PTE 753: exam 2
1/148
Earn XP
Description and Tags
neuro-developmental treatment, cerebrovascular accident, and cerebral palsy
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
149 Terms
what is neuro-developmental treatement (NDT)?
a holistic and interdisciplinary clinical practice model that emphasizes individualized therapeutic handling based on movement analysis for individuals with neurological pathologies
how does a therapist develop an NDT for a patient?
by continuously observing movement of the patient to make an assessment: typical or atypical?
information gathering
examination
evaluation
intervention
what are the factors of NDT that emphasize the characteristics of normal movement?
based on normal tone
flexible postural control which supports normal movement
ability to shift weight with elongation on weight-bearing side
emphasizes transitional patterns not static holding
in what position should a therapist place a patient with high tone so that he can learn and move functionally?
in whichever position the patient experiences reduced tone
what is the key factor for an NDT approach to therapy?
postural control
what does “emphasize transitional patterns” mean within an NDT approach?
always analyze the patient while he is moving in and out of positions to get a solid understanding of his movements
T or F: NDT is a stand alone treatment since it focuses on a patient’s movement patterns.
F; always add functional activities and/or sensory training too
what are the five principles of intervention for an NDT approach?
tone and movement patterns can be influenced by handling, positioning, and sensory information
active movement is required
repetition with variability is required
evaluation and intervention are continuous
work at all levels of the adult or child’s capabilities
why is variability in treatments important?
bc it stimulates life
T or F: NDT evaluations and interventions are always continuous.
T
list some techniques used in an NDT approach to reduce arousal and tone.
perform low intensity, slow rhythm, repetitions of stimuli
apply firm pressure
stimulate antagonist
apply/use warmth
list some techniques used in an NDT approach to increase arousal and tone.
perform brisk, irregular, and high intensity stimuli
perform in upright positions
why do upright positions increase arousal and tone in a patient?
must control more degrees of freedom → more awake/alert → more aware of tone and postural control
how does one normalize tone in an NDT approach?
weight bear in appropriate alignment
elongation and rotation of trunk
active movement
what are the key points of control when facilitating an NDT approach?
wherever the therapist places her hands to stimulate/control the ideal functional movement pattern
what’s the difference between proximal and distal points of control?
proximal points: provide more sensory input and allows for less trial and error; place hands at head, shoulders, trunk, and hips
distal points: provide less sensory input and allows for more trial and error making carry-over higher; place hands at extremities
T or F: an NDT approach should be responsive to the child’s or adult’s ability and mood.
T
an NDT approach places emphasis on ____ of movement by facilitating appropriate movement patterns as needed.
quality
the “as needed” appropriate movement patterns used in an NDT approach should never be _____ because the patient is moving towards her functional independence.
compensatory
T or F: equipment, bracing, and surgery do not replace intervention for an NDT approach.
T
when aiming for whole body alignment during NDT, what should a therapist focus on?
focus on deficits from top to bottom and in all three planes of motion (sagittal, frontal, and transverse)
what is a cerebral vascular accident (CVA)?
a medical emergency where blood flow to the brain is interrupted, either by a blockage or a rupture in a blood vessel, leading to cell damage and potential long-term disability or even death
what are the two classifications of a CVA?
pathologic type: ischemic (thrombosis/ embolism) or hemorrhagic
temporal factors: complete, stroke-in-evolution, transient ischemic attack (TIA)
T or F: a cerebral infarction or ischemic stroke (thrombosis/embolism) is the most common form of stroke.
T
what’s the difference between an ischemic and a hemorrhagic stroke?
ischemic: caused by blockage
hemorrhagic: caused by vessel rupture
what are the four types of ischemic strokes?
embolism: clot from body (usually the heart or lungs) travels to the brain
thrombotic: blockage from plaque buildup in large cerebral vessels
lacunar: blockage from plaque buildup in small cerebral vessels
transient ischemic attacks: temporary blockage resulting in a “mini” stoke
what are the two types of hemorrhagic strokes?
intracerebral: bleeding within brain tissue
subarachnoid: bleeding into subarachnoid space from surface vessels
list some examples of the most common risk factors for a CVA.
hypertension
diabetes mellitus
heart disease
if a patient presented with these risk factors, what could a therapist do to care for this patient?
check vitals; educate and manage PMH/comorbidities; advise for diet and exercise
what are some characteristics and behaviors that increase blood pressure?
