Unit 5 - Neuro and Pediatrics Floors
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
Common Neurological Diagnoses Seen in Acute Care
Traumatic Brain Injury (TBI)
Cerebrovascular Accident (CVA/Stroke)
Spinal Cord Injury (SCI)
Multiple Sclerosis (MS)
Parkinson’s Disease (PD)
Wide spectrum of presentation and recovery potential
Traumatic Brain Injury (TBI) Overview
Common causes: motor vehicle accidents (51%), falls (27%)
Severity: Mild, Moderate (GCS 9–12), Severe (GCS 3–8)
Traumatic Brain Injury (TBI) Overview
Mild TBI (Concussion)
Physical: Headaches, nausea, vomiting, dizziness, balance problems, fatigue
Cognitive: Confusion, difficulty concentrating, memory problems, delayed processing
Emotional: Irritability, anxiety, depression, mood swings
Traumatic Brain Injury (TBI) Overview
Moderate to Severe TBI
Physical: Persistent headaches, repeated vomiting, seizures, loss of coordination, slurred speech, numbness or tingling, weakness
Cognitive: Confusion, disorientation, impaired memory, problem-solving, and abstract thinking
Emotional: Personality changes, disinhibition, apathy, aggression, agitation
Other: Loss of consciousness, impaired vision
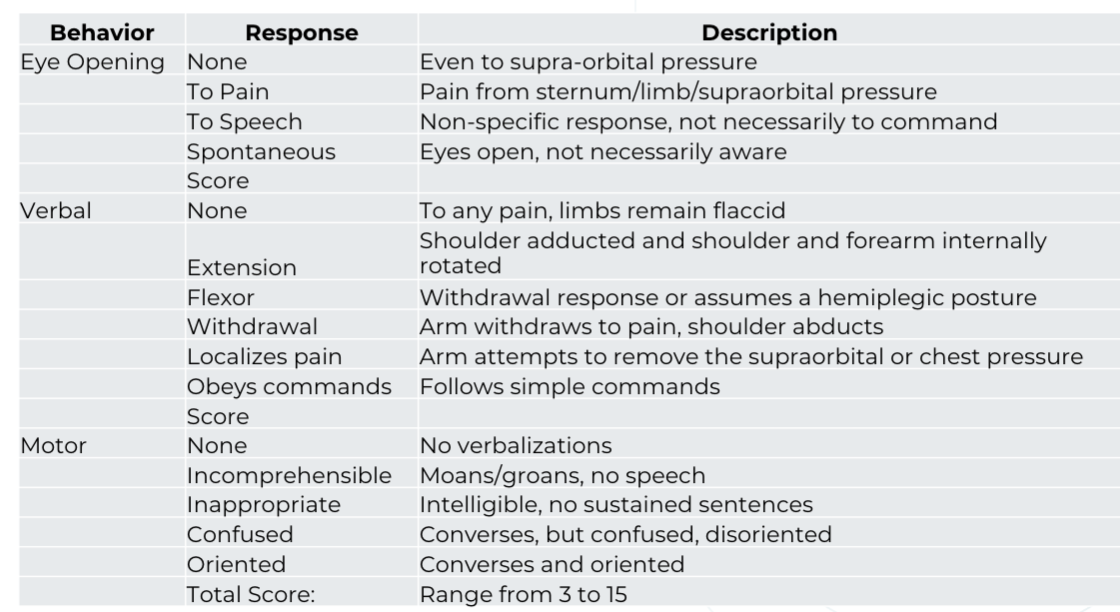
Glasgow Coma Scale
TBI: Key Considerations
Improve physical function, prevent contractures, improve respiratory function
Hypertonus:
Contributes to contractures
Worsened by immobility and poor positioning
Muscle Weakness: More severe in patients with severe TBI
hormonal disturbances
hypercatabolism
Physical Inactivity: extreme in acute care. Increases risk for chronic diseases (e.g., diabetes, heart disease). Adults ≥45 at higher risk
TBI: Key Considerations
Disorders of Consciousness (DOCs)
Continuum: Coma → Vegetative State (VS) → Minimally Conscious State (MCS)
Persistent vs Permanent:
Persistent >1 month
Permanent after 3 months (non-trauma) or 12 months (trauma)
MCS: Inconsistent awareness; requires careful, repeated assessment
Emergence: Functional communication or object use
Agitation common in early stages due to disorientation
Prevalence of spasticity in patients with DOCs ranged from 59% - 89%
Spinal Cord Injury (SCI) Overview
Common causes: motor vehicle accidents (MVA) (38%), falls (32%)
Deficits: Sensory, motor, autonomic
Types:
Incomplete or complete
Paraplegia: Lower trunk/legs
Tetraplegia: All four limbs + trunk
Assessment: AISA Levels A–D
Spinal Cord Injury (SCI) Overview
