Immune System
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Introduction to the immune system
body is constantly exposed to a vary of pathogens
Body needs to have mechanisms to protect itself form pathogens that may cause infections
some of these mechanisms are non-specific
some are specific for certain pathogens
has a mechanism to remember specific pathogens for a faster and more effective response during later infections
Innate Immunity
The primary protective mechanism for the body. It includes two key aspects: first line of defence (skin and mucous membranes) and second line of defence (internal defences)
Key features: it is fast - able to provide rapid initial response but it is non-specific.
refers to wide variety of body responses that serve to protect against invasion of a wide variety of pathogens and toxins.
We are born with this immunity. 1st line of defence (skin and mucous membranes) 2nd line of defence (internal defences)
Epidermis of skin
Forms physical barriers to entrance of microbes
Keeps pathogens on the outside of the body or neutralises them before infection begins.
Skin: the epidermis - closely packed outer epithelial layer of the skin, key physical barrier against the entry of microbes as intact skin is very difficult to penetrate. Damage leads to risk of infection.
Mucous membranes
inhibit entrance of many microbes, but not as effective as intact skin
Keeps pathogens on the outside of the body or neutralises them before infection begins.
Mucous membranes: line the surface of GI tract and respiratory tract and genitourinary tract, slightly less effective than physical barrier.
Mucous
traps microbes in respiratory and gastrointestinal tracts.
Hairs
Filter out microbes and dust in nose/ from the nasal passage
Cilia
together with mucous, trap and remove microbes and dust from upper respiratory tract
Lacrimal apparatus
tears dilute and wash away irritating substances and microbes
tears wash microbes and particles from the eyes
Saliva
washes microbes from surfaces of teeth and mucouse membranes of mouth
Urine and perspiration
urine: Washes microbes from urethra
perspiration: washes microbes from the skin
Defecation and vomiting
Expels microbes from body
Chemical factors of first line of defence
Sebum - forms protective acidic film over skin surface that inhibits growth of many microbes
Lysozyme - antimicrobial substance in perspiration, tears, saliva, nasal secretions and tissue fluids. enzyme which breaks down cell wall of some bacteria.
Gastric juice - destroys bacteria and most toxins in stomach
vaginal secretions - slight acidity discourages bacterial growth,, flushes microbes out of vagina.
Second line of defence - antimicrobial substances
Interferons (IFNs) - secreted by certain virus-infected cells, lymphocytes and macrophages. protect uninfected host cells from viral infection. Interfere with viral replication in neighbouring cells.
Complement system - causes cytolysis of microbes; promotes phagocytosis; contributes to inflammation
iron-binding proteins - inhibit growth of certain bacteria by reducing amount of available iron
Antimicrobial proteins (AMPs) - have broad-spectrum antimicrobial activities and attract dendritic cells and mast cells. Short peptides that can kill a wide range of microbes
Natural killer cells (NK)
Kill infected target cells by releasing granules that contain perforin and granzymes; phagocytes then kill released microbes
Are specific type of white blood cell (leukocyte)
kill a wide variety of infected body cells and some tumour cells
Phagocytes
ingest foreign particulate matter
various types of white blood cells can act as phagocytes
mainly neutrophils and macrophages
neutrophils early in infection and macrophages dominate later in infection
‘Phago’ (eat) and ‘cyto’ (cell)
Migrate to the infected area and are involved in clearing debris of denatured proteins, dead body cells and microorganisms.
Inflammation
Confines and destroys microbes; initiates tissue repair
A non-specific defensive response to tissue injury
limits the effects on the body by confining or walling off the area
involves the release of chemical by stressed or damaged cells (phagocytes are then attracted to the area via chemotaxis). vasodilation and increased permeability of blood vessles, movement of phagocytes from the blood to the interstitial fluid and tissue repair.
conditions involving inflammation are given the suffix -itis
PRISH (pain, redness, immobility, swelling and heat)
Fever
Intensifies effects of interferons; inhibits growth of some microbes; speeds up body reaction that aid repair.
a systemic response to tissue damage
the hypothalamus (body’s thermostat) is usually set at 37C
during fever the hypothalamus is “reset: to a higher temperature which is thought to intensify the effect of anti-viral substances and increase the production of iron-binding proteins which reduces the availability of iron for bacterial growth
if body temperature rises too much, deaths results (44-46C)
Adaptive immunity
Is induced when innate immunity cannot control the situation.
It is also know as third line of defence and has two key components:
antibody-mediated immunity (also known as humoral immunity) which involves B cells (also known as B lymphocytes).
Cell-mediated immunity (also known as cellular immunity) which involves T cells (also known as T lymphocytes)
slower, more specific to type of pathogen and has memory component
Key features of adaptive immunity
specific recognition of foreign molecules known as antigens (antibody generator molecules)
includes a memory component that allows for faster and more effective response to the same pathogen in the future.