high serum cholesterol levels
obesity
diabetes mellitus
heavy alcohol consumption/ elicit drug use/ smoking
why has healthcare seen a drop in mortality rates from stroke in recent decades?
a rise in education and use of hypertensive drugs and more screening and treatment referral centers
where does a thrombotic infarction usually occur?
where plaques form around junctions of branching arteries
these plaques form locally! (do not travel to brain)
where does a embolic infarction usually occur?
where an embolus from the heart, internal carotid artery, or carotid sinus occludes in the brain
usually in branches of the MCA
why does an embolic infarction most commonly occur in the middle cerebral artery (MCA)?
bc it’s branches are a secondary direct continuation of the internal carotid artery making it a straight path for an embolus to travel through
why does healthcare see such a variability in stroke symptoms and outcomes?
strokes affect different brain regions depending on which blood vessel is involved
the brain’s blood supply has individual differences in vascular anatomy
50% of cardioembolic strokes are caused by ___ ____ due to the irregularity of blood flow.
atrial fibrillation
why is surgery to remove a cardiac blood clot risky for a patient on blood thinners?
bc the patient will have to stop taking the blood thinner medication for the surgery which increases the risk of a cardioembolic stroke occurring
what are the four locations for brain hemorrhages?
epidural hematomas
subdural hematomas
subarachnoid hemorrhages
intracerebral hemorrhages
why are subarachnoid hemorrhages the most deadly location for a hemorrhagic stroke to occur?
bc its everywhere and specifically within the ventricles-→ backs up CSF causing elevated pressure in and around the brain
would a hemorrhagic stroke cause focal or global deficits?
both! depends on the artery and amount of blood in affected area
what’s the difference between focal and global deficits?
focal: specific, localized damage leading to problems in a distinct area or function.
global: diffuse, widespread damage impacting multiple brain regions, leading to more general and widespread impairments.
what is a saccular aneurysm?
a type of aneurysm characterized by a sac-like bulge on the side of a blood vessel
usually found at branchings of major cerebral arteries-especially in the anterior circulation
what is the anterior circulation supplying blood to the brain?
carotid artery system:
internal carotid artery
anterior cerebral artery
anterior communicating artery
middler cerebral artery
posterior communicating artery
what is the posterior circulation supplying blood to the brain?
vertebral-basilar system:
vertebral arteries
basilar artery
anterior inferior cerebellar artery
superior cerebellar artery
posterior cerebral artery
posterior inferior cerebellar artery
what is an arteriovenous malformation (AVM)?
an abnormal tangle of blood vessels connecting arteries and veins, bypassing the capillaries
the developmentally weak vessels of an AVM are prone to rupture
an ______ _______ is the most common cause of CVA in a young person (10-35 years of age).
arteriovenous malformation (AVM)
which vessel is mostly commonly affected in strokes?
middle cerebral artery (MCA)
an acute inpatient therapist has a new patient s/p ACA CVA 2 days ago. what symptoms should the therapist prepare for?
motor deficits- specifically LE on affected side
lack of initiation and decision making
urinary incontinence
contralateral neglect!!
an acute inpatient therapist has a new patient s/p MCA CVA 2 days ago. what symptoms should the therapist prepare for?
slurred speech
tingling or numbness in face, arm, or leg on affected side
loss of movement on affected side
an acute inpatient therapist has a new patient s/p PCA CVA 2 days ago. what symptoms should the therapist prepare for?
visual field deficits
possible sensory loss
memory and emotional disturbances
PICA and AICA strokes are rare due their anastomoses, but what symptoms will arise if a patient does have an occlusion within these arteries?
coordination issues, vertigo, and cranial nerve symptoms
an occlusion of the _____ artery results in a pure sensory stroke. why?
thalamic-proliferating
this branch from the PCA supplies the thalamus where sensory pathways synapse before traveling to the somatosensory cortex
an occlusion of the _____ artery results in a pure motor stroke. why?
lenticulostriate
this branch of the MCA supplies the internal capsule where the motor pathways travel
T or F: a stroke within the MCA superior division will cause the greatest amount of paralysis due to the homunculus layout.
F; a stroke within the internal capsule’s division
during an acute thrombosis and TIAs, the goal is to improve cerebral circulation as quickly as possible to prevent ischemic tissue from becoming infarcted tissue. which drug helps with this?
