Endocrine: Part 4: Calcium
1/26
Earn XP
Description and Tags
Write the correct answer for each question.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
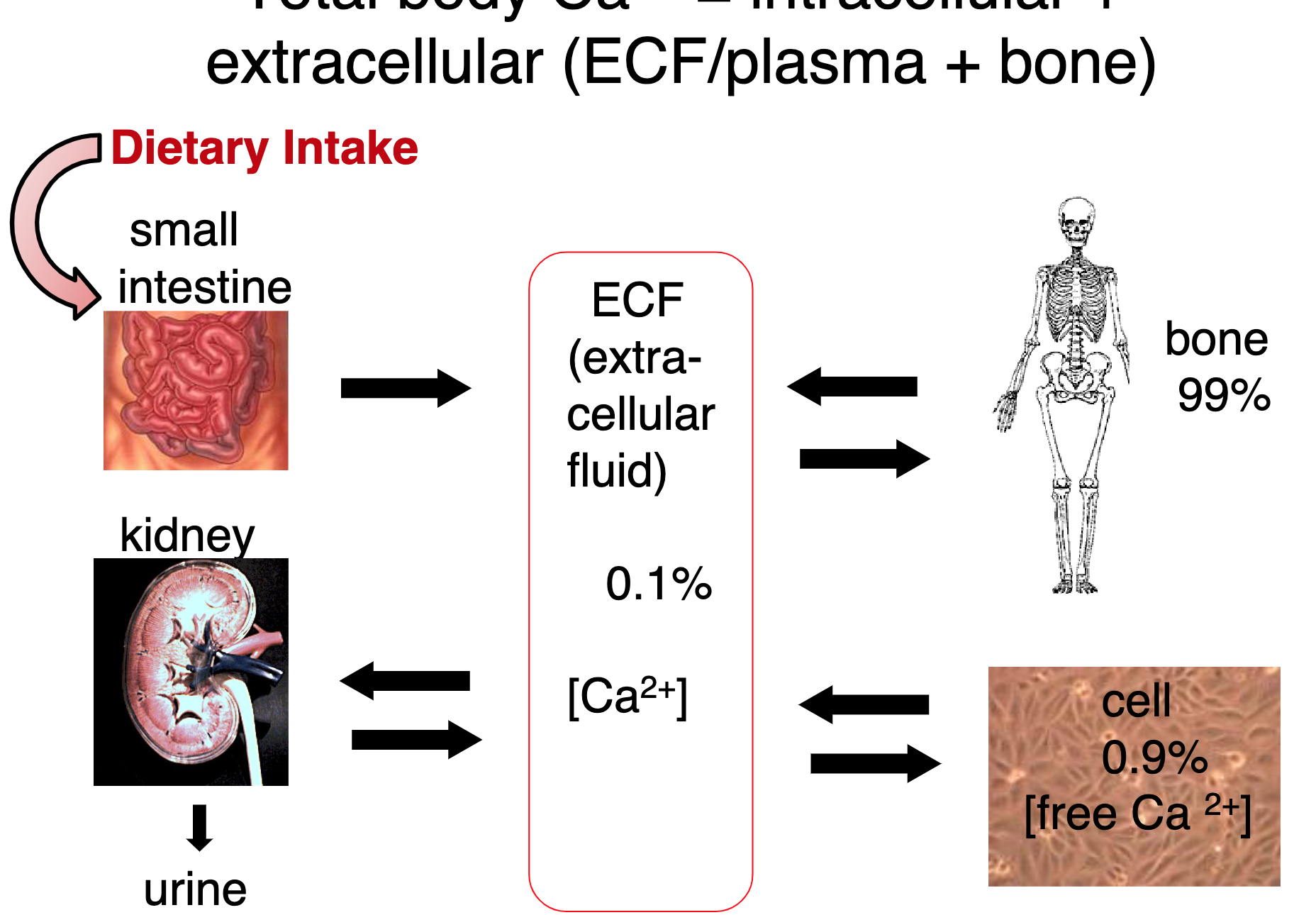
Where is calcium located?
Extracellular matrix, extracellular fluid, and intracellular Ca2+.
What are osteoblasts?
They are bone-forming cells. They build bones until they are trapped in the bone matrix as osteocytes.
What are osteoclasts?
They are bone-resorbing cells that break down bone tissue, releasing minerals into the bloodstream.
What are osteocytes?
Mature bone cells that maintain the bone matrix.
Which bone cells are responsible for bone growth/turnover?
Osteoblasts are responsible for bone growth and turnover by building new bone tissue.
