skeleton and muscle lecture study guide
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
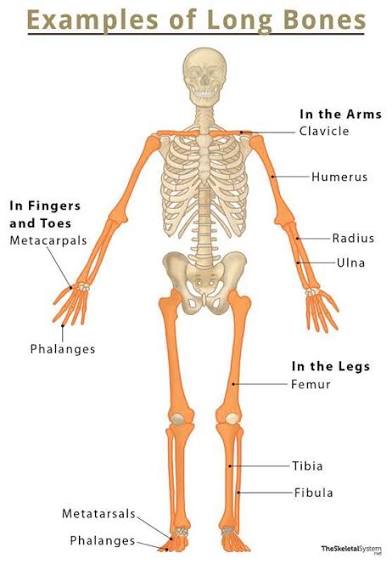
be able to classify bones by shape:
long bones-
Greater in length than width
Example: most limb bones (e.g., humerus, femur, metacarpals)
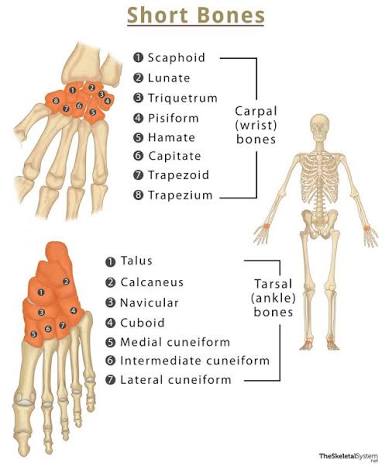
Bone shapes:
short bones-
nearly equal in length and width
Example: wrist and ankle bones (e.g., carpals, tarsals)
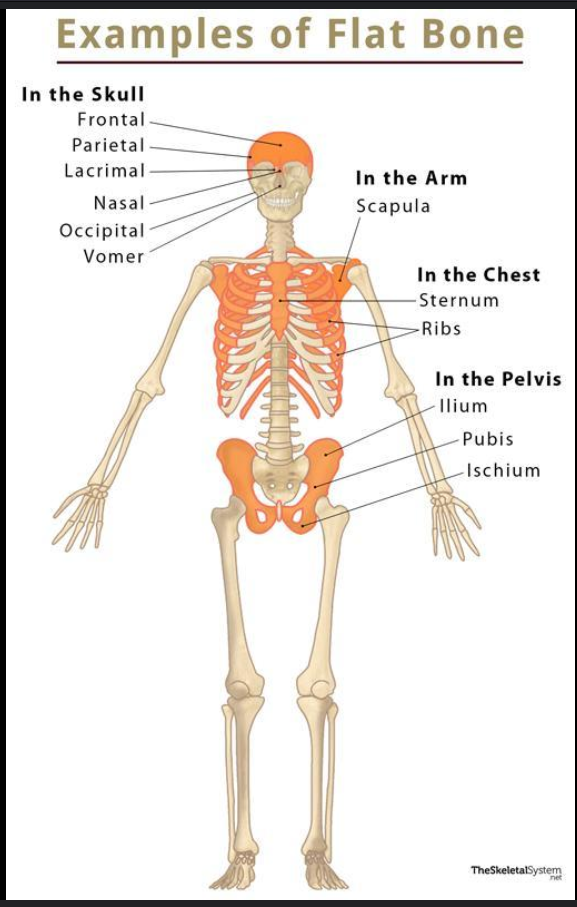
Bone shapes:
flat bones-
Complex shape that does not fit into other classifications
Examples: vertebrae, some skull bones (e.g., ethmoid, sphenoid)
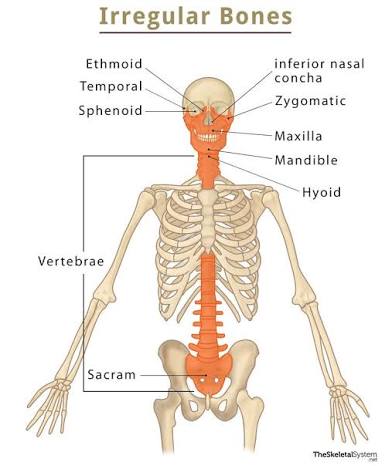
Bone shapes:
irregular bones-
Complex shape that does not fit into other classifications
Examples: vertebrae, some skull bones (e.g., ethmoid, sphenoid)
Bone shapes:
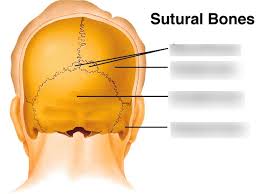
sutural/wormian bones-
Small, flat, oddly shaped bones found between the flat bones of the skull along the sutures. They develop from separate centers of ossification.
Bone shapes:
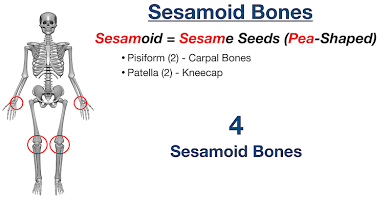
sesamoid bones-
small, sesame seed-shaped bones along the tendons of some muscles, are also classified as short bones.
