Cardiac Muscle Mechanics
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Cardiac output (CO)
HR x SV
What is typically the cardiac ouput at rest?
5000mL/min (5L/min)
Typical HR at rest?
72 bpm
typical stroke volume at rest?
70 mL/beat
Heart rate can increase to a maximum of _______________.
approx 220 - age
ex: my max HR = 220-28 = 192 bpm
What is the maximum that stroke volume can increase?
increase up to 50%
How does stroke volume increase during exercise when the increase in heart rate decreases duration of diastole (ventricular filling time)?
-increase preload
-increase contractility (positive inotropy)
-decreased afterload
SV = End diastolic volume (EDV) - end systolic volume (ESV)
*any factors hat affect these parameters can affect stroke volume
preload
initial stretching of cardiac myocytes prior to contraction; average ventricular sacromere length at the end of diastole ==> pressure inside the ventricles when it's full (stretching)
-wall stretch max @ EDV (EDP) after ventricular filling
*increased EDV = increased sacromere stretching = increased force of next contraction = increase stroke volume
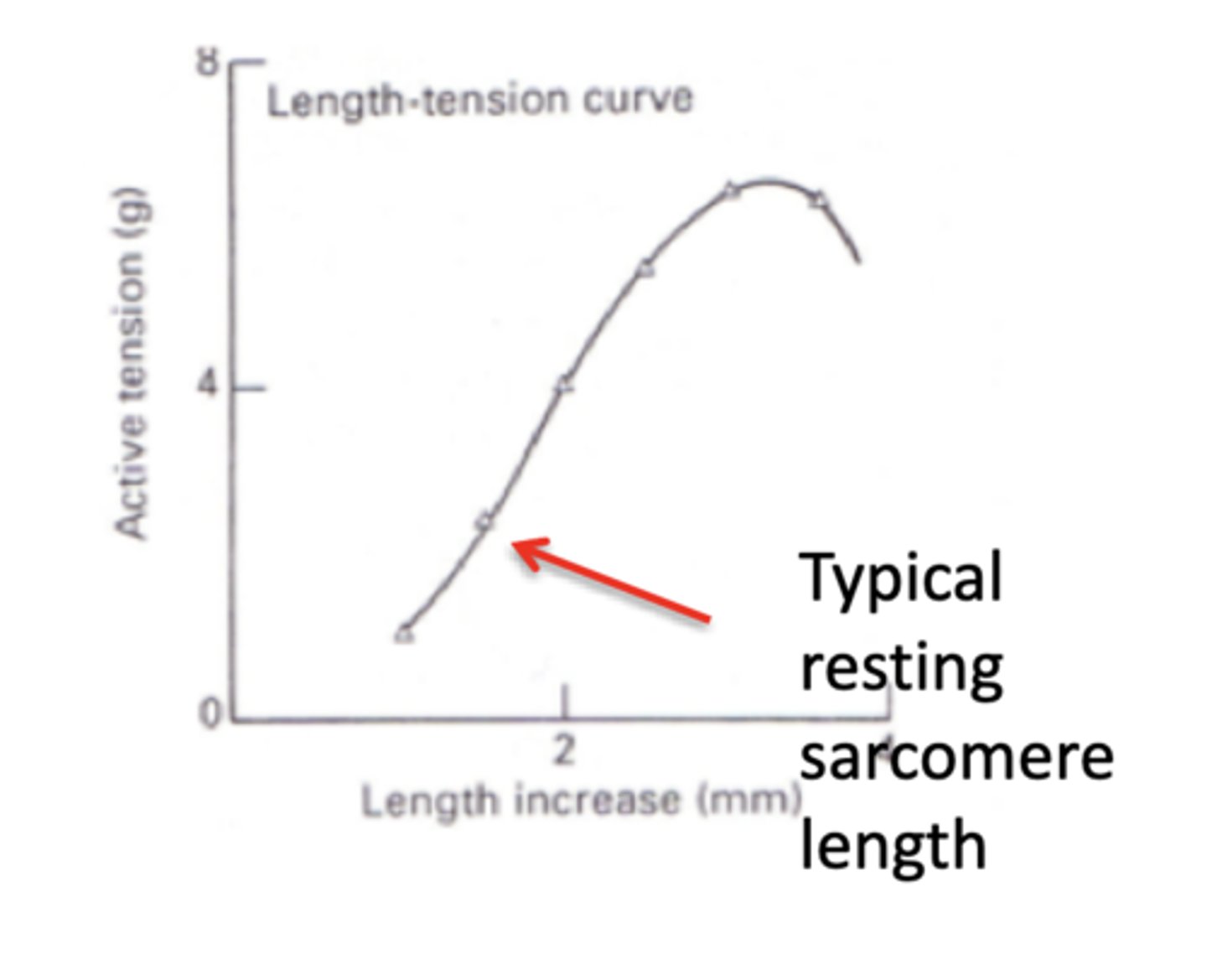
Frank-Starling Law of the Heart
the greater the volume of blood entering the heart during diastole (end-diastolic volume or pressure), the greater the volume of blood ejected during systolic contraction (stroke volume) & vice versa
*stretching a resting cardiac fiber causes an immediate rise in contractile force in the very next contraction (y-axis of graph can be contractile force)
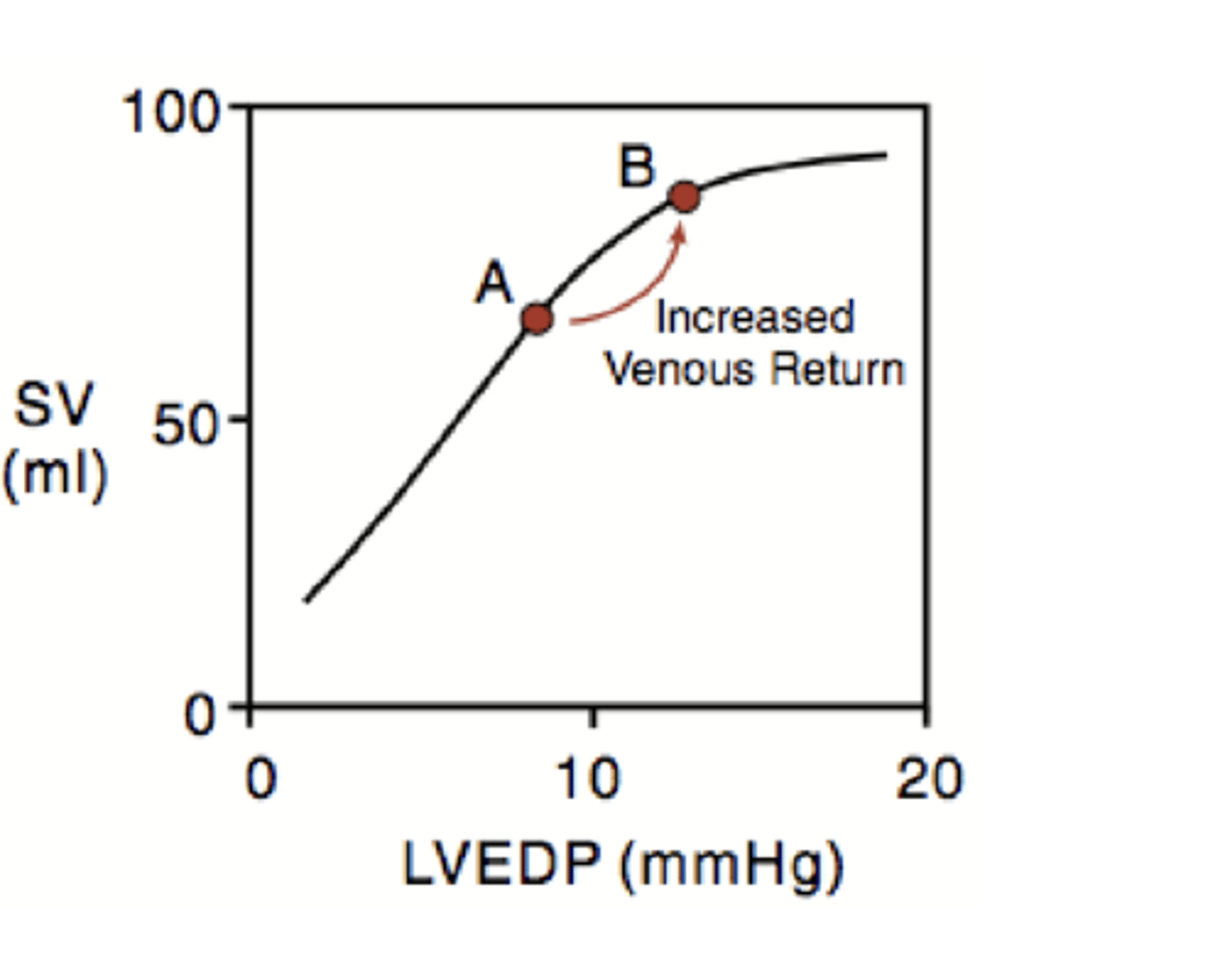
How does EDP (EDV) become increased?
increased venous return to the heart
-exercise
-elevating feet (gravity)
-doing a hand stand
Why does the stroke volume increase when the EDV is increased?