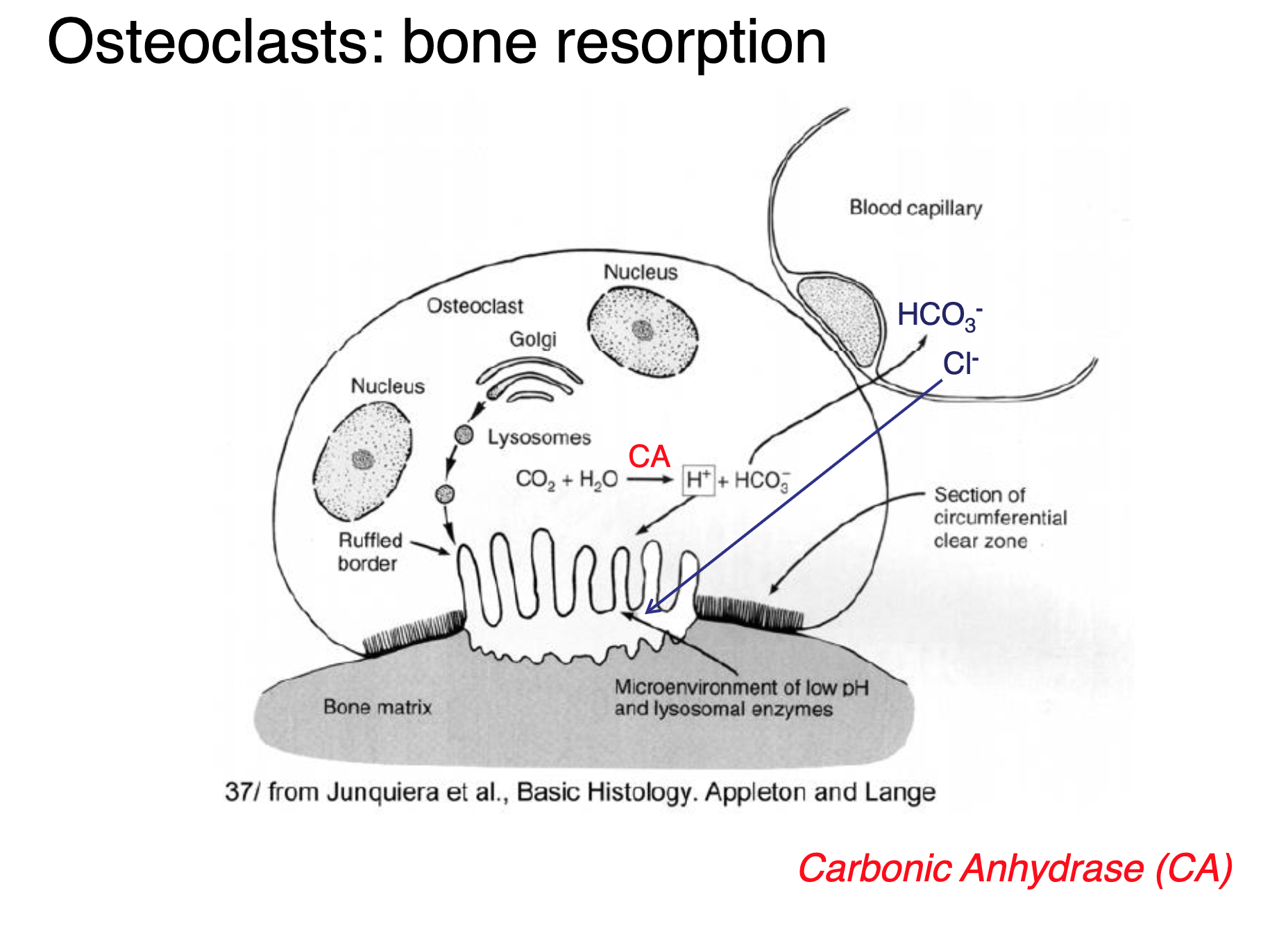
Explain how HCL and proteases dissolve the matrix.
Secreted by osteoclasts, HCl and proteases work together to break down the mineral components and organic matrix of the bone at a low pH.
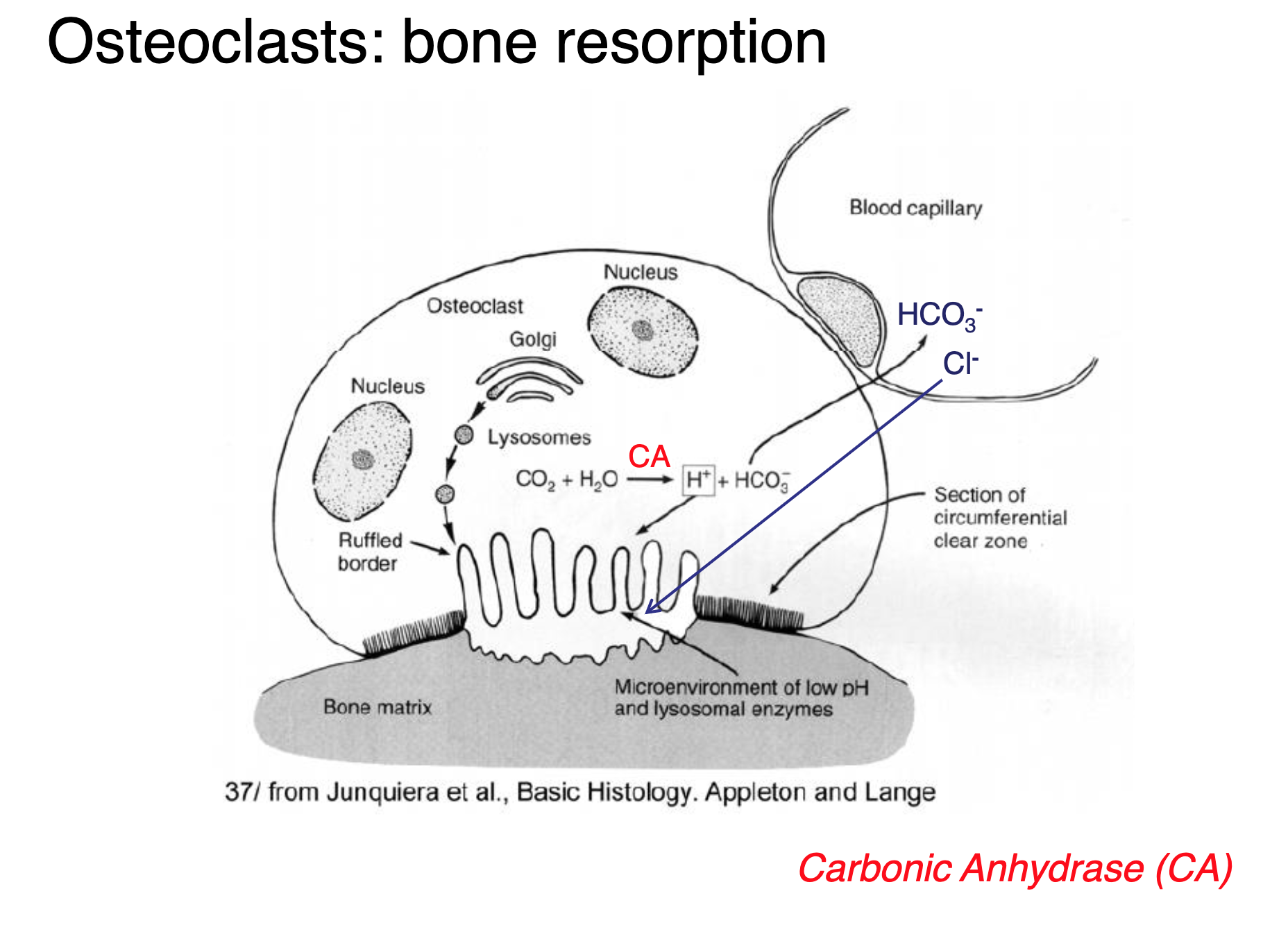
Explain how calcium is released from the bone matrix.
Ca2+ pool gets released into the bloodstream when osteoclasts break down the bone material, releasing calcium ions and facilitating calcium homeostasis in the body.