The patella (kneecap) is the largest sesamoid bone
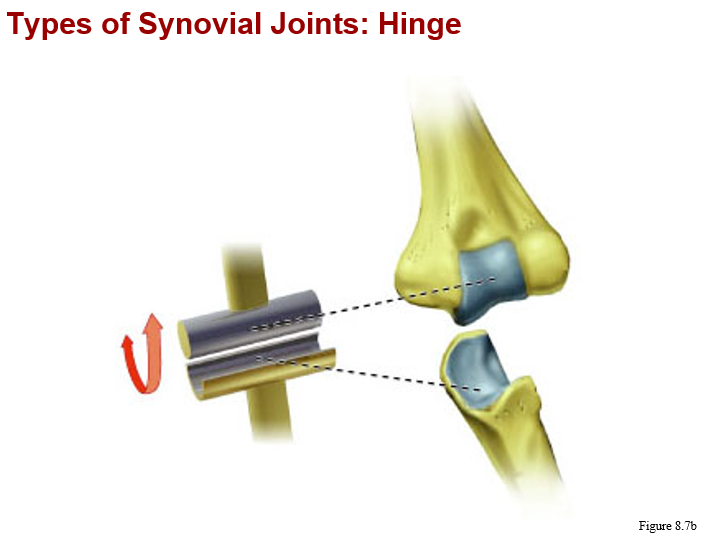
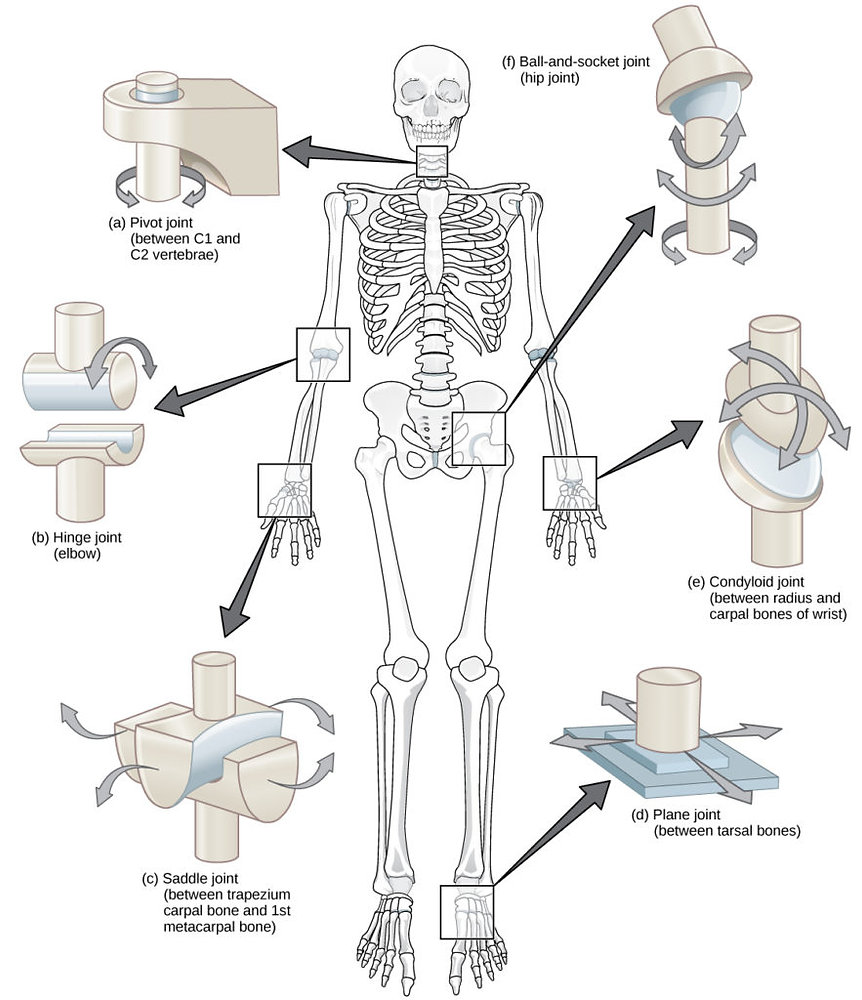
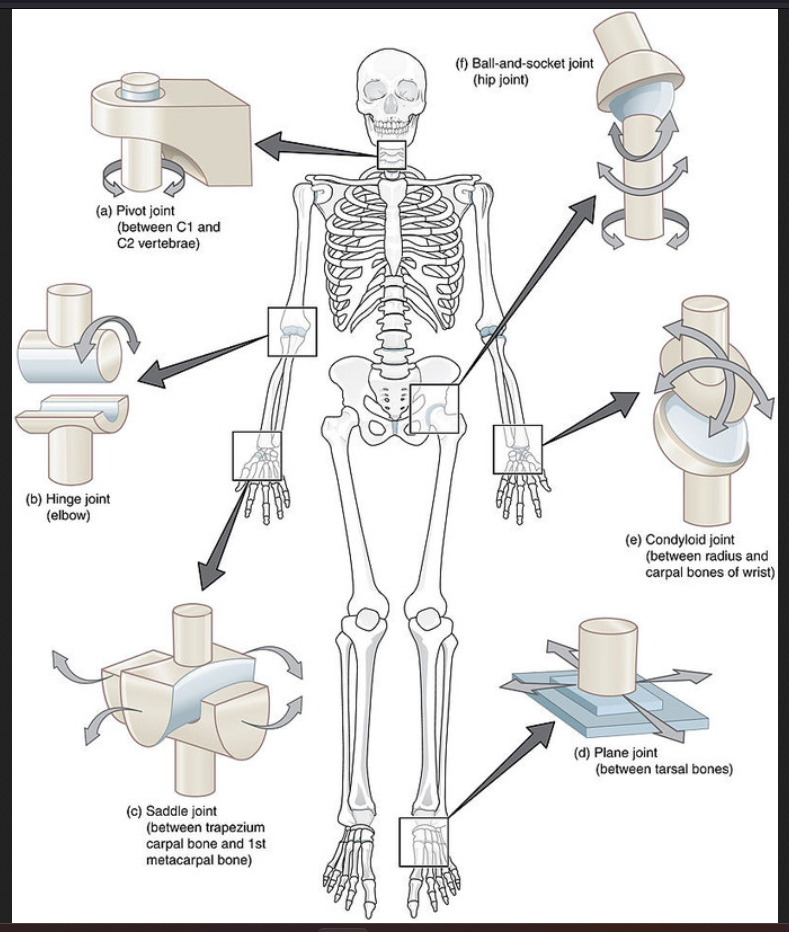
monaxial/uniaxial joints:
hinge
convex feature of one bone fits into concave depression of another bone
knee and elbow joint, IP (interphalangeal) joints
diarthrosis (freely mobile)
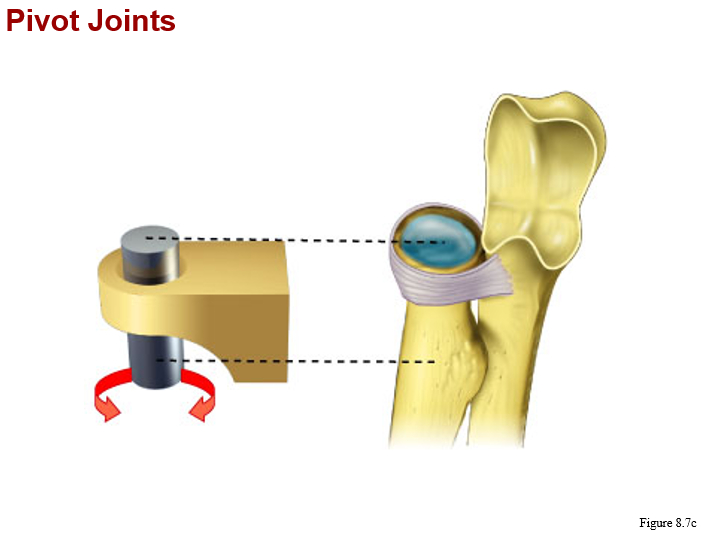
monaxial/uniaxial joints:
pivot
bone with a rounded surface fits into a ring formed by a ligament and another bone
between c1 (atlas) and c2 (axis) vertebrae (atlantoaxial joint), radius and ulna
diarthrosis (freely mobile)
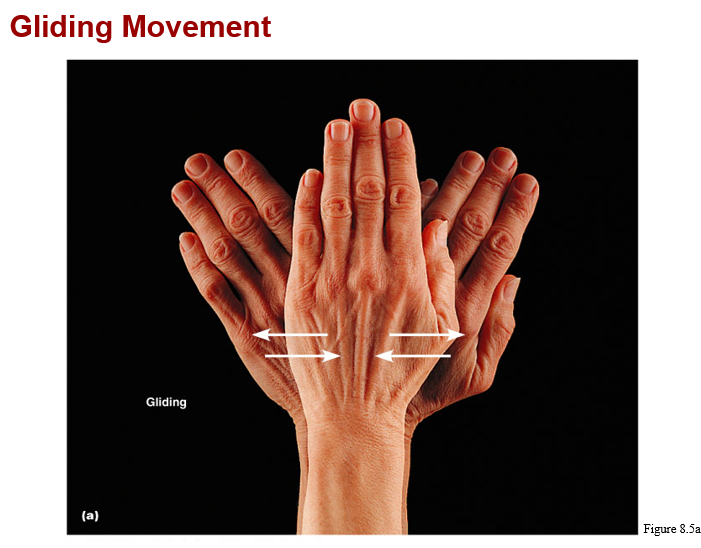
monaxial/uniaxial joints::
gliding (plane)
flattened or slightly curved faces slide across one another
wrist and vertebrae (flat surface), intertarsal joints and some intercarpal joints
diarthrosis (freely mobile)
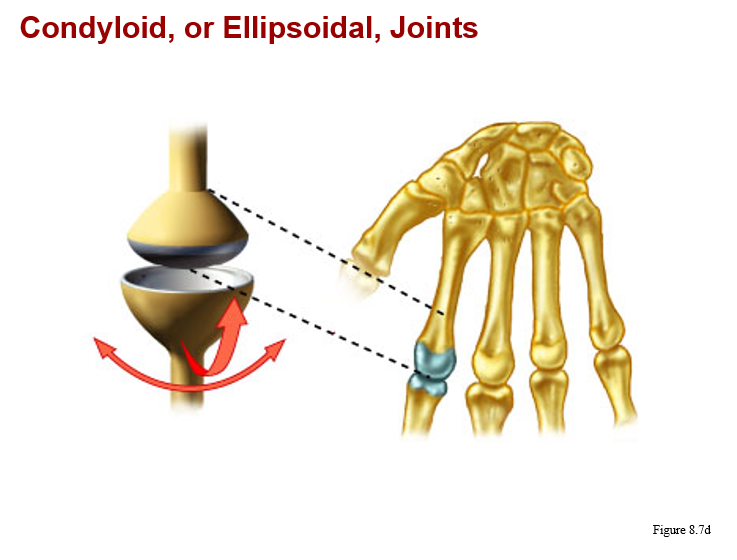
biaxial:
coldyloid (condylar)
