Chapter 17: Physiology of the Kidneys
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
Renal (Next 2)
1. Renal: Pertaining to the kidneys
2. Main function of system is regulation of extracellular fluid (ECF) environment in the human body through urine formation
The Renal System
1. Regulates blood volume
2. Eliminates organic waste products of metabolism (protein breakdown), uric acid (nucleic acids), creatinine (muscle creatine), end products of hemoglobin breakdown
3. Regulates balance of electrolytes (Na, K, HCO3, other ions)
4. With respiratory system, maintains acid-base balance/pH of plasma
Structures of the Renal System (Next 4)
1. Kidneys
2. Ureters
3. Urinary Bladder
4. Urethra
Kidneys (2)
- Formation of urine
- Water and electrolyte balance
- Secretion of toxins and drugs into urine
- Gluconeogenesis: Synthesis of glucose from AAs during prolonged fasting (also occurs in liver)
Ureters (2)
- Transfer to urine to bladder
Urinary Bladder
- Storage and micturition (urination) via the urethra
Urethra
Flow of urine from bladder to outside (micturition)
Female Renal System
1. The paired kidneys form a filtrate of the blood that is modified by reabsorption and secretion
2. Urine destined for excretion moves from the kidneys along the ureters to the bladder
3. Is is then excreted through the urethra
Kidney: Cross Section (Next 2)
1. Outer Layer
2. Inner Layer
Cross Section (Outer Layer)
- Outer layer of kidney is the renal cortex; it is the site of glomerular filtration as well as the convoluted tubules
Cross Section (Inner Layer)
Inner layer of the kidney is the renal medulla; this is the location of the longer loops of Henle, and the drainage of the collecting ducts into the renal pelvis and ureter
Micturition
1. Contractions of smooth muscle in ureter wall cause urine to move from ureter to bladder
2. Bladder walls are smooth muscle (detrusor muscle)
- Contraction of detrusor produces micturition
3. Internal urethral sphincter (smooth muscle) is at the base of bladder
4. External urethral sphincter (skeletal muscle) is below this and surrounds the urethra, its contraction can prevent urination
5. Contraction and relaxation of these muscles is determined by:
- Neuronal input, due to stretching of the bladder when it fills
- Voluntary decision making
Blood Vessels of the Kidney
1. Blood enters the kidney via the renal artery and exits via the renal vein
2. In the kidney there is extensive branching and capillary networking including the glomeruli
The Nephron (Next 5)
1. The functional unit of the kidneys, consisting of a renal corpuscle (glomerular capsule + glomerulus) and tubule
- Branching of renal artery --> afferent arterioles, which bring blood to the glomeruli (a glomerulus is a capillary networking in renal corpuscle)
2. Blood from renal artery --> Afferent arterioles --> Glomeruli
The Nephron (Blood + Plasma Movement)
☆Plasma:
1. Blood from renal artery --> 2. afferent arterioles --> 3. Glomerulus --> 4. 20% plasma filtrate from glomerulus --> 5. Glomerular capsule --> 6. Tubule --> 7. Collecting duct --> 8. Renal pelvis --> 9. Ureters
☆Blood:
1. 80% of blood in glomerulus --> 2. Efferent arterioles--> 3. Peritubular capillaries --> 4. Renal vein