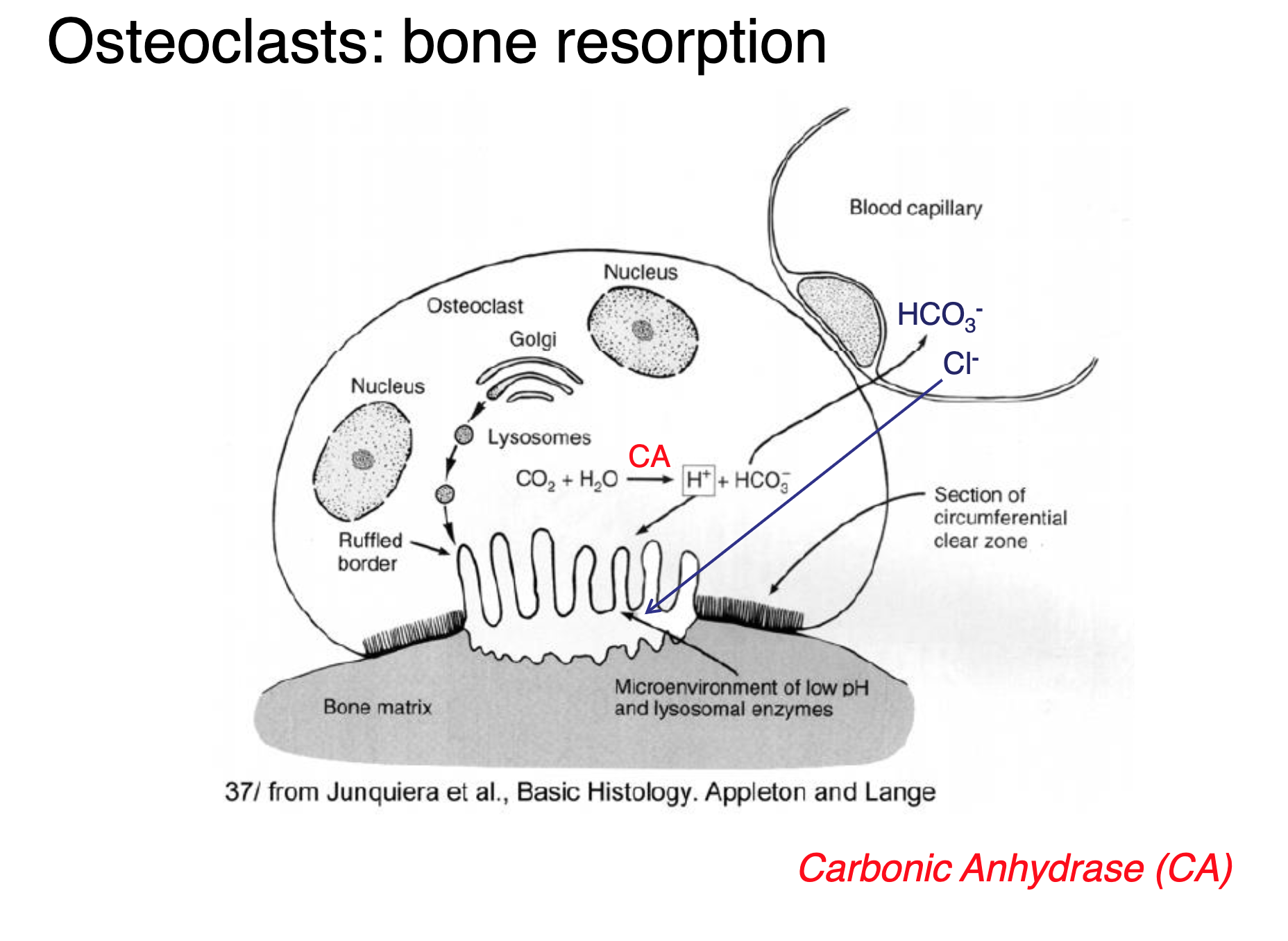
Explain what carbonic anhydrase does based on the equation.
CA is a special enzyme that releases bicarbonate ions and free protons (H+) from carbonic acid, so that they form HCl, facilitating the regulation of pH and the transport of carbon dioxide in the body.
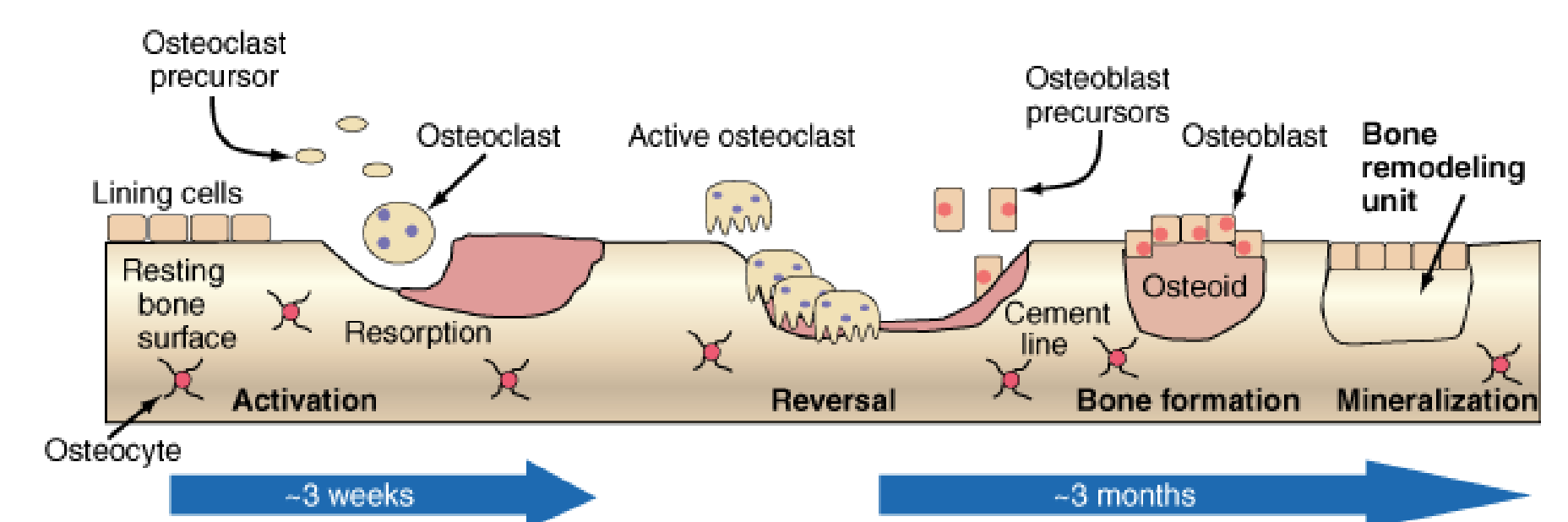
Explain what is happening in this photo.