oval articular surface on one bone closely interfaces with a depressed oval surface on another bone
metacarpals and phalanges (knuckles), wrist and metacarpophalangeal joints
diarthrosis (freely mobile)
biaxial:
saddle
saddle shaped articular surface on one bone closely interfaces with a saddle shaped surface on another bone
at base of thumb (metacarpal with carpal)
diarthrosis (freely mobile)

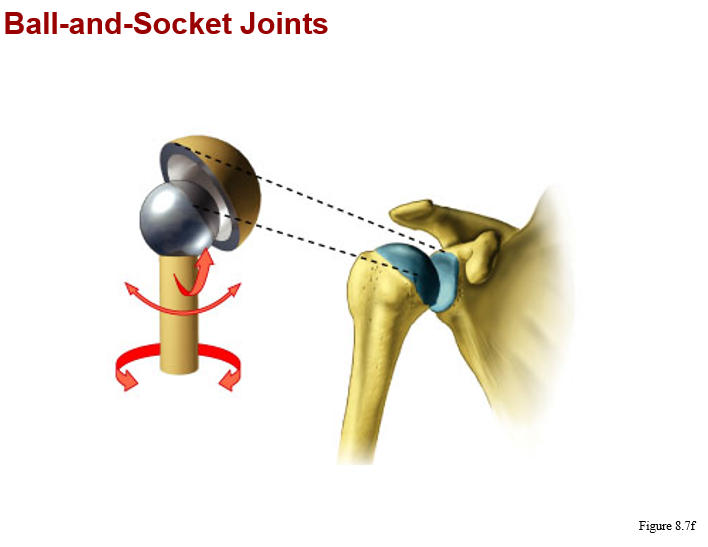
triaxial or multiaxial:
ball and socket
round head of one bone rests within cup-shaped depression in another bone
all ball socket and joints (shoulder, hip)
diarthrosis (freely mobile)
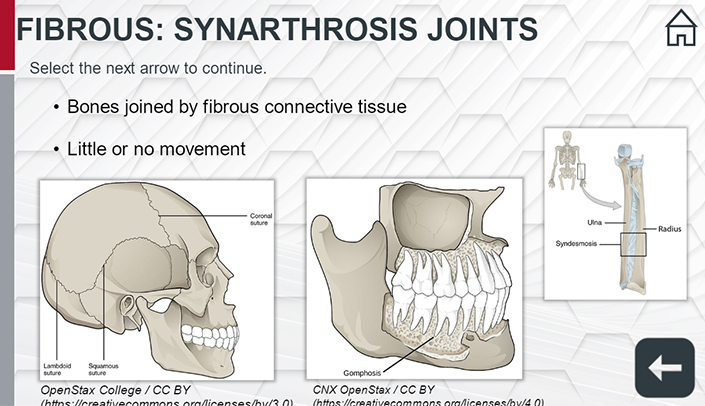
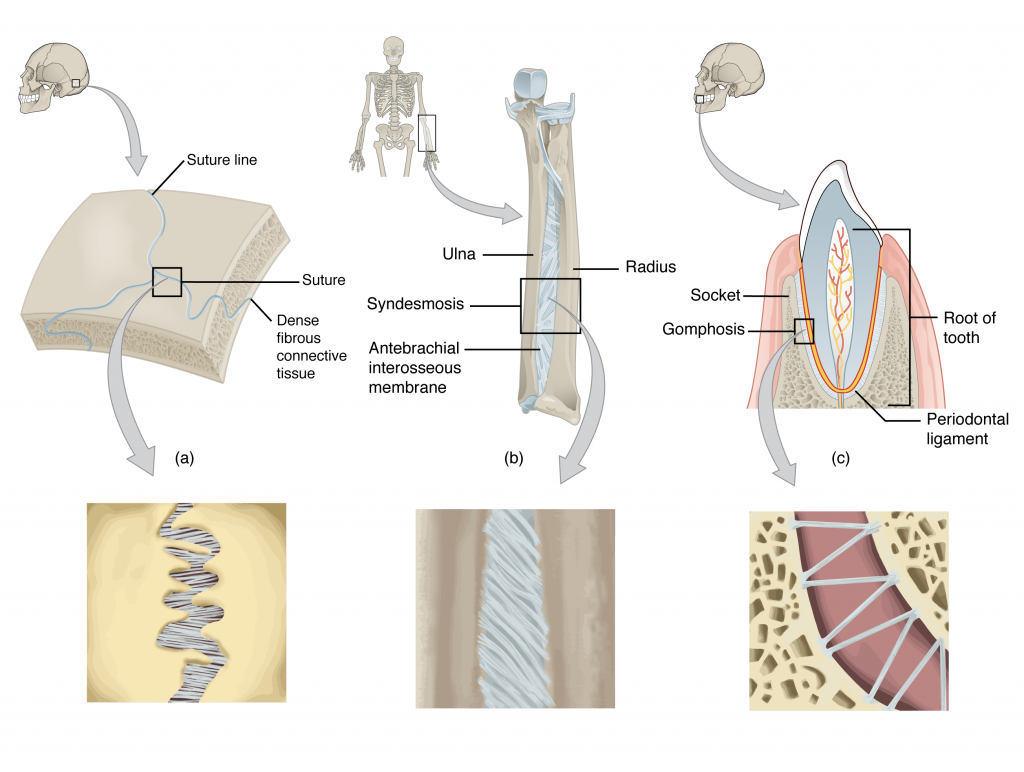
synarthrosis
is an immobile joint.
2 types of fibrous joints and one type of cartilaginous joint are synarthroses
Example:
sutures in the skull, the manubrosternal joint, and gomphoses (tooth sockets)
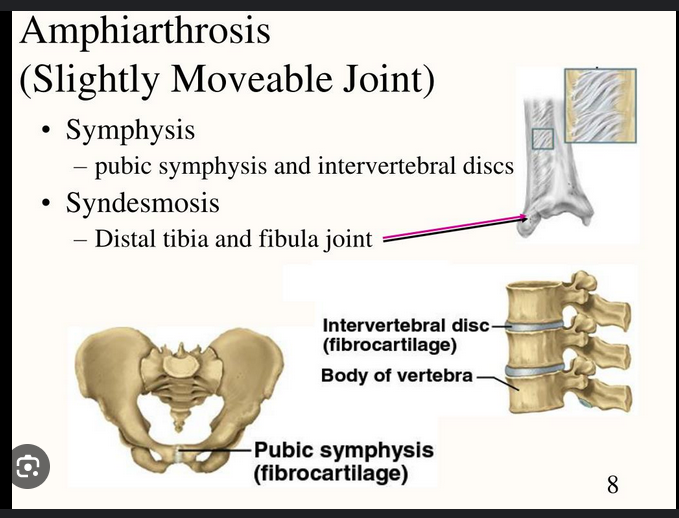
amphiarthrosis
Is a slightly mobile joint.