The Nephron (Bowman's + Proximal + Collecting Duct) (Next 3 Slides)
☆Glomerular capsule or Bowman's capsule:
- Surrounds glomerulus
- Fluid filters out of glomerulus into capsule
Proximal Convoluted Tubule
☆ Proximal Convoluted Tubule:
- Filtrate from glomerulus enters lumen of tubule
- Reabsorption of salt, water, etc. into peritubular capillaries that surround tubule
- Secretion of substances into filtrate
Collecting Duct
☆ Collecting Duct:
- Distal convoluted tubule empties into it
- Duct drains into renal pelvis and then into ureters
Glomerular Filtration
1. Filters through large pores in glomerular capillaries called fenestrae
2. Filtrate (or ultrafiltrate) is cell-free and mostly protein-free; otherwise similar to plasma
Reabsorption of Salt & Water
1. Glomerular filtrate is around 180 L each day, but urine excretion is only around 1-2 L per day
- 1% of this filtrate is excreted as urine and 99% of filtrate returns to vascular system (reabsorbed) to maintain blood volume
- Reabsorption: return of filtrate from tubules to peritubular capillaries, via osmosis
2. Urine volume varies depending on fluid needs of body (e.g. to maintain blood volume and pressure), so volume of fluid reabsorbed varies
3. Most salt and water in filtrate are reabsorbed in proximal tubule, some reabsorbed in descending limp of the loop of Henle
Filtration & Reabsorption
1. Filtration refers to the movement of fluid and solutes from glomerulus into the capsule and then into the tubules
2. Reabsorption refers to the movement of material from the tubules into the peritubular capillaries, i.e. back into general circulation
Reabsorption of Salt & Water in Proximal Tubule
☆ Sodium is actively transported out of filtrate and Chlorine follows passively by electrical attraction
- Due to osmosis, water follows the salt into the peritubular capillaries
Countercurrent Multiplier System (Next 3)
☆ For water to be reabsorbed into bloodstream by osmosis, ISF surrounding tubule must be hypertonic (causing water to move out of tubule)
- Fluid is hypertonic due to Countercurrent Multiplier System
- Countercurrent flow (opposite direction of flow) in ascending and descending limbs in nephrons and close proximity of limbs allow them to interact to create high osmotic pressure in ISF
Countercurrent Multiplier System (Ascending Loop)
☆ In ascending limb of the loop of Henle:
- Sodium is actively pumped into ISF
- Chlorine follows sodium because of electrical attraction
- Not permeable to water so fluid in ascending limb becomes diluted
- Sodium Chloride accumulates in the ISF here, increasing the osmolarity of ISF so that reabsorption occurs in the descending limb
Countercurrent Multiplier System (Descending Loop)
☆ In descending limb of the loop of Henle:
- Permeable to water but not salt
- ISF is hypertonic compared to filtrate here, so water leaves descending limb by osmosis --> ISF --> capillaries
- Hypertonic fluid then enters the ascending limb, where sodium is actively pumped out and chlorine follows, creating diluted tubular fluid and more concentrated ISF
Countercurrent Multiplier System Summary
1. Extrusion of Sodium Chloride from ascending limb makes ISF more concentrated here, Sodium is pumped out and Chlorine follows due to electrical attraction