Third Line of Defence
B and T cells are the key cell types involved in adaptive immunity. We don’t need to fully understand the complex mechanism shown in the figure below, but there are some key important points we need to understand
Key important points:
B and T cells arise from stem cells in the bone marrow
B cells mature in the bone marrow whereas T cells mature in the thymus
B cells are activated to produce specific antibodies in response to recognition of antigens on the surface of pathogens
T cells are activated in response to recognition of pathogen antigens presented on the surface of antigen presenting cells
Activated B and T cells produce memory cells which enable faster and more effective responses to subsequent exposure to the same antigen in the future.
The immune system is highly….
Interconnected
interactive
cooperative
as a whole can produce a more protective response than any individual component on its own
complex!
First line of defence
keeps pathogens on the outside or neutralises them before infection begins. The skin, mucous membranes and certain antimicrobial substances are part of these defences.
Second line of defence
slows and contains infections when first-line of defence fails. They influence proteins that produce inflammation, fever and enhance cytokine activity, and phagocytes and NK cells, which attack and destroy cancer cells
Third Line of defence
includes lymphocytes and target specific pathogens for destruction when the second line of defence fails or don’t contain infections. It includes memory components that allow the body to be more effective when responding to the same pathogen in the future. (also known as adaptive immunity)
Skin and mucous membranes
the skin and mucous membranes are in contact with our environment, thus they are critical in protecting us from pathogens and foreign substances entering our bodies.
They provide protection in two key ways: mechanical (physical barriers where physical processes remove microbes from the body’s surfaces) and chemical protection where substances are produced.
Normal microbiome and innate immunity
Although not considered part of the innate immune response, your normal flora (microbiome) can also play a protective role.
can compete with potentially pathogenic microorganisms by competing for available nutrients and space.
some bacteria of the normal flora produces substances that can inhibit the growth or kill other microorganisms.
Has an impact on the development of the immune system starting from before birth
Innate immunity - 2nd line of defence - internal defences
antimicrobial substances
defensive cells
inflammation
fever
Defensive cells
are principally white blood cells
there are different types of white blood cells which have different roles in the innate and or adaptive immune response
are involved in defence against different types of infections (bacteria, viruses and parasites).
Two difference of adaptive immunity to innate immunity
Specificity for a particular foreign molecule: antibody generator molecules → antigens
Memory as a result of previously encountered antigens
Third line of defence is designed to distinguish between “self” and “non-self”
Antigen = the invader, foreign molecules
antibody = the defender, produced by B cells, specific for different antigens
Easy trick to remember": A before B → antigen before antibody. Antigen enters first (trigger) and antibody comes after (response)
epitopes = specific regions of the antigen that is recognised by antibodies
Humoral and cellular
Humoral (antibody-mediated) immunity
involves B cells which produce antibodies (immunoglobulins, Ig) and defends against extracellular threats (type of white blood cell - B lymphocytes) which are primarily found in the blood and lymphoid organs. Antibodies recognise foreign molecules known as antigens.
Cellular (cell-mediated) immunity
involves T cells, defends against intracellular threats and induces other cells to perform a function
Humoral immunity continued/antibody-antigen interactions
B cells are initially coated on the surface with antibodies corresponding to a specific antigen
once activated B cells secrete the same specific antibody
targets extracellular pathogens: extracellular bacteria and viruses before they enter cells (virons or viral particles)
There are millions of B cells, all with different antibodies on their surfaces, once they encounter an antigen thats a match they clone themselves. Both memory B cells and plasma cells are produced and plasma cells produce large amounts of identical antibodies.
Antibodies can inactivate antigens by binding to them and interfering with their usual functions which enhances phagocytosis
Antibody-antigen interactions
Antibodies inactivate antigens, bind to them to interfere with usual functions.
Inactivation can occur by neutralisation, agglutination or precipitation. This enhances phagocytosis
The binding to antigens can activate the complement system leading to: cell lysis and the enhancement of phagocytosis and inflammation.