1 type of fibrous joint and 1 type of cartilaginous joint are amphiarthroses
Example:
pubic symphysis and the joints between vertebral bodies
diarthrosis
freely mobile joint.
all synovial joint are diarthroses
Example:
shoulder, hip, elbow, knee, ankle, wrist, and finger joints
blood flow:
Bone:
Bone is highly vascularized, meaning it has a rich network of blood vessels that supply oxygen and nutrients to bone cells and facilitate the removal of waste products. This vascularity is crucial for bone growth, remodeling, and repair.
Cartilage:
Cartilage, unlike bone, is avascular, meaning it lacks blood vessels. Nutrients and oxygen reach chondrocytes (cartilage cells) through diffusion from the surrounding tissues.
tissue repair
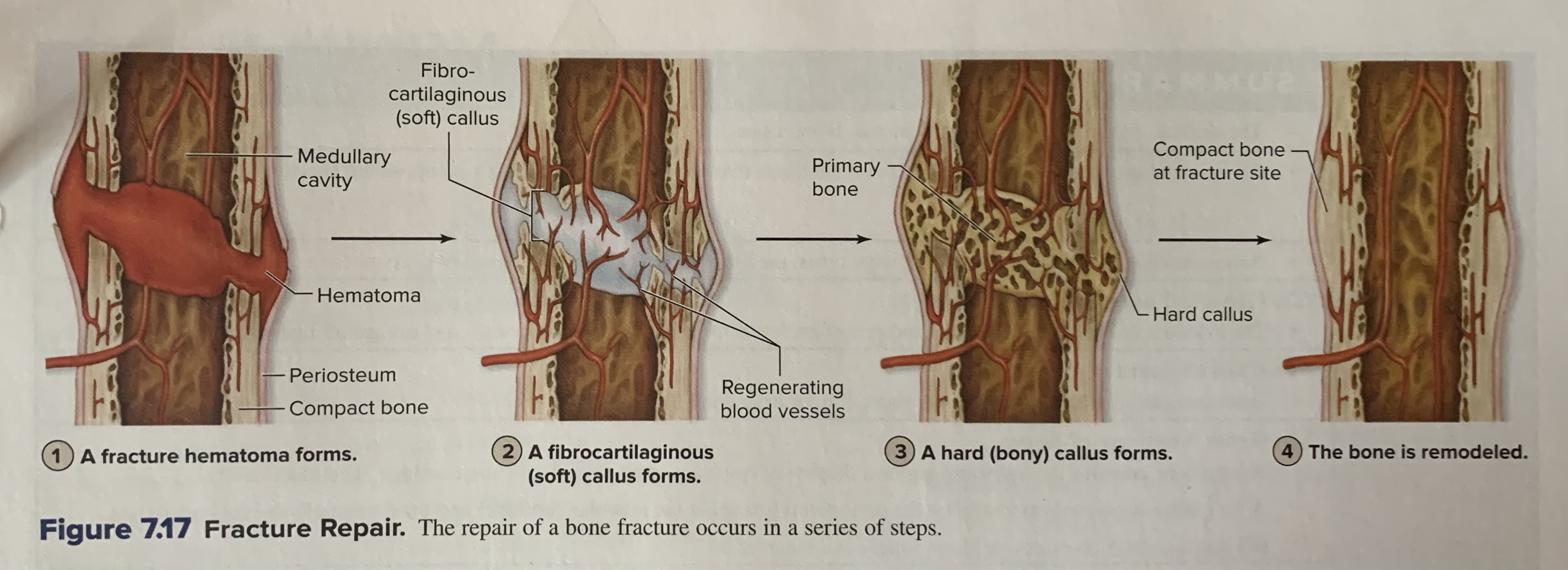
Bone:
Due to its vascularity, bone has a robust capacity for repair, especially after fractures. Bone repair involves a complex process of inflammation, angiogenesis (formation of new blood vessels), and osteogenesis (formation of new bone tissue).
