Quiz 1/Exam 1 BMS2
1/110
Earn XP
Description and Tags
Study guides for Quiz 1 and Exam 1 from Dr. Hussein
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
Lymphocytes
B and T cells
Natural killer cells (NK)
has no Ag-specific receptor, evolves from innate immunity lymphocyte. Has FcR used for ADCC.
Type of white blood cell. They are capable of recognizing and destroying virus-infected cells and cancer cells. These cells release toxic substances to induce cell death in their targets.
B cells
display BCR on their surface; have MHC I and MHC II. Develop in bone marrow. Have two complement receptors CR1 (CD35) and CR2 (CD21)
They produce antibodies that help fight off infections and provide long-term immunity. They are formed in the bone marrow and can differentiate into plasma cells that secrete antibodies or memory cells that remember past infections.
Cytotoxic T cells
Specialized immune cells that recognize and destroy infected or cancerous cells in the body. They use toxic proteins to induce cell death in their targets.
Display TCR and CD8 molecules on their surface. Develop in thymus
Helper T cells
Cells that coordinate and regulate immune responses. They activate other immune cells, like B cells and cytotoxic T cells, through the release of cytokines. They recognize antigens presented by antigen-presenting cells and help eliminate pathogens.
Display TCR and CD4 molecules on their surface. Develop in thymus
What do all nucleated cells have?
MHC 1
What is MHC?
HLA or Human lymphocytes Ag and has two classes.
They play a crucial role in the immune system by presenting antigens to T cells. MHC class I proteins are found on all nucleated cells, while MHC class II proteins are found on antigen-presenting cells.
MHC II is present in…
B cell, Macrophage, Dendritic cell, presents Ag peptides to TH
Examples of Myeloid cells
erythrocyte, neutrophil, monocyte, eosinophil, basophil and mast cell, megakaryocyte
Examples of PMNs
Neutrophil, basophil and mast cells, eosinophils
What do Basophils (in circulation) & mast cells (stationary) do?
Degranulation with IgE by release of histamine, heparin, and other mediators. Also produce eosinophil chemotatic factor (ECF).
Eosinophils
involved in antiparasitic activity. Degranulation: release of contents in surrounding area. Can kill parasites with basic proteins and cationic proteins
Neutrophils
involved in innate immunity, is a major phagocyte, and MOST common WBC, also important in promoting inflammation
Monocytes
enter circulation from bone marrow then migrate into various organs and tissues. Matures into macrophages and others.
Extravasation
enables WBCs (PMNs, T and B) to leave the blood vessels. Its deficiency increases susceptibility to bacterial infections.
What are the 3 main functions of the complement system?
lysis, chemotaxis, opsonization
What is lysis?
The complement system has an intrinsic ability to lyse the cell membranes of many bacterial species
What happens during chemotaxis
Complement products released in this reaction attract phagocytes to the site of the reaction
What happens during opsonization?
Complement components coat the bacterial surface allowing the phagocytes to recognize the bacteria and engulf them
What are the innate immunity opsonins
C3b, C4b (Complement), CRP (produced by hepatocytes)
What is the adaptive immunity opsonin?
IgG
What are the benefits of the immune system?
Immunization and defense against infectious disease. Cancer detection and management, A benefit of immunology (application): Organ transplantation and blood transfusion
What are the harmful effects of the immune system?
Hypersensitivity or allergic reactions, autoimmune diseases, immunodeficiencies, graft rejection
What are the split products of the complement system?
C3a and C5a
C3b
C3b, C6, C7, C8, and C9
What is the function of split products C3a and C5a?
They act as anaphylatoxins, causing inflammation and attracting immune cells to the site of infection.
What is the function of split products C3b?
It opsonizes pathogens, enhancing their recognition and phagocytosis by immune cells.
What is the function of split products C5b, C6, C7, C8, and C9?
They form the membrane attack complex (MAC), which creates pores in the pathogen's membrane, leading to cell lysis.
What is the final product of the complement system?
MAC [C5b678(9)6]
What is the C3 convertase from the alternative pathway?
C3bBb
What is the C3 convertase for the classic pathway?
C4b2a
What is the C5 convertase for the classic pathway?
C3 convertase-mediated C5 convertase (C4b2a3b)
What is the C5 convertase for the alternative pathway?