Osteoclasts break down and resorb the bone, smoothing it out in the process. Osteoblast rebuilds the hole, and the bone remodelling unit neatly corrects the formation of the bone structure.
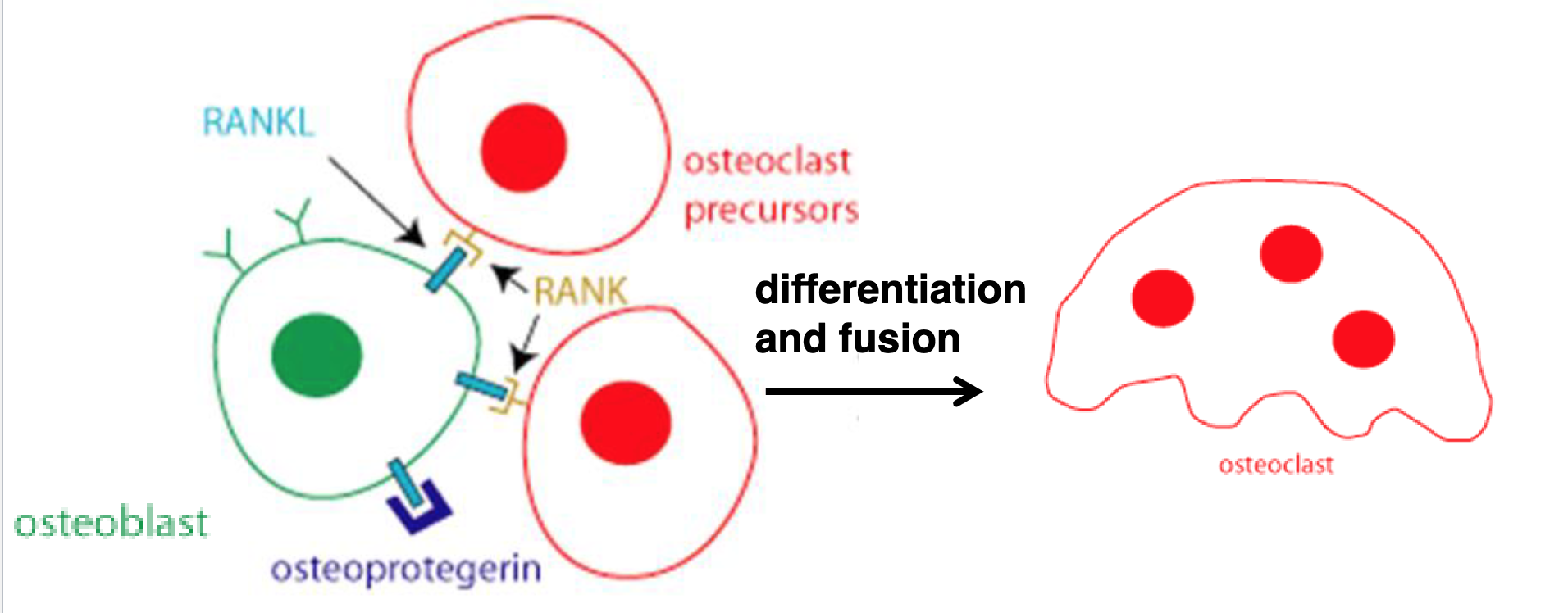
Could you describe the osteoclasts that build up from this image?
The osteoclasts’ receptors bind to the RANKL to be activated. The many osteoclast cells fuse to resorb bone.
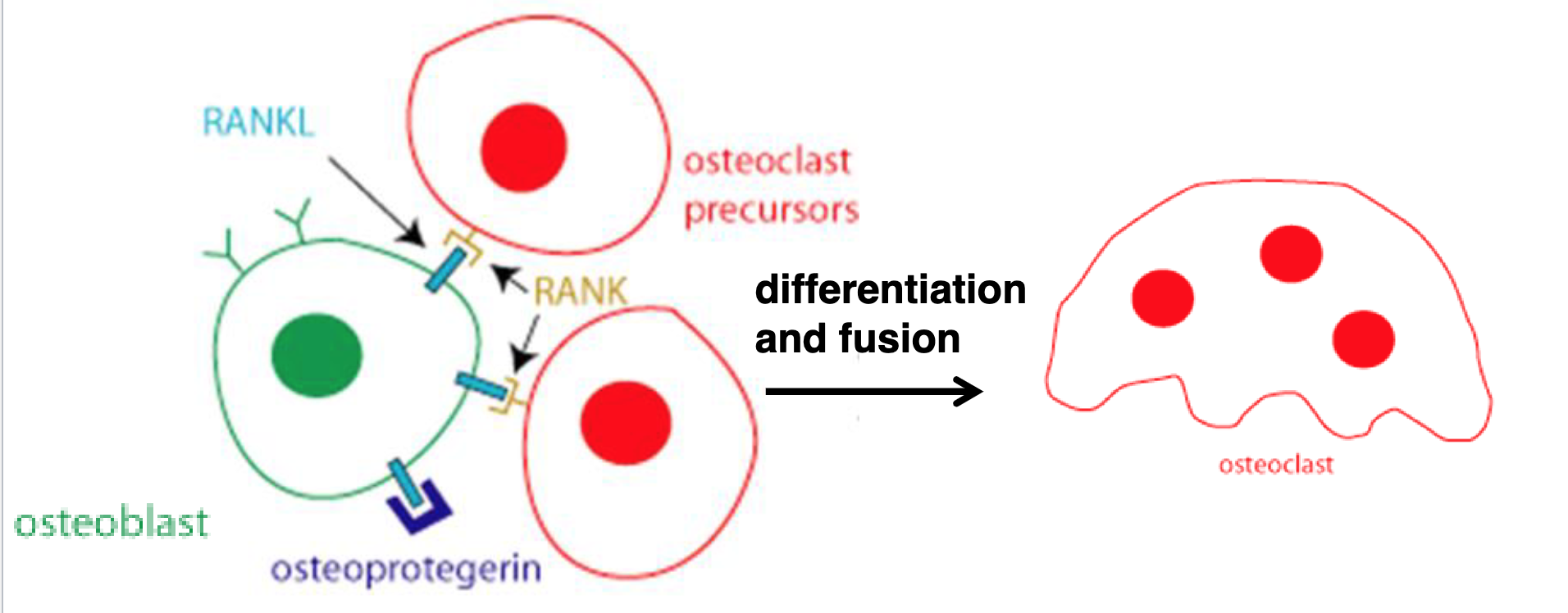
Describe how the osteoblasts inhibit the buildup of osteoclasts.