Cartilage:
The avascular nature of cartilage limits its ability to repair itself effectively. Cartilage injuries often heal slowly, and the repaired tissue may not fully restore the original function. Cartilage repair often involves surgical interventions to stimulate chondrogenesis (formation of cartilage) or to replace damaged cartilage
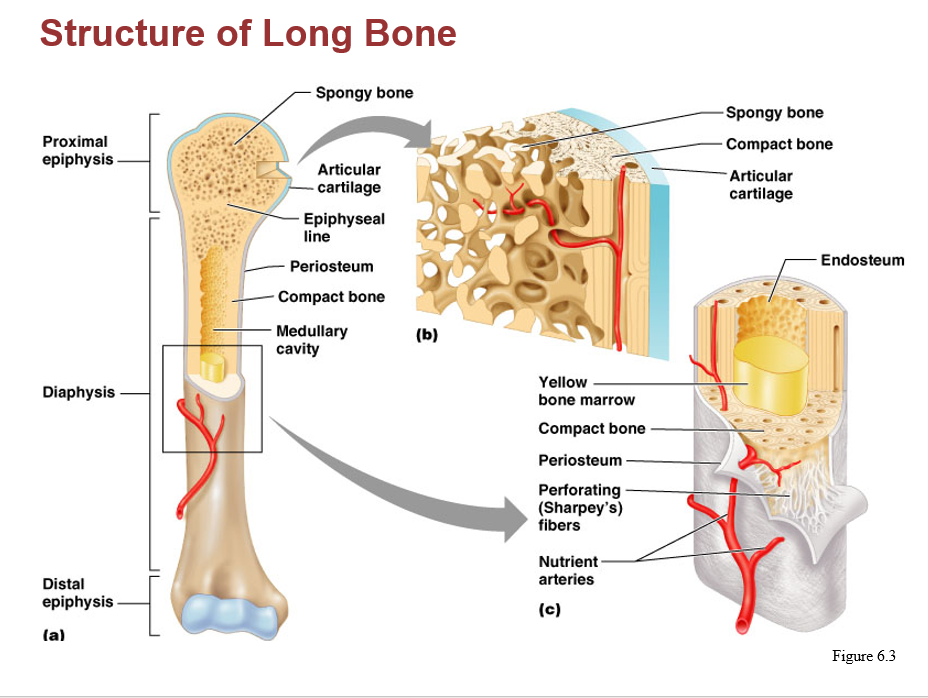
diaphysis:
one of the principal gross features of a long bone is its shaft
elongated, usually cylindrical diaphysis provides for the leverage and major weight support of a long bone.
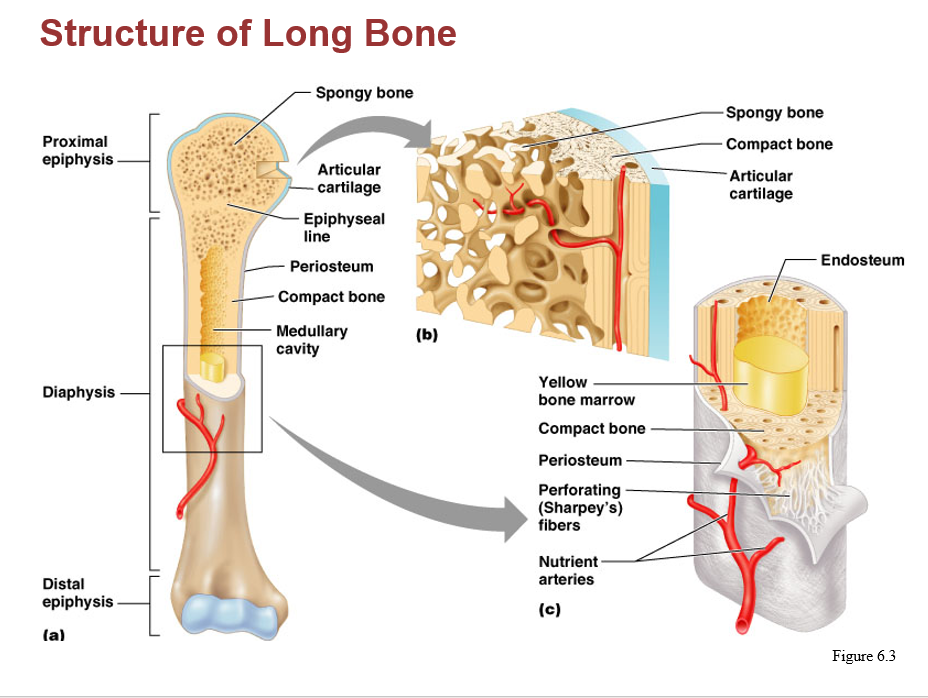
epiphysis:
An expanded, knobby region
