Anatomy and Physiology II - Section 4, Lesson 1/2
1/141
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
142 Terms
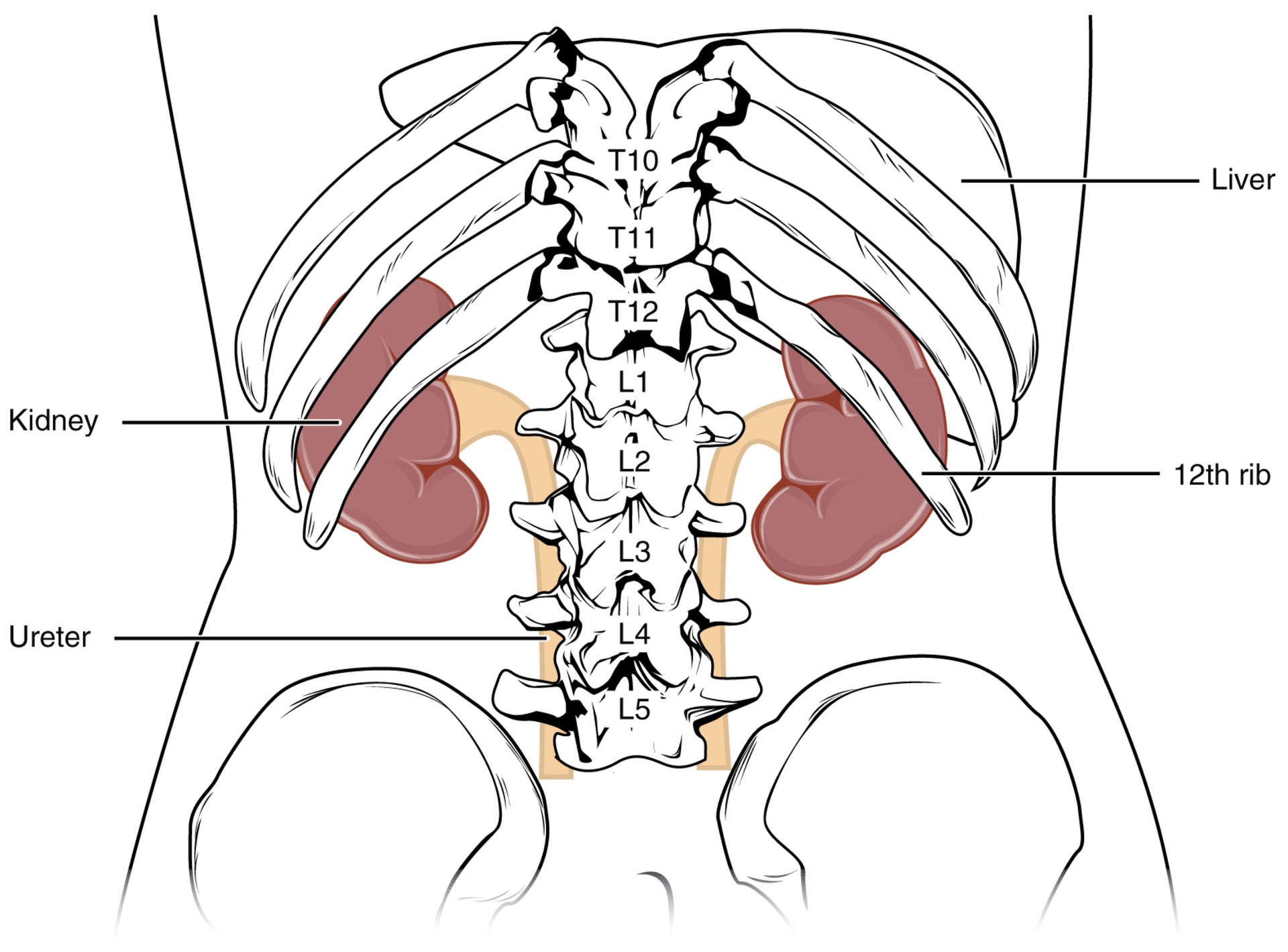
Q: Where is the left kidney located?
A: Between T12 and L3 vertebrae (right kidney is lower due to liver).
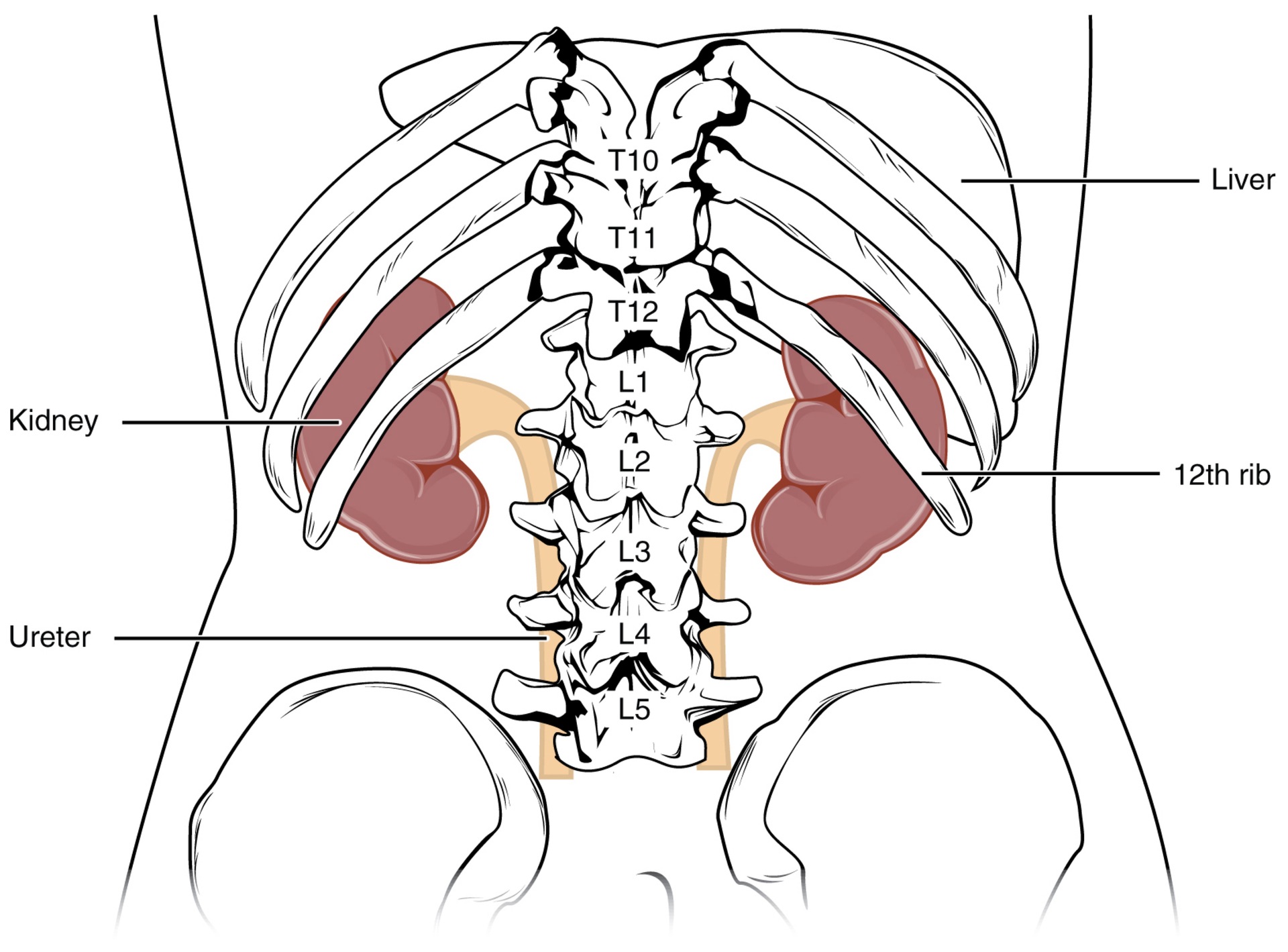
Q: What protects the upper portion of the kidneys?
A: The 11th and 12th ribs.
Q: What covers the kidneys directly?
A: A fibrous capsule made of dense, irregular connective tissue.
Q: What cushions the kidneys and anchors them in place?
A: The renal fat pad and renal fascia.
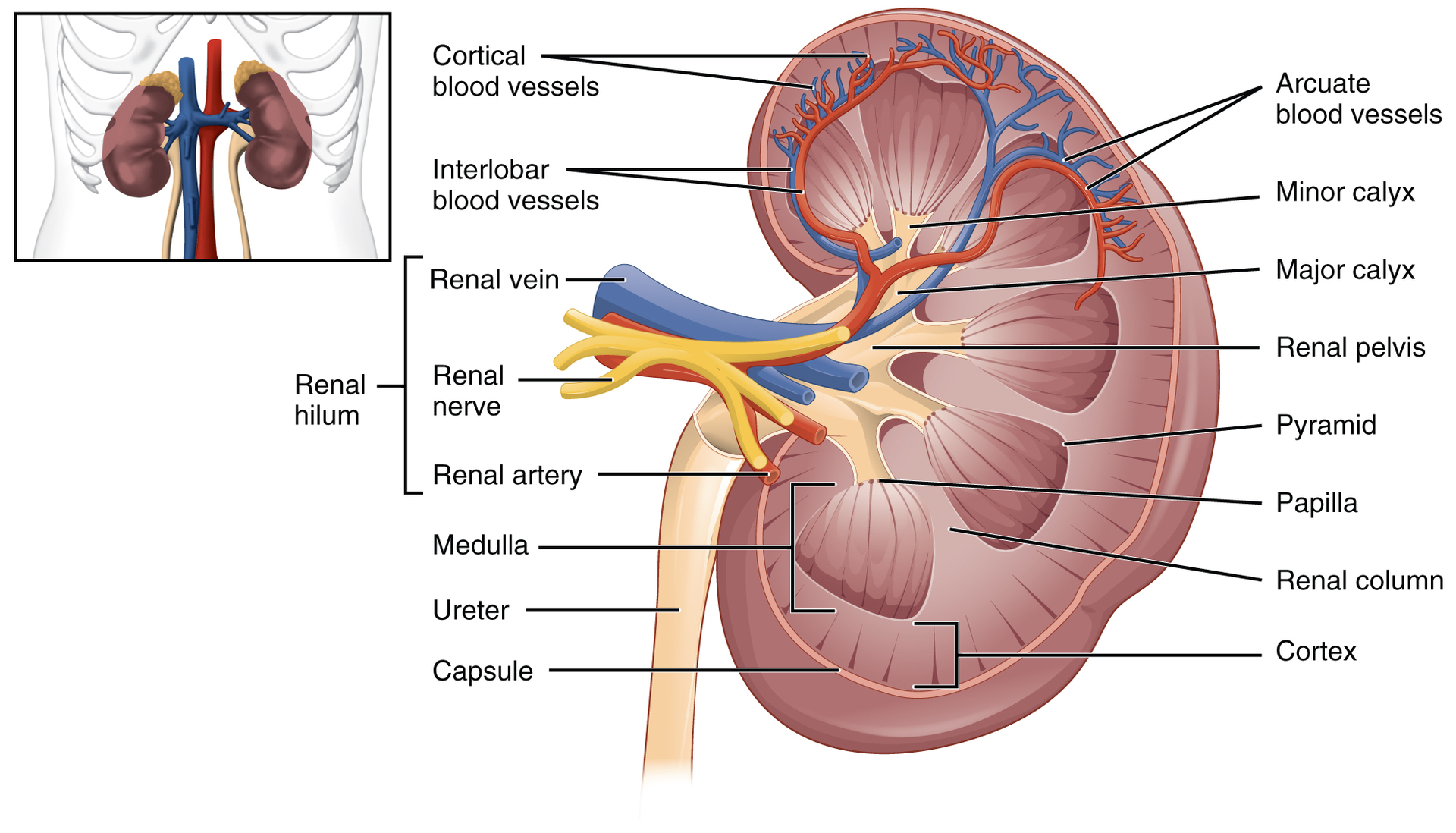
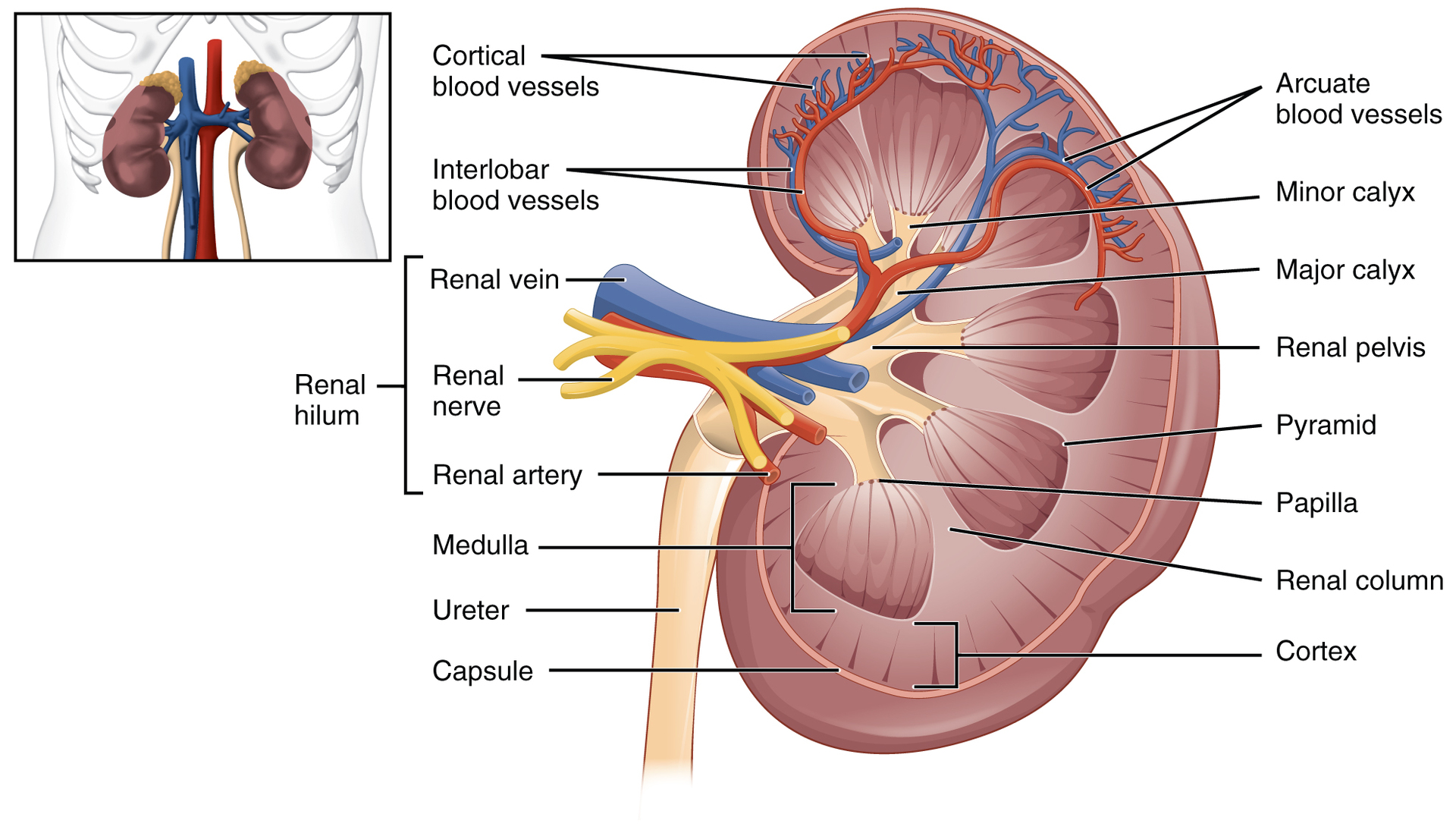
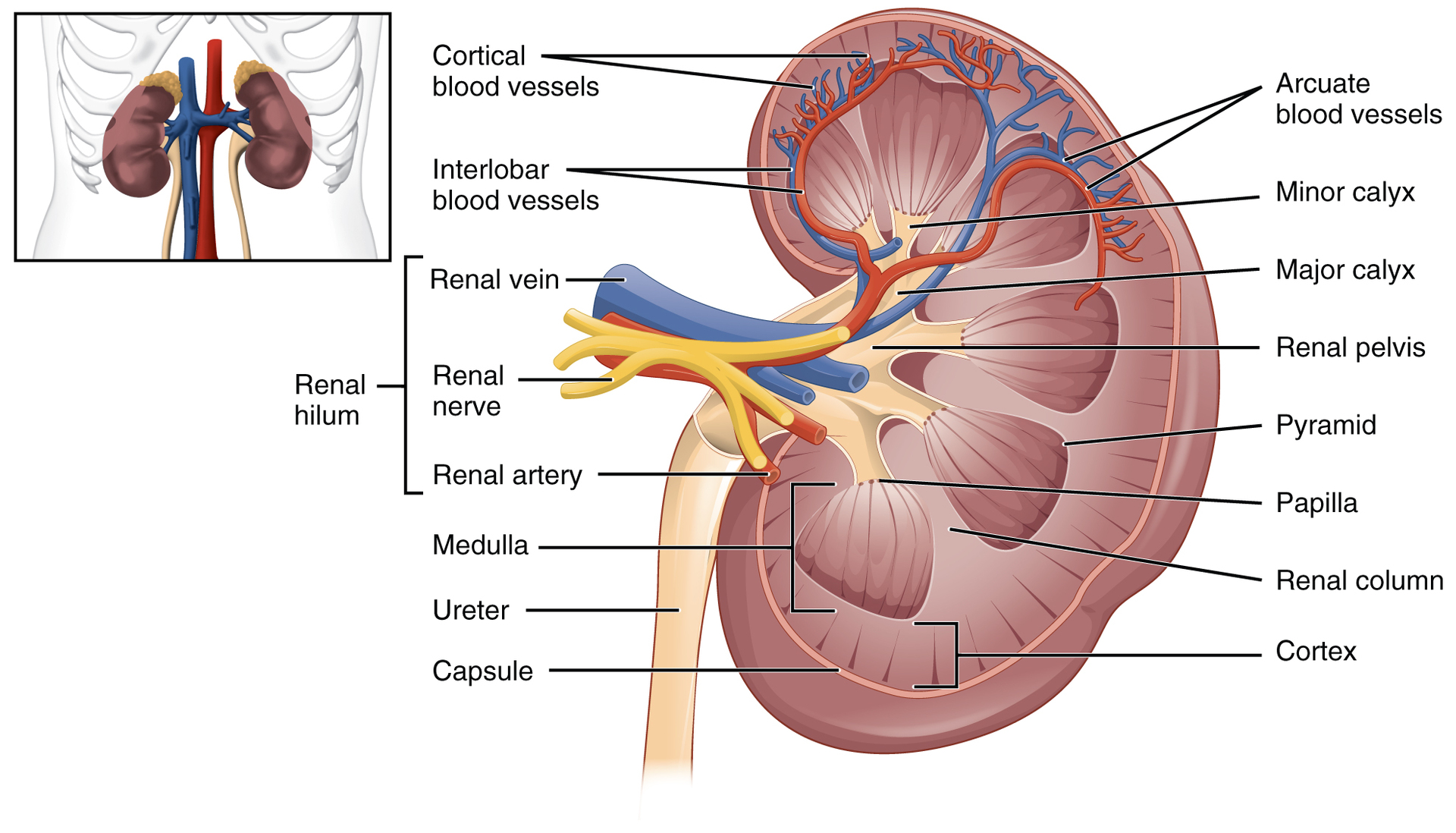
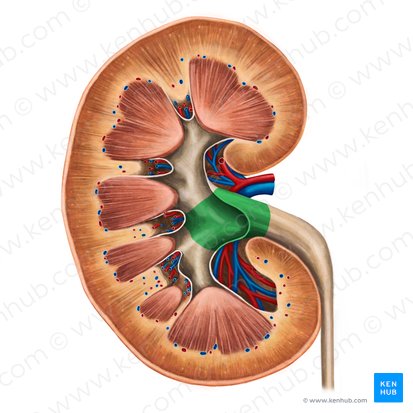
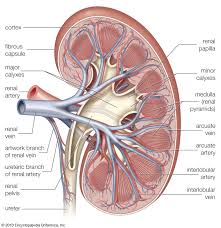
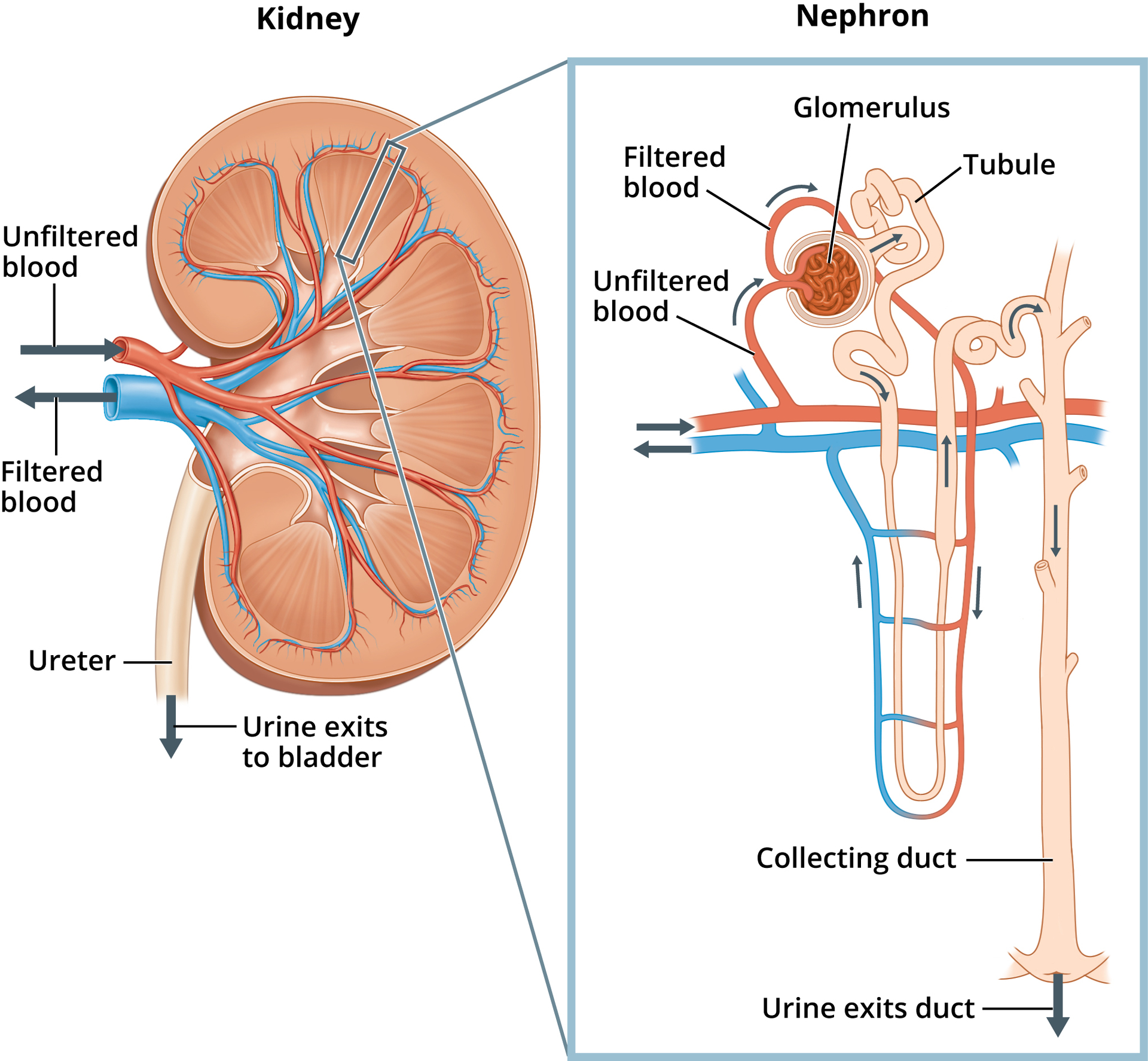
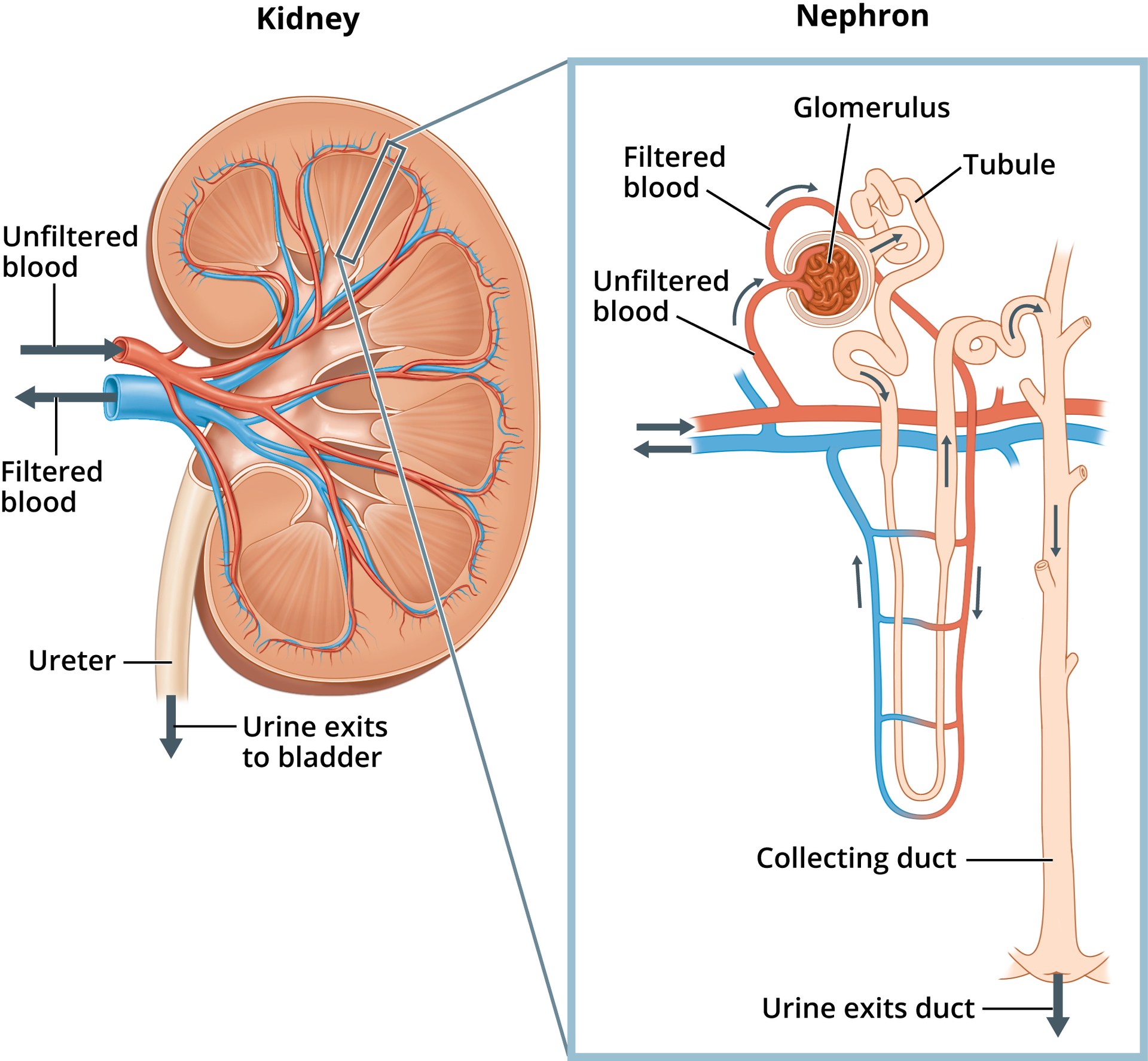
Q: What are the two main internal regions of the kidney?