Immunological memory
Subsequent antibody responses to the same antigen are: faster and stronger
Cell mediated immunity/cellular immunity
involves T cells (T lymphocytes)
mature in the thymus
Mature T cells are found in the blood and lymphoid organs
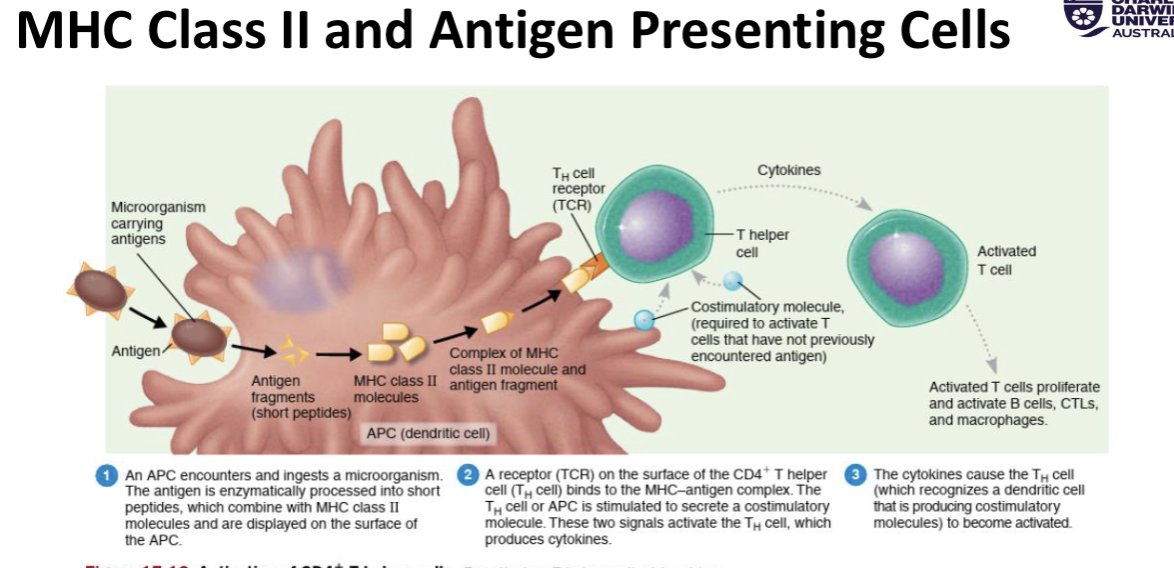
T cells recognise antigenic peptides presented to them by antigen presenting cells
Like B cells, T cells are also specific for a single antigen
Self-recognition and self-tolerance
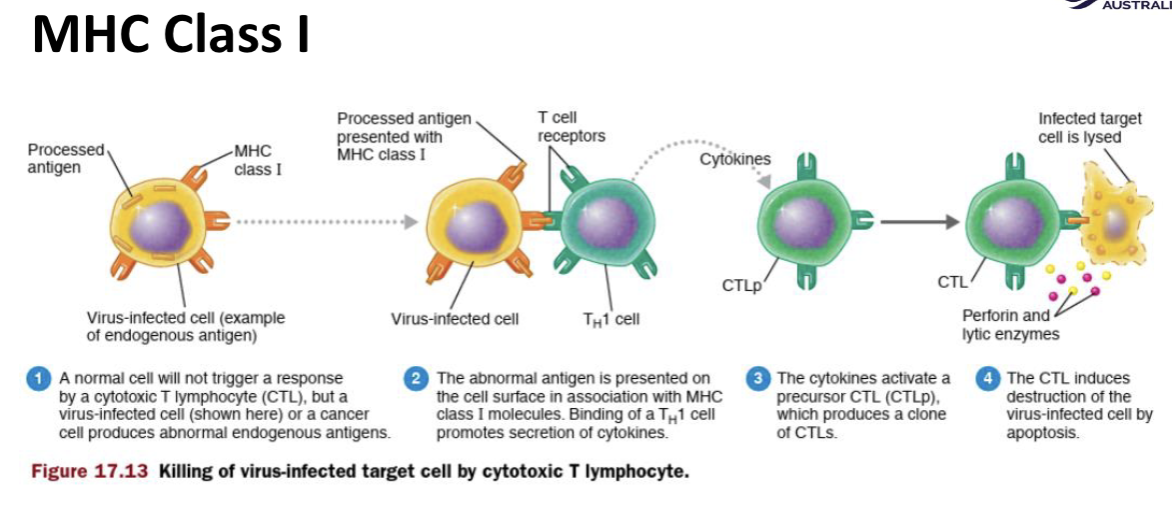
Major histocompatibility complex (MHC) molecules.
molecules on the surface of body cells to help the immune system recognise them as “self”
Two difference classes of MHC molecules:
MHC class l = present on all nucleated body cells
MHC class ll = used by antigen presenting cells to present antigens on their surfaces
MHC class l picture
MHC class ll picture
Types of adaptive immunity
Naturally acquired:
Active = antigens enter the body naturally; body induces antibodies and specialised lymphocytes
Passive = antibodies pass from mother to fetus via placenta or to infant via milk
Artificially acquired:
Active = antigens are introduced in vaccines; body produces antibodies and specialised lymphocytes
Passive = performed antibodies in immune serum are introduced by injection