SV is increased when the EDV is increased to compensate for the increase in volume so that the heart can always have the same ESV
up preload = up SV --> get same ESV
down preload = down SV --> get same ESV
Describe the mechanisms underlying Frank-Starling (Preload)
-myofilament overlap==> need optimal relationship bwtn thin & thick filaments for optimal crossbrige formation--> stretched enough to allow contact bwtn every crossbridge, but can't be too far apart so that they can reach each other
-length-dependent activation ==> stretching sacromeres to expose more binding sites for Ca2+ to activate more thin filaments
Compliance
ratio of volume change to pressure change
-ventricles have decreased compliance @ higher volumes (can't stretch as much the higher the blood volume)
-ventricular hypertrophy decreases compliance--> decreases the volume in the ventricle after filling (decreases EDP)--> decreases sacromere stretch --> decreases preload--> decreases SV
-chronic volume overload --> dilation of ventricles --> increased compliance -->increased EDV @ a lower EDP --> stretches sacromeres --> increased SV temporarily but sacromeres can become over stretched & reduce crossbridge formation
What effect does ventricular hypertrophy have on compliance?
ventricular hypertrophy decreases compliance--> decreases the volume in the ventricle after filling (decreases EDP)--> decreases sacromere stretch --> decreases preload--> decreases SV
What effect does dilation of the ventricles due to chronic volume overload have on compliance?