2. In descending limb, water diffuses out via osmosis (and enters capillaries), this increases osmolarity of tubular fluid and decreases its volume as the fluid descends
3. Fluid at the bend of the loop has a high osmolarity, 1,200 mOsm, the "saltiness" of the ISF is "multiplied" here because of the lack of the permeability to water
Role of Osmoreceptors in ADH Secretion
1. Changes in water intake alter plasma osmolarity, which is sensed by hypothalamic osmoreceptors
2. Secretion of ADH is altered to affect water reabsorption in the kidneys, this affects the volume of urine excreted, to maintain blood volume
Renal Plasma Clearance
☆ Volume of plasma that is "cleared" of substance by kidneys per unit time (i.e. substance removed from plasma)
- Substances are removed from plasma via filtration from glomerulus, or secretion into filtrate
☆ Secretion is the movement of substances from the peritubular capillaries into the tubular fluid, for excretion in the urine
- Reabsorption of a substance reduces its clearance
Renal Plasma Clearance Pt. 2
☆ Filtered glucose and AAs are completely reabsorbed in proximal tubule via active transport
- When the concentration of glucose exceeds the capacity of the transporters, i.e. the transport maximum, the excess glucose is excreted in the urine = glucosuria
- Occurs when plasma glucose concentration is too high, 180-200 mg/dl in diabetes mellitus
Glucosuria
☆ When excess glucose (transport maximum) is excreted in the urine
Renal Control of Sodium/Potassium Balance
☆ Much of the filtered Sodium and Potassium is reabsorbed in early part of nephron
☆ Concentrations of Sodium and Potassium in the urine excreted depend on physiological needs/homeostasis, and are adjusted late in nephron
☆ Decreased plasma [Na+] activates renin-angiotensin-aldosterone system --> secretion of aldosterone (adrenal cortex)
- Stimulates sodium reabsorption, to increase plasma [Na+]
- Causes passive reabsorption of chlorine
- Water follows via osmosis to increase blood volume
- Aldosterone also stimulates potassium secretion into filtrate when plasma [K+] is high
Homeostasis of Plasma Sodium
1. ADH:
☆ Regulates water reabsorption to regulate urine volume and blood volume
2. Renin-angiotensin-aldosterone system:
☆ Stimulates secretion of aldosterone when sodium intake is low
3. Aldosterone:
☆ Stimulates sodium reabsorption in the cortical collecting ducts
Renal Control of Sodium/Potassium Balance Pt. 2
☆ Potassium is filtered from the glomerulus
- Some is reabsorbed in proximal convoluted tubule
☆ Aldosterone stimulates potassium secretion in collecting duct when plasma [K+] is high
Renal Control of Acid/Base Balance
☆ Kidneys regulate blood pH by excreting H+ in the urine, and by reabsorbing bicarbonate into the bloodstream
- Urine is slightly acidic because almost all of the filtered bicarbonate is reabsorbed
☆ Acidosis
☆ Alkalosis
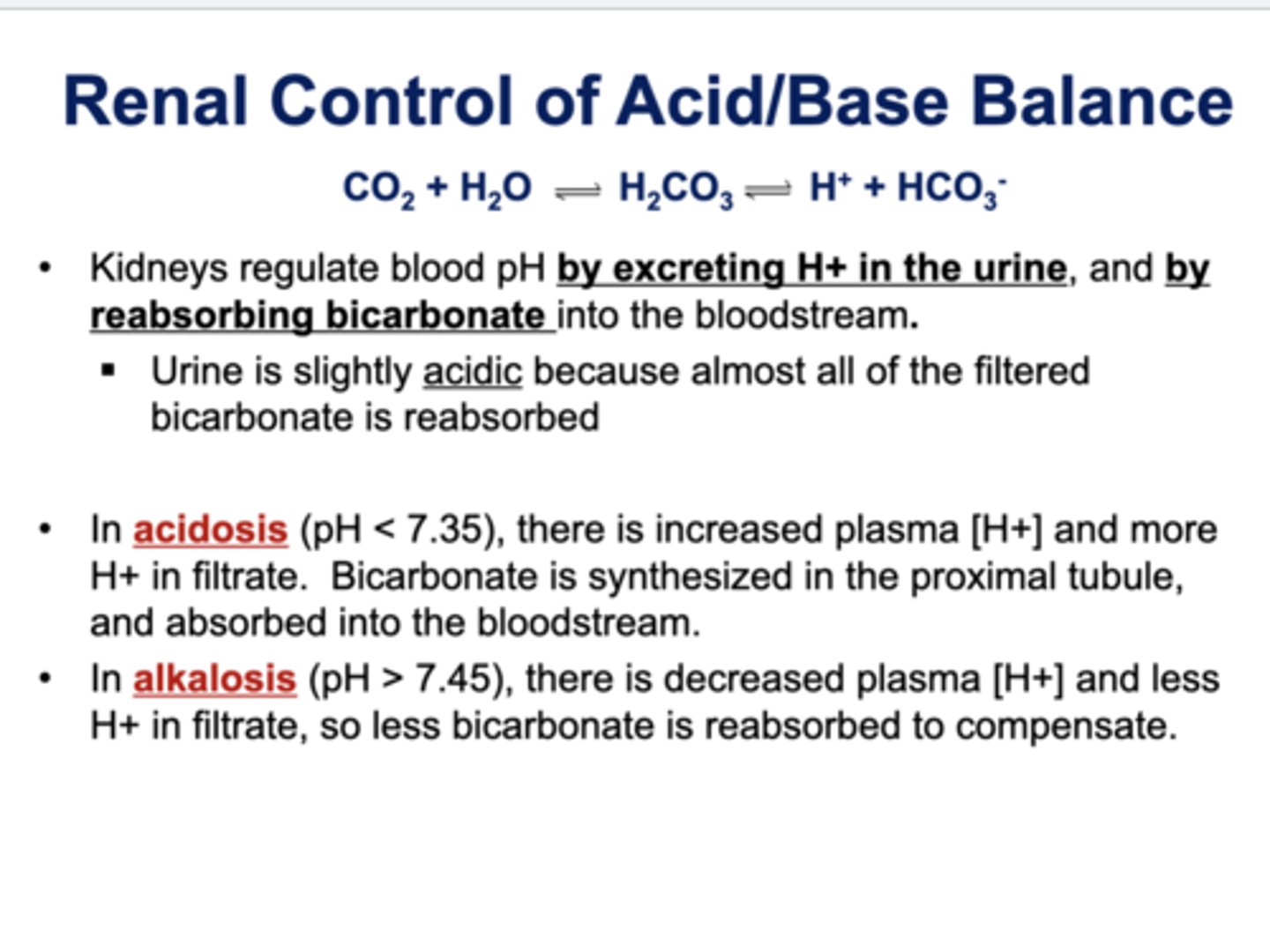
Acidosis
☆ pH < 7.35 (less than)
- There is increased plasma [H+] and more H+ in filtrate
- Bicarbonate is synthesized in the proximal tubule, and absorbed into the bloodstream
Alkalosis
☆ pH > 7.45 (greater than)
- Decreases plasma [H+] and less H+ in filtrate
- So less bicarbonate is reabsorbed to compensate