A: Renal cortex (outer) and renal medulla (inner).
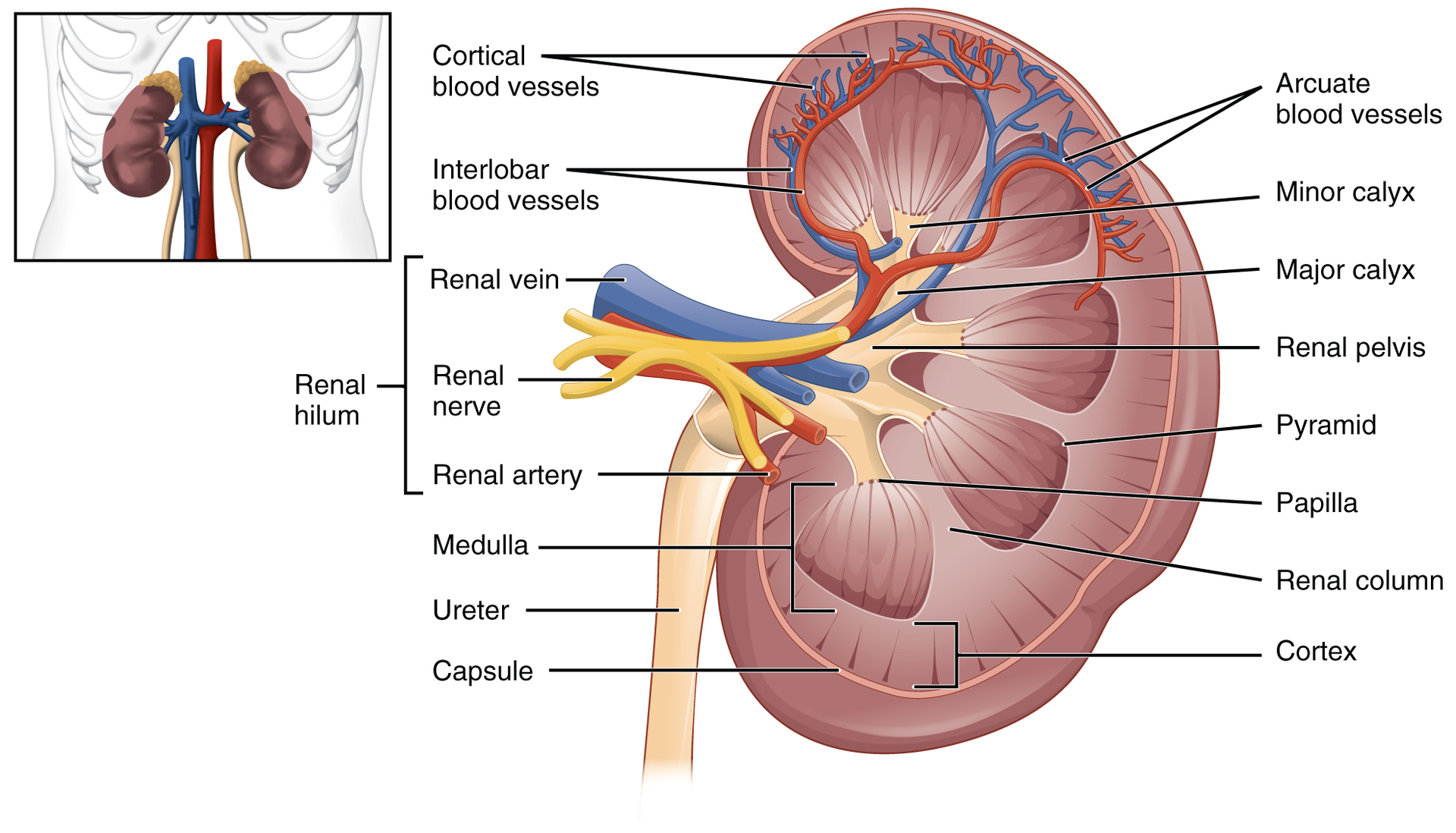
Q: What structures separate the renal pyramids in the medulla?
A: Renal columns.
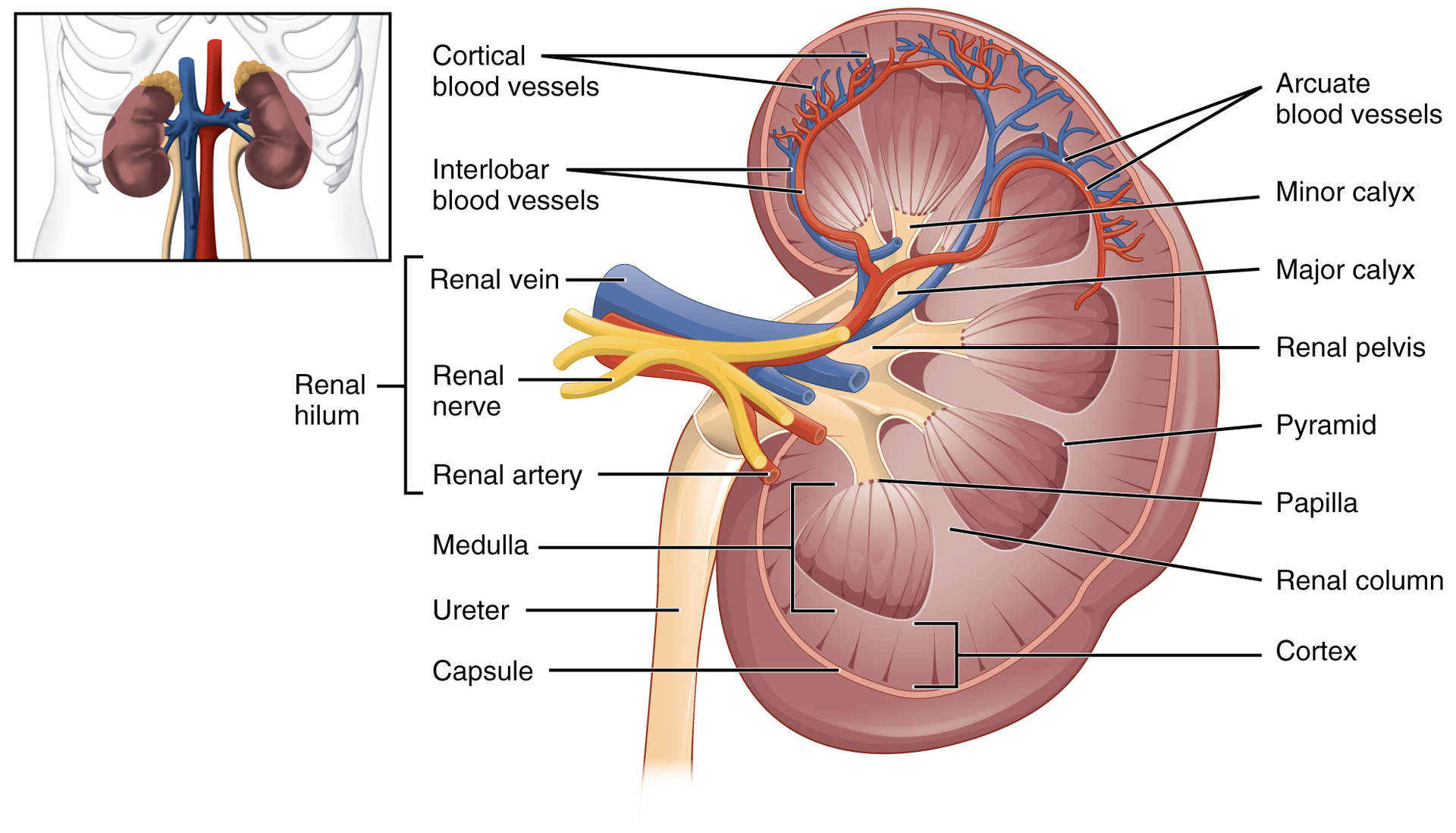
Q: What are renal papillae?
A: Bundles of collecting ducts that transport urine to the calyces.
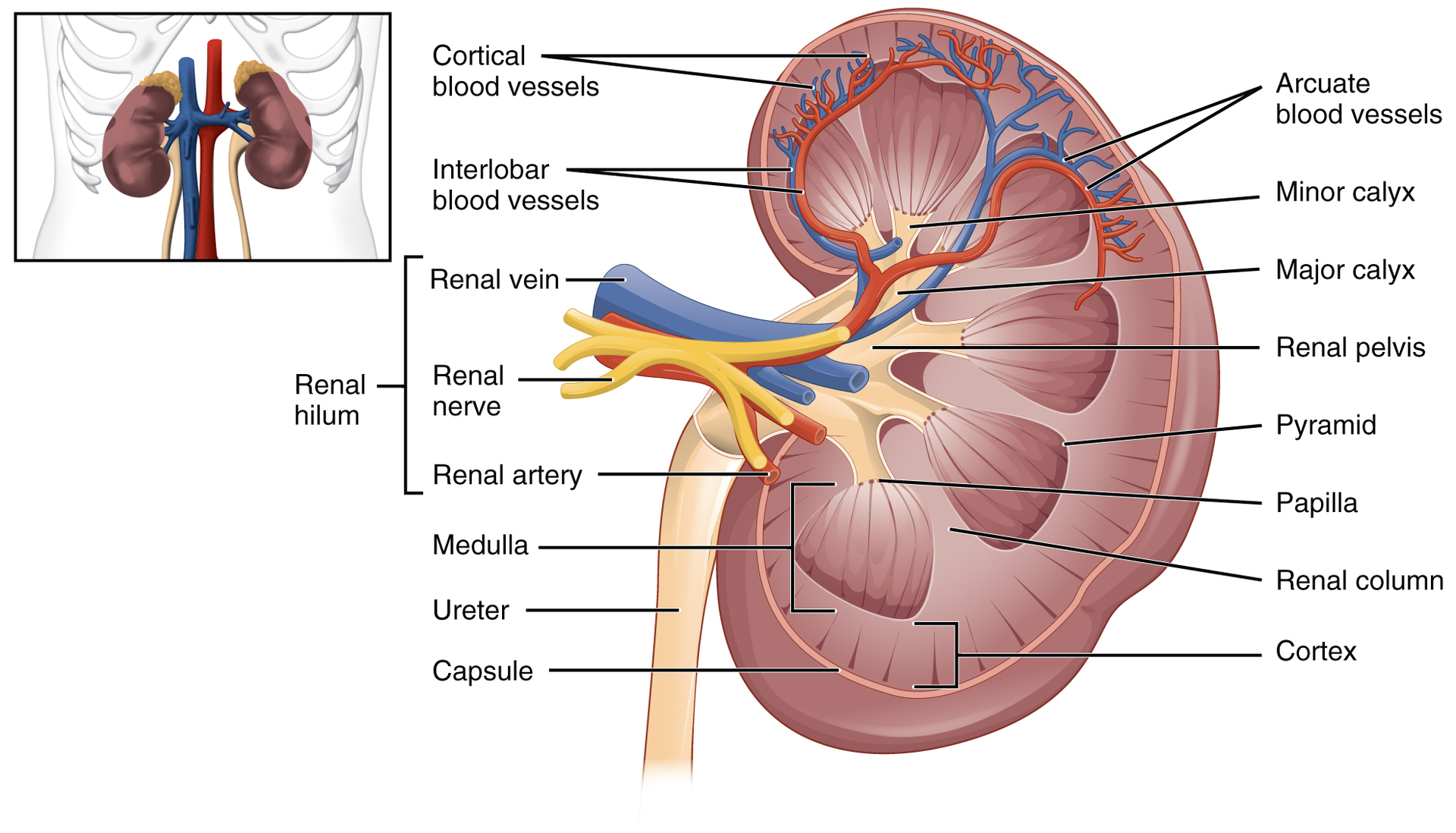
Q: What do the pyramids and renal columns together form?
A: Kidney lobes.

Q: Where are the renal corpuscles, PCTs, and DCTs located?
A: In the renal cortex.

Q: What are cortical nephrons?
A: Nephrons with short loops of Henle that do not extend into the medulla.

Q: What are juxtamedullary nephrons?
A: Nephrons with long loops of Henle that extend deep into the medulla.