chronic volume overload --> dilation of ventricles --> increased compliance -->increased EDV @ a lower EDP --> stretches sacromeres --> increased SV temporarily but sacromeres can become over stretched & reduce crossbridge formation
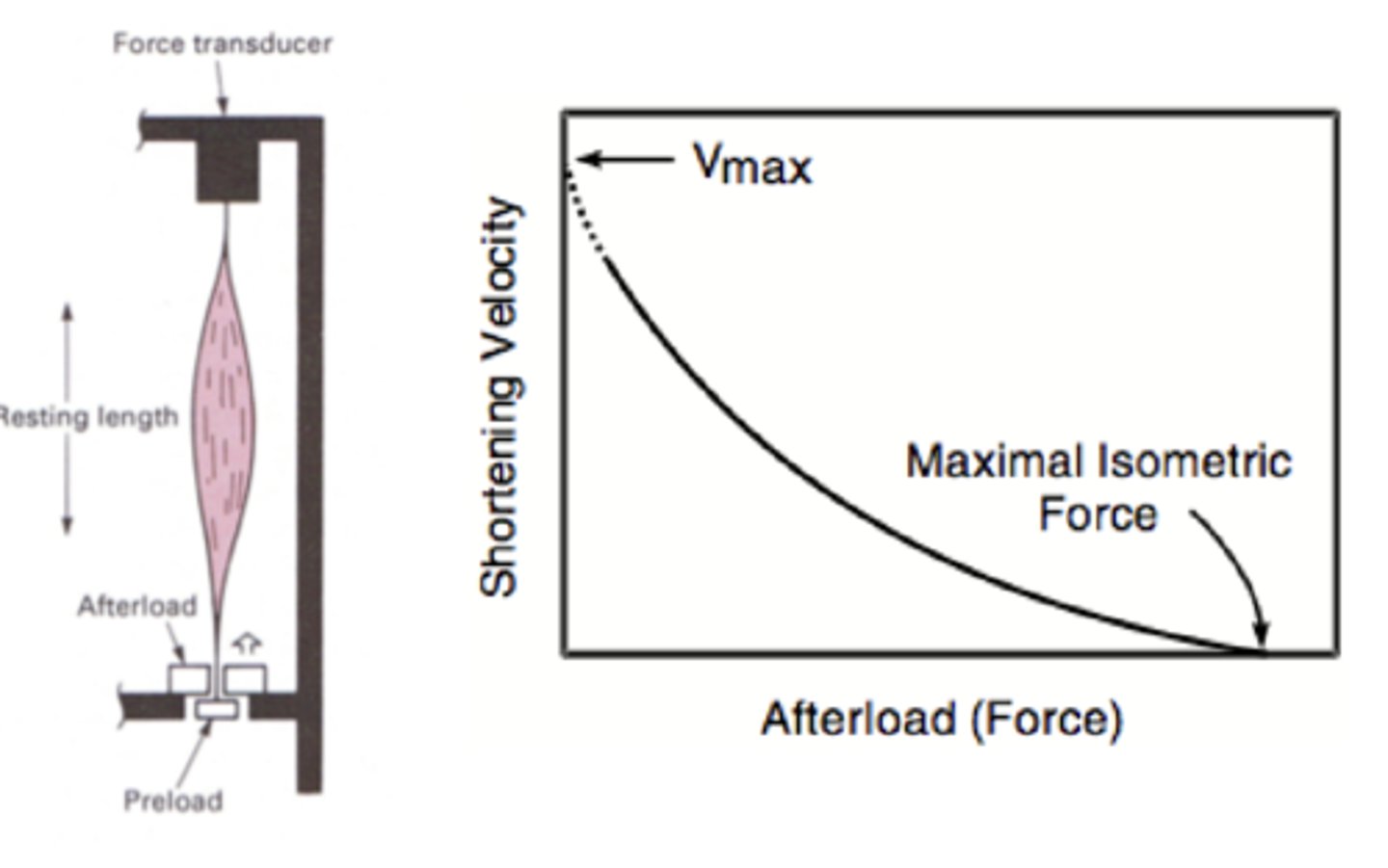
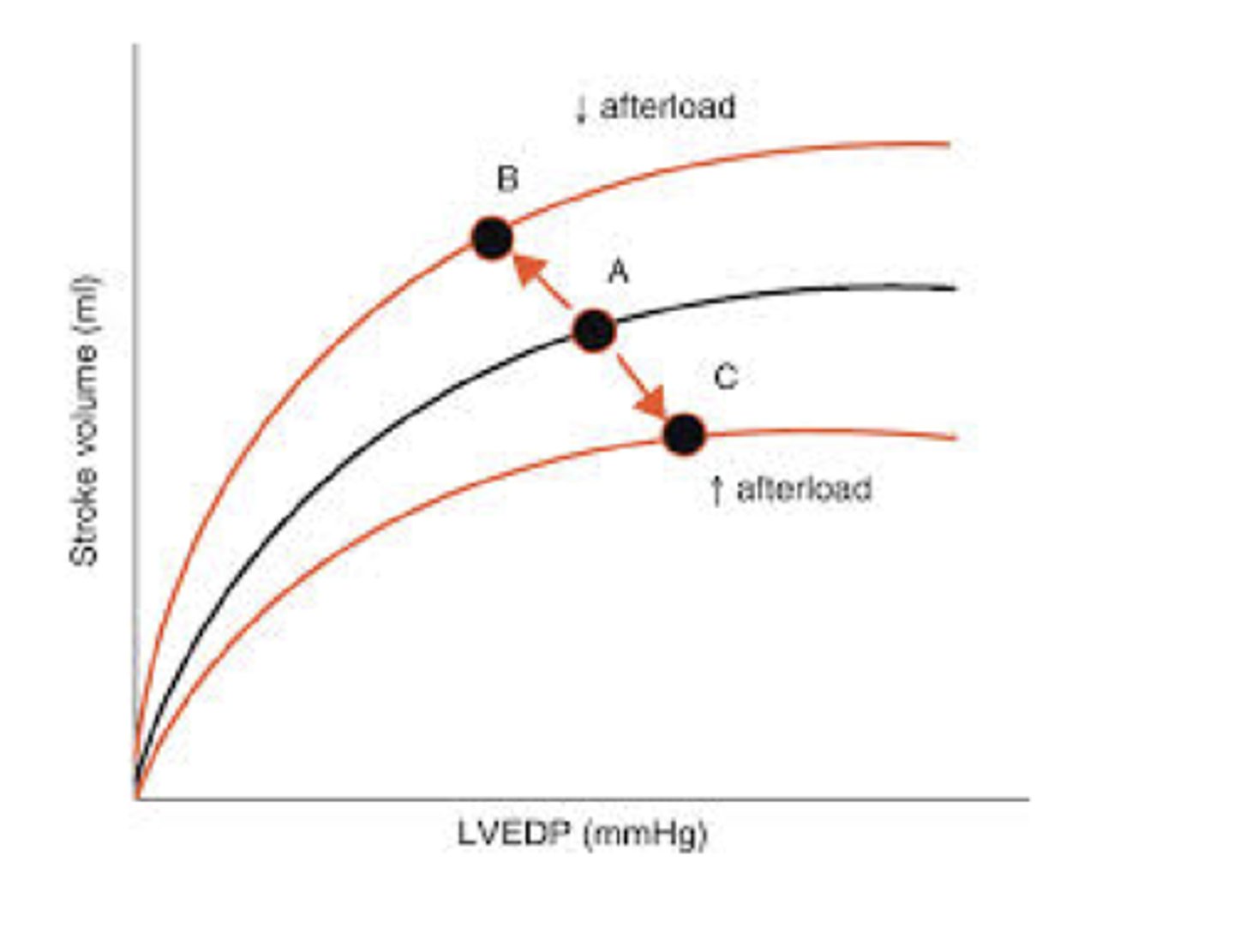
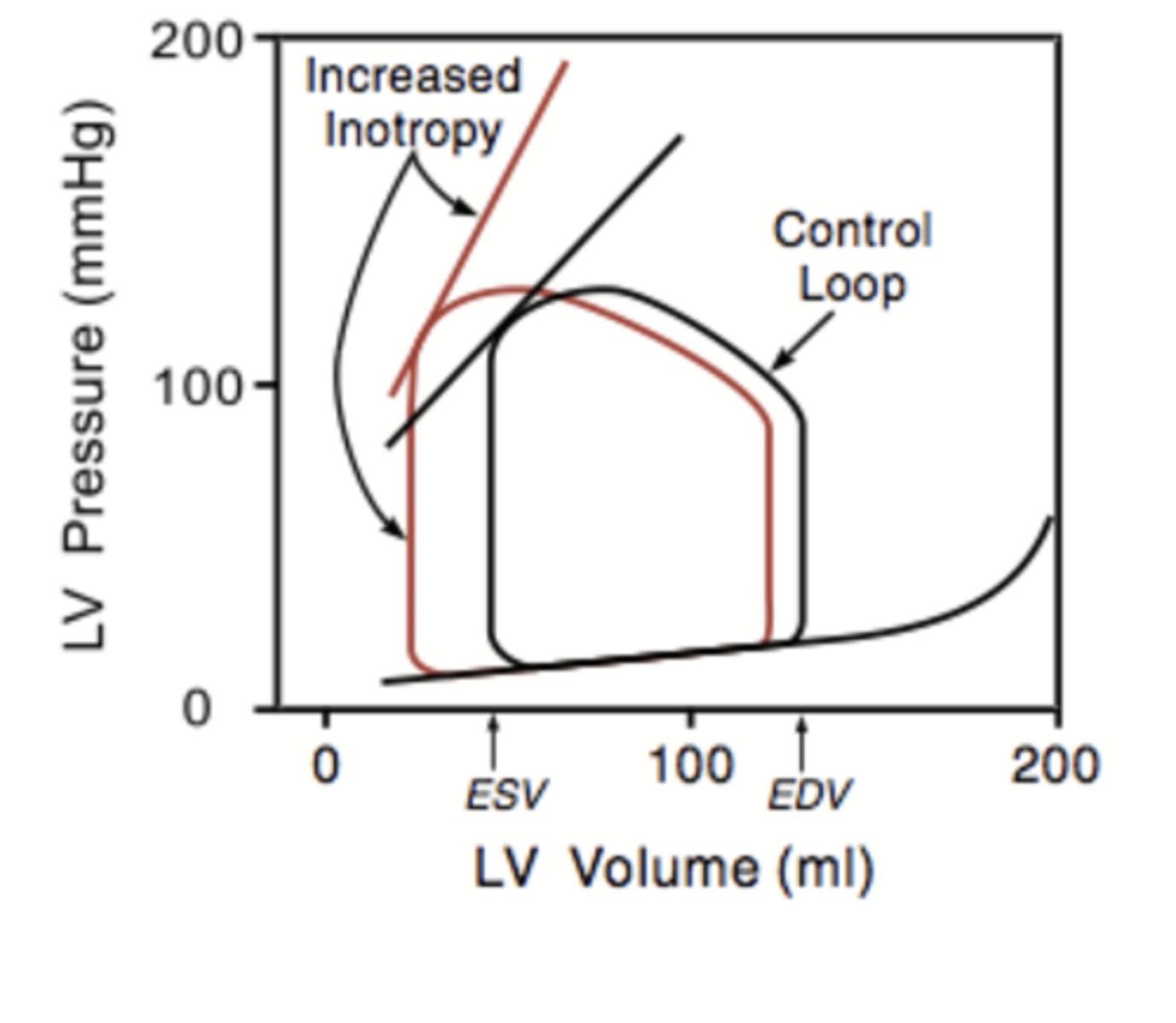
Flow Volume Loop Illustrating Frank-Sterling Regulation of Stroke Volume
increasing the venous return stretches the volume v. pressure graph
-up SV (increase distance bwtn ESV & EDV lines)
-increased volume of blood ejection to reach ESV (meets at same point as control graph) --> heart will compensate for changes to preload to get the same ESV (ejected volume will change to get the same ESV)
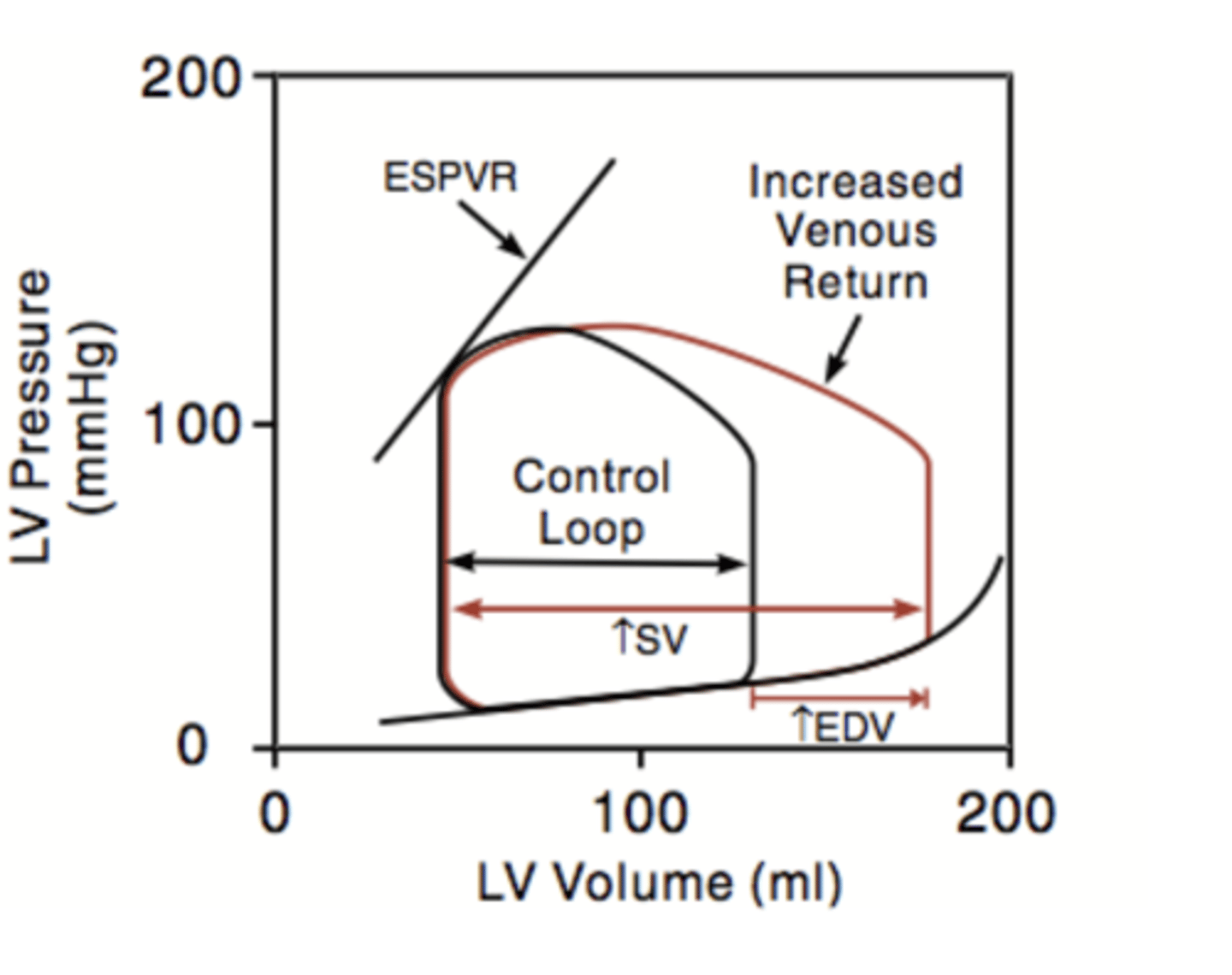
heterometric regulation
preload affects cardiac function by changing sacromere length ==> ejected volume will change to give the same ESV
-increased venous return --> extra blood over & above the "normal" EDV will be ejected
-decreased venous return --> the volume ejected will be decreased
Afterload
the load against which the heart must contract to eject blood
- = aortic pressure for left ventricle
- =pulmonary arterial pressure for right ventricle
*ventricular wall will thicken (hypertrophy) to overcome high afterload
o = Pr/h
*wall stress is a component of afterload
-r = radius of ventricle
-o = wall stress
-h = thickness of ventricle wall ==> increase thickness, decreases the wall stress (hypertrophy that overcomes the high afterload)