Osteoblasts secrete OPG. OPG blocks the RANKL binding site to prohibit osteoclasts from building up.
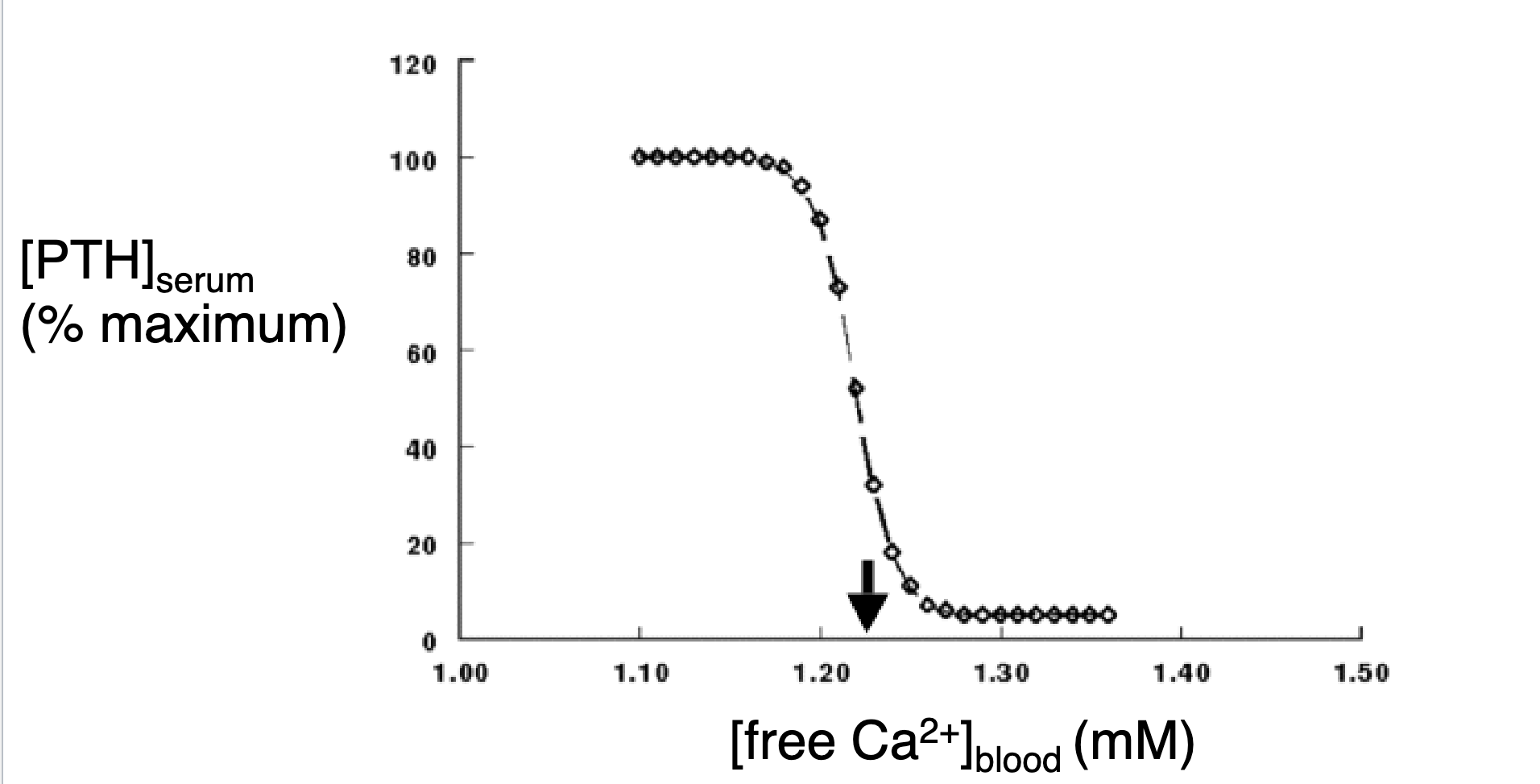
Explain how the parathyroid hormones act on low plasmic Ca2+.
Parathyroid hormones jump in very high amounts to increase free Ca2+. Parathyroid hormones are sensitive to less than normal release in Ca2+.