ASIA A
Complete
no sensory or motor function is preserved in S4-S5
Spinal Cord Injury (SCI) Overview
ASIA B
incomplete
the preservation of sensory function without motor function below the neurological level and includes S4-S5
Spinal Cord Injury (SCI) Overview
ASIA C
incomplete
the preservation of motor function below the neurologic level. muscle function of more than half key muscles below this level is less than 3/5
Spinal Cord Injury (SCI) Overview
ASIA D
incomplete
the preservation of motor function below the neurologic level. muscle function of at least half of key muscles below this level is equal to or greater than 3/5
Spinal Cord Injury (SCI) Overview
ASIA E
normal
muscle and sensory function are intact
Spinal Cord Injury (SCI) Overview
C4 lesion: Expected level of function
spontaneous breathing
Spinal Cord Injury (SCI) Overview
C5 lesion: Expected level of function
elbow flexion
Spinal Cord Injury (SCI) Overview
C6 lesion: Expected level of function
wrist extension
Spinal Cord Injury (SCI) Overview
C7 lesion: Expected level of function
elbow extension
Spinal Cord Injury (SCI) Overview
C8-T1 lesion: Expected level of function
finger flexion
Spinal Cord Injury (SCI) Overview
T1-T12 lesion: Expected level of function
intercostal and abdominal muscles — trunk control
Spinal Cord Injury (SCI) Overview
L1-L2 lesion: Expected level of function
hip flexion
Spinal Cord Injury (SCI) Overview
L3 lesion: Expected level of function
knee extension
Spinal Cord Injury (SCI) Overview
L4 lesion: Expected level of function
ankle DF
Spinal Cord Injury (SCI) Overview
L5 lesion: Expected level of function
toe extension
Spinal Cord Injury (SCI) Overview
S1-S2 lesion: Expected level of function
ankle PF
Spinal Cord Injury (SCI) Overview
S2-S4 lesion: Expected level of function
rectal sphincter tone
SCI: Key Considerations
Recent Injury
Spinal protection: brace, halo, body jacket, internal fixation
Avoid pulling on LE; logroll for turning
SCI: Key Considerations
Chronic Injury
Risk of osteoporosis in vertebrae & long bones
Even mild strain may cause fracture (e.g., during transfers)
SCI: Key Considerations
Positional Syncope
Watch for fainting when moving from supine to sitting due to BP changes
SCI: Key Considerations
Above T6 Injuries
Impaired sympathetic response
↓ HR response, blood pooling, ↓ vasoconstriction
Monitor for orthostatic hypotension (SBP ↓ ≥20 mmHg, DBP ↓ ≥10 mmHg)