Maximal Isometric Force
reached when the muscle can no longer contract against the afterload ==> generates an equal amount of force as the afterload but not greater than the afterload b/c it can no longer lift the weight
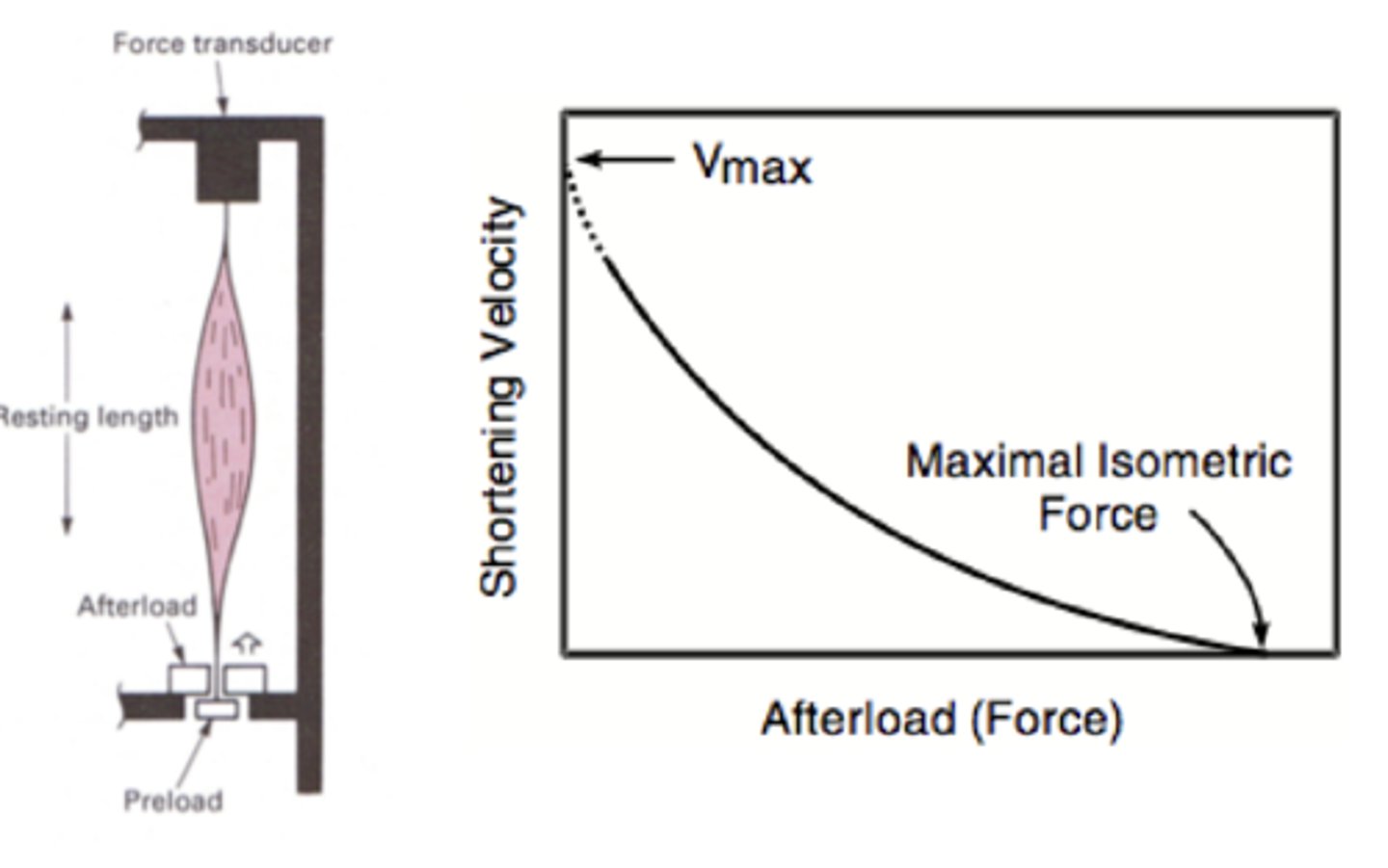
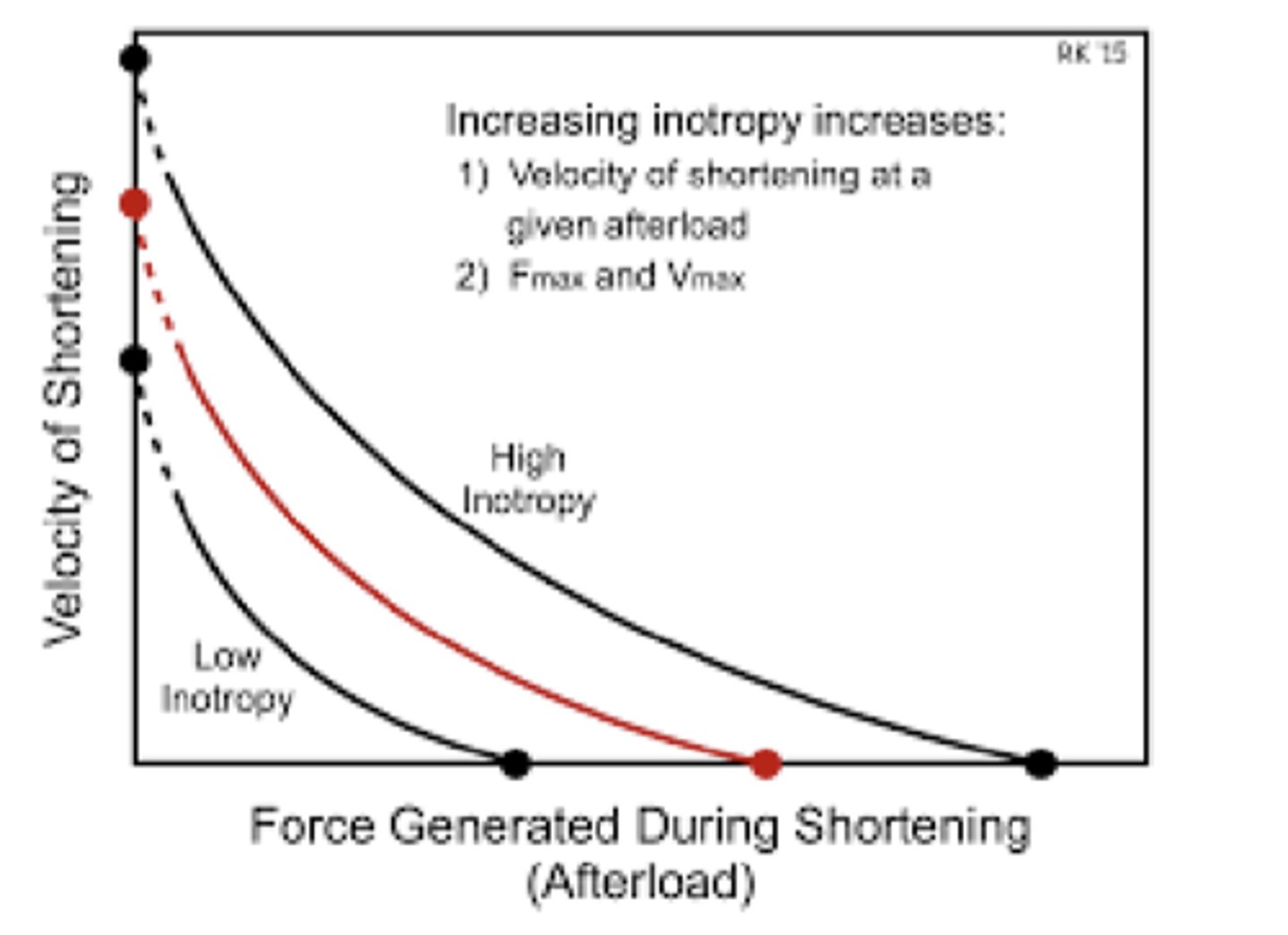
Force-velocity Relationship
the greater the afterload the slower the muscle is able to shorten ==> eventually afterload is too heavy & muscle is unable to shorten b/c can only generate equal amount of force as the afterload
*Heart
-increasing aortic pressure = increasing afterload
-heart must develop higher pressure to open the aortic valve & shortening velocity will decrease with increasing afterload
True or False: Given that systole occurs in a finite time, increased afterload will reduce the stroke volume
True
Flow-Volume Loop for Increased Afterload
increased aortic pressure (afterload) --> decreased SV --> increased ESV --> venous return from next heart beat added to increased ESV --> increased EDV--> increased left ventricle pressure to overcome high aortic pressure to open the aortic valve (ends w/ abnormally high diastolic pressure)--> increased ejection pressure needed to overcome aortic pressure to pump blood into it (ends w/ abnormally high systolic pressure)
*afterload effects on cardiac performance = homeometric regulation
*Increased EDV = increased preload --> might partially compensate for decrease in SV
Afterload effects on cardiac performance are not a function of sacromere length and are termed _______________________.
