cooling
Fever is induced by ______________.
- Pyrogens
Describe how pyrogens induce fever.
- (1) Exogenous pyrogens or immune cells, (2) Activated immune cells, and (3) Endogenous pyrogens (IL-1, IL-6, TNF-alpha, others) in circulation affect the Anterior hypothalamus (prostaglandins, PGE2) which Increases the "set point", stimulating heat conservation and heat production
What are some examples of exogenous pyrogens?
- Infectious agents and their products (Bacterial, fungal, viral, rickettsial, protozoal)
- Immune complexes
- Tissue inflammation or necrosis
- Pharmacologic agents
What are some causes of fever?
- Infection (Bacterial, fungal, viral, rickettsial, protozoal)
- Tissue trauma
- Immune-mediate disease (IMHA, IMTP, IMPA, purpura, systemic lupus eythematous)
- Neoplasia
- Drugs (allergic reaction, immune-mediated, poorly prepared injections with bacterial contamination)
- Toxins
- Metabolic causes
What are the mechanisms by which neoplasia causes fever?
- Secondary infection
- Para-neoplastic syndrome (FUO)
- Administration of blood products
What types of toxins can cause fever?
- Heavy metals, chlorinate hydrocarbons, bracken fern, mycotoxins, blister beetle
- Note: Other clinical signs will predominate in these instances
What are some metabolic causes of fever?
- Hyperthyroidism
- Eclampsia (mares and humans)
- HYPP
What is an FUO?
- Febrile episodes of >3 weeks with no diagnosis after a week of routine diagnostics
What are some diagnostic aids for FUOs?
- BW (CBC/Chemistry/UA/fibrinogen/globulins)
- Body cavity examinations (imaging, centesis, fluid analysis)
- Infectious disease testing
- Blood culture
What are some specific considerations to keep in mind when collecting a sample for blood culture?
- D/C antibiotics for 48-72 hours prior to sampling
- 3-5 samples at least 45 minutes apart, placed directly into culture media
- Sample just before and during fever if possible