SCI: Key Considerations
Autonomic Dysreflexia (AD)
Triggered by noxious stimuli (e.g., bladder/bowel distention)
Signs: ↑ BP (>20 mmHg above baseline), ↓ HR, headache, flushing, sweating
Risks: Retinal/cerebral hemorrhage, MI, CHF, death
Management: Immediate stimulus removal, BP/HR monitoring, medication based on HR
Stroke: Key Considerations
Unilateral Neglect:
Impairs balance & weight shift; ↑ rehab LOS, ↓ FIM/GG scores at DC
Strong predictor of poor outcomes and fall risk
Stroke: Key Considerations
Therapeutic Strategies
Constraint-induced movement therapy (CIMT) improves UE function with some wrist/finger movement
Corticospinal integrity = key for hand dexterity recovery
Stroke: Key Considerations
Rehabilitation Impact
Inpatient rehab reduces LOS and improves function
Specialized IRF stroke rehab linked to greater independence, survival
Stroke: Key Considerations
Prognosis
Ischemic stroke = slower functional gains vs. hemorrhagic
Walking speed = strongest predictor of community ambulation
Fall risk: 73% incidence in mild/moderate stroke within 6 months
Stroke: Key Considerations
Poor Prognostic Indicators for Independent Living (1-year post-stroke)
Advanced age, female gender, non-lacunar stroke
Hemiparesis, prior hemiplegia, homonymous hemianopia
Incontinence, low ADL function, decreased consciousness
Visual/spatial deficits, no stroke unit transfer
Stroke: Key Considerations
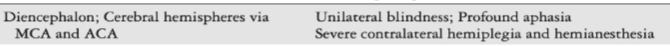
Internal carotid
Stroke: Key Considerations
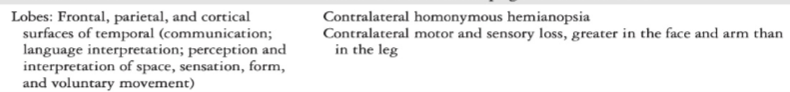
Middle cerebral artery
Stroke: Key Considerations
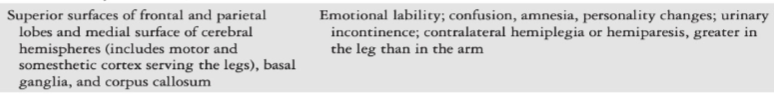
Anterior cerebral artery
Stroke: Key Considerations
Posterior cerebral artery
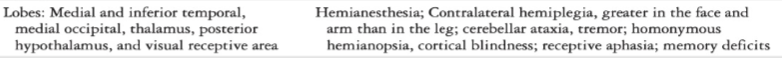
Stroke: Key Considerations
Vertebral or basilar artery
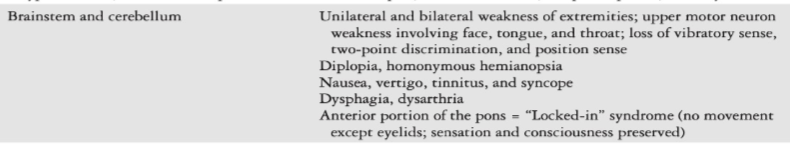
Stroke: Key Considerations
Posterior inferior cerebellar artery
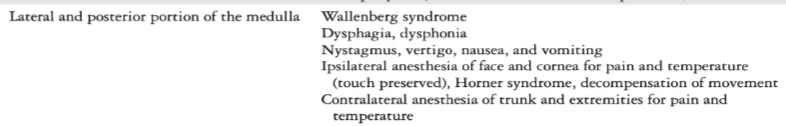
Stroke: Key Considerations
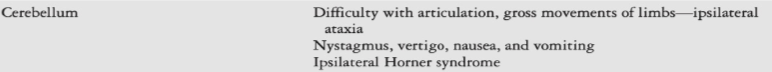
Anterior inferior and superior cerebellar arteries
Parkinsonism Overview
Idiopathic
slow, progressive, basal ganglia disorder
Parkinsonism Overview
Secondary
from tumors, infections, or medications (e.g. certain antipsychotics)
Parkinsonism Overview
Medication
Sinemet (dopamine agonist): Levodopa/Carbidopa
“On-off” effect → fluctuation in motor and non-motor symptoms.