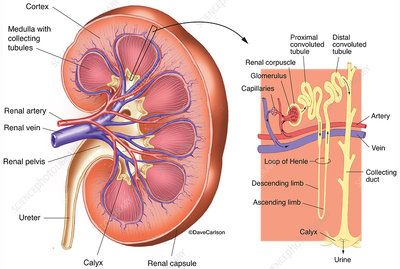
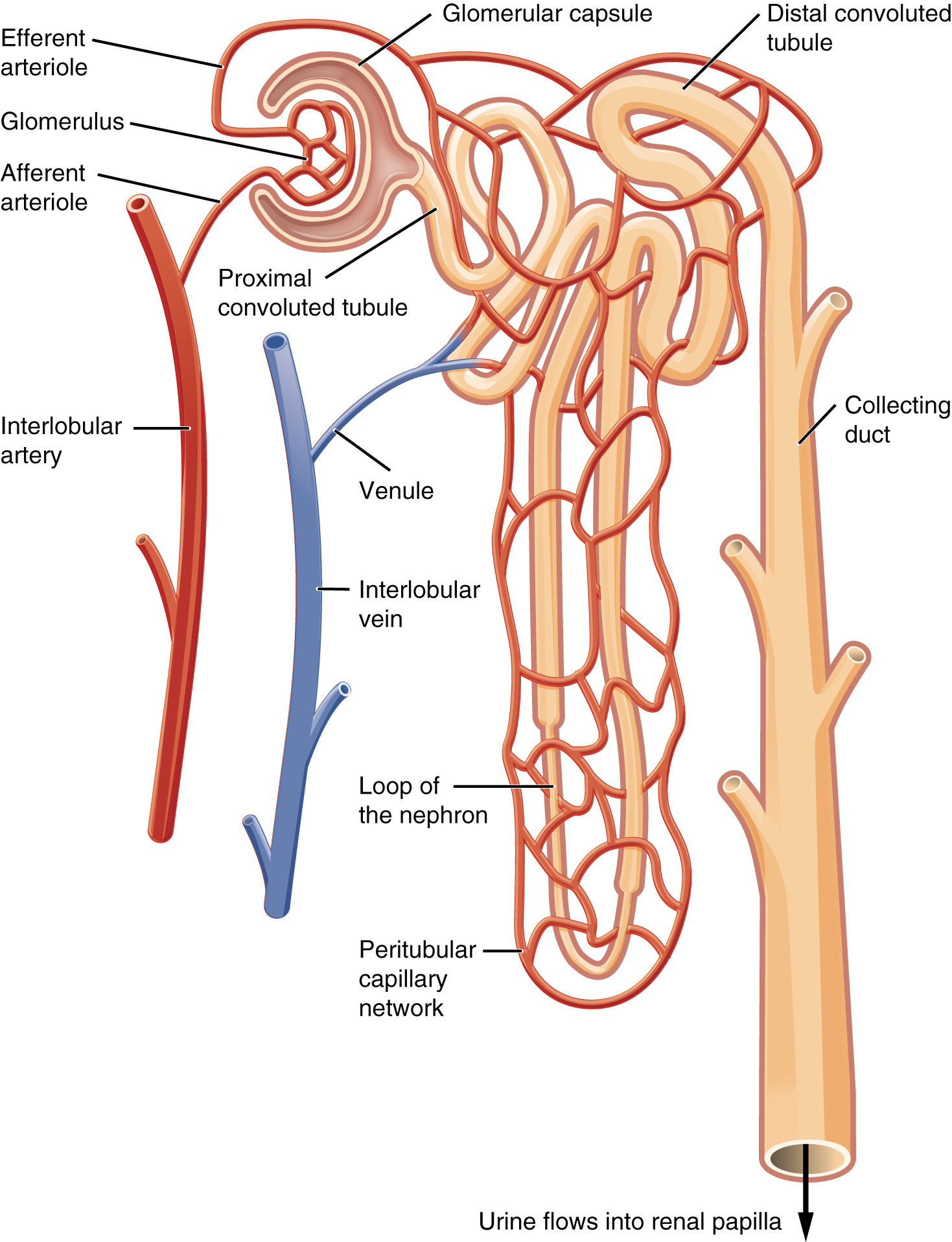
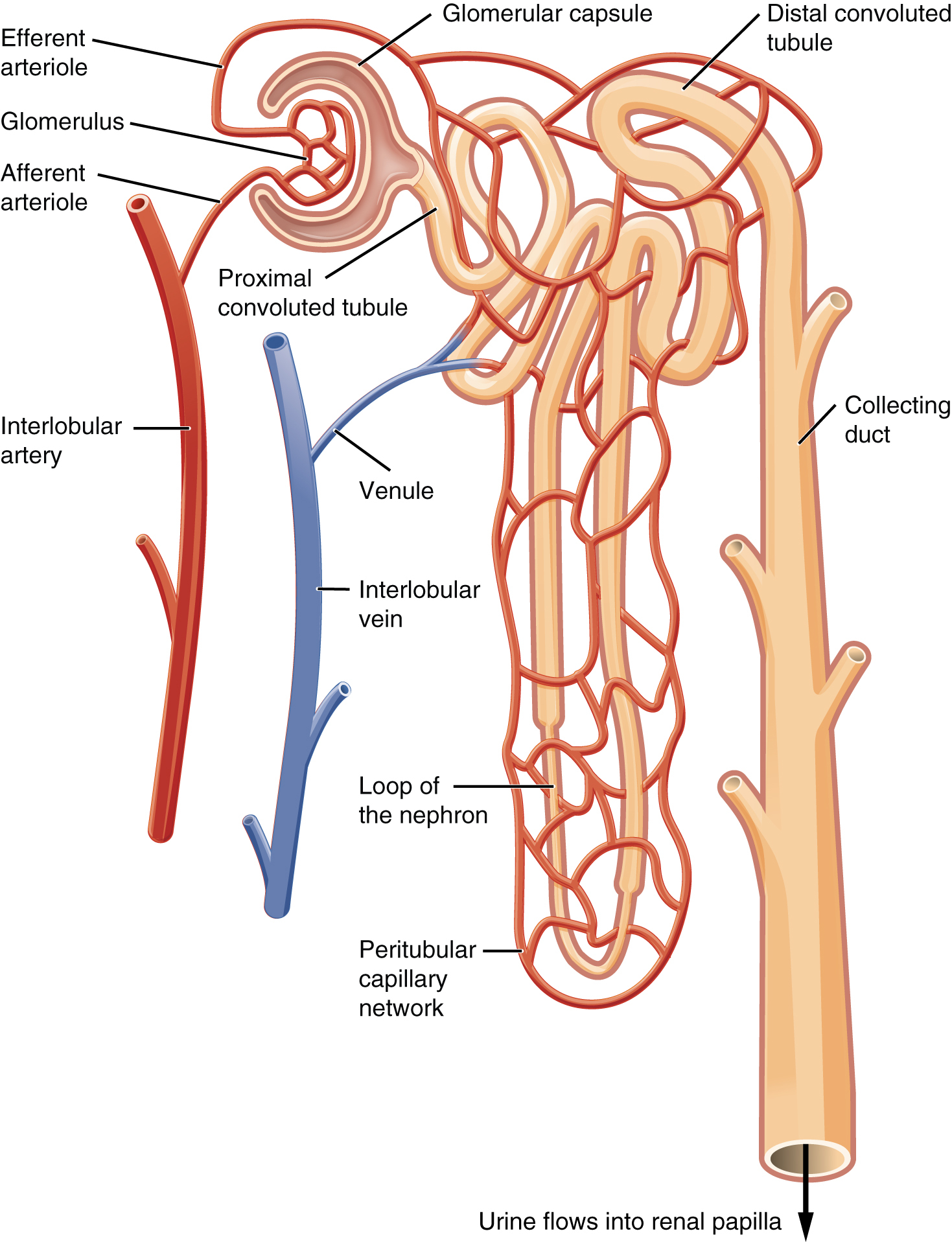
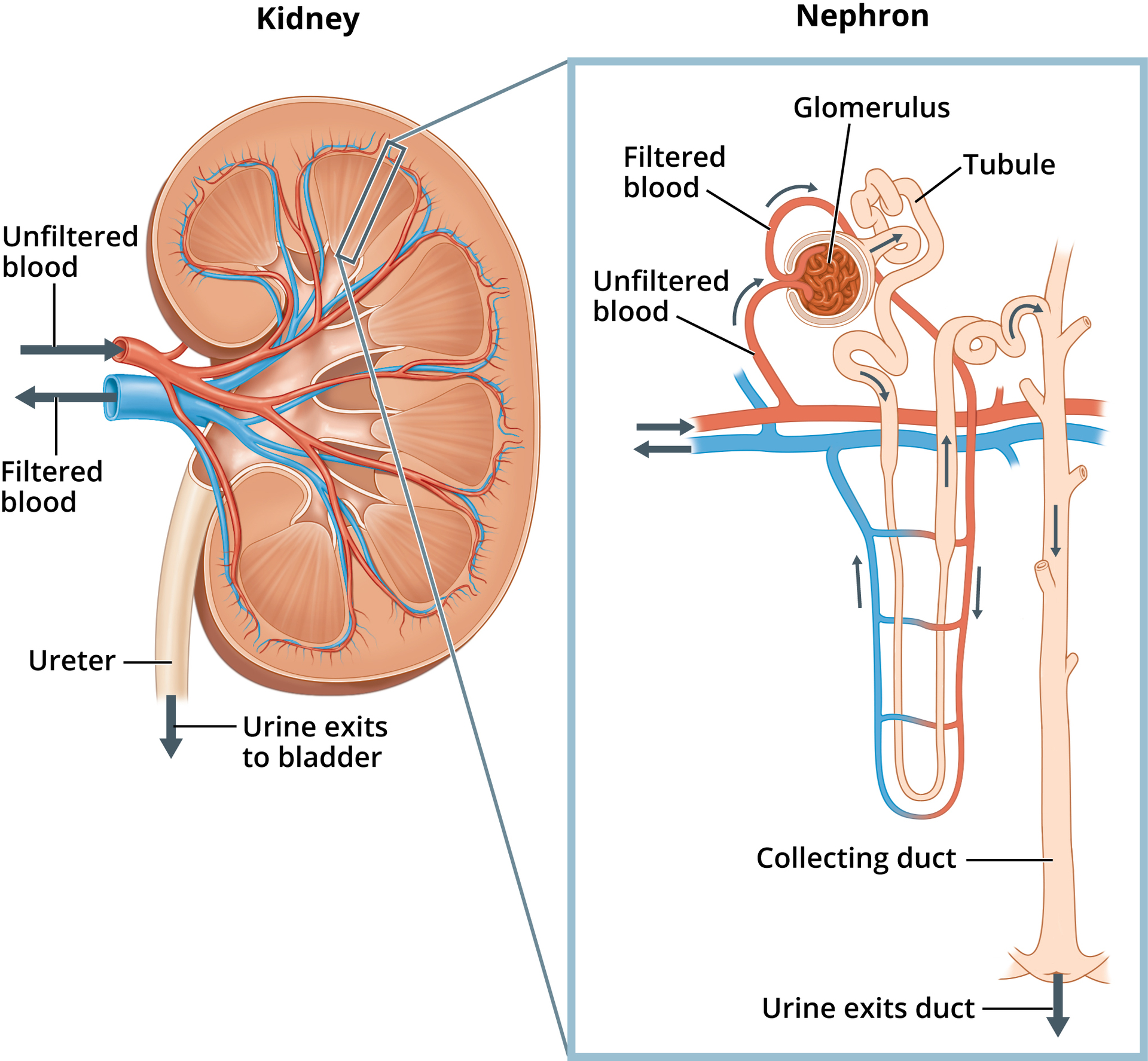
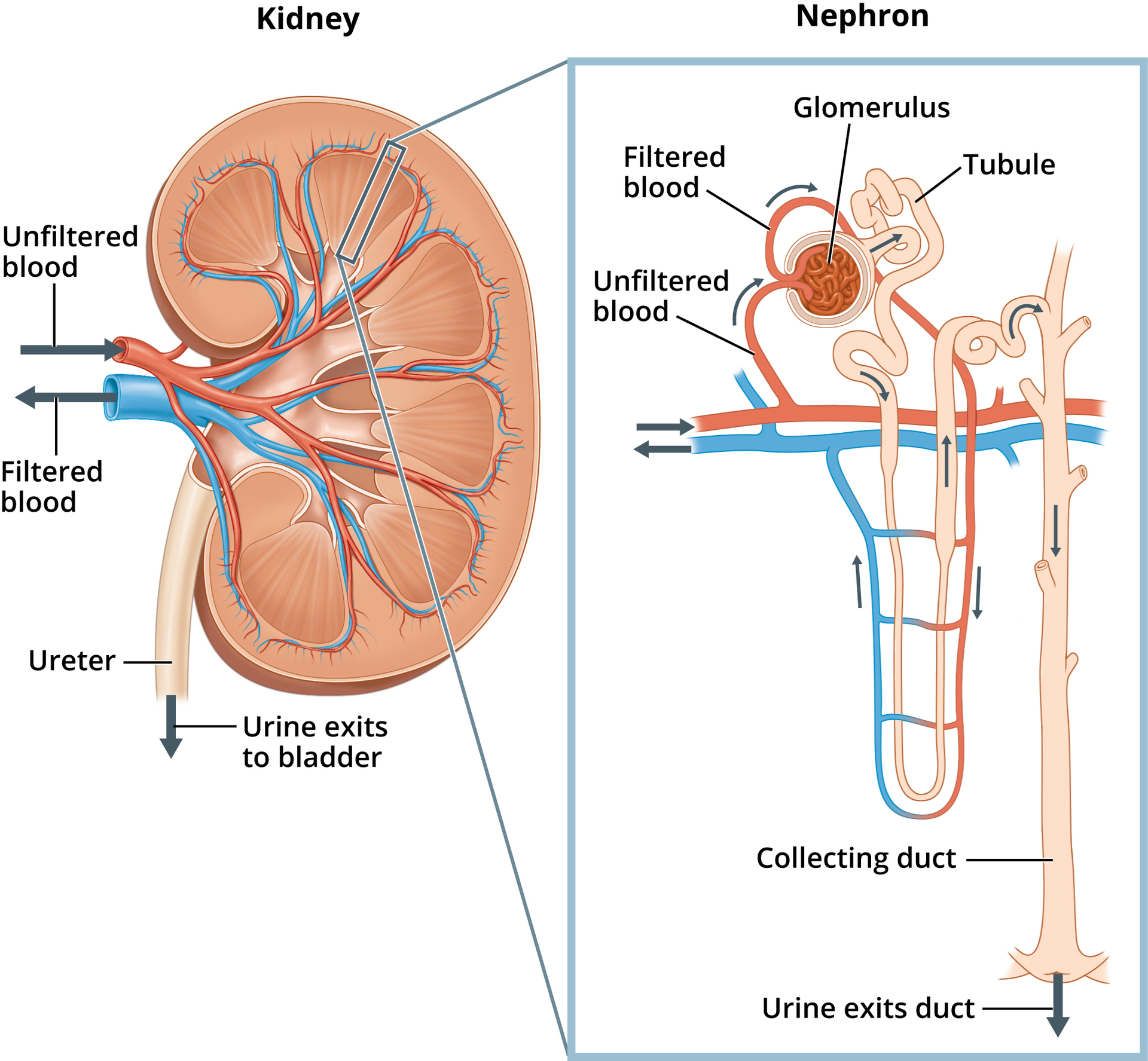
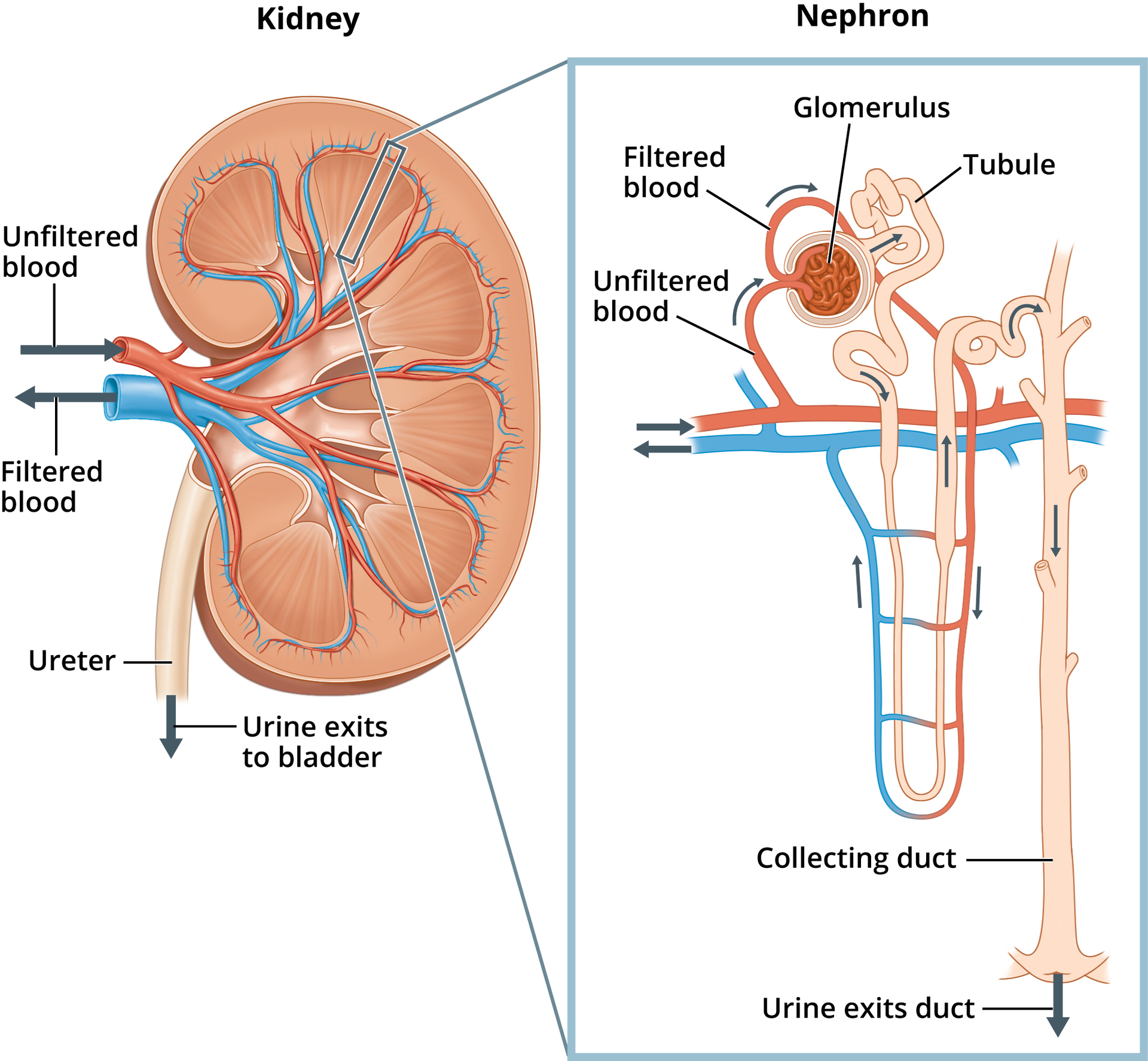
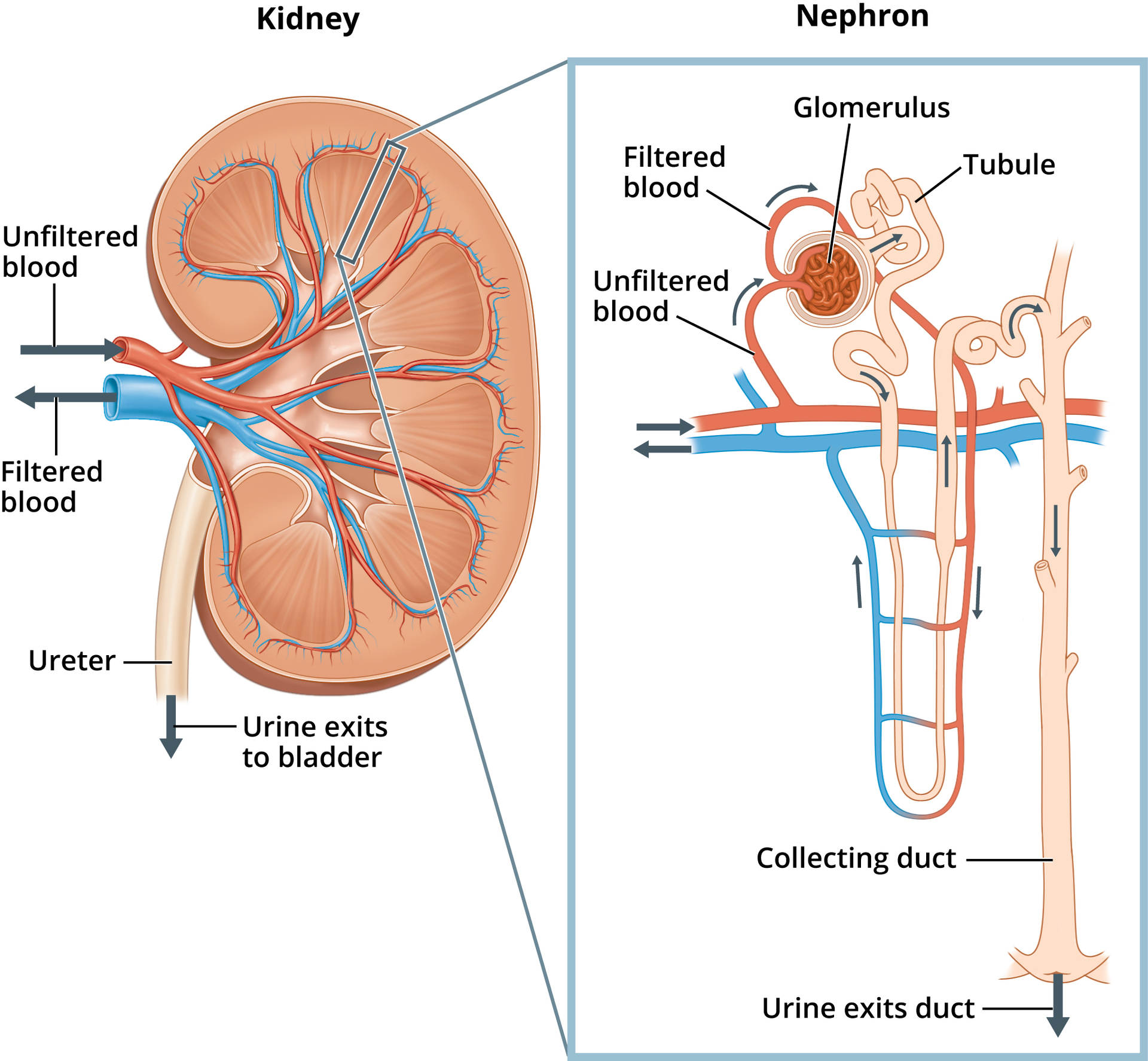
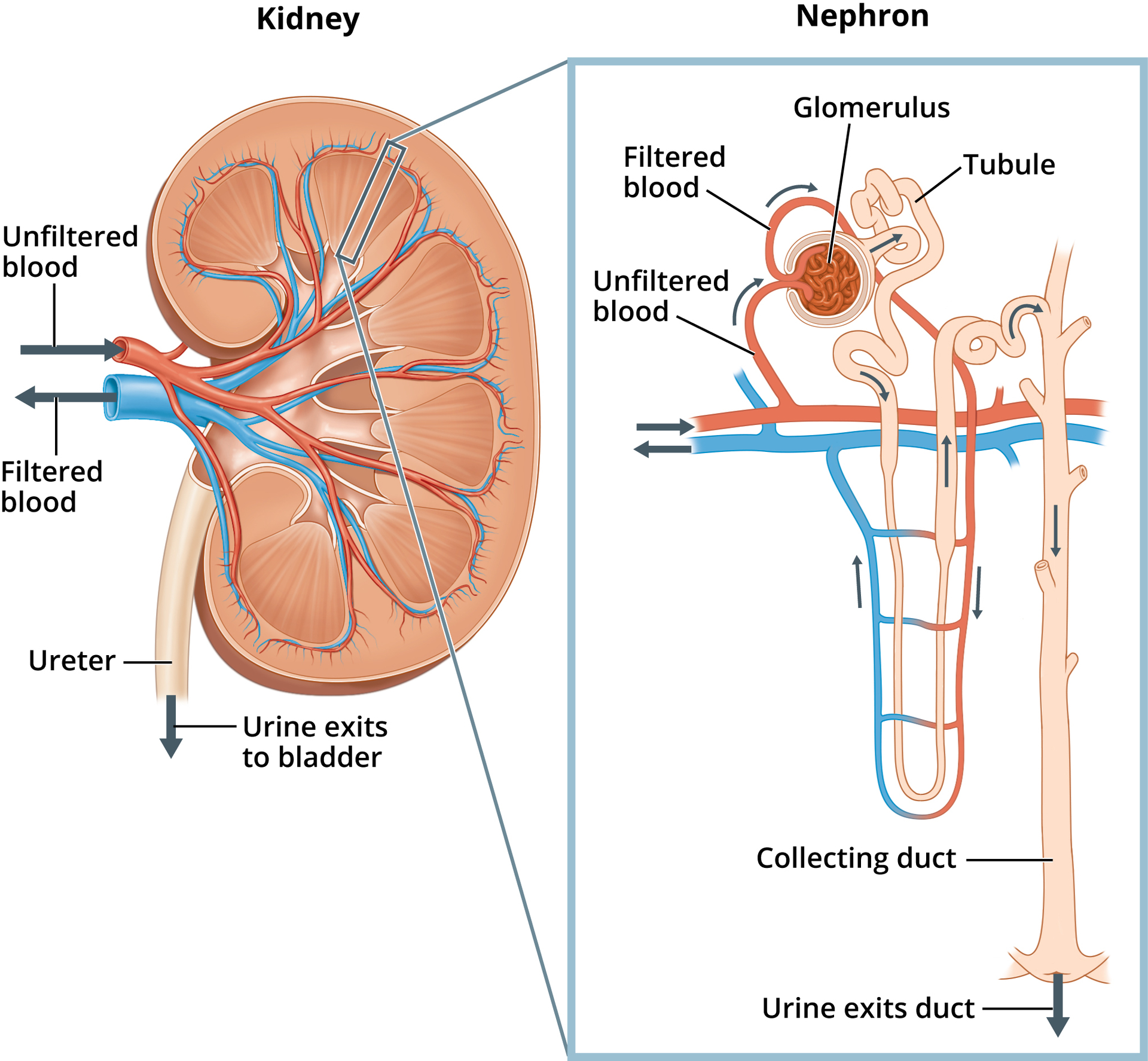
what is a nephron?
the basic structural and functional unit of the kidney. They are the microscopic structure composed of a renal corpuscle and a renal tubule.