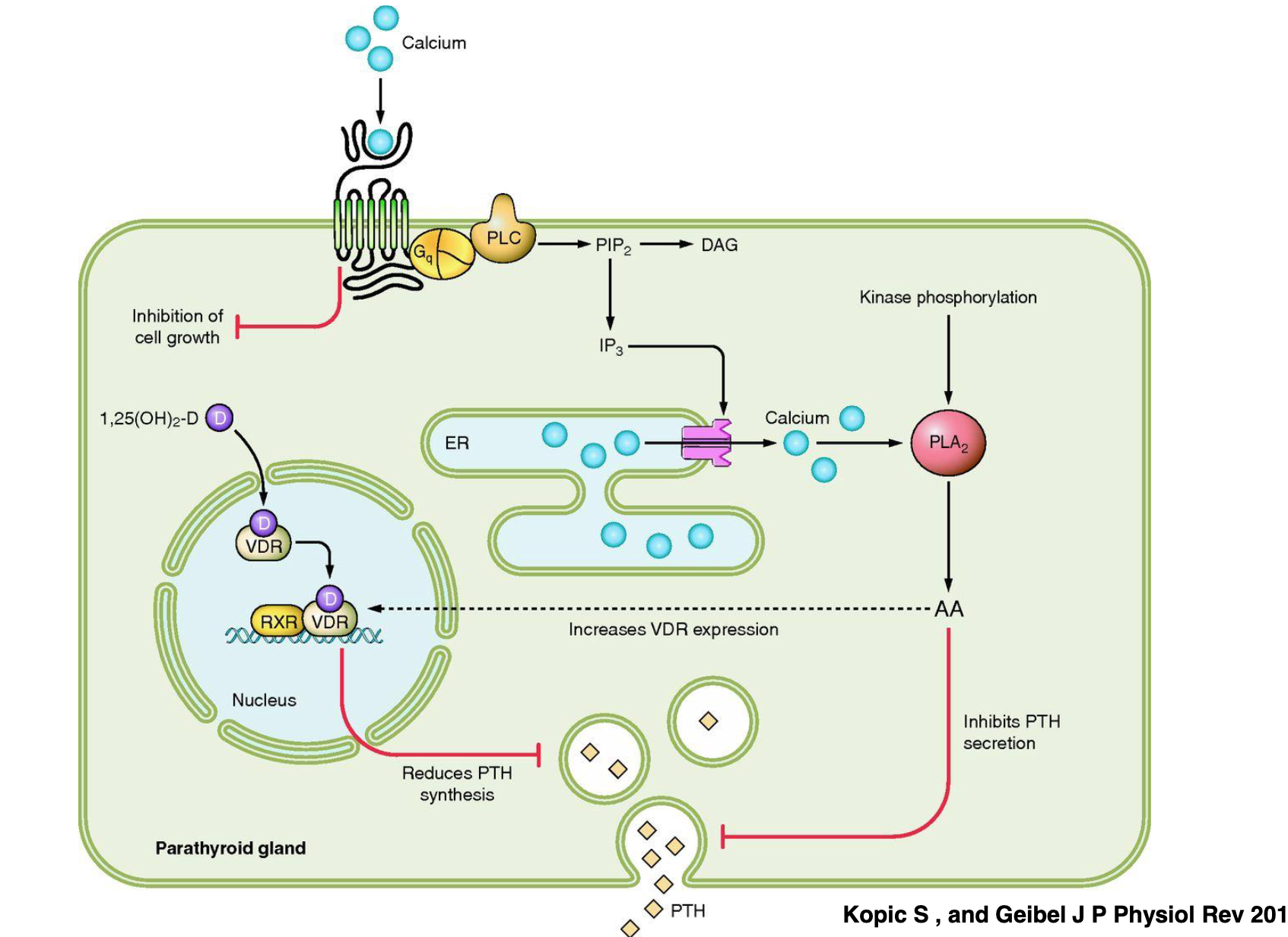
Explain the Ca2+-sensing receptor on the plasma membrane used to monitor extracellular Ca2+.
Ca2+ binds to the receptor→cell growth is inhibited, but the ligand signals G-alpha-q to bind to PLC→PLC activates PIP2, which generates IP3 →IP3 secretes calcium ions from the ER to activate kinase phosphorylation→both form PLA2, which inhibits PTH secretion. Vitamin D3 binds to VDR to reduce PTH synthesis. When there is no Ca2+ or vitamin D3 present, PTH is released, until the rise of calcium levels goes up again.
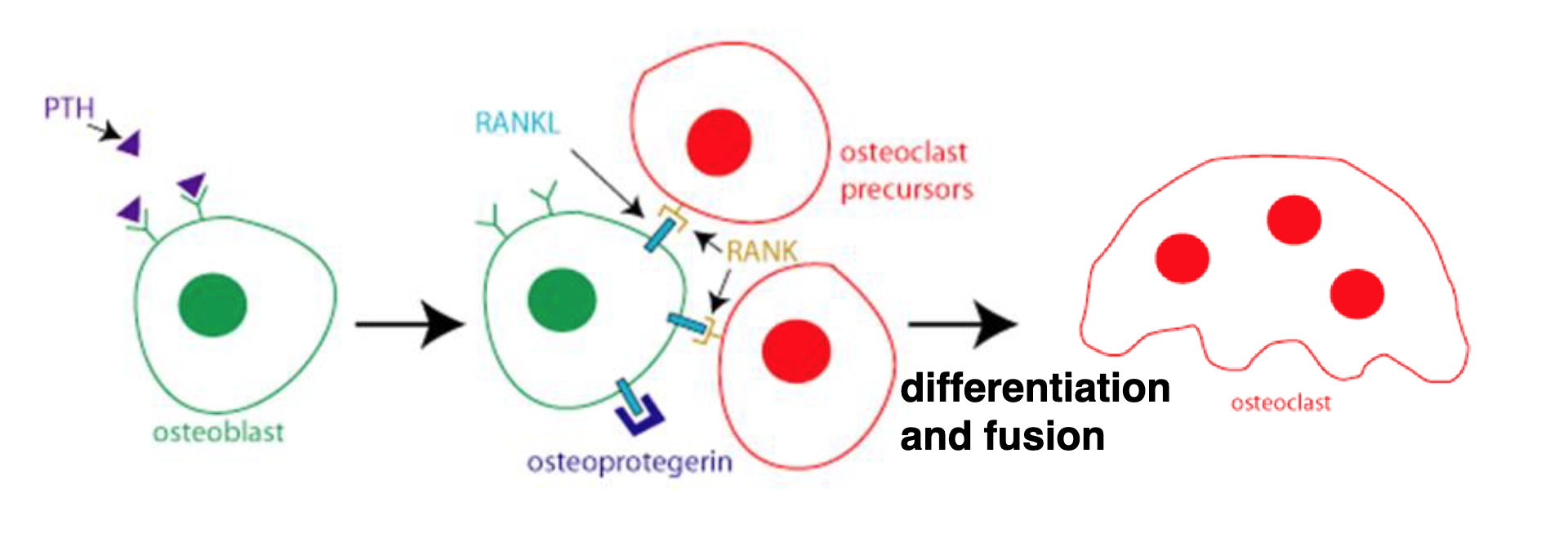
Explain the PTH effects on the bone.
PTH acts on the osteoblasts by increasing cAMP to increase RANKL and decrease OPG expression. More osteoclasts are formed leading to bone resorption.
What are the organs crucial in the production of calcitriol?
Skin, liver, and kidneys.