Time sessions after meds
Dyskinesias may occur at peak dose
Parkinsonism Overview
Balance
Comprehensive balance assessment is essential
Movement initiation delays and postural rigidity impair protective extension
PD: Key Considerations
Motor symptoms
Resting tremor, bradykinesia, rigidity, postural instability
Freezing episodes, shuffling/festinating gait, stooped posture
Arm swing, masked facial expression,
Dysarthria/dysphagia
PD: Key Considerations
Non-motor symptoms
Fatigue, depression, cognitive decline
Autonomic/GI/cardiopulmonary involvement
PD: Key Considerations
Fall risk
Impaired protective reactions & delayed movement initiation
Balance assessment is critical in acute care
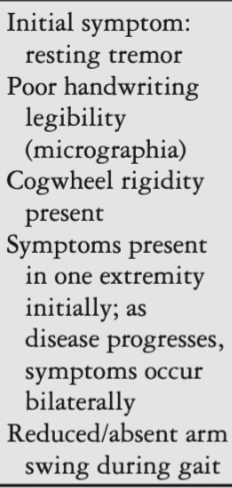
PD
Early to mid-stage
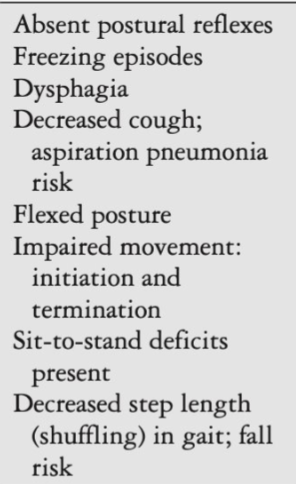
PD
late or advanced-stage
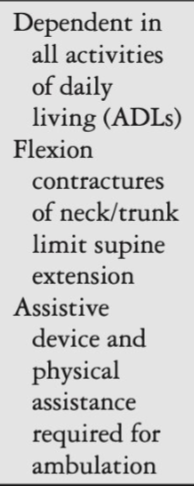
PD
end-stage
Multiple Sclerosis (MS) Overview
Autoimmune CNS disorder, most common demyelinating disease
Multiple Sclerosis (MS) Overview
Relapsing-remitting
Exacerbations with recovery
Multiple Sclerosis (MS) Overview
Secondary progressive
Starts RR, becomes progressive
Multiple Sclerosis (MS) Overview
Progressive relapsing
Flare-ups with lasting deficits
Multiple Sclerosis (MS) Overview
Primary progressive
Continuous decline from onset
Multiple Sclerosis: Key Considerations
Common Symptoms
Fatigue (reported by >80%)
Optic neuritis → visual changes often first sign
Sensorimotor, balance, and coordination deficits
Multiple Sclerosis: Key Considerations
PT Implications
Monitor for fatigue, vision issues, coordination changes
Symptom fluctuation with disease course → adjust interventions accordingly
Types of Tone: Review
Hypotonia
Seen in: CP, SCI, MS, muscular dystrophy
Types of Tone: Review
Spasticity
Seen in: Stroke, SCI, MS
Types of Tone: Review
Dystonia
Seen in: CP, stroke, TBI, brain tumors, encephalitis, medications
Types of Tone: Review
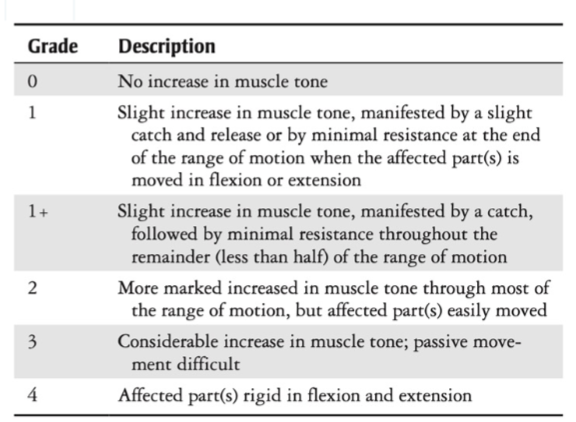
Rigidity
Types: Lead pipe or cogwheel
Seen in: PD
Common Tone Patterns: Review
Decorticate Posturing

Common Tone Patterns: Review
Decerebrate Posturing

Tone Assessment
Tone Management
Slow, controlled movements
Weight-bearing activities