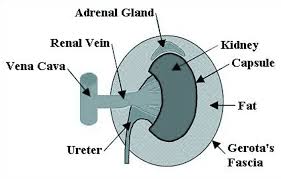
Q: What is the renal fat pad?
A: Adipose tissue that cushions the kidney between the renal fascia and capsule
Q: What are renal pyramids?
A: Cone-shaped tissues in the medulla that contain collecting ducts and loops of Henle.
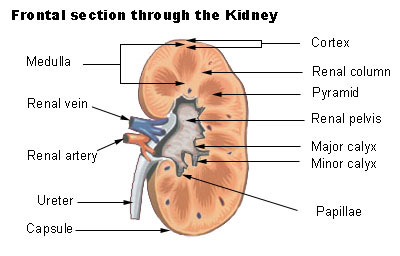
Q: What are calyces?
A: Cup-like structures that receive urine from collecting ducts and pass it to the renal pelvis and ureter.
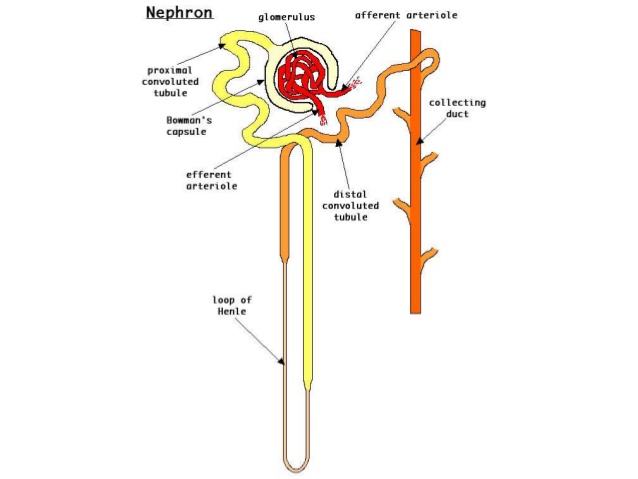
Q: What are proximal convoluted tubules (PCTs)?
A: Tubules that receive filtrate from Bowman’s capsule; major site of reabsorption and secretion.
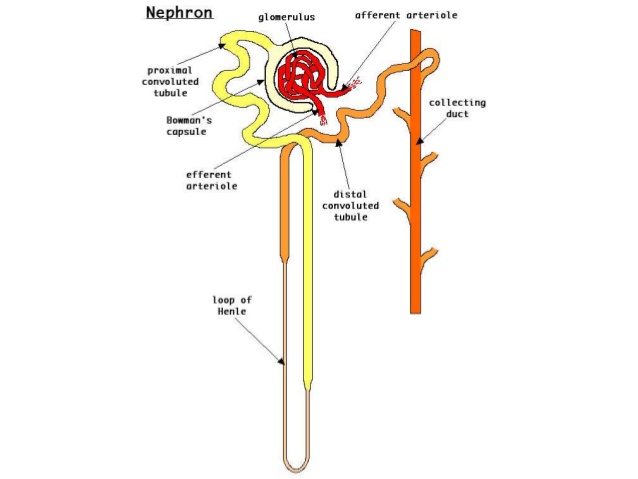
Q: What are distal convoluted tubules?
A: Tubules that receive filtrate from the loop of Henle and empty into collecting ducts.
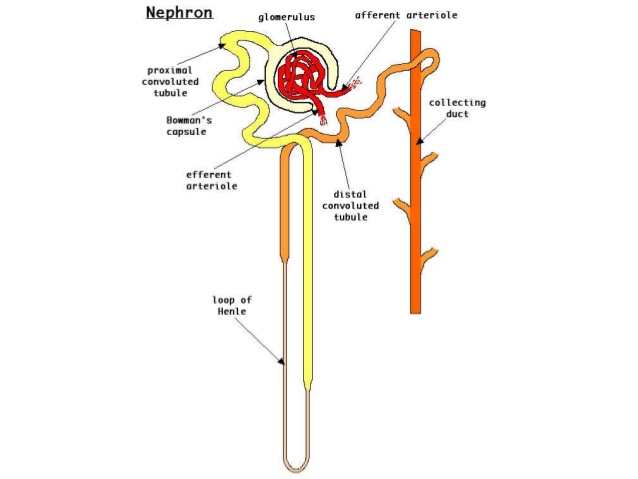
Q: What is the loop of Henle?
A: The descending and ascending parts of the nephron tubule between the PCT and DCT.
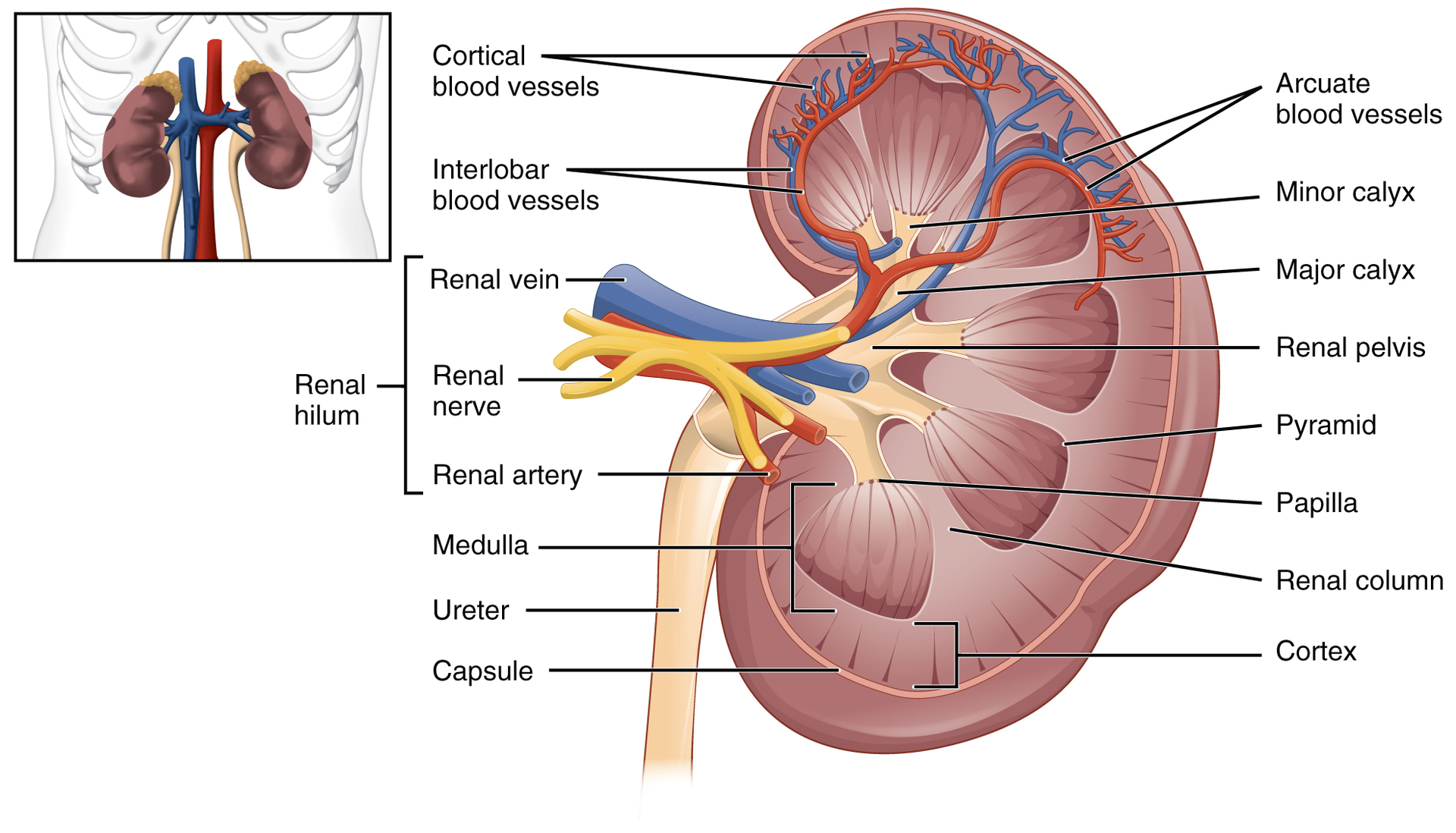
Q: What is the renal hilum?
A: The entry and exit site for vessels, nerves, lymphatics, and ureters of the kidney.
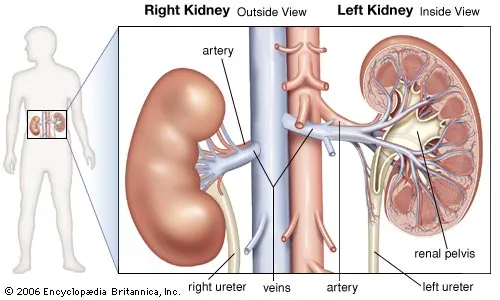
Q: What emerges from the renal hilum?
A: The renal pelvis, which funnels urine into the ureter via peristalsis.
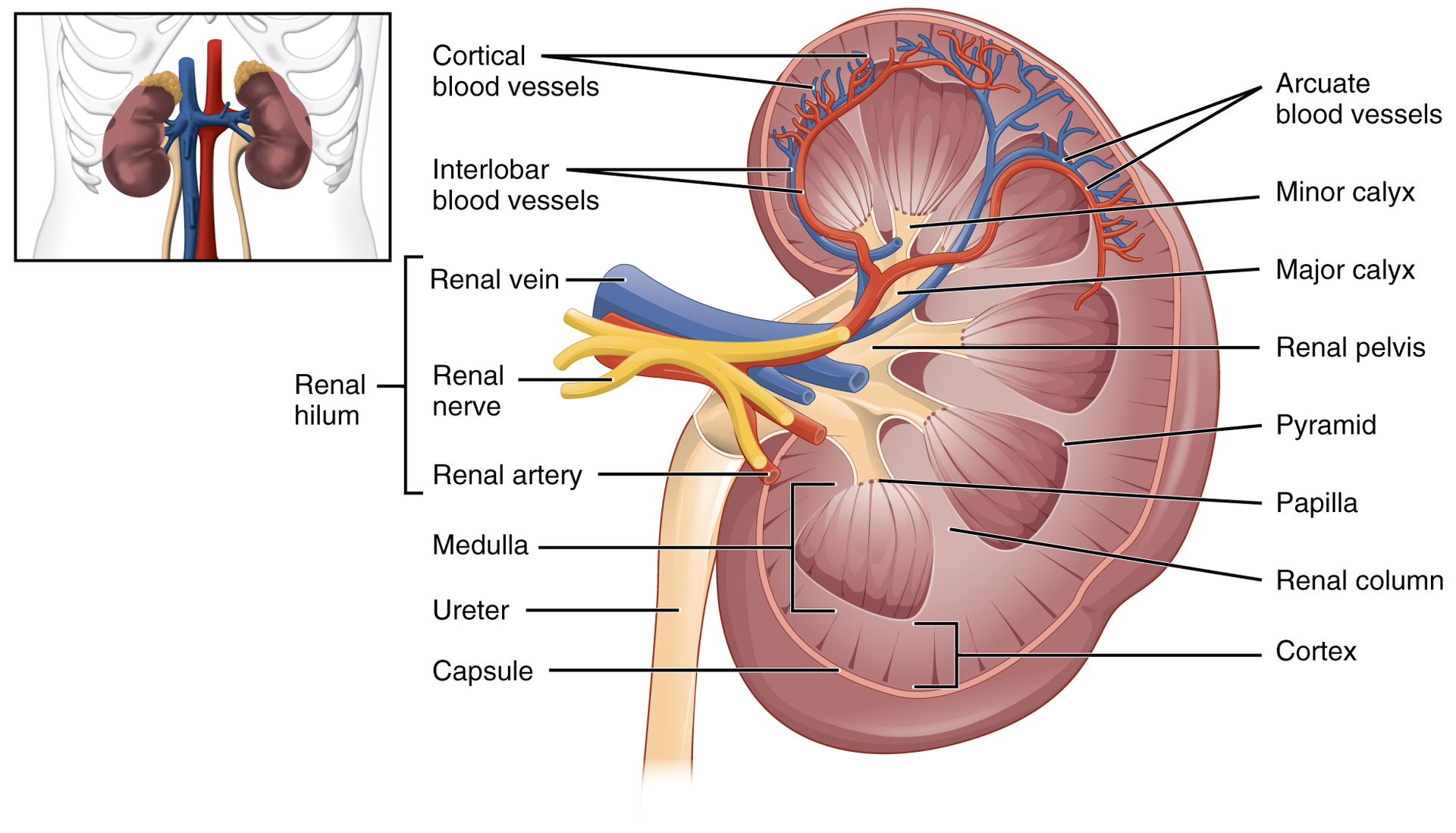
Q: What is the correct anterior-to-posterior order of structures at the renal hilum?
A: Renal artery → renal vein → renal pelvis.
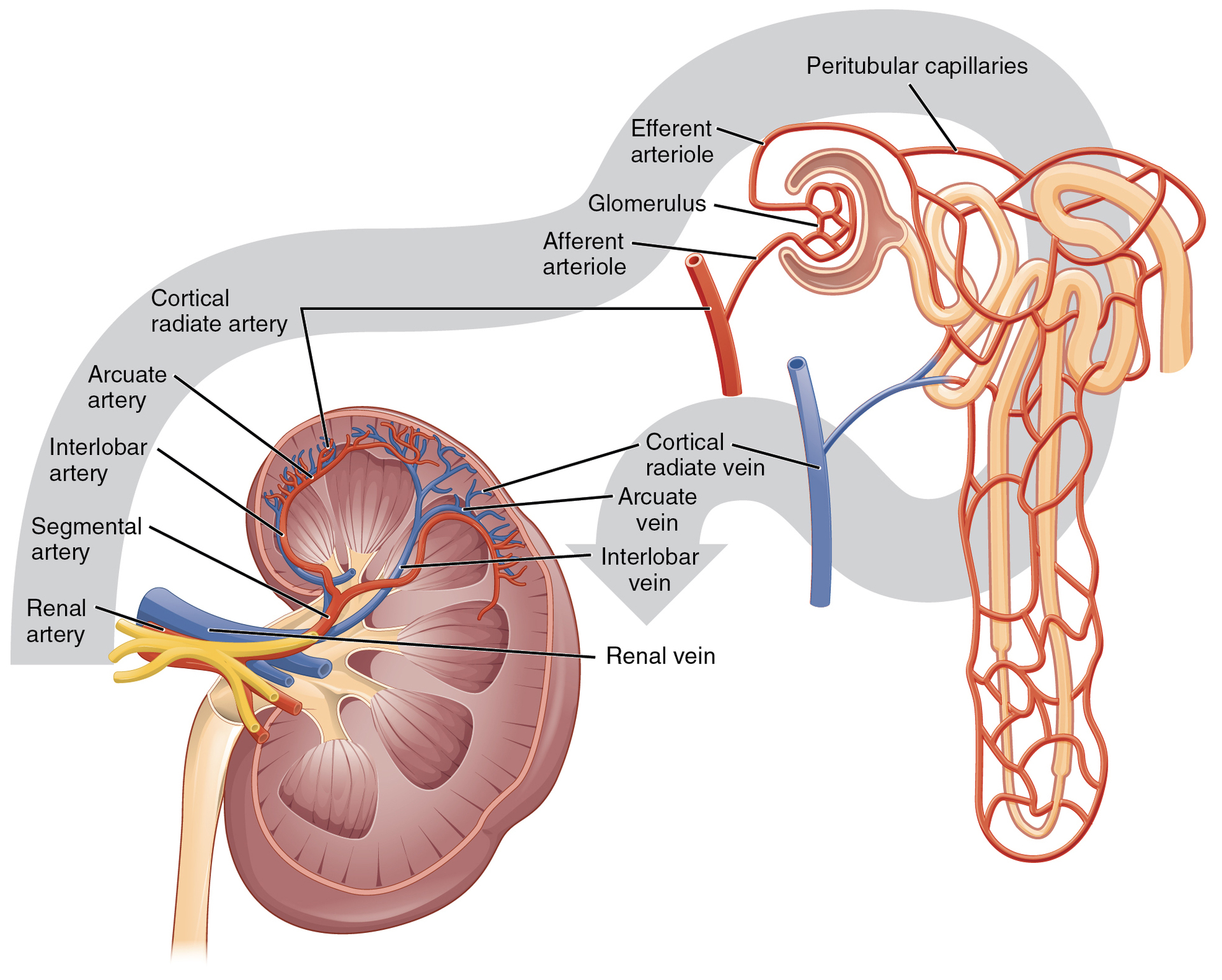
Q: Where do the renal arteries branch from?
A: Directly from the descending aorta.
Q: Where do the renal veins drain into?
A: The inferior vena cava.
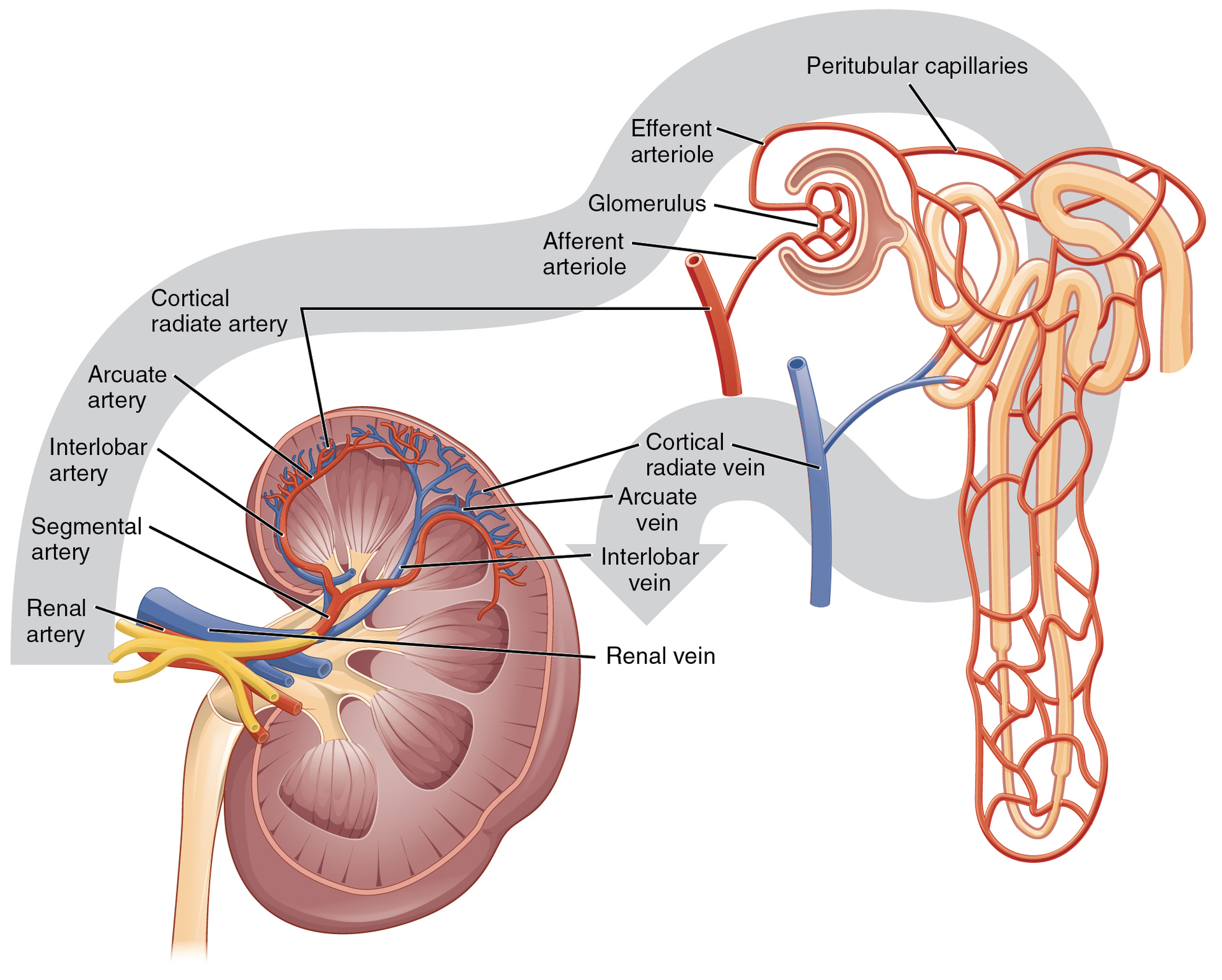
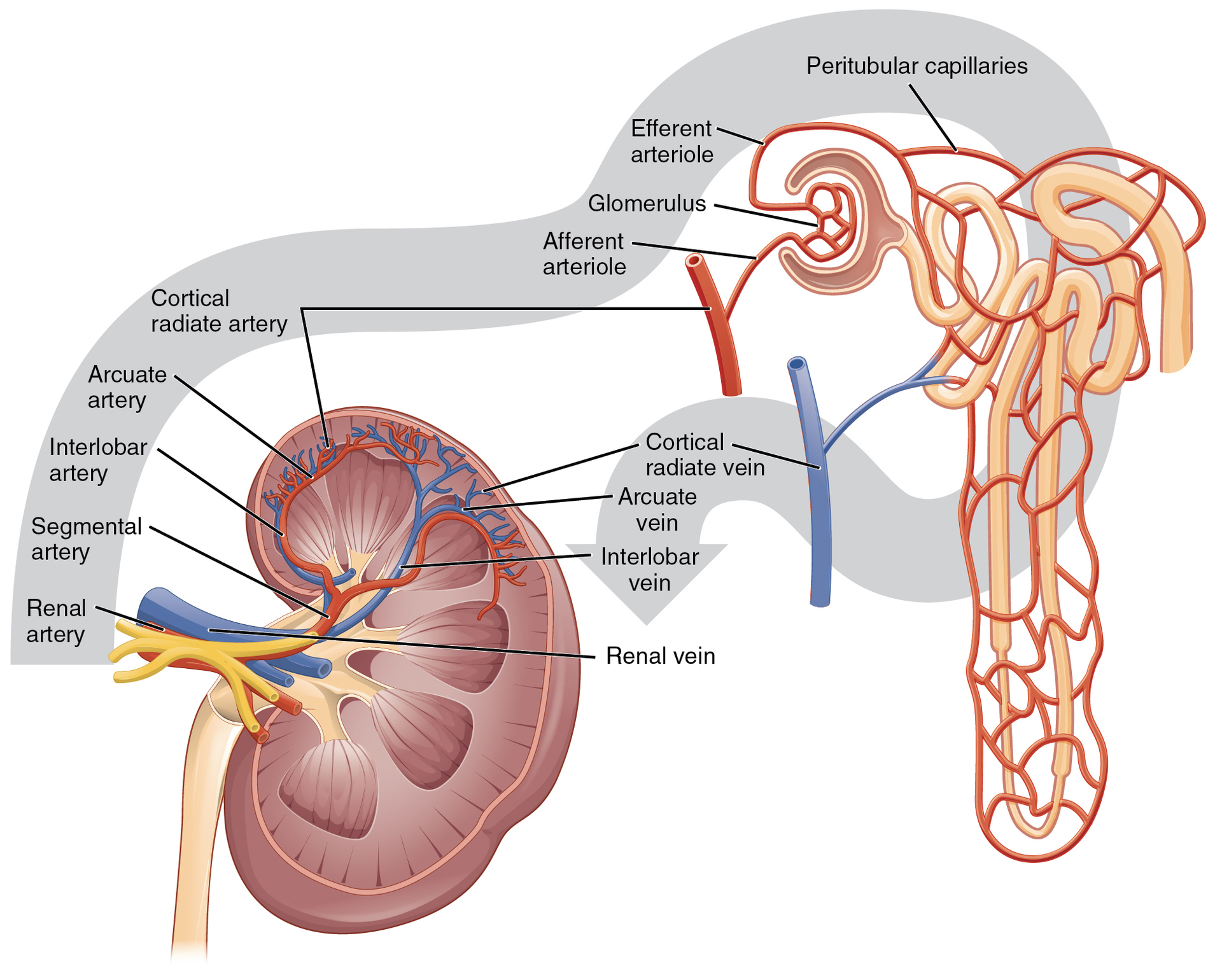
Q: What is the path of blood flow to nephrons starting from the renal artery?