Is at each end of a long bone
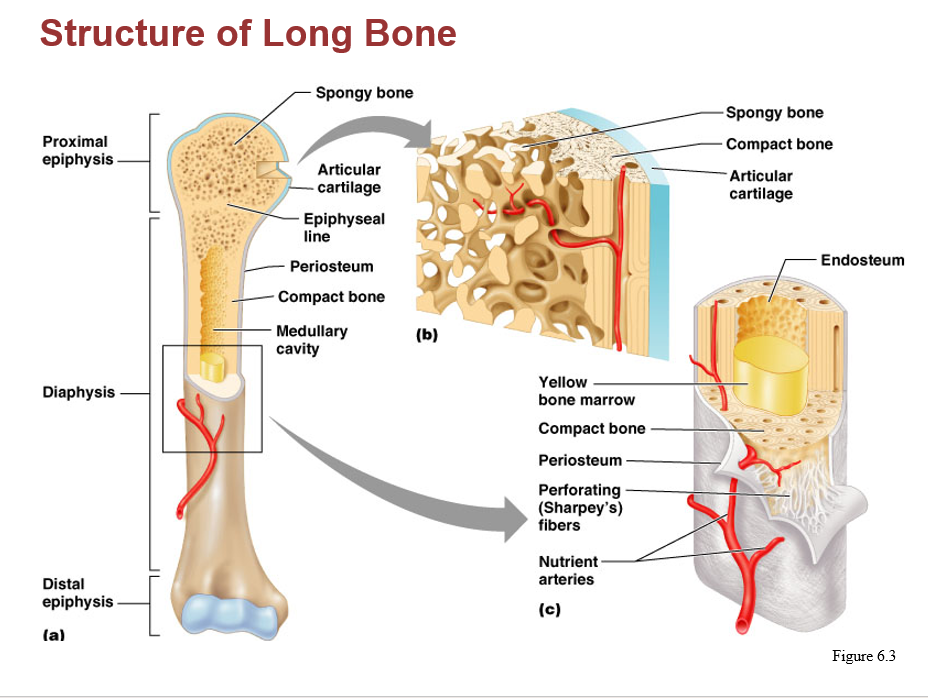
compact bone (a.k.a dense or cortical bone):
is a relatively rigid connective bone tissue that appears white, smooth, and solid.
makes up approx. 80% of the total bone mass
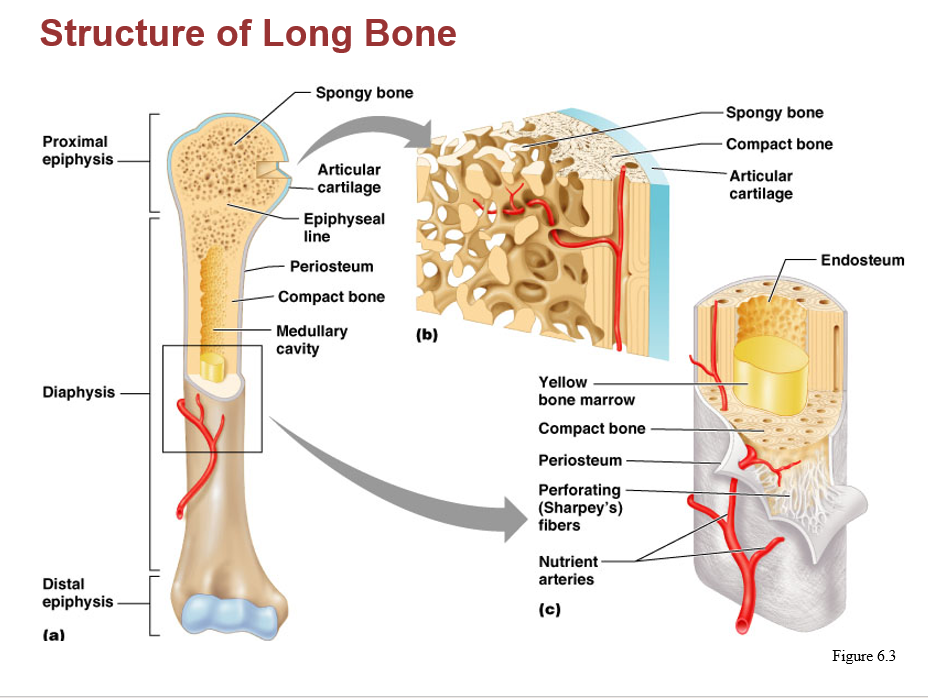
spongy bone (a.k.a cancellous or trabecular bone):
located internal to compact bone, appears porous, and make up approx. 20% of the total bone mass
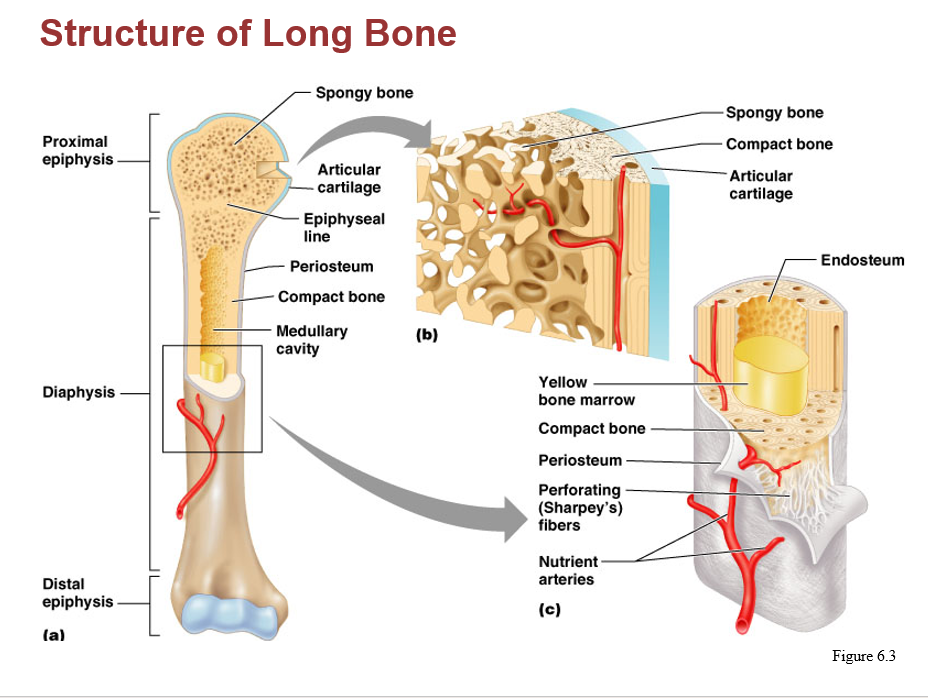
yellow (bone) marrow:
primarily within the medullary cavities of long bones and the inner core of most epiphyses, there is a decrease in developing blood cells and an increase in adipocytes.