Modalities (if available): NMES, cold/heat
Positioning to inhibit tone
Medications
Interventions for Tone Management
Hypertonia
NMES, weight-bearing activities, positioning, orthotics, mirror therapy
Interventions for Tone Management
Spasticity
NMES, casting + pharmacology
Interventions for Tone Management
Rigidity
NMES, exercise
Interventions for Tone Management
Research
serial casting versus thirty (30) minutes of stretching
Early Mobility
Benefits
Reduced length of stay, improved outcomes
Early Mobility
Guidelines
Begin ASAP once medically stable
Bed mobility → sitting EOB → standing/walking as tolerated
Include simple cognitive stimulation for TBI/MS
Early Mobility
Considerations for neuro populations
Fatigue (MS/PD)
Motor planning deficits (CVA)
Orthostatic hypotension (SCI)
Common Pediatric Diagnoses in Acute Care
Congenital conditions (present at birth): CP, Congenital Muscular Torticollis (CMT), Spina Bifida, congenital heart defects
Genetic conditions (caused by DNA mutation(s)): Duchenne Muscular Dystrophy (DMD), Spinal Muscular Atrophy (SMA), Osteogenesis Imperfecta (OI), Rett Syndrome, Fragile X Syndrome, Down Syndrome
Acquired conditions: TBI, SCI, burns, orthopedic injuries
Acute illnesses: cancer, infections, respiratory conditions/distress (e.g. Cystic Fibrosis (CF) exacerbations, pneumonia)
Post-surgical: trauma, non-traumatic orthopedic surgeries (posterior spinal fusion, pectus excavatum), thoracic/abdominal, neurological, cardiac, amputations
Pediatric Prognostic Factors
Age at time of injury/diagnosis
Severity and location of injury
Prior function and developmental status
Family support and resources
Access to early intervention, prior physical therapy and/or specialized care
Pediatric Evaluation in Acute Care
Focus on safety and function: bed mobility, transfers, ambulation
Developmentally appropriate assessment methods and standardized tools
General: PEDI, AM-PAC "6-Clicks" (peds version)
Neurological function:
TBI: Pediatric Rancho Level of Cognitive Functioning Scale and Pediatric Rancho LOC
SCI: ASIA
Developmental Assessments: PDMS-2/PDMS-3, GMFM-66 or GMFM-88
NICU (many require training): TIMP, HINE, GMA
Need for equipment? Assistive Technology?