homeometric regulation
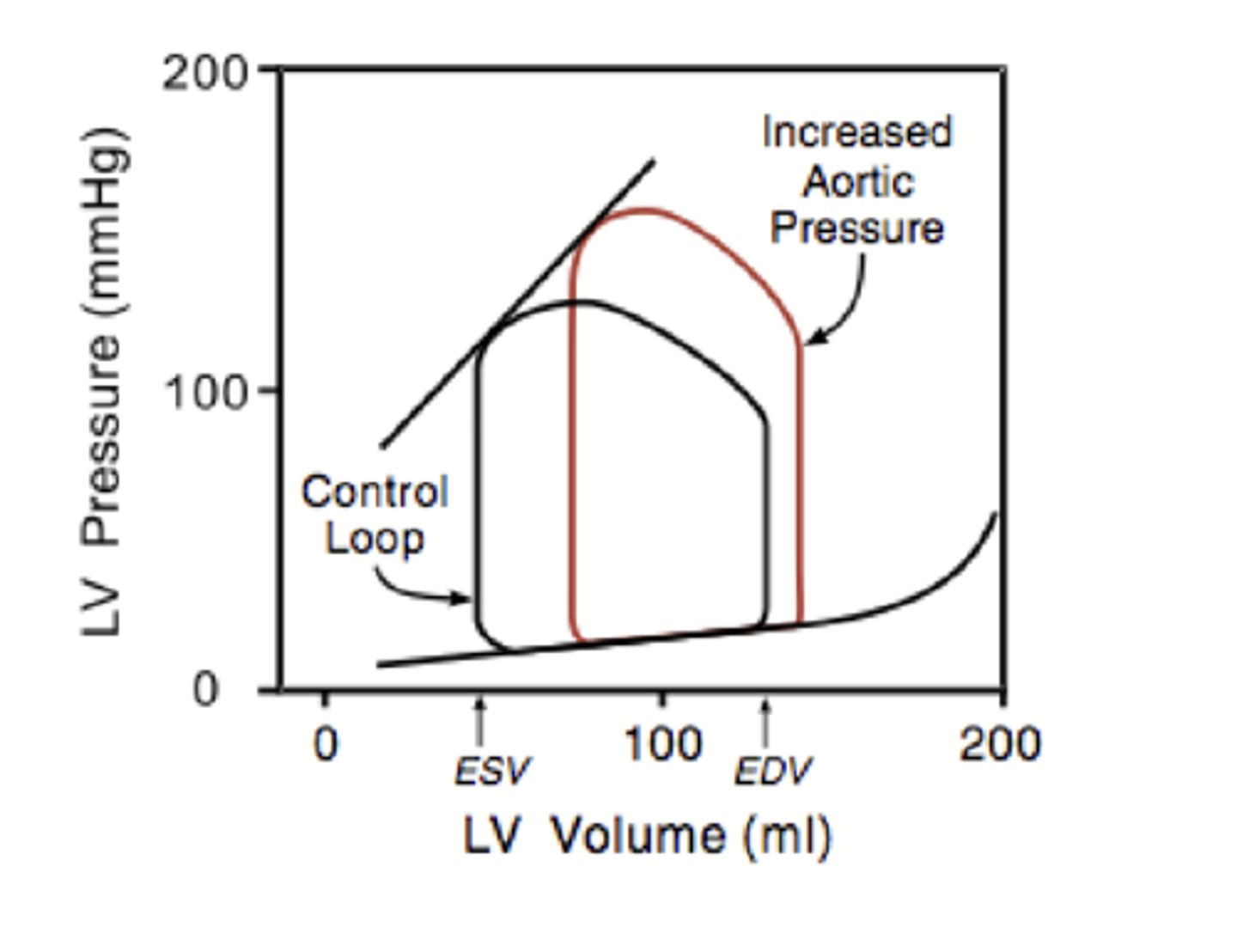
What is the effect of an increased afterload on preload?
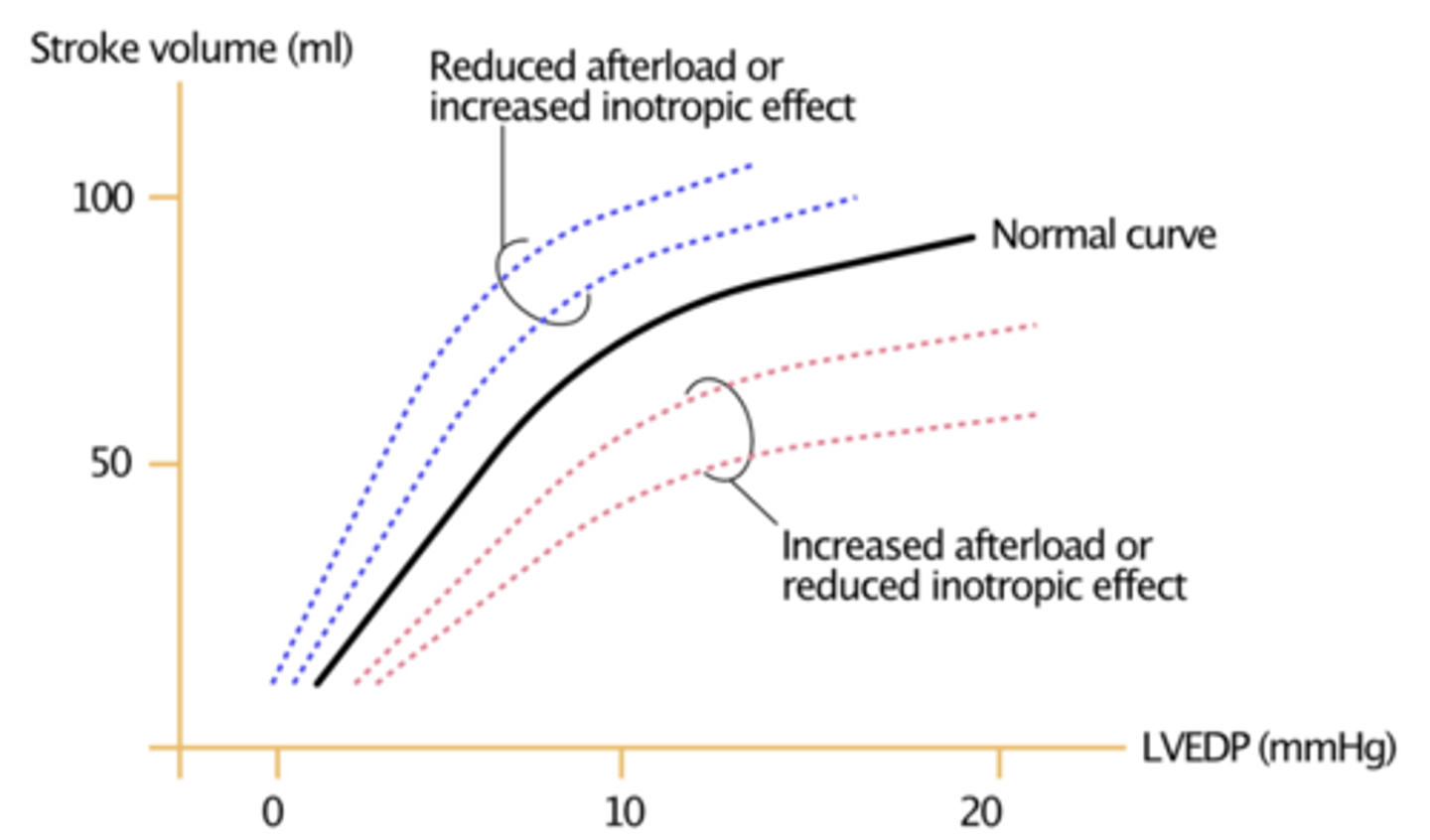
increase in afterload shifts the Frank-Starling curve downward & to the right ==> decreases SV at any preload
What is the effect of decreased afterload on preload?