A: Renal artery → segmental arteries → interlobar arteries → arcuate arteries → cortical radiate arteries → afferent arterioles.
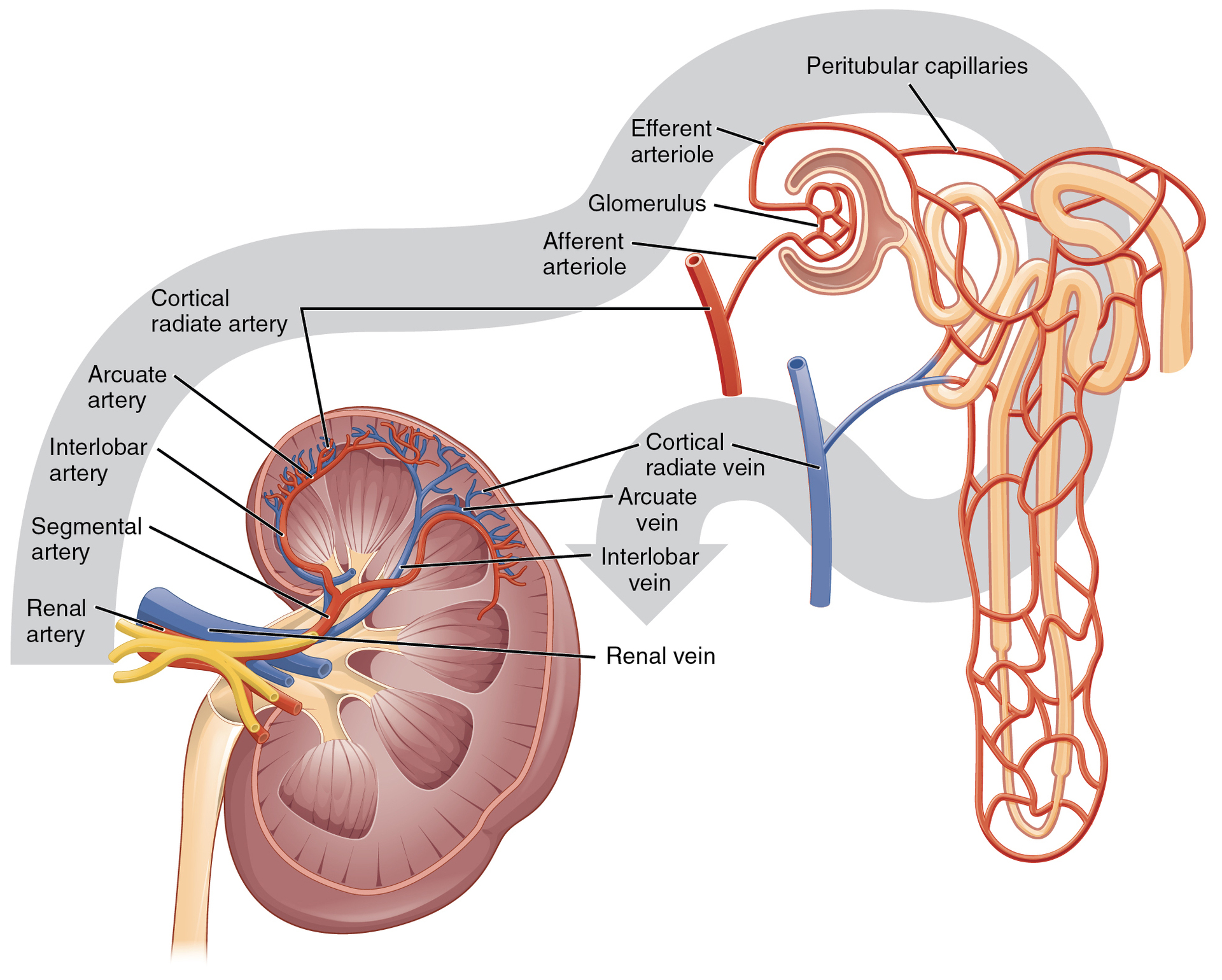
Q: What do afferent arterioles supply?
A: Approximately 1.3 million nephrons in each kidney.
renal hilum:
recessed medial area of the kidney through which the renal artery, renal vein, ureters, lymphatics, and nerves pass
Upon entering the kidney, the renal artery branches to form which vessel?
Interlobar arteries
Peritubular capillaries
Afferent arteriole
Segmental artery
Segmental artery
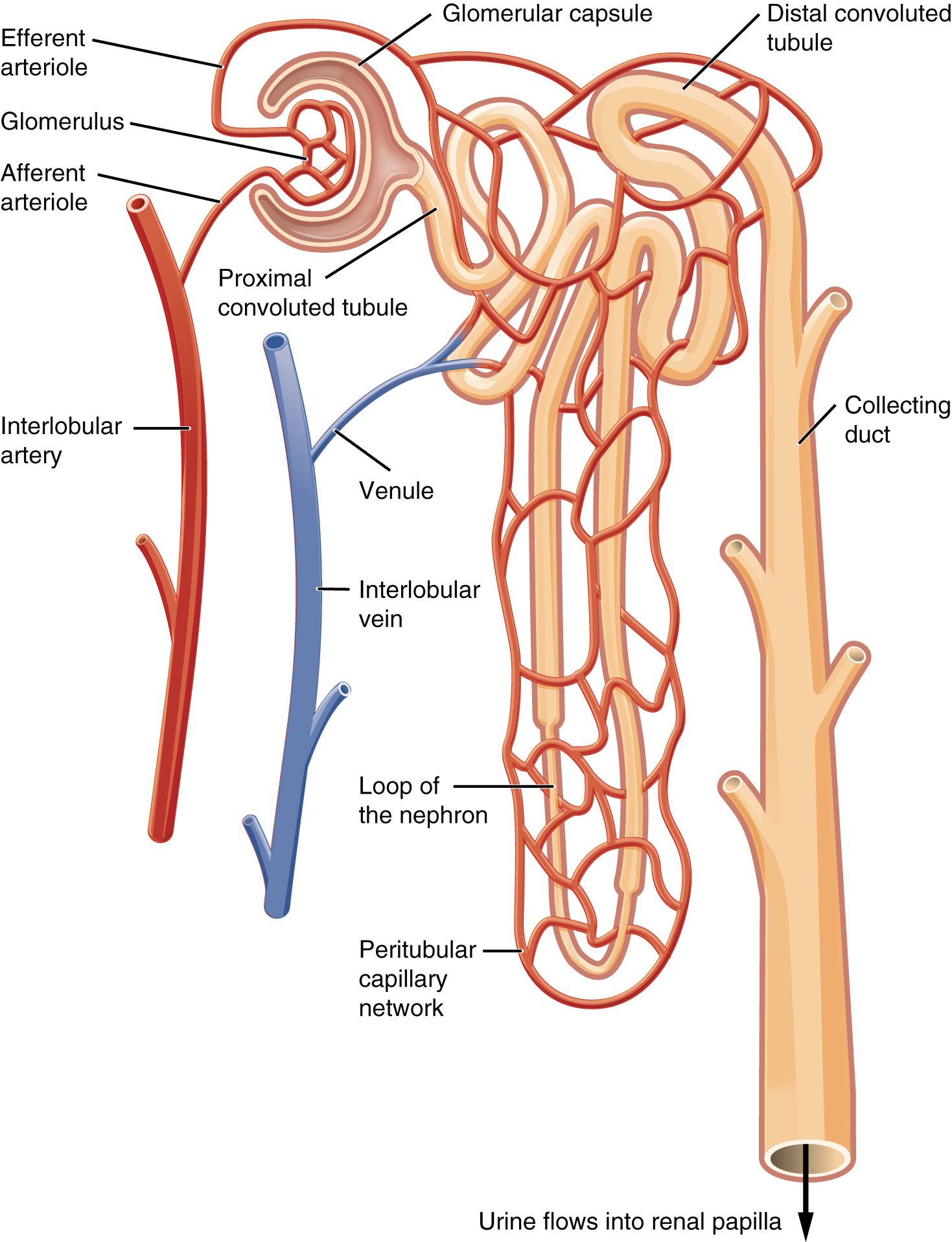
Q: What is the functional unit of the kidney?
A: The nephron.
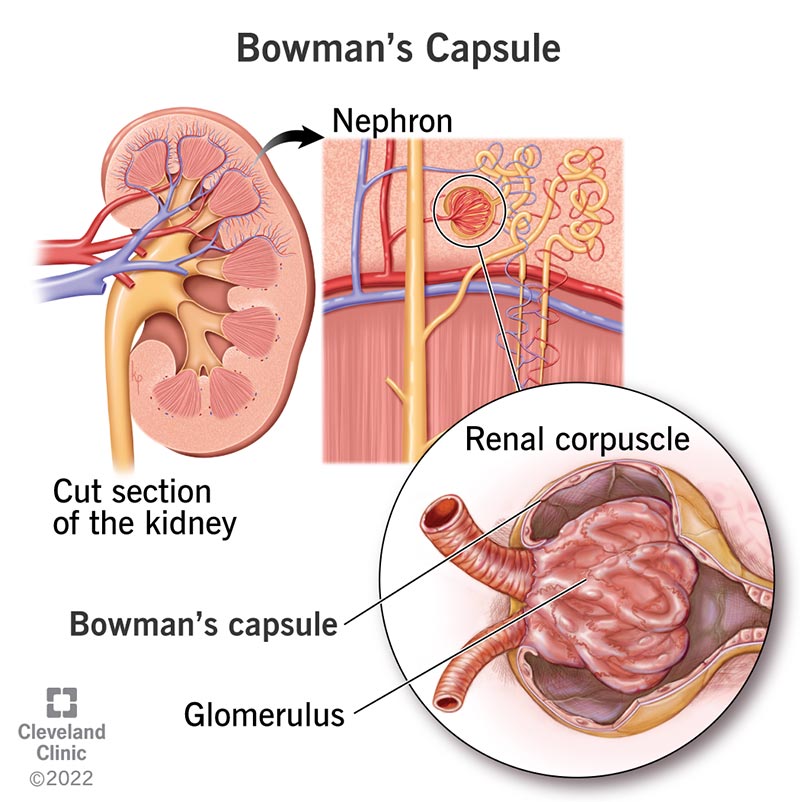
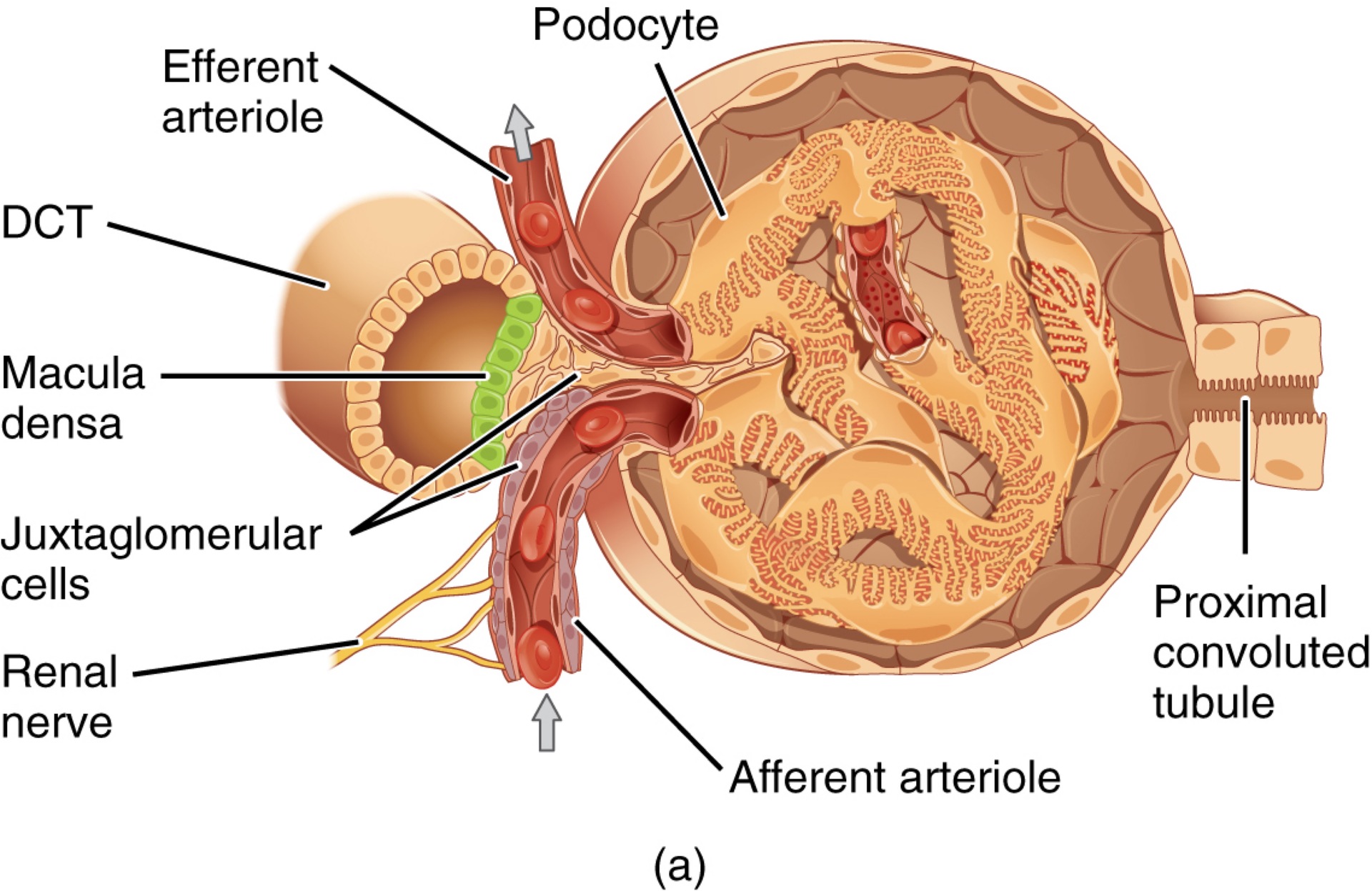
Q: What two structures make up the renal corpuscle?
A: The glomerulus and Bowman’s capsule.
Q: What is the glomerulus?
A: A tuft of high-pressure capillaries that filter blood based on particle size.
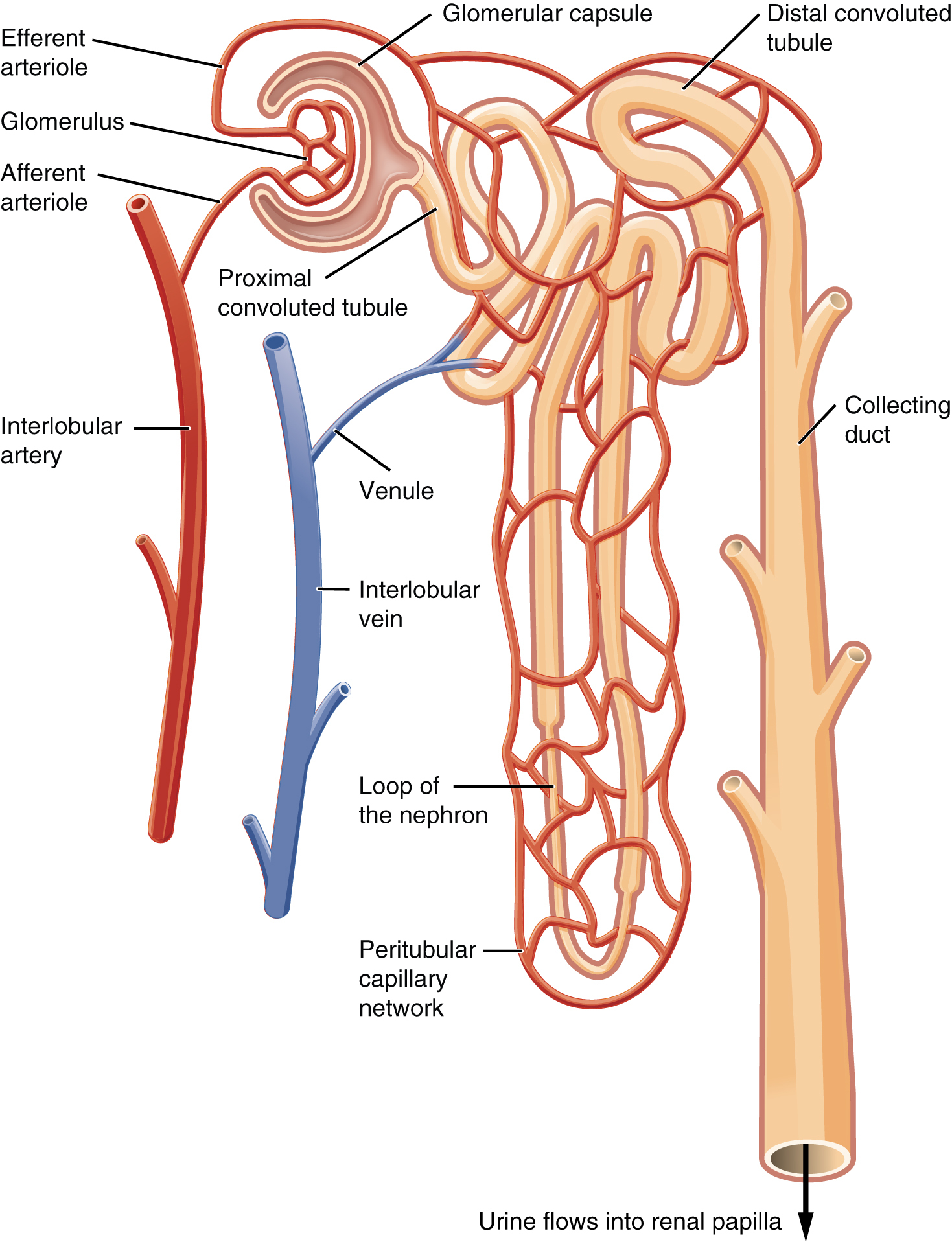
Q: What vessel brings blood into the glomerulus?
A: The afferent arteriole.
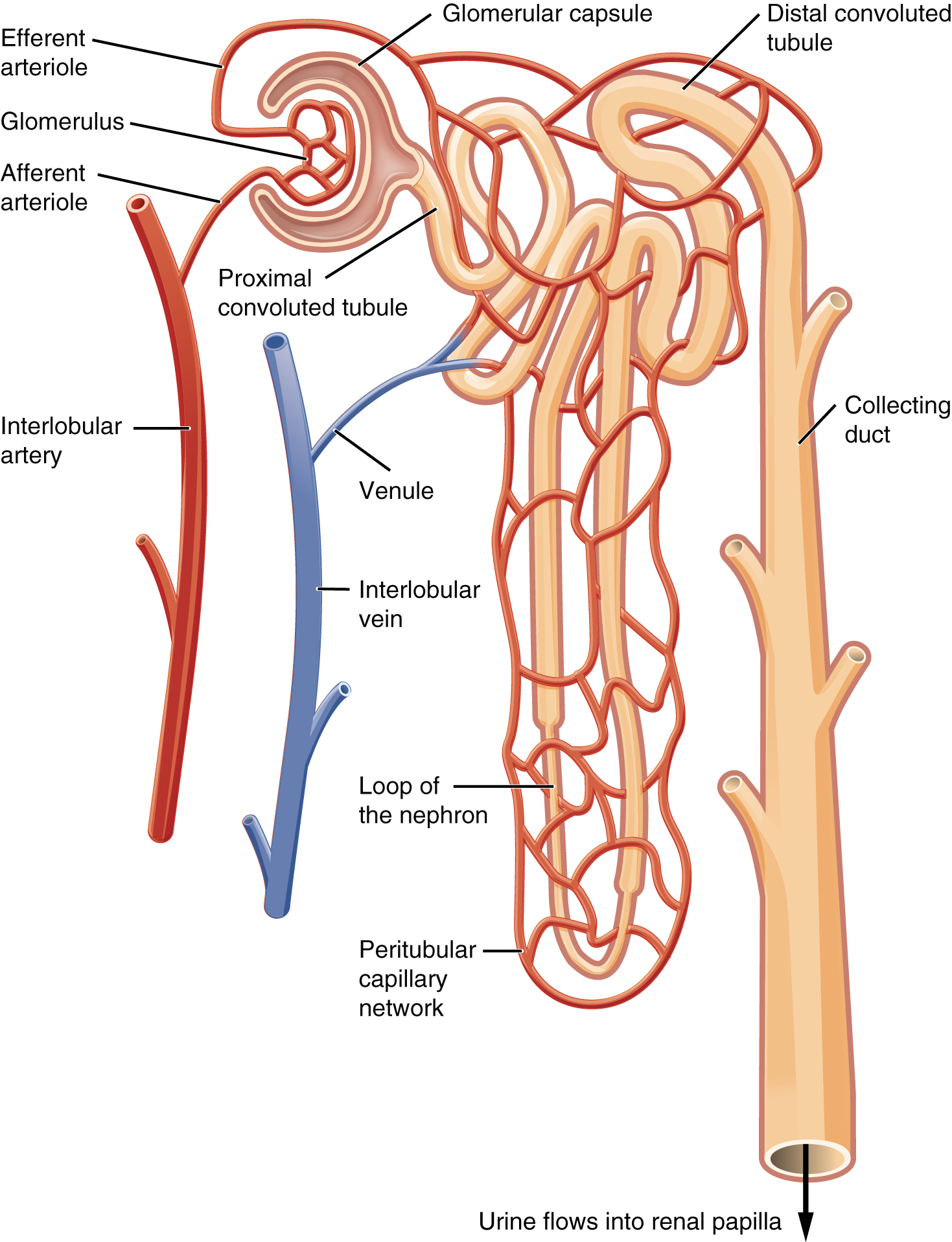
Q: What vessel carries blood away from the glomerulus?