Pediatric Frequency and Dosage in Acute Care Setting
Consult
1-2 visits total
Chronic impairments and developmental delays
Little to no risk for loss of skills
Need referral to next level of care or community resources
Pediatric Frequency and Dosage in Acute Care Setting
Occasional
1-2x/wk
A potential for weekly/monthly progress toward functional goals
At risk for loss of skills for prolonged hospitalization
Currently receiving early intervention therapy services or needs referral
Pediatric Frequency and Dosage in Acute Care Setting
Regular
3-4x/wk
New impairments and functional limitations
Potential for daily/weekly progress toward functional goals
Currently receiving therapy services, or likely to be referred to outpatient
Pediatric Frequency and Dosage in Acute Care Setting
Frequent
5x/wk
Acute loss of functional skills due to injury or illness
Good to excellent potential for daily progress
High risk for deconditioning without skilled PT
Potential referral to inpatient rehab or high-frequency outpatient
Pediatric Frequency and Dosage in Acute Care Setting
Intense
>6x/wk
Acute loss of functional skills due to injury or illness
Excellent potential for daily progress or at high risk for loss of function with a lower frequency
Potential referral to inpatient rehab or high-frequency outpatient
Safety Considerations in Pediatric Acute Care
Medical & Environmental Awareness
Know your lines: IVs, NG/G-tubes, O2, EVDs, telemetry
Monitor alarms before mobilizing
Observe for clutter, fall risks, and safe transfer space
Safety Considerations in Pediatric Acute Care
Physiological Awareness
Review most recent vitals (age-appropriate norms)
Watch HR, RR, BP, SpO₂ during activity
Stop if: ↓SpO₂, arrhythmia, mental status change, vomiting, increased distress
Safety Considerations in Pediatric Acute Care
Developmental & Behavioral Cues
Adjust expectations by age and development
Use child-friendly language and play-based approaches
Partner with caregivers for comfort and support
Safety Considerations in Pediatric Acute Care
Interprofessional Check-ins
Confirm orders: activity level, bedrest status
Clarify precautions after procedures or med changes
Collaborate with RN/MD if unsure about safety
Pediatric Early Rehab Strategies
Prevent contractures
Early mobility
Chest physiotherapy when indicated
Promoting participating in daily activities
Sensory stimulation and play-based interventions
Family involvement positioning: promote alignment, from day one
Pediatric Long-Term Rehab Planning
Continuum of care: transition from acute care to inpatient rehab, home, or outpatient/early intervention
Goal setting: short-term functional goals, long-term developmental milestones
School re-integration and adaptive strategies
Ongoing team communication and care coordination
Family and Caregivers: Pediatrics
Diagnosis and expected outcomes
Family-centered care
Family and caregiver involvement in therapy sessions
Safe handling and mobility techniques
Equipment training (braces, walkers, wheelchairs)
Signs of complications or regression
Home exercises and strategies for ongoing support
Neuro
Why Discharge Planning Matters
patients are very high-risk:
Readmission
Falls
Functional decline
Unpredictable hospital course
Discharge decisions impact long-term function and quality of life
Planning starts at day 1 of admission
Neuro
Key Discharge Considerations
Neurological Diagnosis & Prognosis
Each condition (CVA, TBI, SCI, MS, PD) has a unique recovery trajectory
Neuro
Key Discharge Considerations
Current Functional Status
Mobility (e.g., transfers, gait)
Cognition and communication abilities
Continence and overall ADL performance
Neuro
Key Discharge Considerations
Support System
Availability of caregivers
Home setup and accessibility
Transportation and community support
Neuro
Key Discharge Considerations
Medical Complexity
Comorbidities and medication management
Presence of feeding tubes, seizures, tracheostomy, or ventilators
Anticipated medical needs post-discharge
Discharge: Stroke
Admission to inpatient rehab influenced by age, incontinence, living situation, and insurance coverage
44.9% discharged to community; 55.1% to institutional care
Community-discharged patients:
Younger, still working
Less dysphagia/tube feeding,
Shorter time from onset to rehab, less severe deficits
Greater and faster functional gains during stay
Early mobilization predicts favorable outcomes
Discharge: TBI
Longer time to rehab is associated with greater disability
Longer rehab LOS linked with:
Tracheostomy at admission
Transfers due to complications
Infection
Seizure
Respiratory needs
Neuro changes
Discharge: MS
Predictors of rehab success:
Relapsing-remitting course
Shorter disease duration
Less severe baseline impairments including balance
Balance impairment = negative predictor of rehab outcome
IPR improves ADL autonomy, especially in early-stage MS
Discharge: PD
Positive predictors of ADL improvement after IPR:
Younger age, high baseline ADL impairment
Strong dexterity skills and steady gait
≥3 daily mobilizations linked to:
Shorter LOS
Higher likelihood of home-to-home discharge
Neuro
Discharge Planning
Ongoing Rehabilitation Needs
Inpatient rehab, SNF, home health, outpatient
Neuro
Discharge Planning
Cognitive Screening Results
Impact on safety, independence, and follow-up care