decreased afterload shifts the Frank-Starling curve upward to to the left ==> increases SV at any preload
What is the effect of an increase in preload on afterload?
an increase in preload shifts the shortening velocity upward & the X intercept to higher isometric force generation
*muscle is able to shorten against higher afterload than it would w/o increase in preload (reaches isometric contraction at higher force)
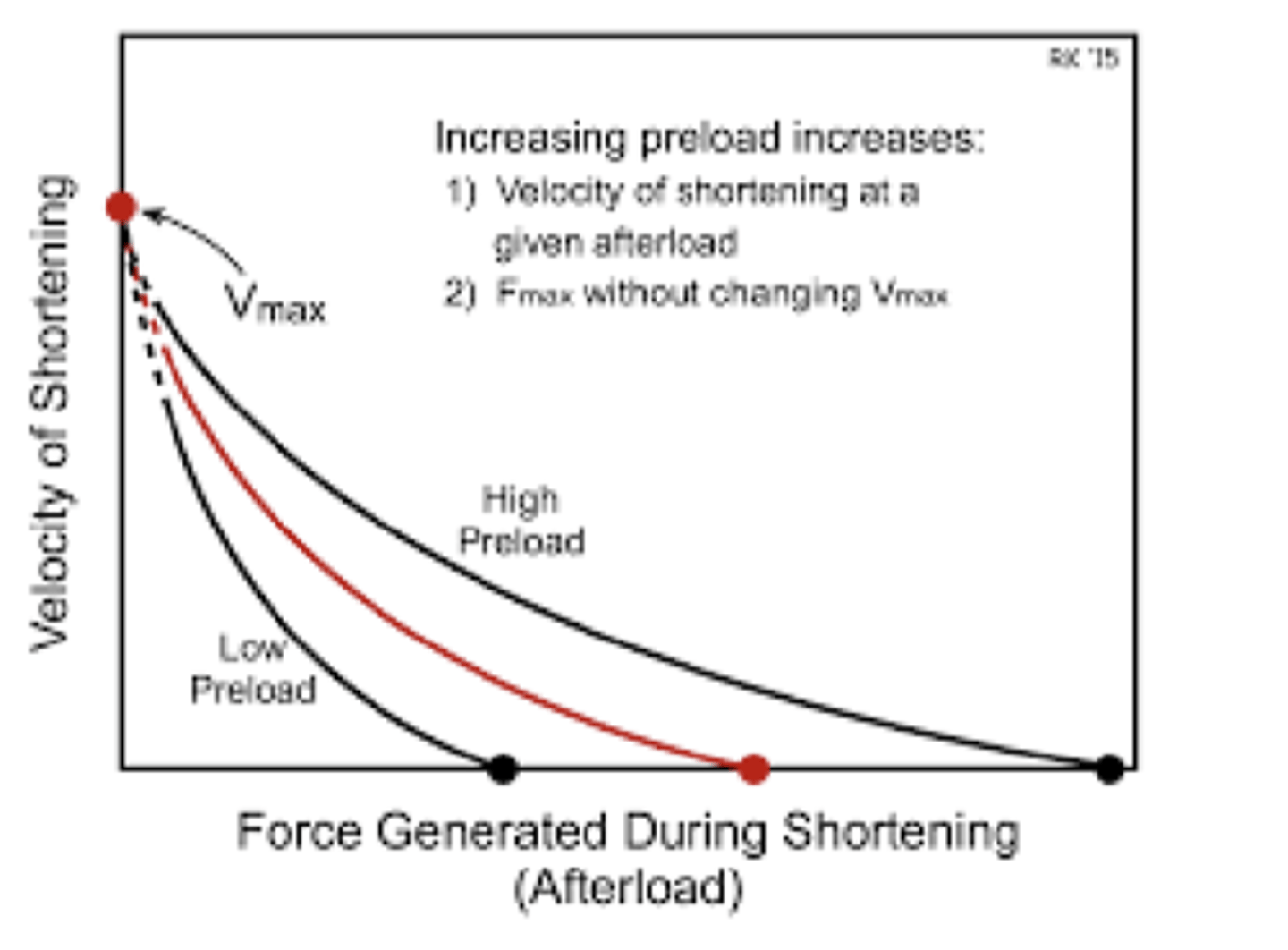
What is the effect of a decrease in preload on afterload?
a decrease in preload shifts the shortening velocity downward & the x-intercept to lower isometric force
*muscle reaches isometric force generation at a afterload force that in lower than it would w/ decreased preload
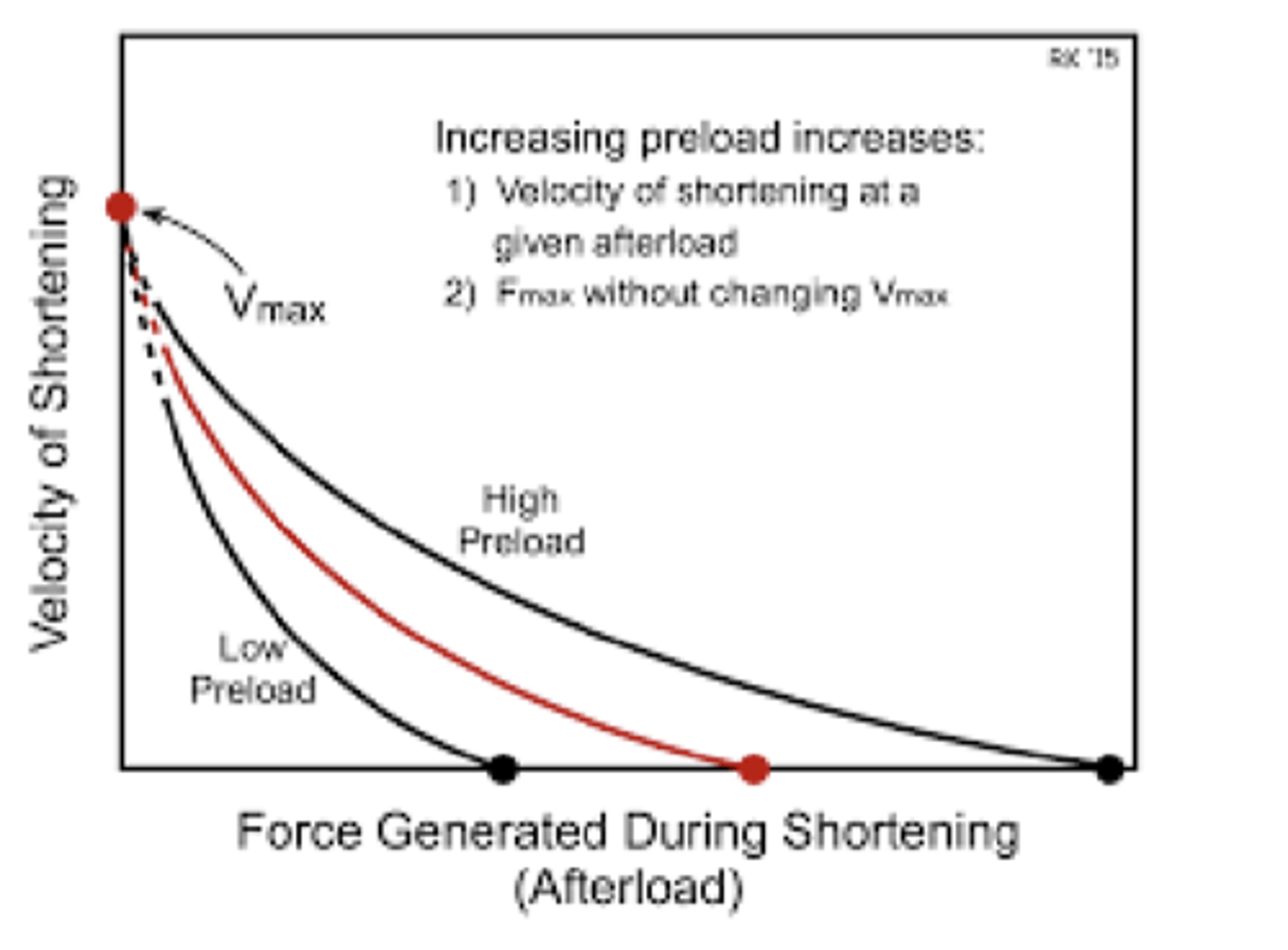
True or False: Changes in preload alter the Vmax of muscle shortening v. force of afterload