A: The efferent arteriole.
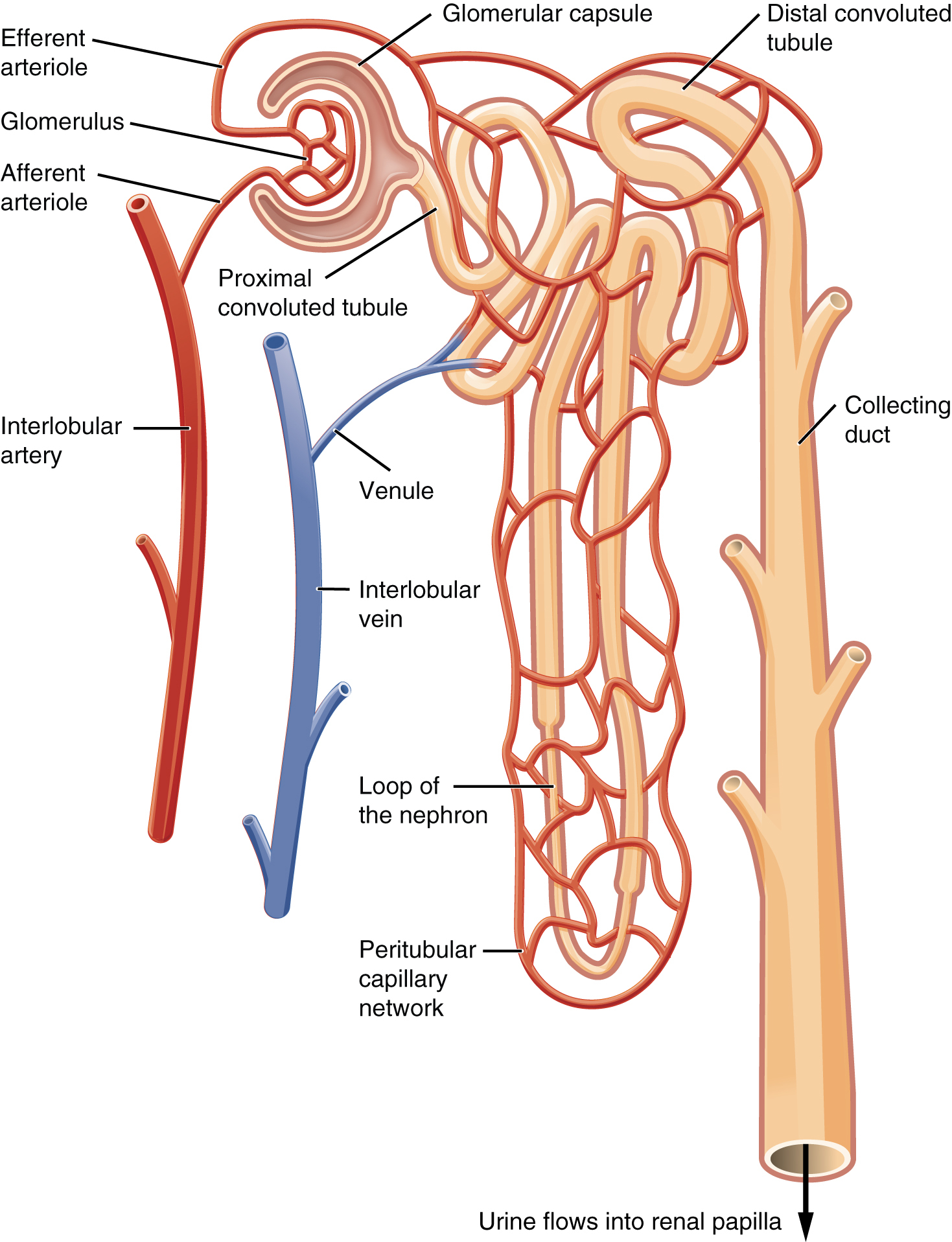
Q: What does the efferent arteriole give rise to?
A: The peritubular capillaries and the vasa recta.
vasa recta capillaries
long, hairpin-shaped blood vessels that run parallel to the loops of Henle.
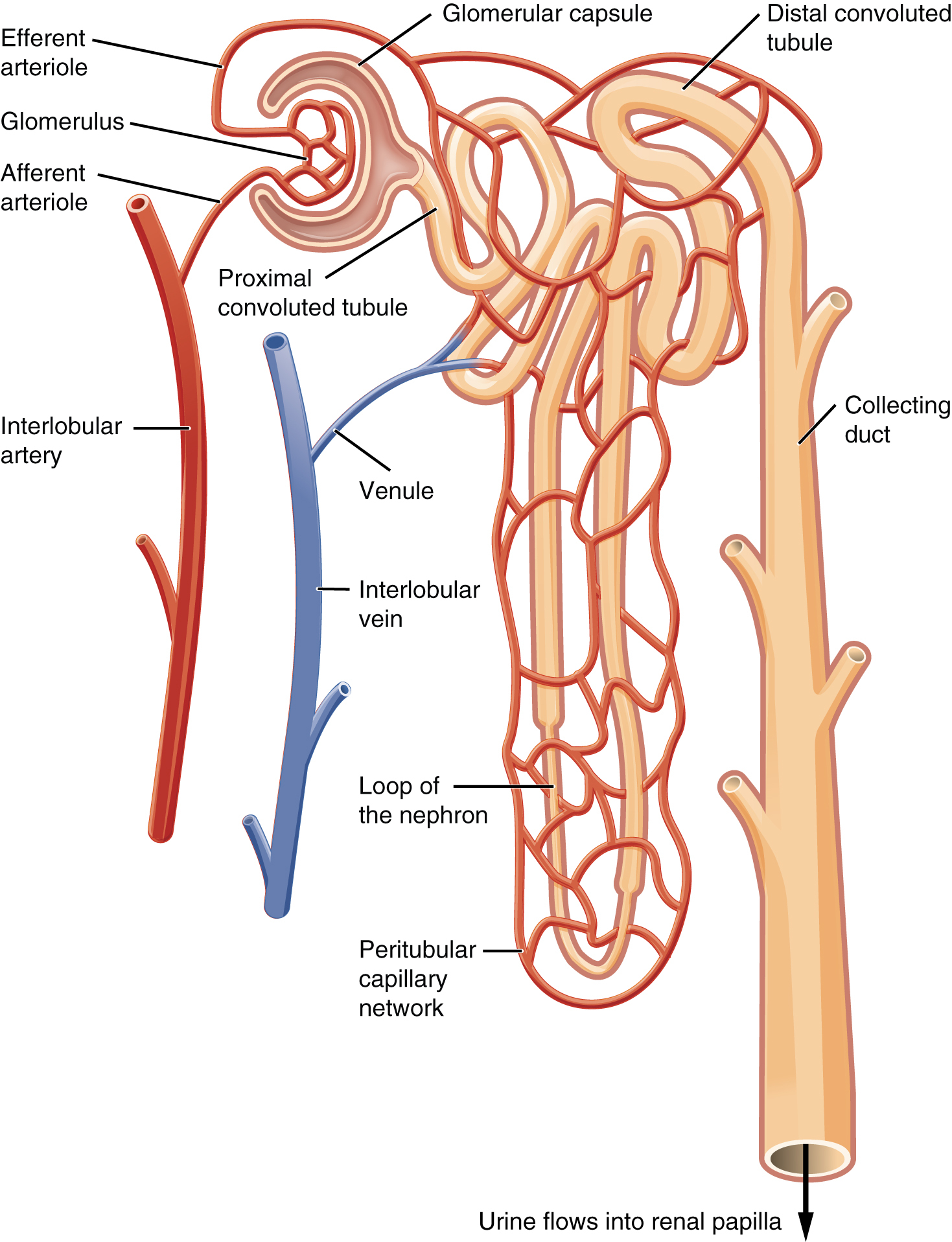
Q: What do peritubular capillaries and vasa recta do?
A: Reabsorb solutes and water from the filtrate and return them to circulation.
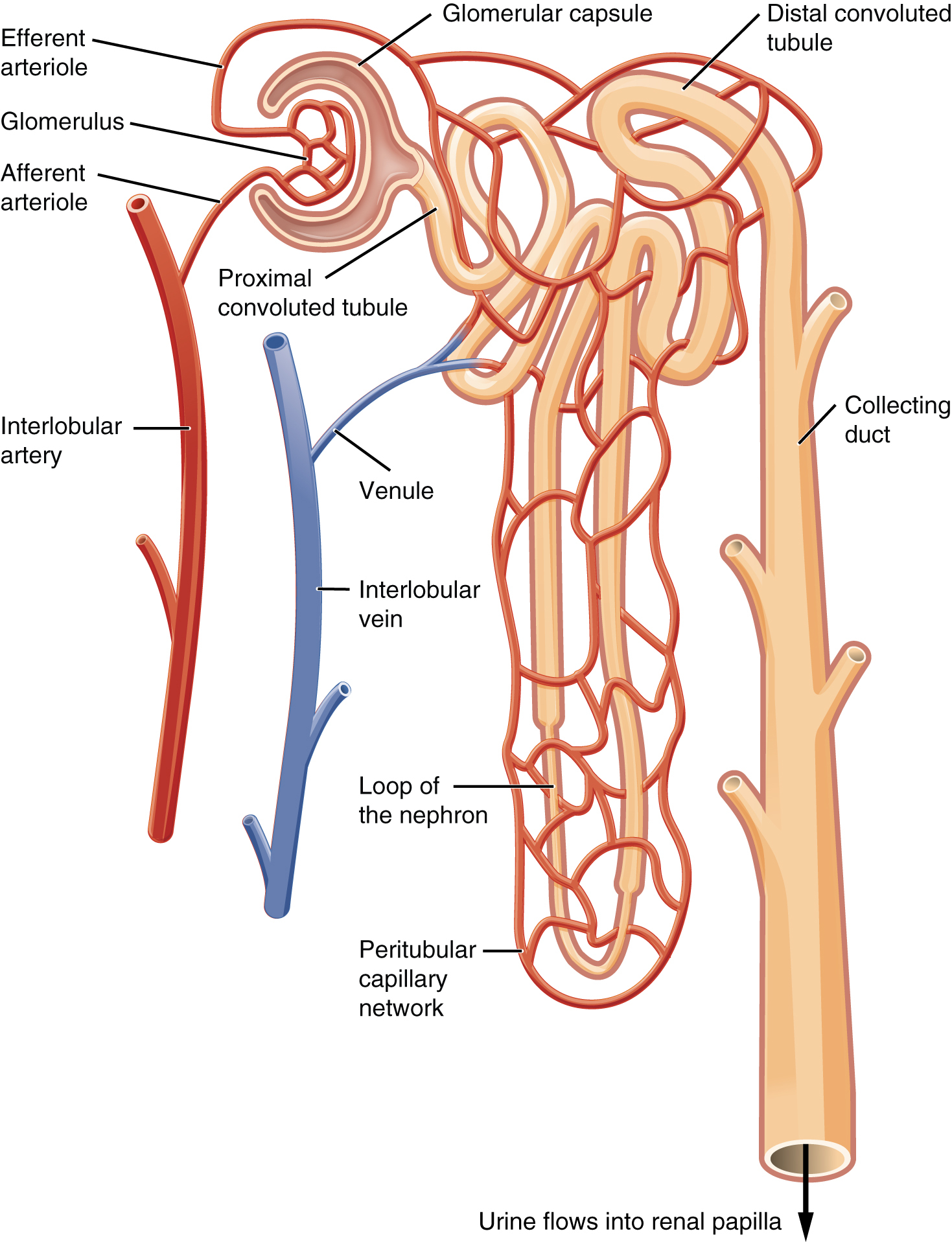
Q: Why is the nephron’s blood supply considered a portal system?
A: Because a capillary bed (glomerulus) drains into an arteriole, which then forms a second capillary bed (peritubular capillaries/vasa recta).
Q: What are the three principal functions of nephrons?
A: Filtration, reabsorption, and secretion.
Q: What hormone does the nephron release to regulate blood pressure?
A: Renin.
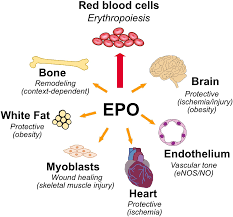
Q: What hormone does the nephron release to stimulate red blood cell production?
A: Erythropoietin (EPO).
Q: What role do the kidneys play in calcium absorption?
A: They convert calcidiol into calcitriol, the active form of vitamin D.
Which two structures comprise the renal corpuscle?
Choose 2 answers.
Glomerulus
Bowman’s capsule
Efferent arteriole
Vasa recta
Glomerulus
Bowman’s capsule
Q: What are nephrons?
A: Functional units of the kidney that carry out filtration and modification to produce urine; consist of renal corpuscles, proximal and distal convoluted tubules, and loops of Henle; drain into collecting ducts.
Q: What is the glomerulus?
A: A tuft of capillaries surrounded by Bowman’s capsule that filters the blood based on solute size.
Q: What is Bowman’s capsule?
A: A cup-shaped sac lined by simple squamous epithelium and podocytes; it receives the filtrate from the glomerulus.
Q: What makes up the renal corpuscle?
A: The glomerulus and Bowman’s capsule.
Q: What does the efferent arteriole do?
A: Carries blood from the glomerulus to capillary beds around the nephron tubules (peritubular capillaries and vasa recta).
Q: What is the peritubular capillary?
A: The second capillary bed in the renal portal system; surrounds the convoluted tubules.
Q: What is the vasa recta?
A: Branches of the efferent arterioles that parallel the loop of Henle and are part of the portal system.
Q: What is "forming urine"?
A: Filtrate undergoing secretion and reabsorption before becoming true urine.
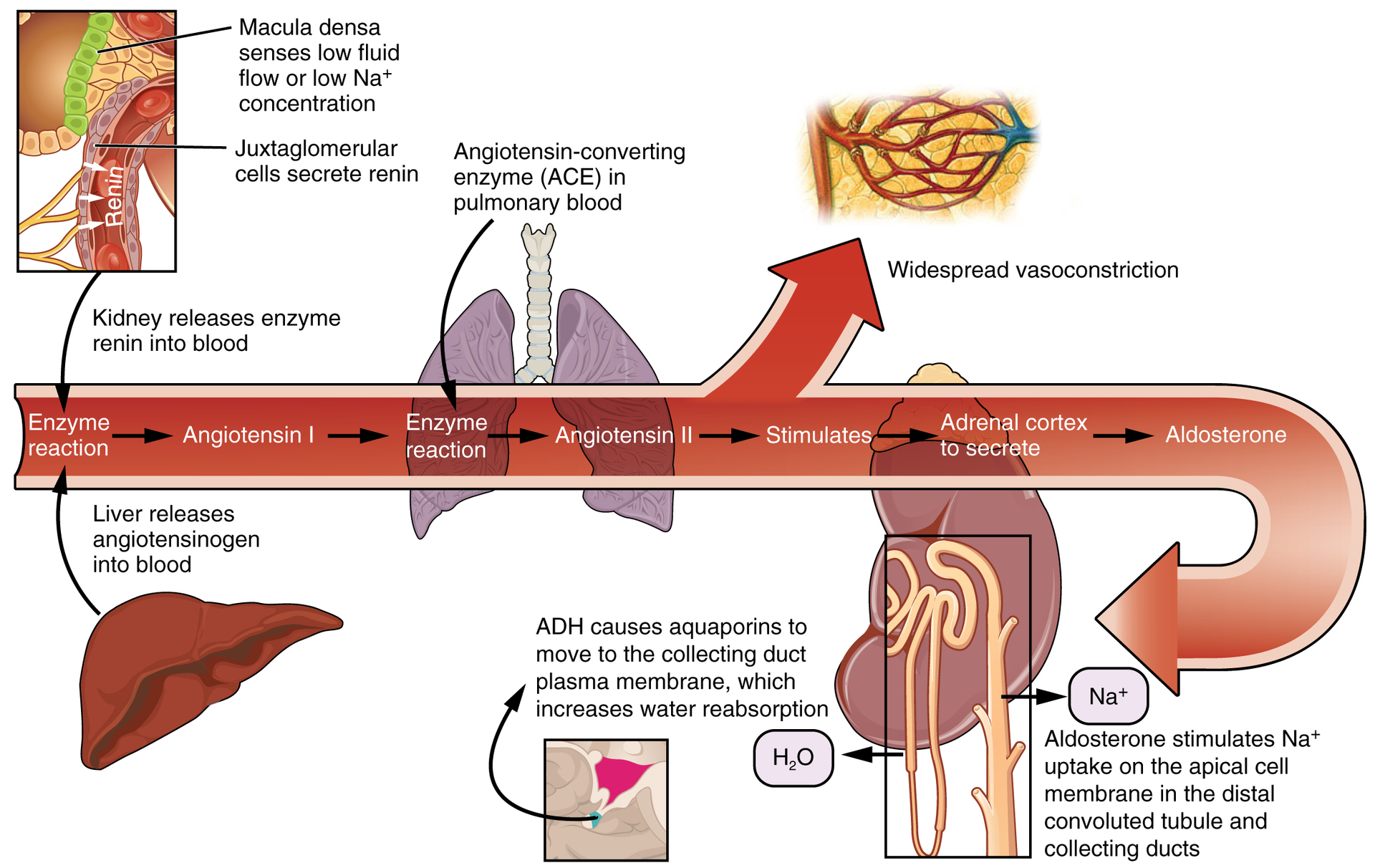
Q: What is renin?
A: An enzyme from juxtaglomerular cells that responds to low blood pressure and initiates the conversion of angiotensinogen to angiotensin I.
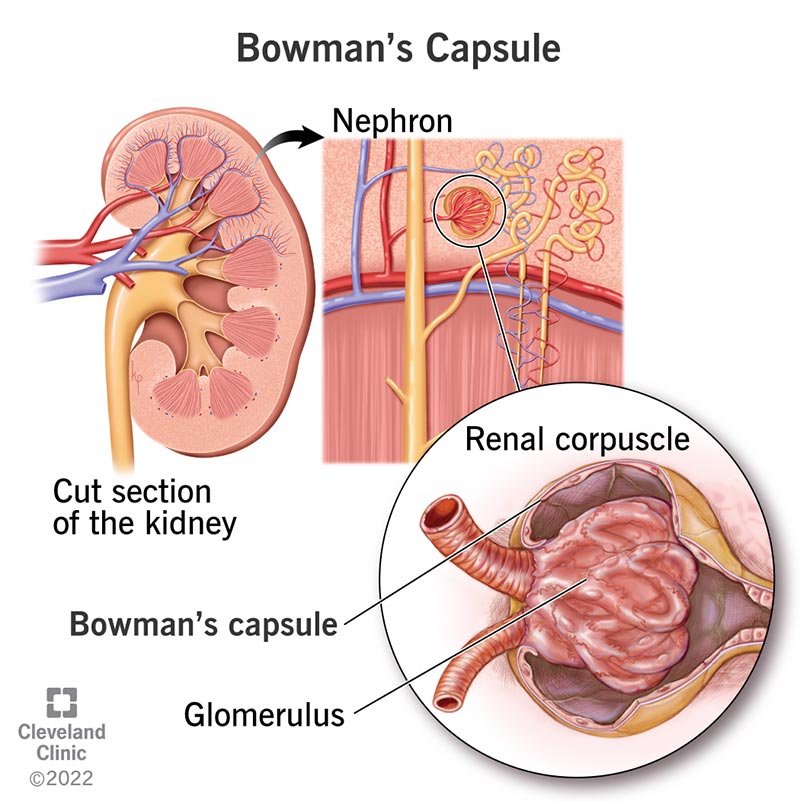
What are the two layers of Bowman’s capsule and their functions?
A: The parietal layer is a simple squamous epithelium forming the outer wall; the visceral layer is made of podocytes that wrap around the glomerular capillaries and participate in filtration.