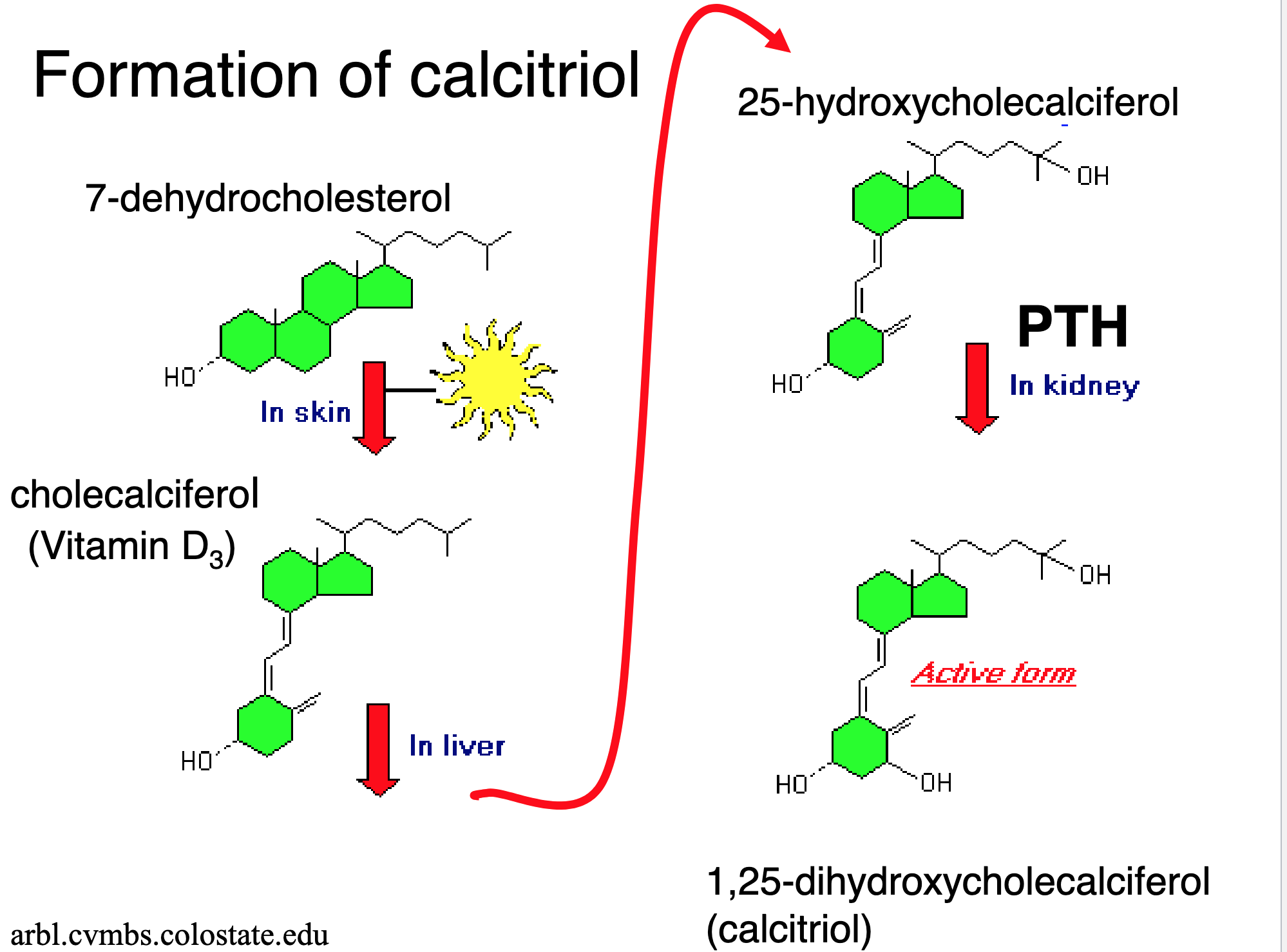
Explain the formation of Calcitriol.
7-DHC is derived from precursors of our skin→UV light absorbed in our skin changes 7-DHC into vitamin D3→in the liver, it changes vitamin D3 into 25-HCC→in the kidneys, by the PTH, 25-HCC is converted into calcitriol.
How does calcitriol act?
The vitamin D3 hormone helps absorb Ca2+ into the small intestine and the kidneys.
Explain the production of calcitriol.
Production is regulated in the kidneys by the PTH. Decreased plasma Ca2+ increase PTH secretion, which stimulates calcitrol synthesis. Intestinal and renal reabsorption of Ca2+ raises blood Ca2+. Turning off PTH in a negative feedback loop decreases calcitrol synthesis.
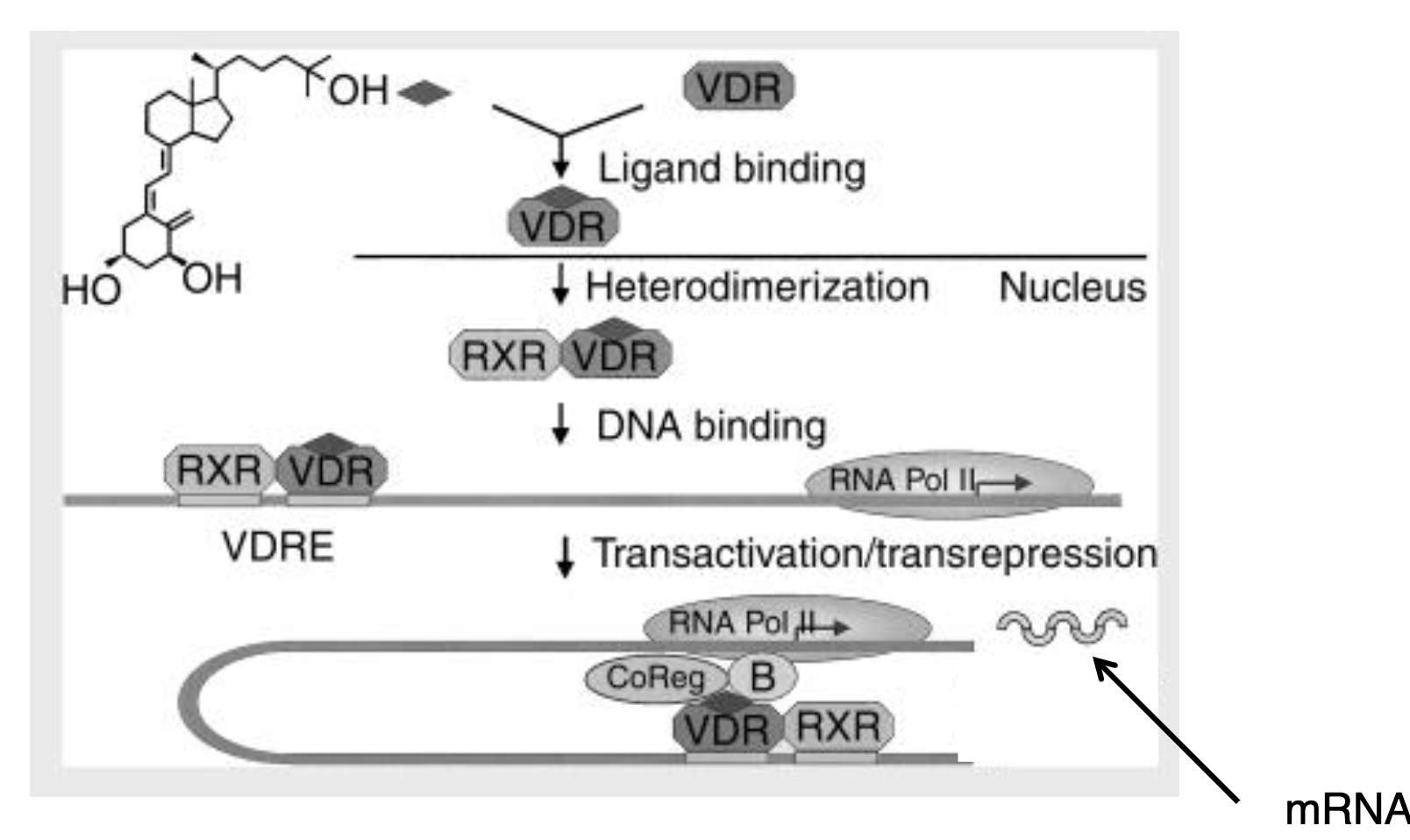
Explain what is happening in this image.