Fatty appearing substance
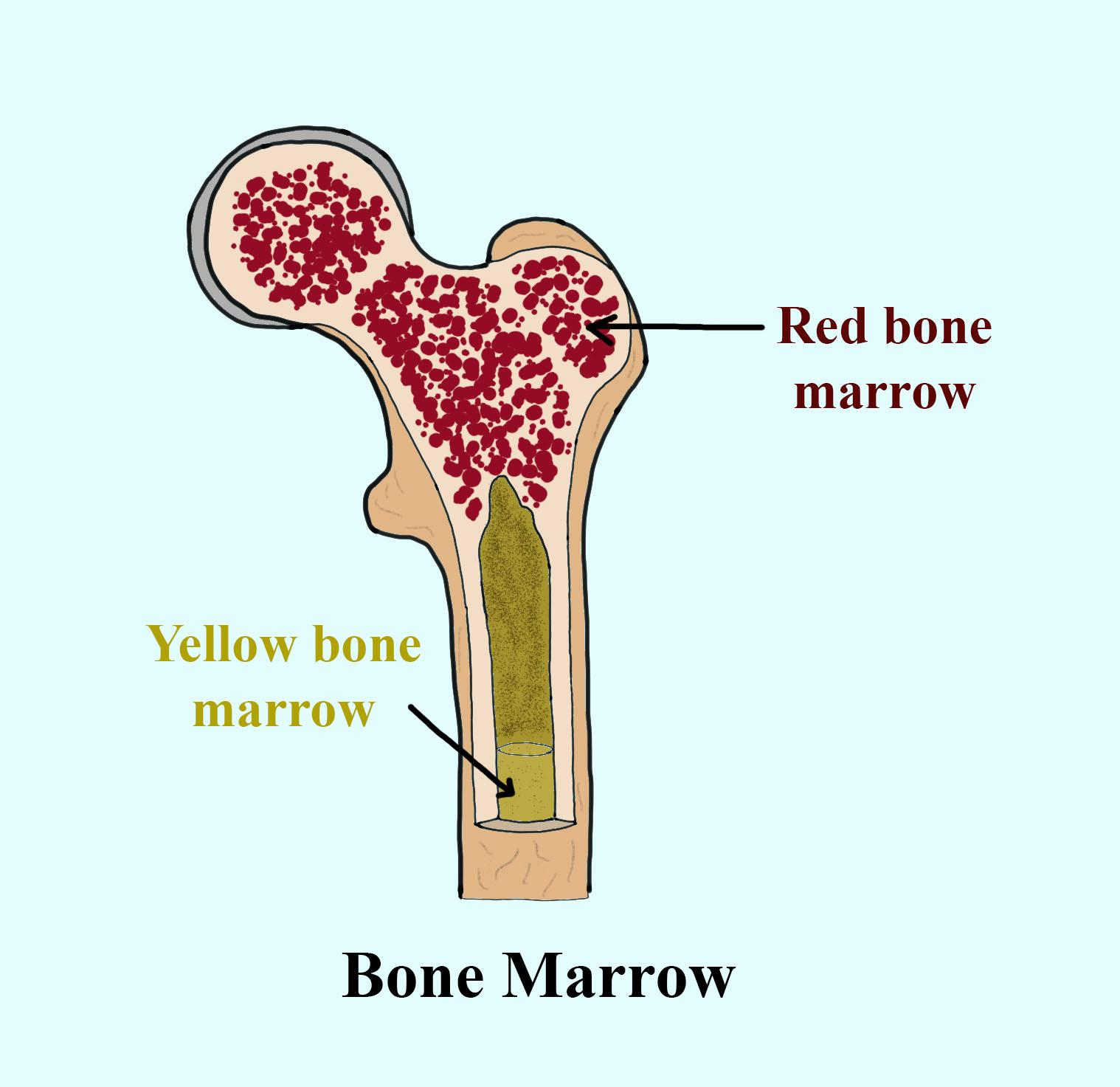
red (bone) marrow (aka myeloid tissue):
contains reticular CT, developing blood cells, and adipocytes. Primary function is forming the blood cells of the body (i.e., it is hematopoietic)
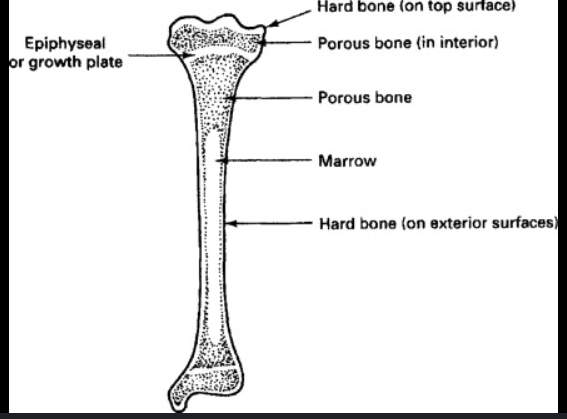
epiphyseal plates:
In a growing bone, this region contains the growth plate. It is a thin layer of hyaline cartilage that provides for the continued lengthwise growth of the bone