False
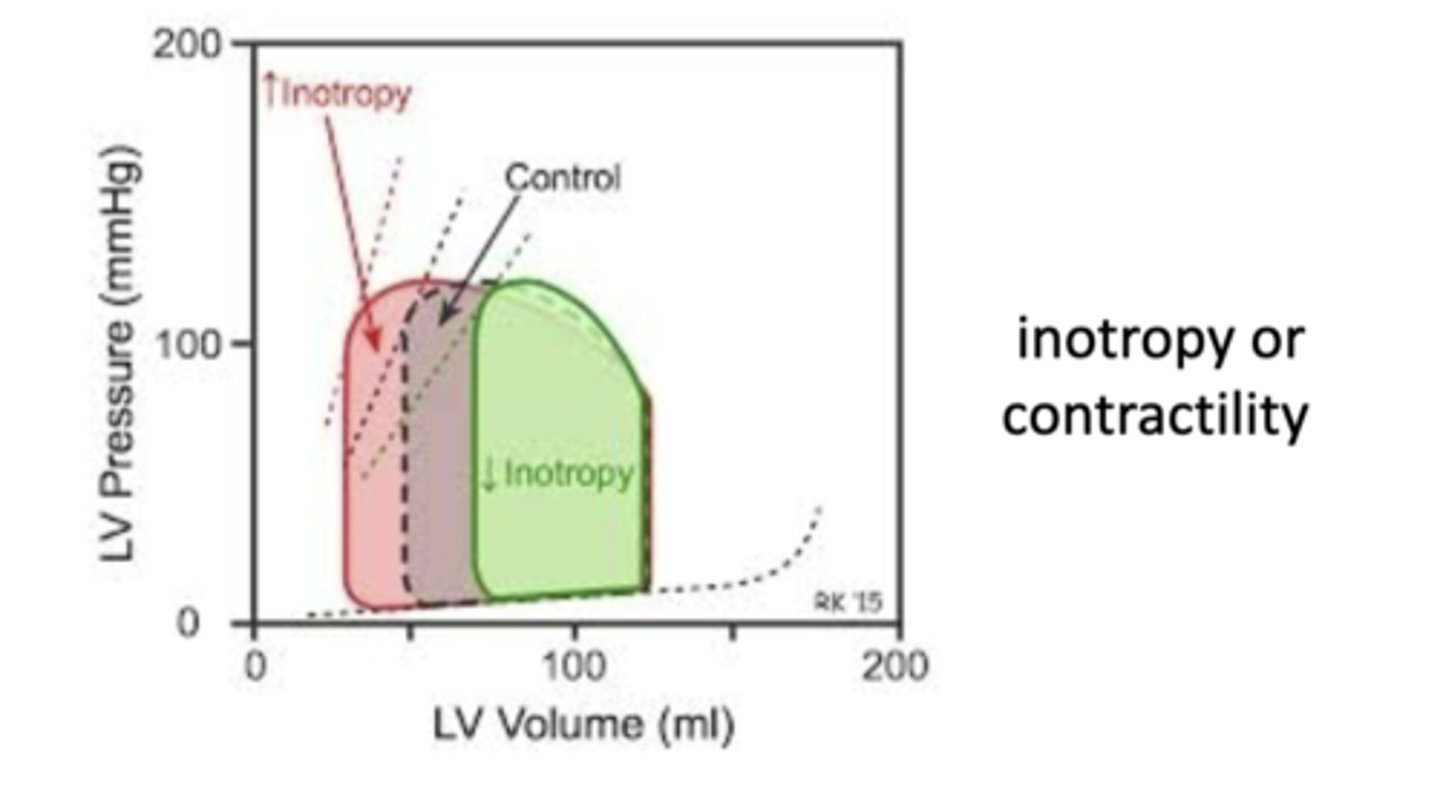
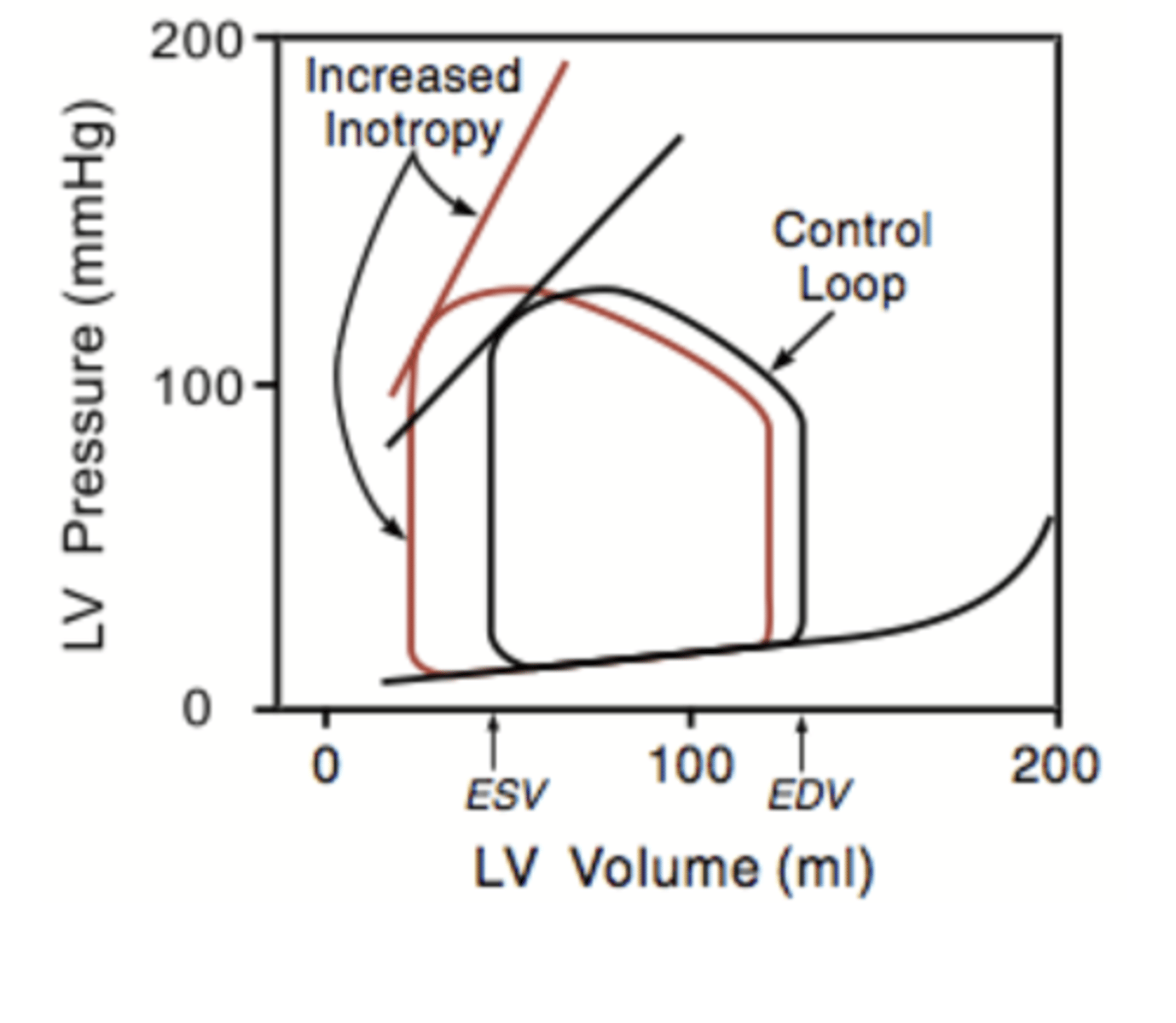
Inotropy (contractility)
an increase or decrease of heart contractility due to autonomic stimulation ==> intrinsic measure of cardiac function independent of extrinsic factors like preload & afterload
-related to rate of force development during ejection (P/t)
-related to end systolic pressure-volume relationship (ESPVR)==> increase in contractility increases the slope of
ESPVR line
-increases stroke volume
-inotropic state ==> increased by SNS, decreased by PNS
inotropic state
increased HR & increased force of contraction
-increased by SNS stimulation to the heart (& epinephrine released by the adrenal medulla)
-decreased by PNS stimulation
What is the effect of increased inotropy on the Frank-Starling curve?