Calcitriol binds to VDR→VDR forms heterodimers with RXR→ the heterodimer tries to find VDRE to bind to DNA→the VDR binds to other basal transcription factors to increase expression→it transfers the mRNA to the intestines and kidneys to help with absorption.
How is blood phosphate controlled by the PTH?
It increases phosphate release from the bone. It decreases phosphate reabsorption in the kidneys. The combined concentration of Ca2+ and PO43- needs to be below a certain level. High concentrations of Ca2+ and PO43- in urine would result in kidney stones.
How is blood phosphate controlled by the calcitriol?
Calcitriol increases phosphate reabsorption in the kidneys and enhances intestinal absorption. This helps maintain optimal blood phosphate levels.
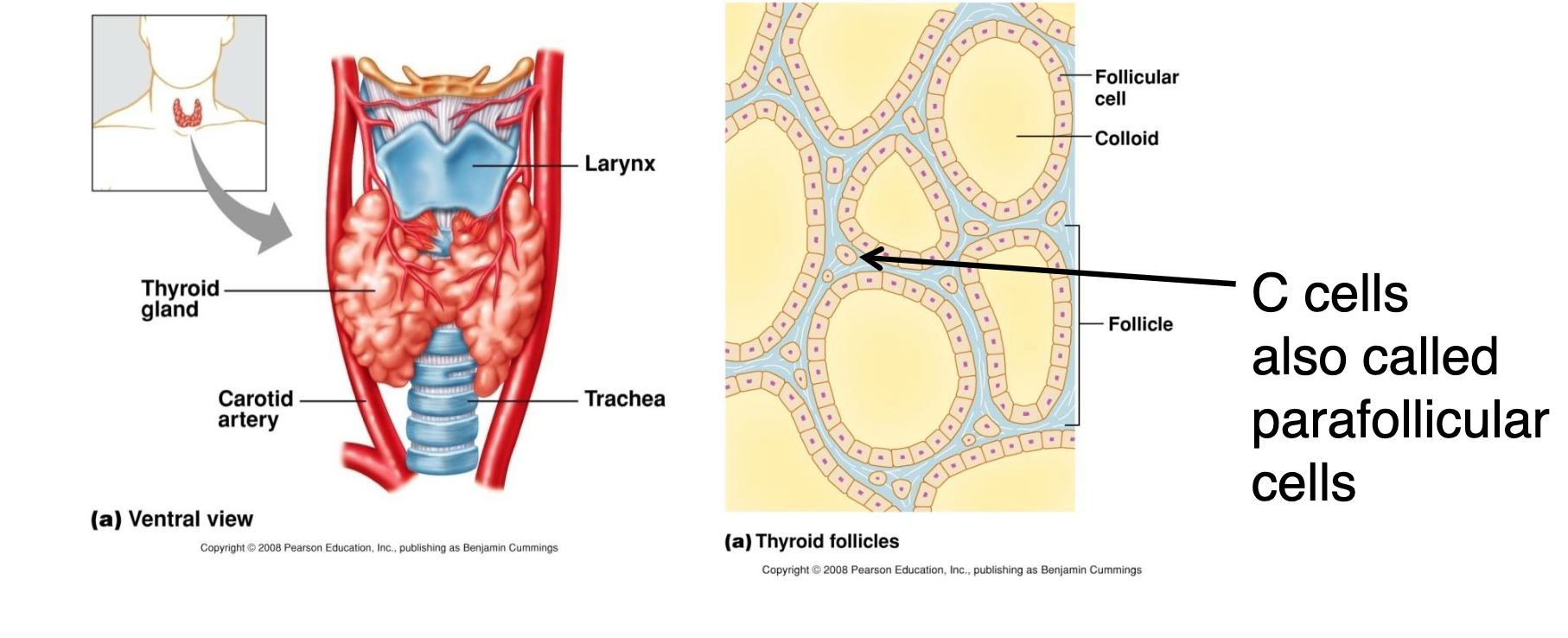
What is calcitonin?
Calcitonin is a peptide hormone that is produced by C cells from the thyroid gland.
When is calcitonin released?
Calcitonin is released when there are high amounts of plasma [Ca2+ ].
What is the action of calcitonin?
Calcitonin decreases bone resorption and increases renal calcium excretion. It protects the skeleton from calcium loss during pregnancy and lactation.
List the symptoms of hypercalcemia.
Constipation, fatigue, depression, bone pain, and kidney stones.
List the symptoms of hypoglycemia.
CATS→ Convulsions, arrhythmias, tetany, spasms, seizures, and stridor. People can die from these.