Lecture 39 Learning disabilities and medicines management
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
What is a learning disability
Impaired Intelligence: A significantly reduced ability to understand new or complex information and to learn new skills.
Impaired Social Functioning: A reduced ability to cope independently.
Onset: Started before adulthood, with a lasting effect on development.
How do we measure IQ
Measurement
Assessed via tools like WAIS-IV. A Full Scale IQ (FSIQ) score of < 70 indicates a learning disability.
What is the prevalence of LD
Prevalence
This score falls two standard deviations below the mean, representing ~2% of the population.
In the UK, this equates to ~1.5 million people (905,000 adults).
What are some pointers of LD
Pointers: Delayed developmental milestones, special schooling, needing support with daily living activities (ADLs), and significant communication difficulties.
What is the cause of LD
Antenatal
Perinatal
Perinatal
Aetiology (Antenatal): Any insult to the developing brain. Examples: Genetic conditions (e.g., Down Syndrome), congenital infections, or teratogens.
Aetiology (Perinatal): Events around birth. Examples: Birth asphyxia/hypoxia, severe prematurity.
Aetiology (Perinatal): Events around birth. Examples: Birth asphyxia/hypoxia, severe prematurity.
What are some major co-morbidities associated with LD
Epilepsy: ~40% have epilepsy (often refractory, high SUDEP risk).
Dementia: 2.5x higher dementia risk. In Down Syndrome, Alzheimer's risk is high, with onset in 40s-50s
Cardiovascular and metabolic diseases: Increased risk of heart disease, high blood pressure, and obesity, often linked to poorer diet, less exercise, and reduced access to health promotion.
Sensory impairment
Hearing/sight issue
Poor dental hygiene,
gastro-intestinal problems (GORD, dysphagia, GI cancers).
Generally describe the access to health for LD individuals
Increased rate of mortality due to poor access, most of which are avoidable
What are some causes of these preventable deaths
Communication difficulties (est. 50%).
Lack of specialist understanding.
Capacity issues.
"Diagnostic Overshadowing" (symptoms blamed on LD).
Negative perceptions / QoL judgements (e.g., DNARs).
How can we address these barriers
Annual Health Checks (AHC): For everyone >14 on the GP LD Register. A vital opportunity to review health and medication (e.g., using STOPP-START)
How can we make reasonable adjustments during appointments
Reasonable Adjustments: A legal requirement (Equality Act 2010). Examples: longer appointments, quiet/first appt, easy-read leaflets, carer input.
What is the role of LD nurses
LD Liaison Nurses: "Bridge the gap" in general hospitals. They support staff in making adjustments and navigating the Mental Capacity Act (MCA).
What is the mental capacity act 2005
designed to protect and empower people who may lack the mental capacity to make their own decisions about their care and treatment
2 stage capacity
4 point functional test
What is the 2 stage capacity test
The 2-Stage Test of Capacity
Stage 1 (Diagnostic): Is there an impairment of, or disturbance in the functioning of, the person’s mind or brain?
Stage 2 (Functional): Is the impairment sufficient that the person lacks the capacity to make that particular decision at that time?
What is the 4 point functional test
To have capacity, the person must be able to:
Understand the relevant information.
Retain the information.
Use or Weigh the information in the decision process.
Communicate their decision.