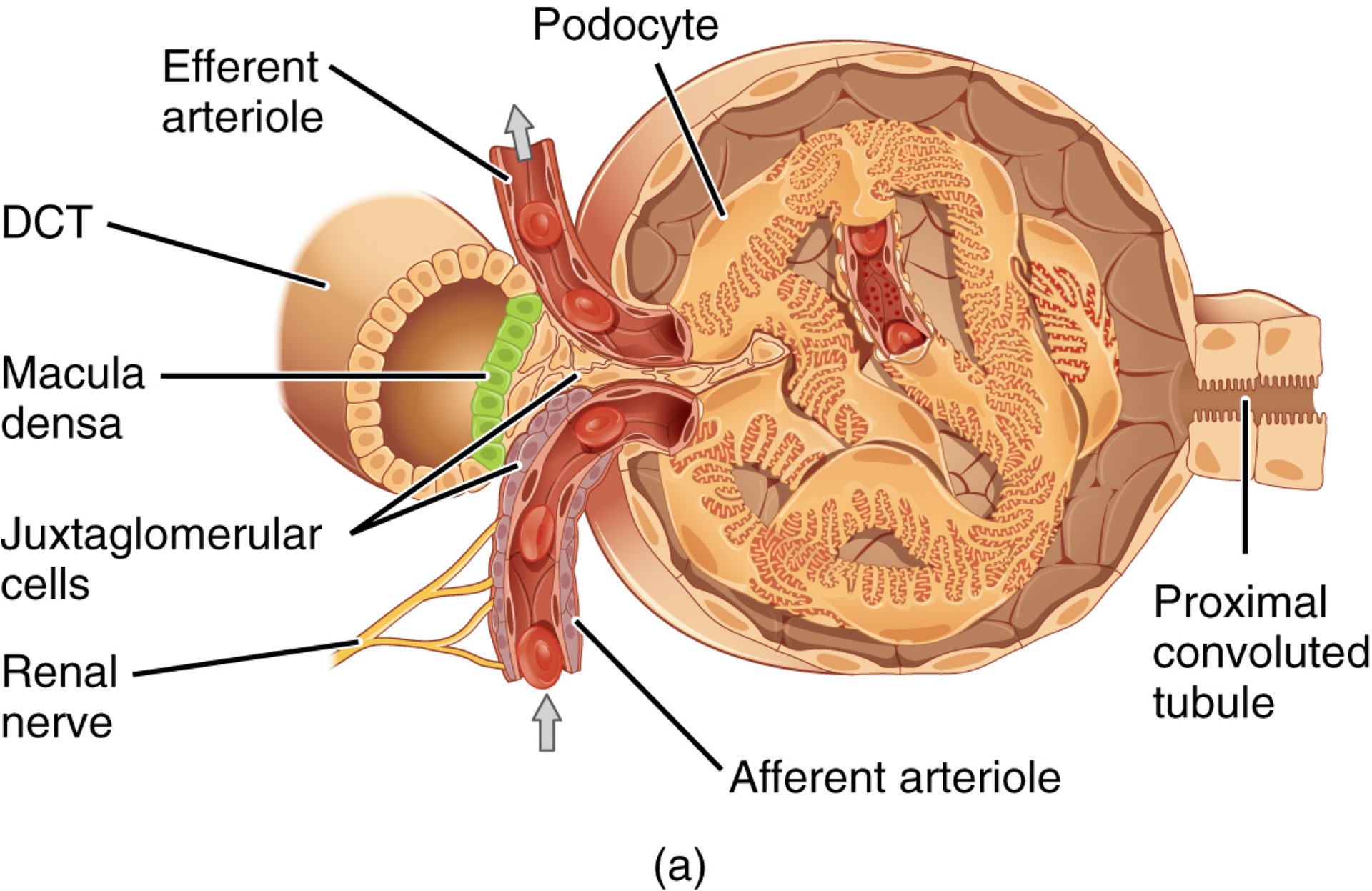
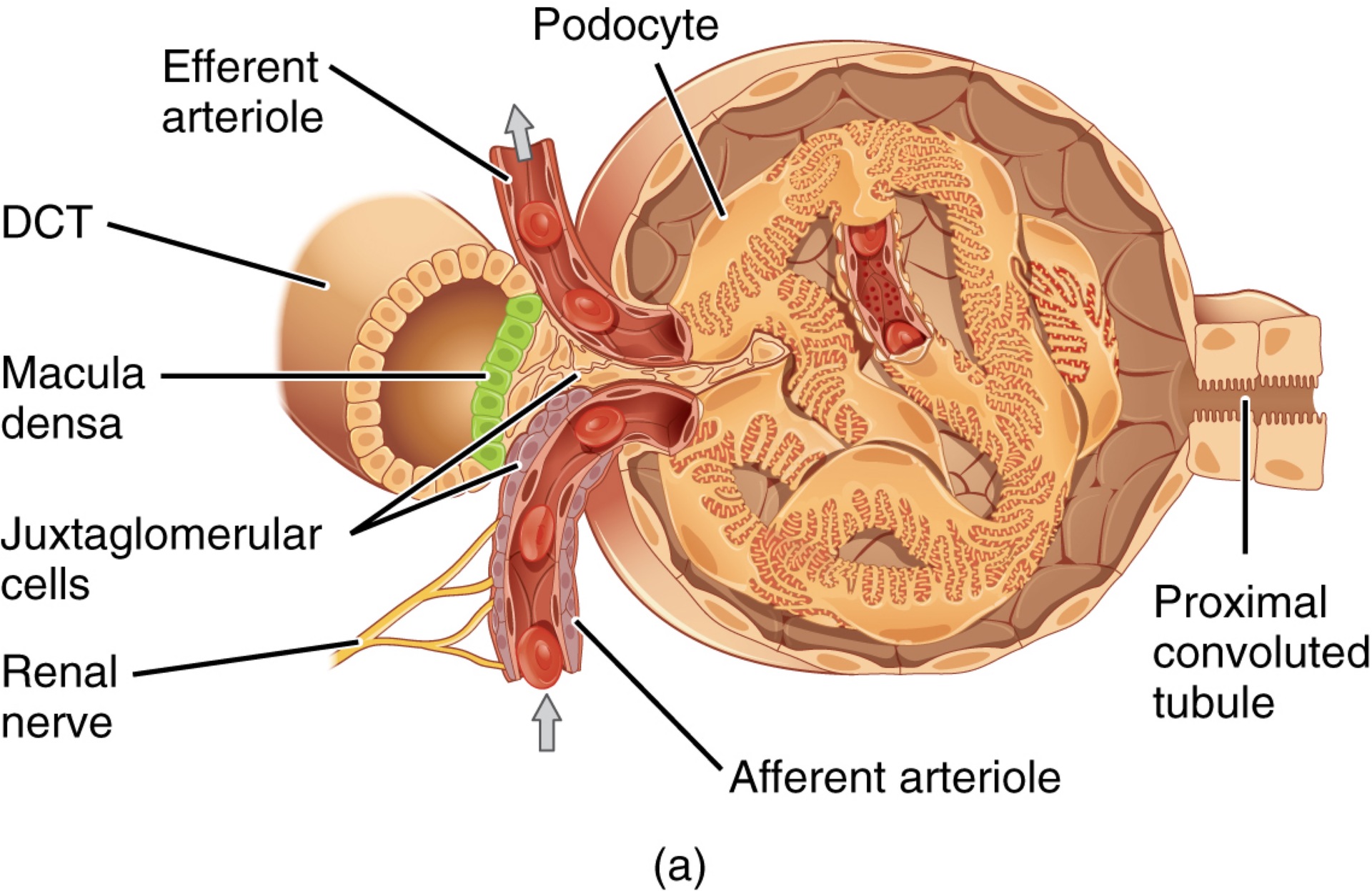
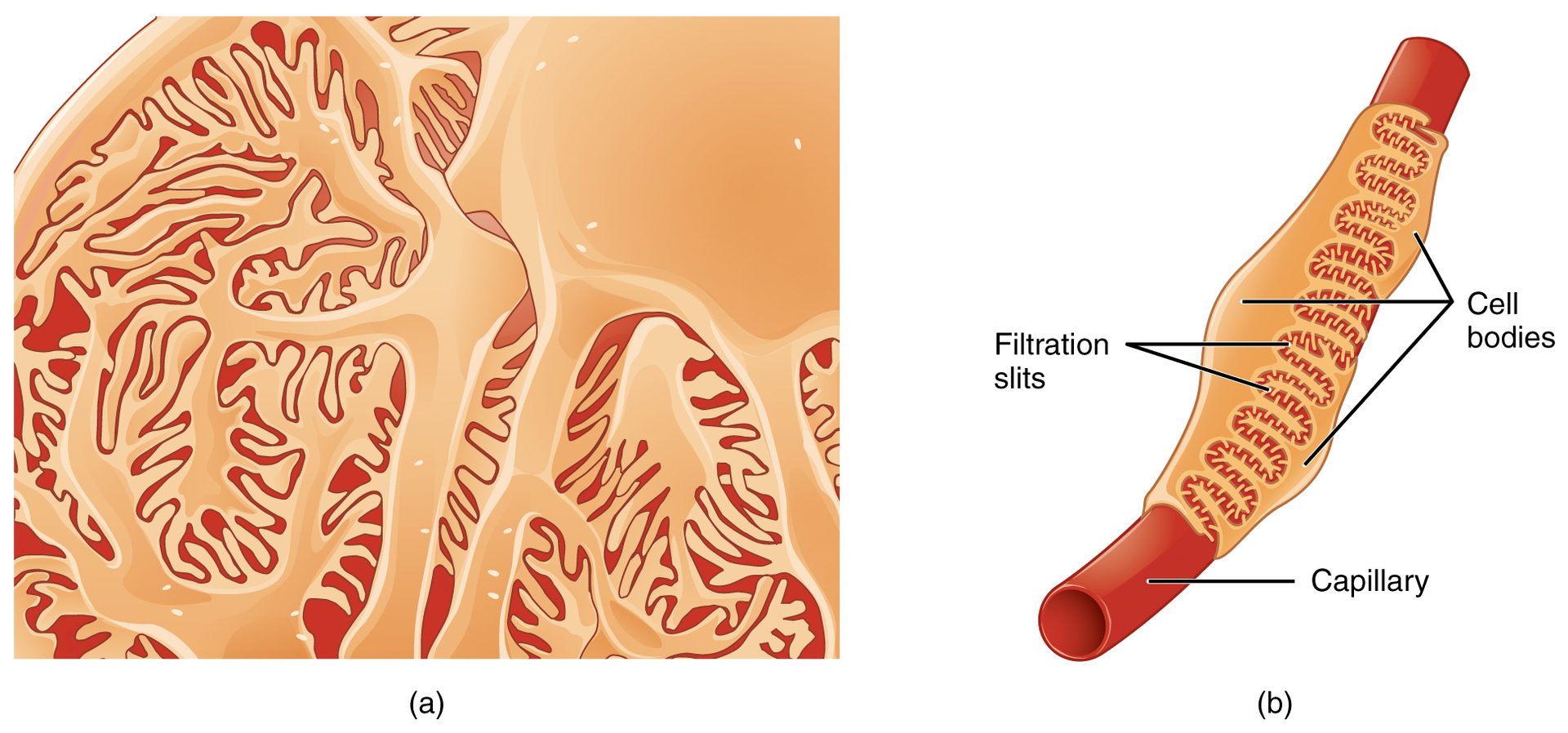
Q: What are podocytes and their function in the glomerulus?
A: Specialized cells with pedicels that interdigitate to form filtration slits, regulating the passage of substances into Bowman’s capsule.
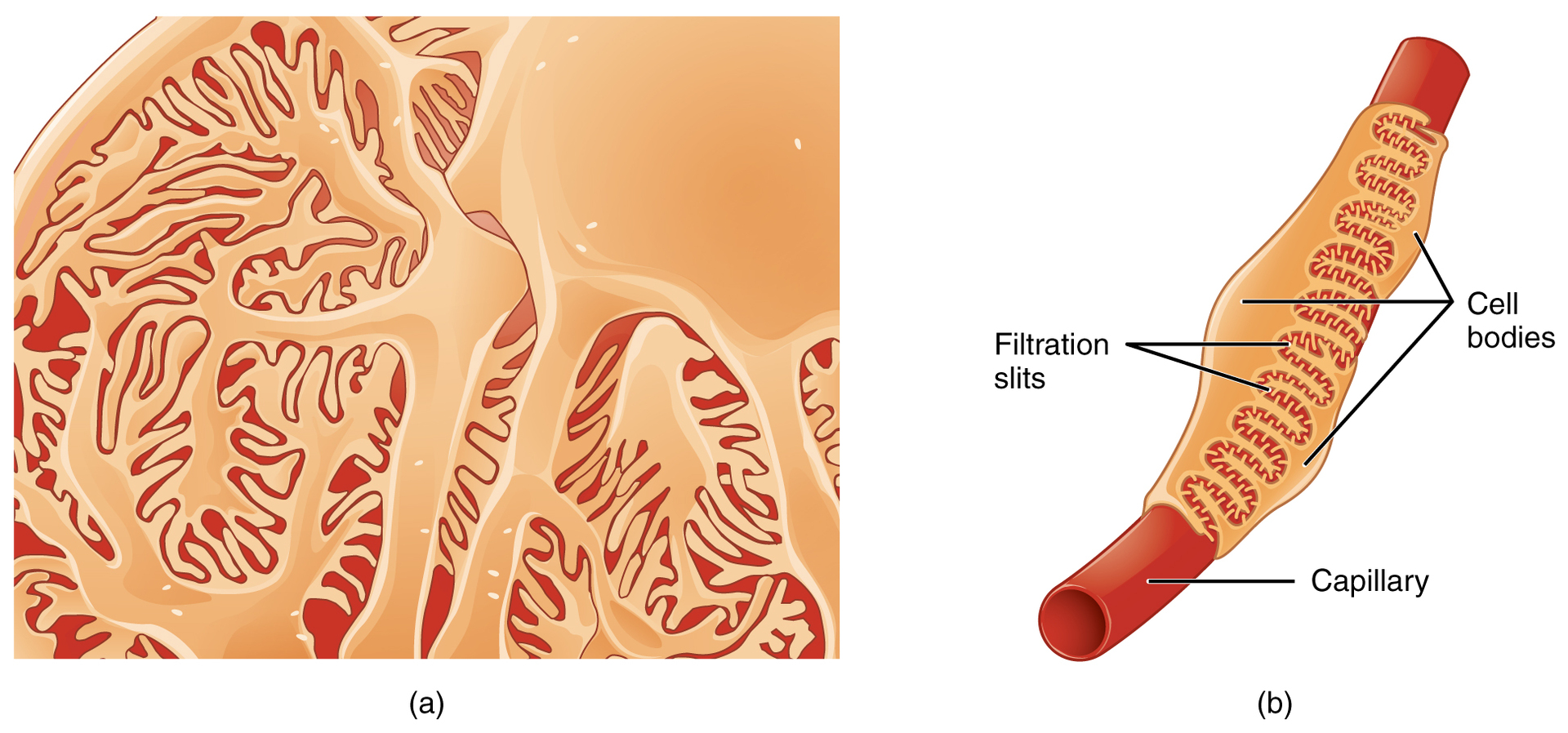
Q: What is the filtration membrane composed of?
A: Fenestrated endothelium, basement membrane, and podocyte filtration slits.
Q: What size and charge characteristics determine whether a substance passes the filtration membrane?
A: Substances <4 nm pass freely; most up to 8 nm may pass; negatively charged molecules are repelled, while positively charged molecules pass more easily.
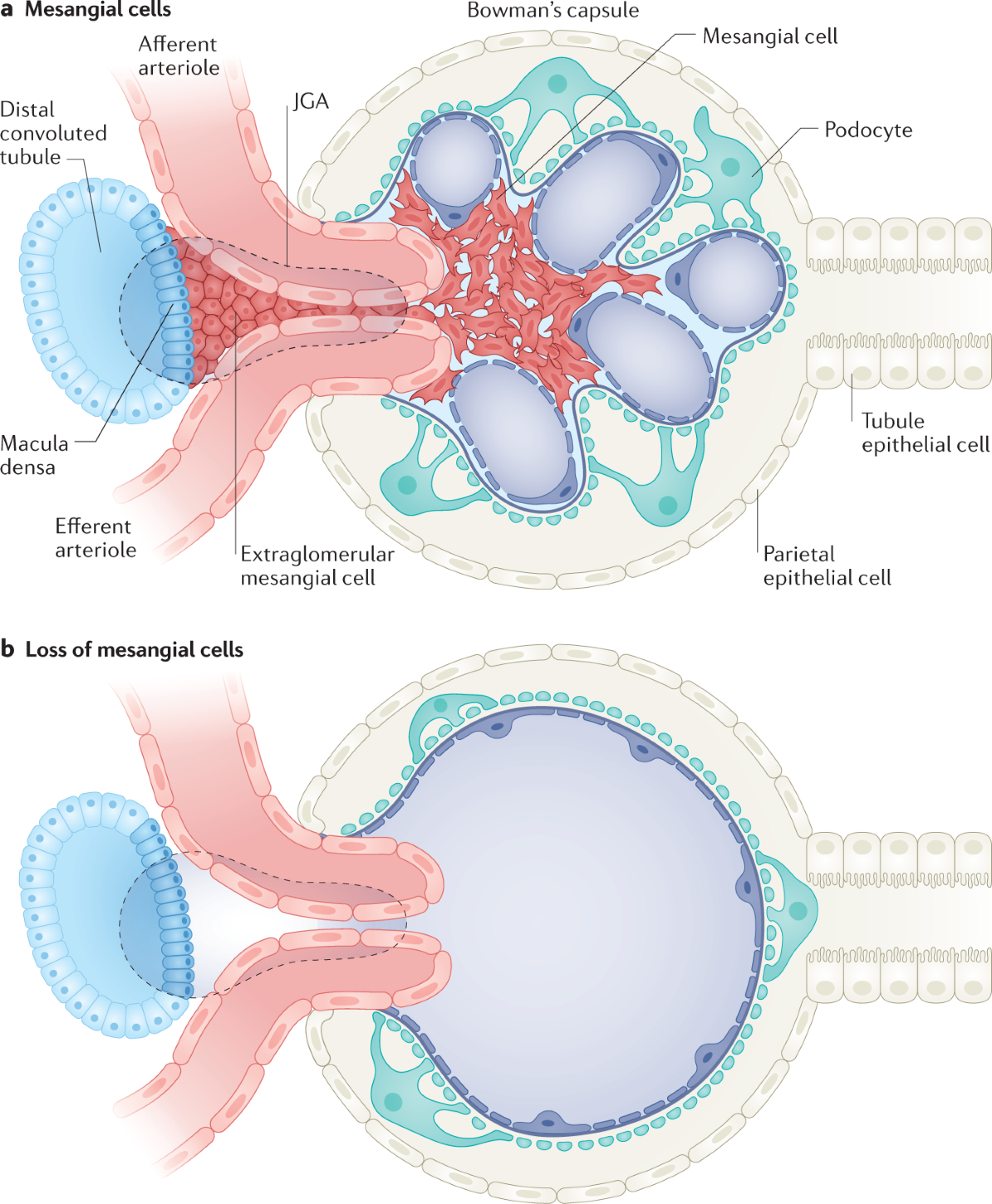
Q: What are mesangial cells and their function?
A: Contractile cells in the glomerulus that help regulate the rate of filtration.
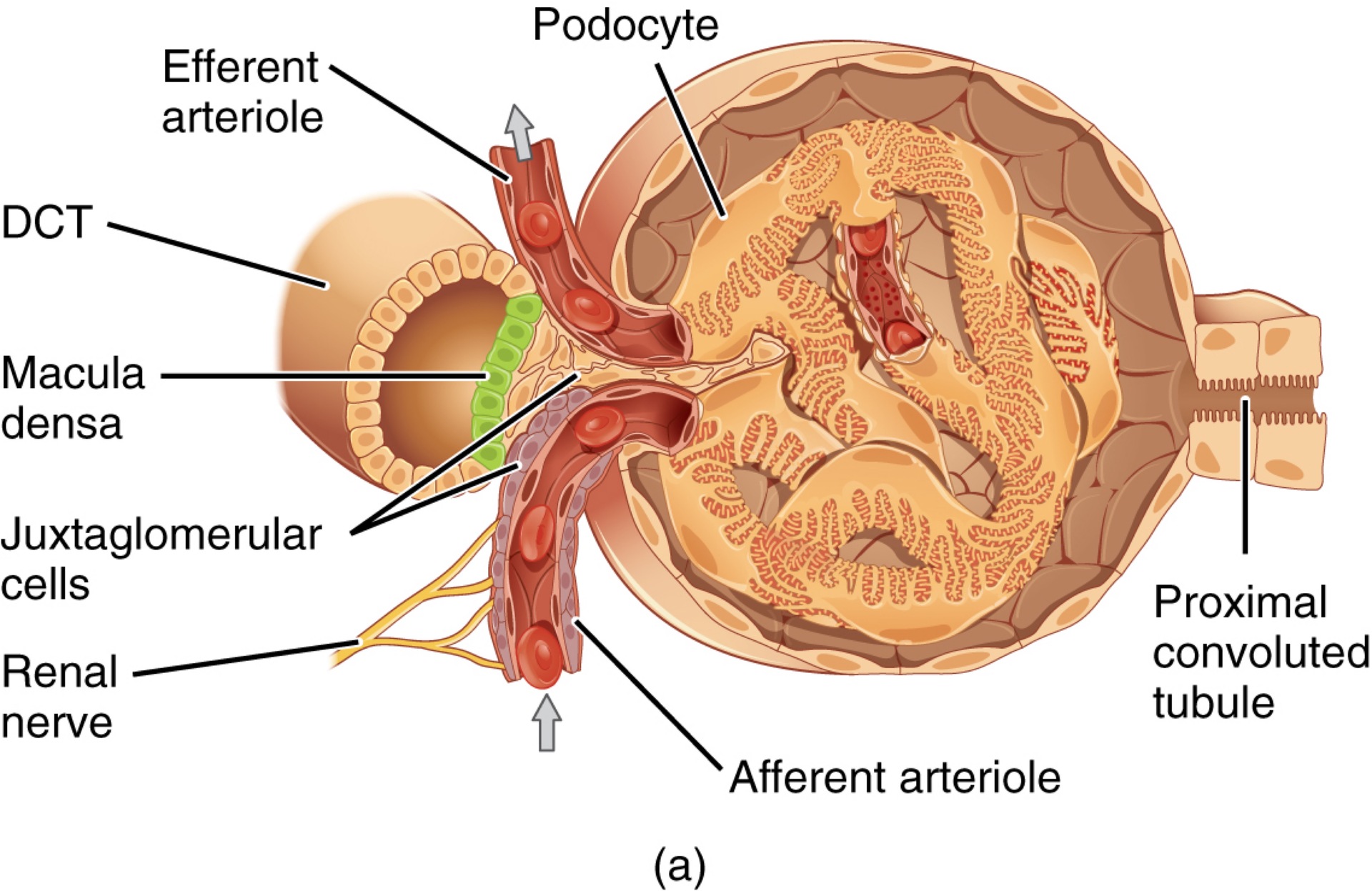
Q: What is the juxtaglomerular apparatus (JGA)?