C5 convertase (C3bBbC3b)
What are the Activators of the alternative pathway?
Lipopolysaccharides (LPS), Bacterial cell walls, Cell walls of yeasts
What are the Activators of the classic pathway
Antigen-IgG complex – Pentameric IgM
What is clone selection
refers to the process where B cells with BCRs that can bind to the antigen are selected for further development, while those that cannot bind are eliminated.
What is proliferation?
occurs when the selected B cells undergo rapid division, resulting in the expansion of the antigen-specific B cell population.
What is Ag specificity?
refers to the ability of B cells to recognize and bind to specific antigens. During antigen-dependent processes, B cells develop antigen specificity through the rearrangement of their BCR genes to generate a diverse repertoire of BCRs capable of recognizing a wide range of antigens.
What does Antigen-dependent processes in B cell development involve?
involve clone selection, proliferation, and the development of antigen-specific B cells in response to the presence of antigens.
What does Ag-independent processes in B cell development involve?
include the development and maturation of B cells in the bone marrow and the generation of BCR diversity through V(D)J recombination.
What are examples of natural defense mechanisms?
- Acidic pH of the stomach
- Skin
- Lysozyme
- Microflora
- Enzymes
What are the characteristics of acquired immunity system in terms of Ag-receptors, specificity, and memory?
Utilizes B-cell receptors (BCRs) and T-cell receptors (TCRs) to recognize antigens (Ags).
Exhibits high specificity towards individual Ags due to the diverse repertoire of BCRs and TCRs.
Possesses immunological memory, allowing for a faster and more robust response upon re-exposure to a specific Ag.
What are the characteristics of innate immunity system in terms of Ag-receptors, specificity, and memory?
Uses pattern recognition receptors (PRRs) to detect conserved molecular patterns on pathogens.
Shows limited specificity as PRRs recognize common patterns shared by various pathogens.
Lacks immunological memory, resulting in a similar response to subsequent encounters with the same Ag.
What is Humoral adaptive immunity?
is a branch of the immune system that involves the production of antibodies to fight against pathogens. It is mediated by B cells, which are responsible for producing antibodies.
What is IgG? And its main function?
a type of antibody, that is the most abundant antibody in the bloodstream. It plays a crucial role in providing long-term immunity against infections. It is produced by plasma cells, which are differentiated B cells.
What is Cell-mediated adaptive immunity? What role do Tc and Th play?
is a branch of the immune system that involves the activation of T cells to fight against specific pathogens. T cells:
Cytotoxic T cells: Destroy infected or abnormal cells with toxic substances.
Helper T cells: Coordinate immune response by releasing chemical messengers and activating other immune cells.
What split-products of complement is chemotactic for neutrophils?
C5a
What component is an essential part of the adaptive humoral immune response?
Immunoglobulins such as IgG
List the blood types
A, B, AB, O
Each type is determined by the presence or absence of specific antigens on red blood cells.
What blood type is the universal recipient?
AB
What is the universal donor?
O
What is an allograft? And what happens when it is rejected?
Donor and recipient are genetically different members of the same species. When the immune system of the recipient attacks and rejects a transplanted tissue or organ from a different individual.
What is an Isograft?
a type of graft where the donor and recipient are genetically identical, such as in the case of identical twins. Generally accepted well.
What is a Xenograft?
a surgical procedure where tissue or organs are transplanted from one species to another. eg. Pig’s heart to human, strong rejection
What are acute rejections?
Severe immune responses after organ transplant. They occur when the recipient's immune system attacks the transplanted organ as foreign.
what is a Chronic Rejection?
A long-term immune response in which the body's immune system gradually damages a transplanted organ, leading to its dysfunction or failure.
takes months or years, cells deposited in the blood vessel wall; delayed type hypersensitivity, kidney transplant rejection
What is Hyperacute rejection?
a rapid and severe rejection of an organ transplant caused by pre-existing antibodies in the recipient. It happens shortly after transplantation, leading to blood vessel clotting and organ failure. The transplant must be removed immediately.
What is GvHR? (Graft-versus-Host Reaction)
a complication of organ or stem cell transplantation. It occurs when the transplanted immune cells attack the recipient's tissues, causing inflammation and damage.
Bone marrow → leukemia patient
What is the acute phase of inflammation test?