increased inotropy cause shift upward & to the left (just like w/ decreased afterload)
*increased contractile force & SV at any preload
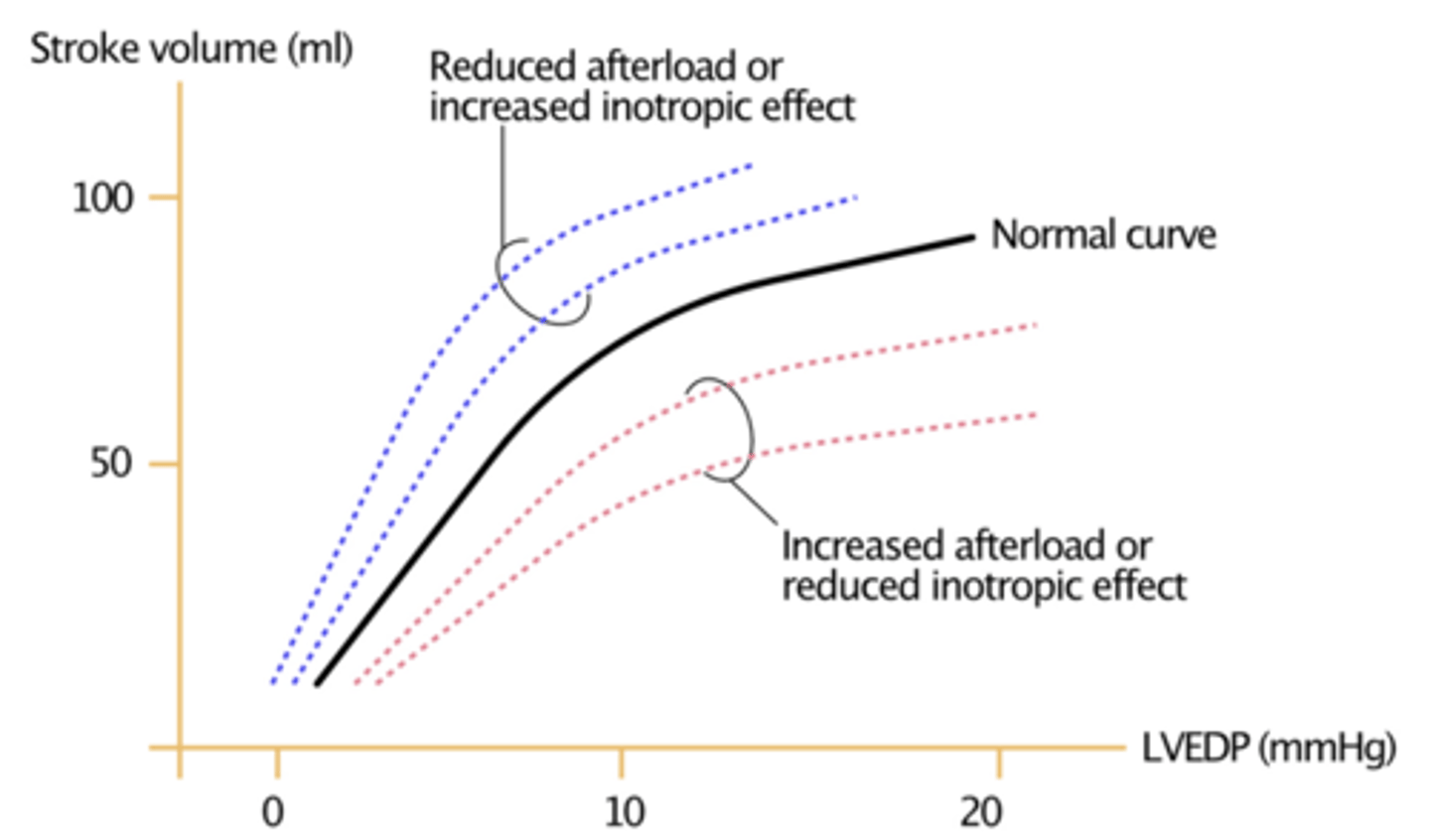
What is the effect of decreased inotropy on the Frank-Starling curve?
decreased inotropy cause shift downward & to the right (just like w/ increased afterload)
*decreased contractile force & SV at any given preload
What is the effect of increased inotropy on the Force-Velocity curve (afterload)?
-increase in inotropy shifts curve upward & increases X-intercept (increases isometric force = able to shorten up to a higher afterload than normal) ==> increases velocity of shortening at any afterload
-increases Vmax
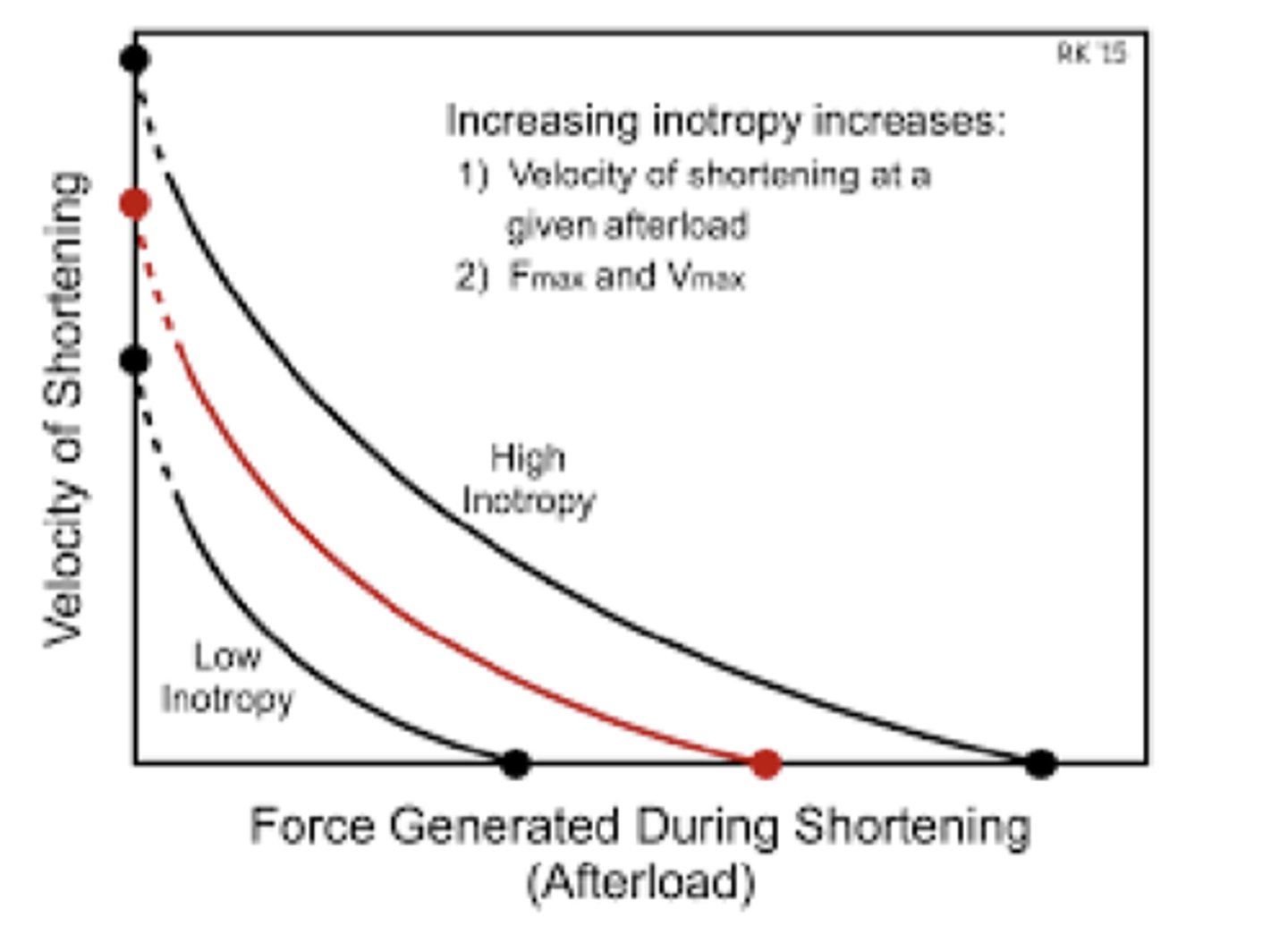
Why is inotropy able to alter the Vmax of Force-Velocity curve (Vmax of muscle shortening v. afterload)?
autonomic stimulation increases or decreases that rate of actin/myosin turnover & ATP use which can increase or decrease the rate of muscle shortening
What is the effect of decreased inotropy on the Force-Velocity curve (afterload)?
-decreased inotropy shifts curve downward & decrease the X-intercept (decreases isometric force = only able to shorten up to a lower afterload than normal) ==> decreases the velocity of shortening at any afterload
-decreases Vmax
What do the positive inotropic effects result from?
-increased rate of delivery of Ca2+ to the myofibrils ==> increased HR increases intracellular Ca2+
-increased binding of Ca2+ to troponin C
-increased rate of cross-bridge cycling
What can result from loss of inotropy?
-heart failure
-cardiomyopathy
-ischemia
What are some examples of drugs that are used clinically to increase inotropy?
-digoxin
-adrenergic receptor agonist
Flow-Volume Loop for Positive & Negative Inotropy