TNKase tenectepase
strong breaker of clots (reduces or eliminated clots) but may still have deficits following dosage
_____ _____ are used to prevent TIAs and may stop a stroke-in-evoultion.
anticoagulant drugs
what type of stroke are individuals with sickle cell anemia likely to experience and why?
ischemic
abnormal red blood cell shape gets hung up at branch points, leading to clots
describe an ischemic core and a penumbra
ischemic core: where most decrease in blood flow within tissue occurs; may be dead tissue and show no improvement
penumbra: area around ischemic core where potential for recovery is possible; area for neuroplasticity
T or F: aphasia and dysarthria are the same.
F; aphasia is difficulty understanding and processing speech and dysarthria is difficulty speaking due to motor issues
an injury within the ___ lobe may lead to Broca’s aphasia and an injury at the ____ ____ intersection may lead to Wernicke’s aphasia.
frontal
parietal-temporal lobes
Broca’s aphasia (expressive)
a language disorder that primarily affects the ability to produce fluent speech, characterized by difficulty forming complete sentences and finding the right words
usually aware of their communication struggles and comprehension of language is intact
Wernicke’s aphasia (receptive)
a language disorder characterized by difficulty understanding spoken and written language, despite that ability to produce fluent speech
speech often lacks meaning and may include random words; may not realize their speech is incomprehensible
as a physical therapist treating stroke patients, why is it important to emphasize combining movement with speech?
dual-tasking with speech and movement can seem “natural”, making recovery come easier to the patient
the prefrontal cortex allows us to be visually attentive to the contralateral visual field. what treatment strategies could a therapist use to help a patient visually scan to the affected side?
enhance sensory stimulus to that side (physical, auditory, visual) and allow patient to learn via making errors and problem-solving
use things that patient loves to keep activity engagement up
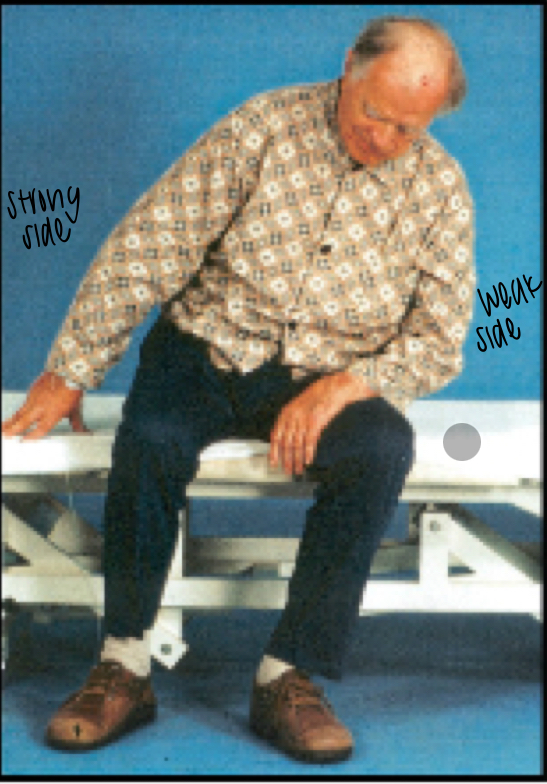
pusher syndrome
a condition following a stroke or TBI where the patient pushes away from the non-paretic side towards the paretic side, leading to a tilted posture and a loss of balance
a stroke or TBI to what specific area would result in pusher syndrome?
damage to the ventroposterolateral thalamus (VPL); believed to be responsible for gravioception (perception of one’s body relative to gravity)
T or F: a patient with pusher syndrome usually has an intact perception of upright but he cannot feel that his body is tilted.
T; (perception of) visual vertical is always preserved
why wouldn’t physically helping a patient move into a more vertically aligned position be helpful?
the patient will fight back, making it (balance and alignment) worse
rehab stays are generally ~2-3 times longer because of this
a lot of patients lean toward a weak side in the early stages of recovery. how does a therapist know if a patient has pusher syndrome?
bc the patient fights against/pushes back if the therapist tries to passively move them
pusher syndrome is a frontal plane deficit so a therapist will want to work on balance with _____ into the frontal plane.
perturbations
describe the gait deficits seen in a patient with pusher syndrome following a right medullary infarct.
longer stride length with L foot and shorter stride length with R foot
what is the biomechanical effect on posture by carrying a weight on the side to which the patient pushes?
forces the patient to correct and counter the weight by leaning/shifting center of mass to other side
what is one of the best treatment options for a patient with pusher syndrome?
mirror therapy! never use parallel bars
on which side would a therapist guard someone with pusher syndrome?