A test that measures a protein in the blood associated with inflammation.
Serum CRP level
What is hematopoiesis?
Process of blood cell formation in the body, occurring in the bone marrow. Making of WBCs
What are the Primary Lymphoid tissues?
Thymus and Bone marrow
What are the Secondary lymphoid tissues?
Spleen and Lymph Nodes
What does the Lysozyme do?
It is an enzyme in body fluids, that breaks down beta glycosidic bonds in bacterial cell walls.
What MHC complex does CD4 (Th) cells have?
MHC II
What MHC complex does CD8 (Tc) cells have?
MHC I
What cells produce IFN-a, β ?
Macrophages for antiviral purposes
What cell produces IFN-γ ?
T cells
What cells are examples of phagocytes?
Macrophages and neutrophils
What is hereditary angioedema?
Rare genetic disorder causing sudden swelling in body parts like face, hands, feet, and airway. Caused by low levels or dysfunctional C1 esterase inhibitor protein.
What is Acquired angioedema?
a rare condition that causes sudden swelling of the skin, mucous membranes, and internal organs due to low levels of C1 esterase inhibitor auto-Ab. It is not hereditary and can occur later in life.
What cell produces immunoglobulins?
Plasma cells (from B cells)
What are the characteristics of T-dependent antigens?
Peptides only
Only antigens for T cells
Class-switching of Antibodies
Memory B cells
Require APC
What are the characteristics of T-Independent antigens?
Recognized by B cell
W/out APC
Include carbohydrate, DNA, RNA, LPS etc.
No memory
No T cell recognition
What is the function of IgA?
Breast feeding; Secretory protection/mucosal immunity; dimer secreted
What is the function of IgE?
Antiparasitic; Type I hypersensitivity
What is the function of IgG?
Opsonin;
neonatal immunity;
feedback inhibition;
IgG-Ag complex activates C protein
ADCC
Clearance of encapsulated bacteria in the spleen by Ab-mediated phagocytosis
What is the function of IgM?
B-cell Receptor; complement activation; pentameric, indicates acute infection
What is the function of IgD?
B cell receptor
What is the structure of an Antibody (Ab)?
2 H chains; 2 L chains
Variable domain (V); Constant domains ©
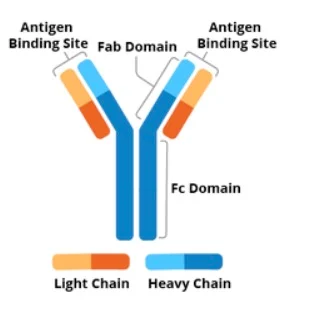
What are some characteristics of an antibody?
Papain digest →Fab + Fc
CH determines Class Ig A, D, E, G and M
CH binds FcR on some WBCs such NK, macrophage
V domains of both the H & L chains, in Fab, form Ag binding site
Random combinations of V, D, and J gene segments determine Ab diversity
What are characteristics of a monoclonal Ab?
secreted by a single clone
produced in hybridoma
has the same affinity
no avidity
Produced by a single clone of B cells. Highly specific for a single epitope. Homogeneous population of antibodies. Consistent in structure and function. Can be generated in large quantities.
What are characteristics of a polyclonal Ab?
Produced by different B cells
Recognizes multiple epitopes
Heterogeneous in structure
Higher chance of cross-reactivity
Greater variability in affinity and specificity
How does Ab affinity maturation work?
strengthens antibody binding through mutations and selection. B cells produce diverse antibody variants. High-affinity antibodies are selected and proliferated, improving immune response efficiency.
Mutations in Ab’s variable regions of L- and H-chains
What are characteristics of MHC I?
Alpha chain has 5 domains
β-2m on cell surface; non-covalent; not in HLA locus
Cleft between α1 and α2 binds the presented peptide
Found On all nucleated cells
Presents to CD8+ cells
Tc recognize viral peptide, MHC-I on surface of infected cell and kill it
Direct effector function
Tc are MHC I restricted
Alpha MHC-I coding region: HLA-A, HLA-B and HLA-C
What are characteristics of MHC II?