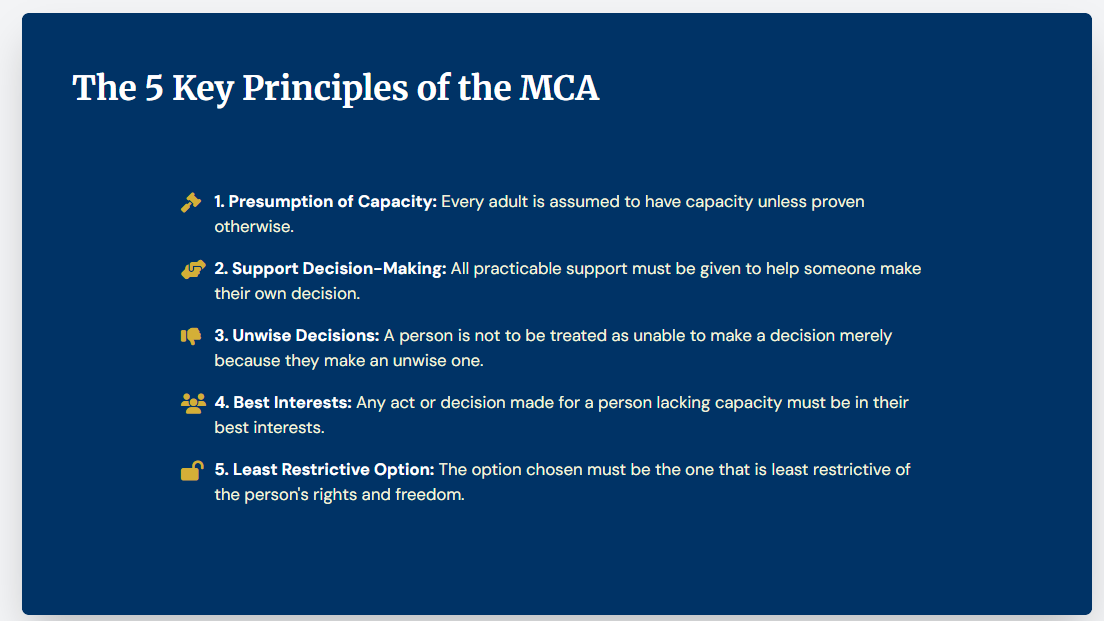
The 5 Key Principles of the MCA
1. Presumption of Capacity: Every adult is assumed to have capacity unless proven otherwise.
2. Support Decision-Making: All practicable support must be given to help someone make their own decision.
3. Unwise Decisions: A person is not to be treated as unable to make a decision merely because they make an unwise one.
4. Best Interests: Any act or decision made for a person lacking capacity must be in their best interests.
5. Least Restrictive Option: The option chosen must be the one that is least restrictive of the person's rights and freedom.
What are some hazards and side effects in prescribing for LD
Higher risk due to co-morbidities
Drug interactions e.g. antiepileptics
BBB dysfunction
Genetic differences e.g. down syndrome
Difficulty communicating side effects
Missing side effects ‘diagnostic overshadowing
How can we prevent prescribing associated side effects and hazards
Start low and go slow
Monitor for deterioration in seizure control
Mood/behaviour changes
Cognitive side effects e.g. antimuscarinics
Mobility impairment/ falls
Weight gain
Swallow difficulties use NEWT guidelines
How is PK altered in LD
Down syndrome patients have altered blood brain barrier
This leads to higher plasma concentrations of drugs e.g. Donepezil
Which leads to higher rates of adverse effects e.g. GI symptoms, altered ,mental state
Require more monitoring and caution
What is does the acronym STOMP-LD stand for
Stopping
Over
Medication of
People with learning disabilities, autism or both
What is the purpose of STOMP-LD
NHS England initiative
improves quality of life
ensures psychotropics are used for the right reason, right dose, right time
Promotes non-drug interventions
Improves shared decision making
Is there medication for the core symptoms of autism
No
These people should not be offered antipsychotic unless they are psychosocial or other interventions are insufficient
How can we treat challenging behaviour: Antipsychotics
Used at low doses if other interventions fail
Examples: Aripiprazole, risperidone
S/E: high monitoring burden of weight, ECG, blood
Aripiprazole and Fluoxetine can be used in severe CB if no effective psychosocial interventions
How can we treat challenging behaviour: Antidepressants
Trial SSRIs to treat underlying anxiety and depression, may help correct difficult behaviour
E.g.: Fluoxetine
What are some other options for LD CB
Propranolol: somatic anxiety
Naltrexone: self injury
What monitoring is involved in LD
Plan for discontinuation (if for CB).
Monitor weight, BMI, and lifestyle (antipsychotics).
Monitor bloods (U&Es for hyponatraemia with SSRIs, prolactin with Risperidone).
The use of anticonvulsants in learning disabilities
Anticonvulsants: RARE
But valproate can be used
annual risk acknowledgment form, regardless of capacity
Pregnancy prevention program
Sultiame: A red drug, initated by specialist, may not be suitable for everyone
Lacosamide: some patients experience improved cognition
ALL PATIENTS MUST BE REGULARLY REVIEWED
What is a best interests decision
People must act in your best interests before taking certain steps that affect you while you lack capacity. This includes taking certain steps relating to your care and treatment.
Considers your condition, age, wishes, circumstances
CYP inducers and inhbitors

How do we treat dementia and downsyndrome in LD
Fluoxetine and donepezil
But we have to be cautious as down syndrome patients have altered metabolism
This can lead to toxicity especially when combined with CYP inhibitor fluoxetine
Higher risk for ADV and interactions
How can we improve communication with LD
V: validation
E: emotion
R: reassurance
A: activity
Check their understanding by asking to repeat back
Take you time this can be life saving