A: A structure near the glomerulus where the DCT contacts afferent and efferent arterioles; it regulates GFR and renin release.
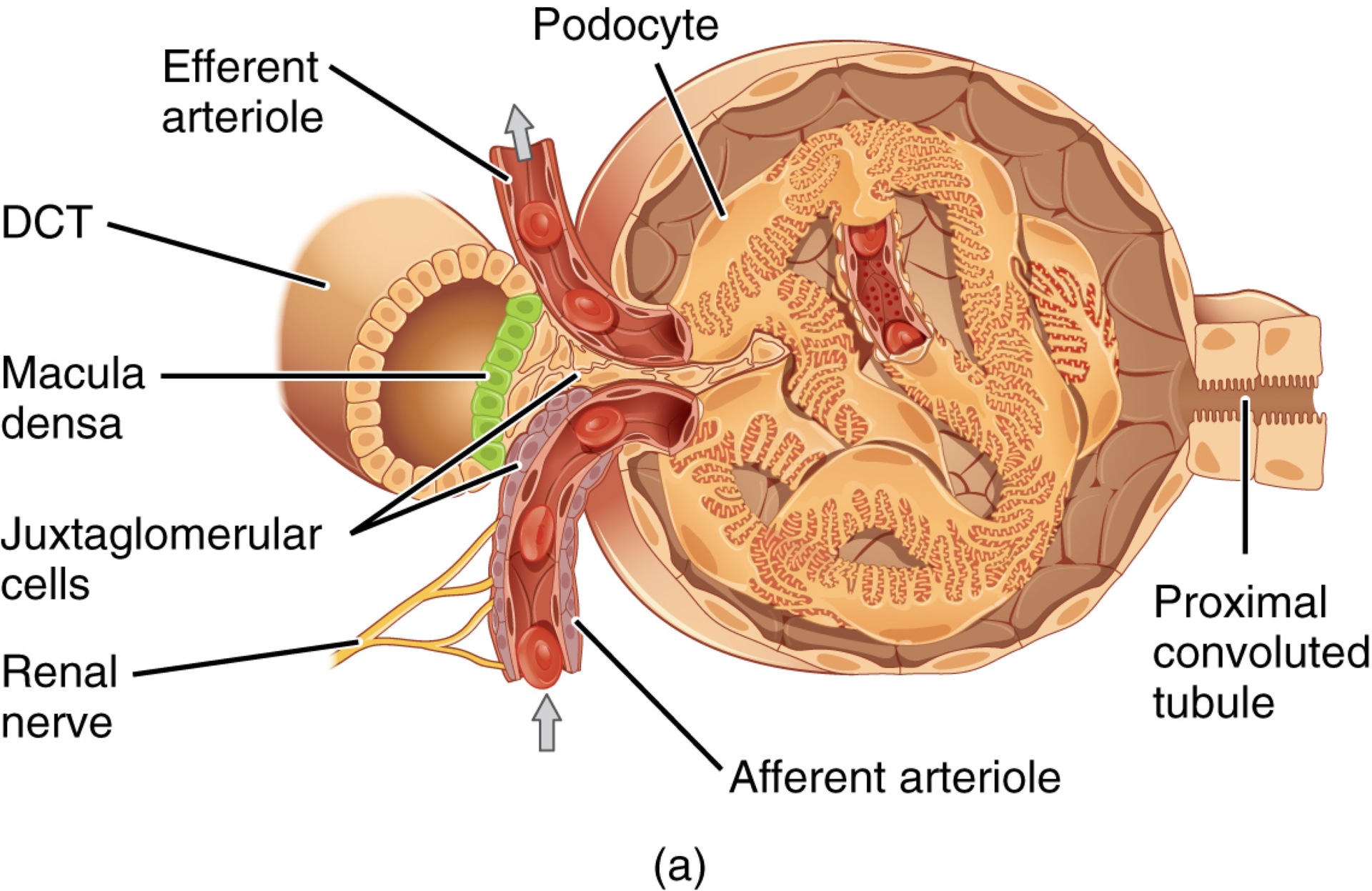
Q: What is the macula densa?
A: A group of cuboidal epithelial cells in the DCT that detect Na⁺ concentration and flow rate, releasing paracrine signals (ATP, adenosine) to regulate GFR.
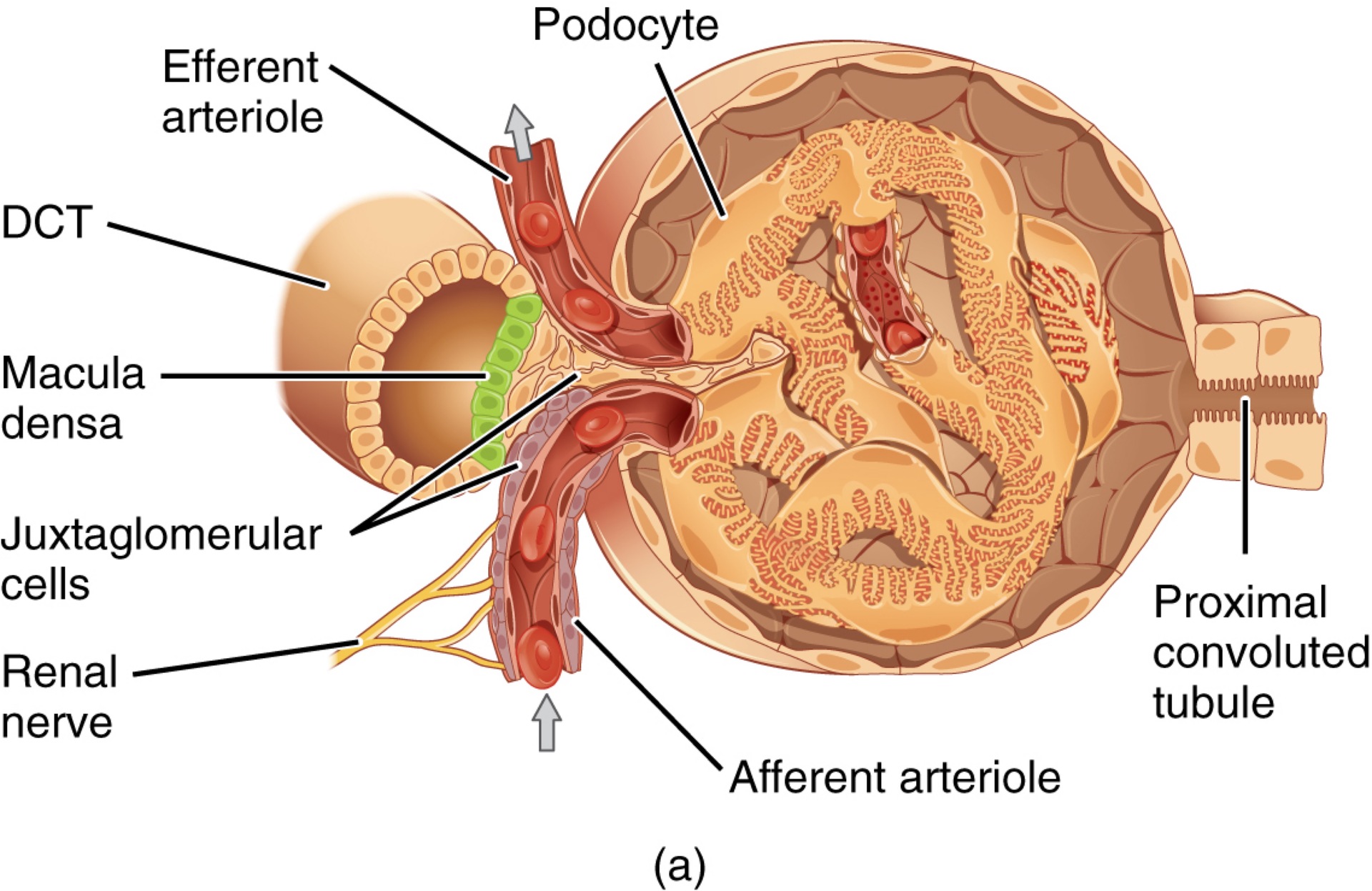
Q: What are juxtaglomerular cells?
A: Modified smooth muscle cells in the afferent arteriole that contract/relax in response to signals from the macula densa and secrete renin.
Q: How does the JGA regulate blood osmolarity and urine output?
A: High osmolarity → JG cells contract → ↓GFR → fluid retained;
Low osmolarity → JG cells relax → ↑GFR → fluid excreted.
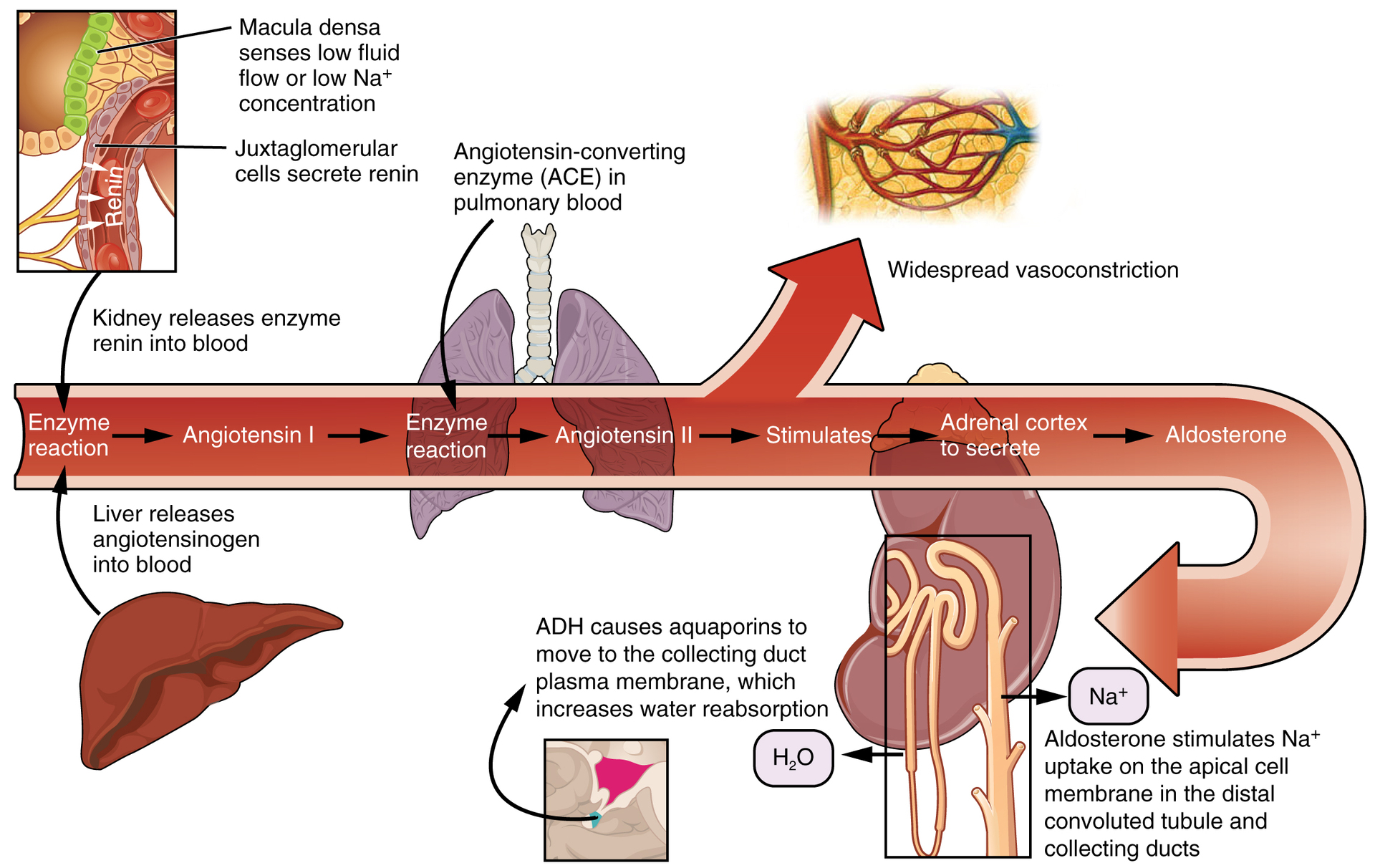
Q: How does renin influence blood pressure?
A: Renin converts angiotensinogen → angiotensin I → (via ACE) angiotensin II → vasoconstriction + aldosterone release → ↑Na⁺ reabsorption → ↑water retention → ↑BP.
Which substance directly causes vasoconstriction, thus increasing blood pressure?
Renin
Angiotensinogen
Angiotensin II
Angiotensin-converting enzyme
Angiotensin II
Q: What are podocytes and what do they form?
A: Cells forming finger-like processes (pedicels); they make up the visceral layer of Bowman’s capsule and contribute to the filtration membrane.
Q: What are pedicels and what is their role in filtration?
A: Finger-like projections from podocytes that interdigitate around glomerular capillaries to form filtration slits.
Q: What are filtration slits and what determines what passes through them?
A: Gaps between interdigitating pedicels of podocytes where substances are filtered based on size.
Q: What is a fenestration?
A: A pore or opening, especially in capillary endothelial cells, that permits filtration of small solutes while blocking cells and large proteins.
Q: What is angiotensinogen and where is it produced?
A: An inactive protein precursor to angiotensin I, produced by the liver.
Q: How is angiotensin I formed and what is its role?
A: Formed when renin acts on angiotensinogen; it is an inactive precursor to angiotensin II.
Q: What is ACE and what does it do?
A: Angiotensin-converting enzyme from the lungs that converts angiotensin I into active angiotensin II.
Q: What does angiotensin II do?
A: Causes vasoconstriction and stimulates aldosterone release from the adrenal cortex to raise blood pressure.
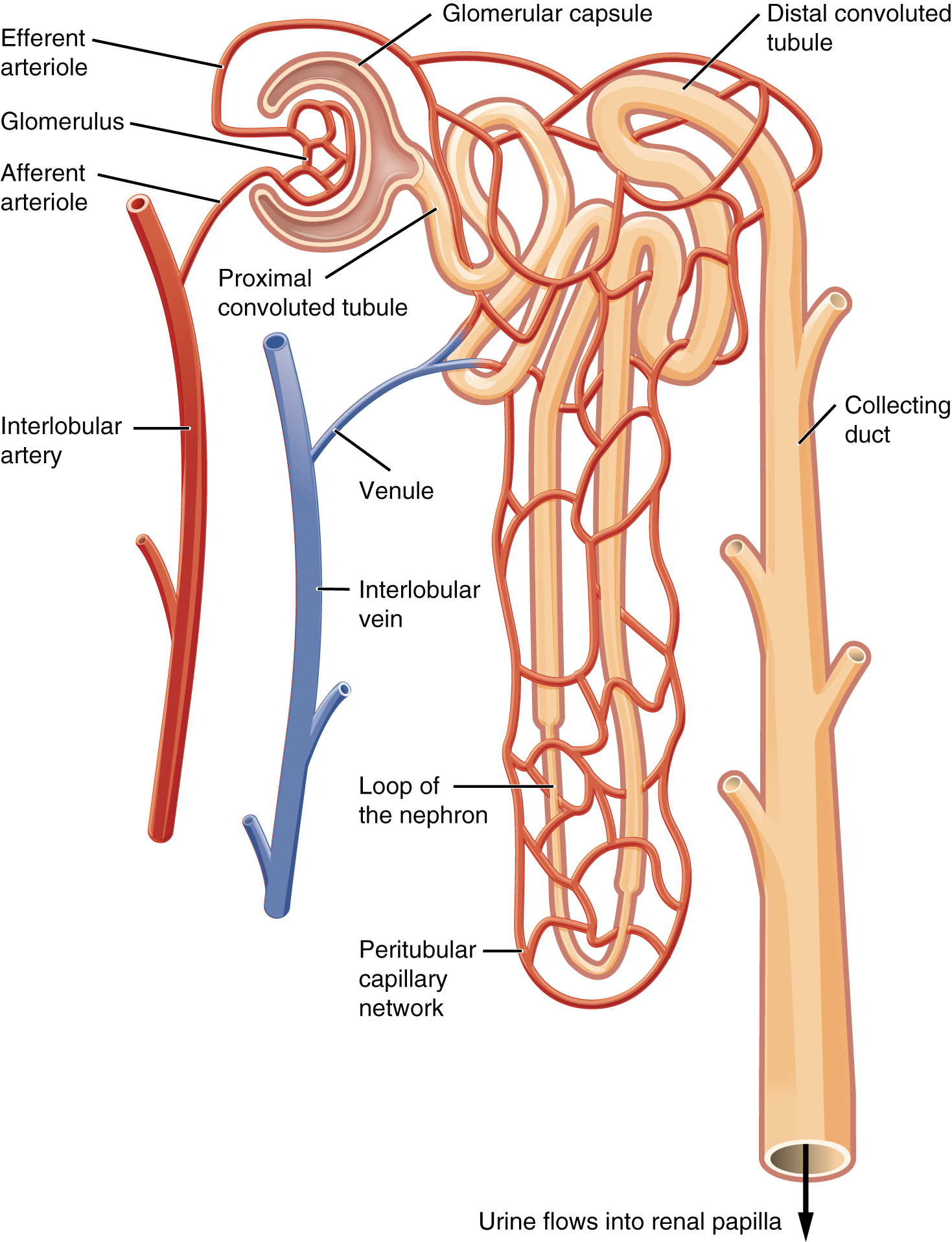
Q: What is the primary function of the proximal convoluted tubule (PCT)?
A: Reabsorption and secretion of solutes like Na⁺, Cl⁻, and glucose; it's the most active nephron segment in these processes.
Q: What structural features of the PCT aid in its function?
A: Simple cuboidal epithelium with a brush border of microvilli and numerous mitochondria for active transport.
Q: What is the loop of Henle and how is it structurally divided?
A: A U-shaped tubule with descending and ascending limbs; descending limb has thick (cuboidal) and thin (squamous) segments, and ascending limb has thin and thick (cuboidal) segments.
Q: Why is the epithelium type in the loop of Henle important?
A: Different epithelium types (cuboidal vs. squamous) correlate with varying permeability to water and solutes.
Q: What is the main functional difference between the PCT and DCT?
A: Both perform reabsorption and secretion, but the DCT is less active, with fewer microvilli and mitochondria than the PCT.
Q: What is the function of the collecting ducts in the kidney?
A: They collect filtrate from multiple nephrons and perform final urine modification, especially water reabsorption under ADH control.
Q: How does ADH affect the collecting ducts?
A: ADH stimulates insertion of aquaporins, increasing water reabsorption and reducing urine volume.
Q: What are aquaporins and their function in the kidney?
A: Water channel proteins that facilitate water reabsorption; their activity in collecting ducts is regulated by ADH.
Q: What is the brush border and where is it found in the nephron?
A: A dense array of microvilli on the apical surface of PCT cells that increases surface area for absorption.
When ADH is released, in which section of the nephron do aquaporin channels develop?
Glomerulus
Bowman’s capsule
Proximal convoluted tubule
Collecting duct
Collecting duct
Q: What vessel carries blood away from the glomerulus?
A: The efferent arteriole.
Q: What capillaries arise from efferent arterioles and supply the renal cortex?
A: Peritubular capillaries.
Q: What is the function of peritubular capillaries?
A: To supply the proximal and distal convoluted tubules in the renal cortex and facilitate reabsorption and secretion.
Q: What capillaries supply the renal medulla and arise from efferent arterioles?
A: Vasa recta.
Q: What is the structural characteristic of the vasa recta?
A: Long, looping capillaries that run parallel to the loops of Henle.
Which statement is correct about vasa recta?
They arise from the aorta.
They arise from the afferent arteriole.
They arise from the renal artery.
They arise from the efferent arteriole.
They arise from the efferent arteriole.
Which structure anchors the kidneys to the peritoneum and the posterior abdominal wall?
Pararenal fat
Perirenal fat
Renal fascia
Renal capsule
Renal fascia
What is the correct sequence of the segments of the renal tubule?
Distal tubule, loop of Henle, proximal tubule
Proximal tubule, loop of Henle, distal tubule
Loop of Henle, proximal tubule, distal tubule
Proximal tubule, distal tubule, loop of Henle
Proximal tubule, loop of Henle, distal tubule
What are the functional units of kidneys that regulate volume and solute concentration and remove waste from the blood?
Renal medulla
Nephrons
Juxtaglomerular apparatus
Renal columns
Nephrons
Where does the renal artery enter the kidney?
Renal papilla
Renal hilum
Renal medulla
Renal pelvis
Renal hilum
What is the correct sequence of blood flow through the kidneys on its route to the glomeruli of the nephrons?
Renal artery, segmental artery, interlobular (cortical radiate) artery, arcuate artery, interlobar artery, afferent arteriole
Renal artery, segmental artery, interlobar artery, arcuate artery, interlobular (cortical radiate) artery, afferent arteriole
Renal artery, segmental artery, interlobar artery, interlobular (cortical radiate) artery, arcuate artery, afferent arteriole
Renal artery, segmental artery, interlobular artery, interlobar (cortical radiate) artery, arcuate artery, afferent arteriole
Renal artery, segmental artery, interlobar artery, arcuate artery, interlobular (cortical radiate) artery, afferent arteriole
Q: What part of the nephron is responsible for filtering the blood?
A: The glomerulus.
Q: What is excluded from the filtrate during glomerular filtration?
A: Large particles like red blood cells, platelets, antibodies, and albumin.
Q: How much filtrate is produced daily by the kidneys?
A: About 200 liters.
Q: How much urine is excreted per day under normal conditions?
A: 750–2000 mL.
Q: What pigment gives urine its yellow color?
A: Urochrome.
Q: What does a dark urine color usually indicate?
A: Dehydration or presence of bilirubin.
Q: What is the normal pH range of urine?
A: 4.5–8.0.
Q: What is the normal range of urine specific gravity?
A: 1.003–1.032.
Q: What is the normal range for urine osmolarity?
A: 40–1350 mOsmol/kg.