Alpha chain has 4 domains
Has Beta chain with 4 domains
On professional APC
Presents to CD4+ cells
TH recognize peptide, MHC-II on surface of APC and get activated
CD4+ T cell has indirect cell mediated effector function by activating macrophage
TH are MHC II restricted
α & β MHC-II coding region: HLA-D [DN, DO, DP, DQ & DR]
TH1 cells secrete IFNγ → Activate macrophage → MΦ kill ingested microbes
TH2 cells secrete IL-4 → Activate B cell → Ab production & class switching
TH2→Release IL-10→inhibits TH1 production of IFNγ/→No IFNγ→inhibit MΦ
What is MHC Codominant inheritance?
MHC diversity in the individual → increased presenting to T cells
What is MHC Polymorphic inheritance?
MHC diversity within population → increased populations recognition of Ags
Compare Ab and TCRs
Both as membrane receptors
Both- specific
Ab has effector function→ Performed by the Fc region of H chain
TCR- no effector function
Ab recognize; proteins, polysaccharides and lipids, linear and 3-dimensional configuration conformational epitope
TCR recognition: Complex, Linear epitope, Peptides only, Pep. Must be presented by APC, With appropriate MHC: I to CD8 , II to CD4
TCR signaling require the cross-linking of two receptors (TCR & CD4 or 8)
How do microbes evade humoral immunity?
Antigenic variation → influenza virus, HIV, E.coli, Neisseria gonorrhoeae
Inhibition of complement system activation → many bacteria
Resistance of phagocytosis → encapsulated bacteria, Streptococcus pneumoniae, Haemophilus influenzae
What bacteria causes Leprosy and what are the two forms?
Mycobacterium leprae
Tuberculoid leprosy- mild → TH1 and cell-mediated immunity intact
Lepromatous leprosy- severe → TH1 deficiency → cell-mediated immunity deficient
How do microbes evaded cell-mediated immunity?
Inhibition of phagosome-lysosome fusion→ mycobacterium tuberculosis
Inhibition of Ag presentation → HSV peptide interference with TAP transporter, Inhibition of proteasomal activity (CMV, EBV), removal of MHC 1 from ER (CMV)
IL-10 production → inhibition of MΦ activation (EBV)
Inhibition of effector cell activation by→ soluble cytokine receptor (Pox virus)
What are the different types of vaccines?
Conjugate vaccine → Haemophilus influenzae type B
Live attenuated virus → Sabin polio vaccine
Subunit (antigen) vaccine → Tetanus toxoid, Diphtheria
Synthetic vaccine →Hepatitis recombinant
Killed bacteria → BCG for TB
What is Type 1 hypersensitivity?
Involves IgE and mast cells mostly, bee, wasp stings, hay fever, penicillin allergy (drug or byproduct acts as hapten, binds protein becomes immunogenic; treated by acute desensitization)
What is Type 2 hypersensitivity?
Involves IgG or M against self Ag. activates complement, inflammation (Graves disease- Ab to TSH receptor → thyroid activation; Myasthenia gravis: Ab to Acetylcholine receptor inhibits muscle tone; Transient MG because IgG crosses the placenta to the fetus) Rheumatic fever
What is type 3 hypersensitivity?
Uses Immune complex with Abs other than IgG
What is congenital immunodeficiency?
A genetic condition where the immune system is impaired from birth, leading to increased susceptibility to infections.
a. adenosine deaminase (ADA);
b. Autosomal SCID
c. X-linked SCID
d. Prevention of B cell and T cell maturation
e. Chronic granulomatous disease, phagocyte defect
What is Acquired Immunodeficiency?
A weakened immune system caused by HIV, leading to increased vulnerability to infections and diseases. If untreated, it progresses to AIDS.
What is Type 4 hypersensitivity?
Tc, Th-macrophage, cytokine mediated
poison ivy- hapten
Contact allergy
What are tolerogens?
Tolerogens are substances that induce immune tolerance, preventing an immune response. They promote the development of regulatory T cells, which suppress the activation of immune cells.
What are some cancer markers?
CEA/ colon cancer marker
CALLA
Alpha-fetoprotein/ hepatocellular carcinoma
PSA/prostate
GM1 monosialoganglioside/pancreatic carcinoma
How does cancer evade the immune system?
Cancer evades the immune system by downregulating immune cell activation and producing inhibitory molecules. Genetic mutations help cancer cells avoid detection and resist immune-mediated cell death. These strategies allow cancer cells to grow and spread unchecked.