Dr. Shaw’s answer: on weak side to act as protection
boards’ answer: on strong side to act as a target
why is it important to include divided attention (dual-tasks) to a stroke patient’s recovery process?
most of our movements and the control of our posture occur without much thought. when the pathways that control autonomic movement are damaged, then intact cortical pathways try to compensate, leading to inefficient methods. we want to correct that as best as possible.
list an example of a motor-motor and a motor-cognitive divided attention (dual-task) activity.
motor-motor: walking while holding a cup of water
motor-cognitive: walking while reading street signs aloud
what is learned non-use?
a phenomenon where individuals, often after a neurological injury, suppress the use of a limb even though they have the capacity to use it
list some examples of effective strategies to prevent learned non-use.
ask the patient to “help” you
transfer to/from using both sides
use affected side during activities
what is constraint-induced movement therapy (CIMT)?
focuses on increasing use of the paretic limb post-stroke by restricting the non-paretic limb
patient must have an intact ____ ____ to use and see the benefits of FES and NEMS.
reflex arc
per this class, what is the difference between FES and NMES?
FES: passive and active motions; activate muscle during context of use (best for gait training)
NMES: passive and active motions; solo contraction of an isolated muscle
how is FES like a “neuroprosthesis”?
assists in muscle stimulation to achieve a desired response like when using an AFO
is FES considered a compensatory or recovery intervention?
sike its both again!; it depends on the patient’s preference and his/her ability to recover/improve
for FES to be considered recovery, it needs to show benefits and improvement in a specific and desired task
while the ultimate end-goal is _____ movement that is coordinated and not synergy bound, often after a stroke the first purposeful movement that can be elicited is _____ movement.
voluntary
facilitated
describe Ramistes.
the movements of hip abduction and adduction are neurologically coupled, such that greater effort in one extremity will “overflow” to the other
“yoked” together → cue at same time to get a synergistic response
T or F: when treating hemiparesis and neglect syndrome, always start with the safety issues related to neglect.
T
describe a good cue given to a stroke patient when working on sit to stands.
“lean over your bad side to shift, bringing your nose over your toes, and weight bear on bad side to stand” → works on head hip relationship and avoids learned non-use of paretic side
what are two key components when working with patients suffering from hemiparesis and neglect syndrome?
want to enhance all senses on neglect side- visual, auditory, physical/self, touch
give little feedback to allow patient to respond to environment
what are the ten principles of neuroplasticity to treatments?
use it or lose it
use it and improve it
specificity
repetition matters
intensity matters
time matters
salience matters
age matters
transference
interference
what is cerebral palsy (CP)?
a group of permanent disorders of the development of movement and posture, causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain
what are the top three associated disabilities of CP?
language disability
visual disability
cognitive delays; seizure disorders
what are the two ways to define CP?
types of signs and symptoms present
limb involvement
what are the types of CP that are categorized by their signs and symptoms?
spastic: stiff muscles and exaggerated reflexes
dyskinesia
athetoid: involuntary, fluctuating muscle movements, often described as slow, writhing, or twisting
dystonia: sudden, uncontrollable movements
ataxia: problems with balance and coordination
mixed
what are the types of CP that are categorized by their limb involvement?
hemiplegia: one side of the body
diplegia: lower extremities more than upper extremities
quadriplegia: all limbs
what are the five levels/classifications of CP (12-18 yrs old)?
youth walk at home, school, outdoors, and in the community
youth walk in most settings but environmental factors and personal choice influence mobility choices
youth are capable of walking using a hand-held mobility device
youth use wheeled mobility in most settings
youth are transported in a manual wheelchair in all; self mobility is severely limited
list the body function impairments associated with CP.
muscle tone and extensibility
strength
skeletal structure
selective and postural control
motor learning
pain
why do patients with CP develop arthritic pain earlier in life?
they experience limited movement through the full range resulting in decreased diffusion of nutrition to the joint cartilage
muscle tone
a muscle’s typical resting tension
extensibility
resistance of muscle to passive movement or muscle lengthening (stretching)
T or F: persistence of hypotonicity changes the muscle fibers leading to extensibility (stiffer).
F; hypertonicity