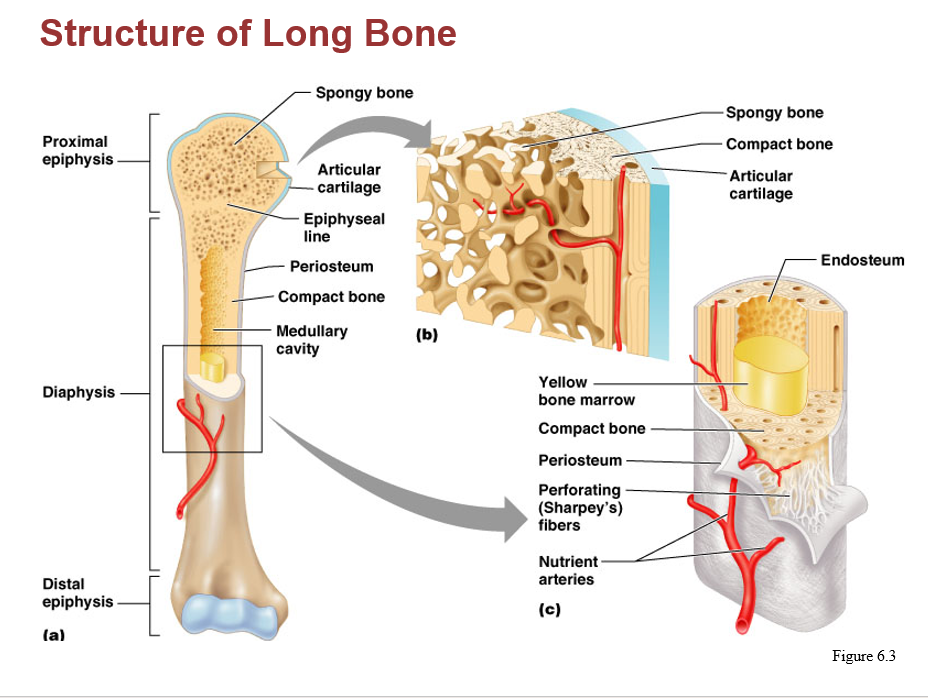
epiphyseal line:
The remnant of the epiphyseal plate in adults is a thin, defined area of compact bone
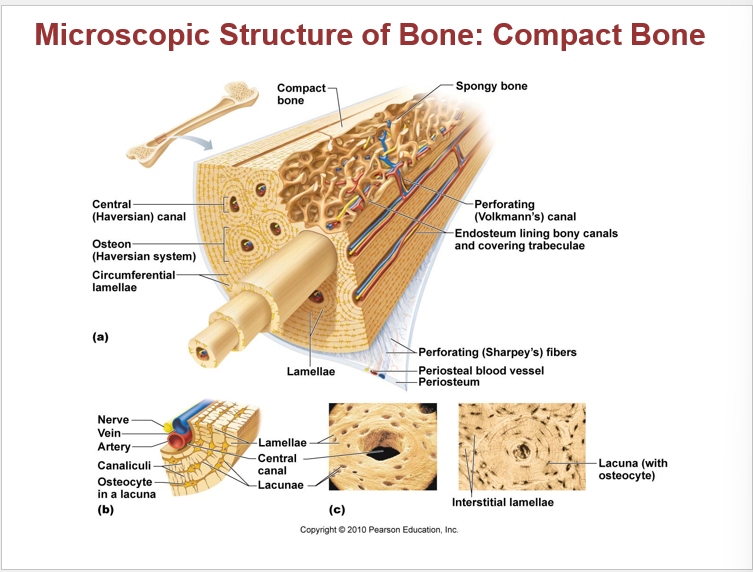
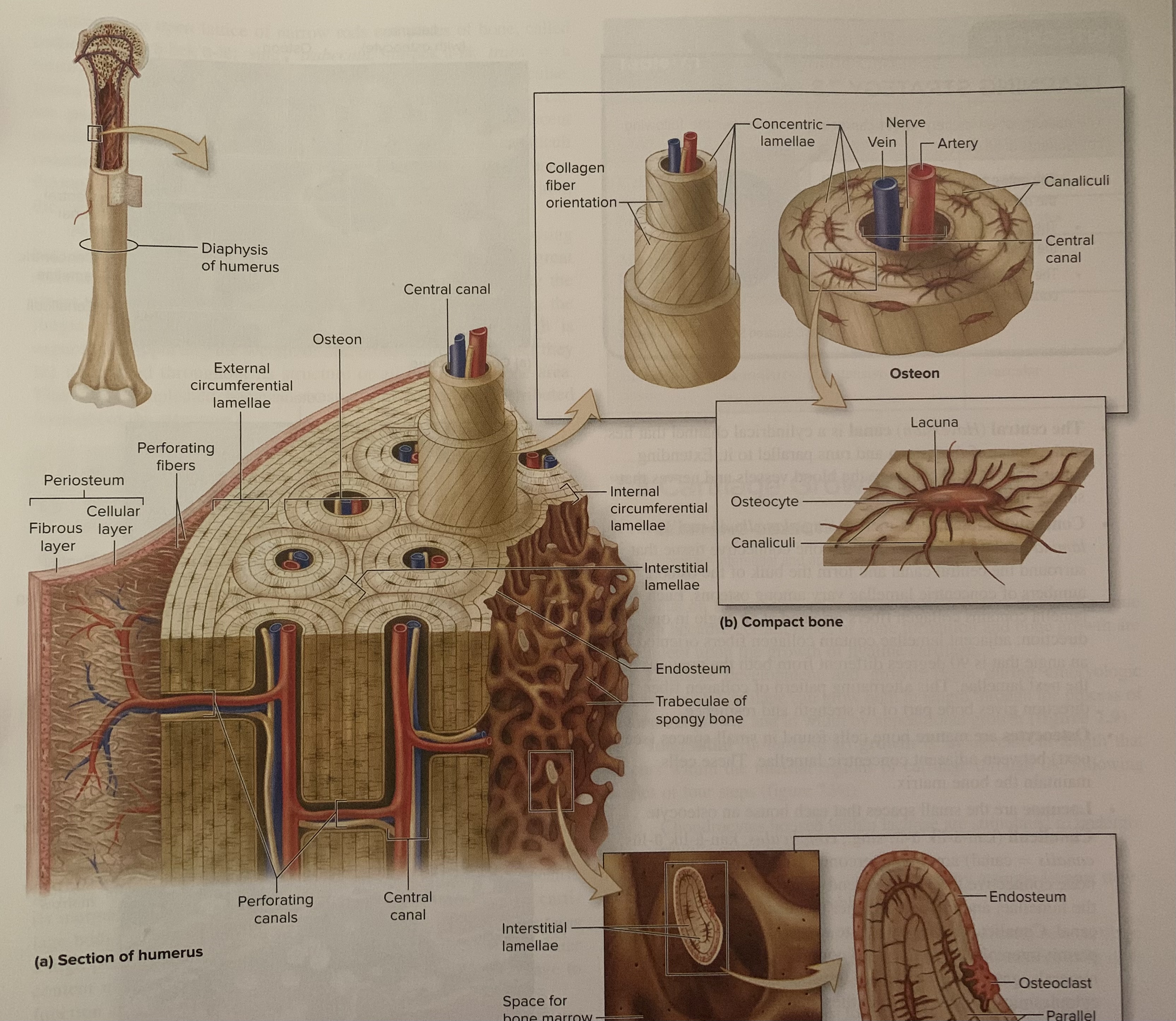
osteon (haversian system):
compact bone is composed of small, cylindrical structures. An osteon is the basic functional and structural unit of mature compact bone.
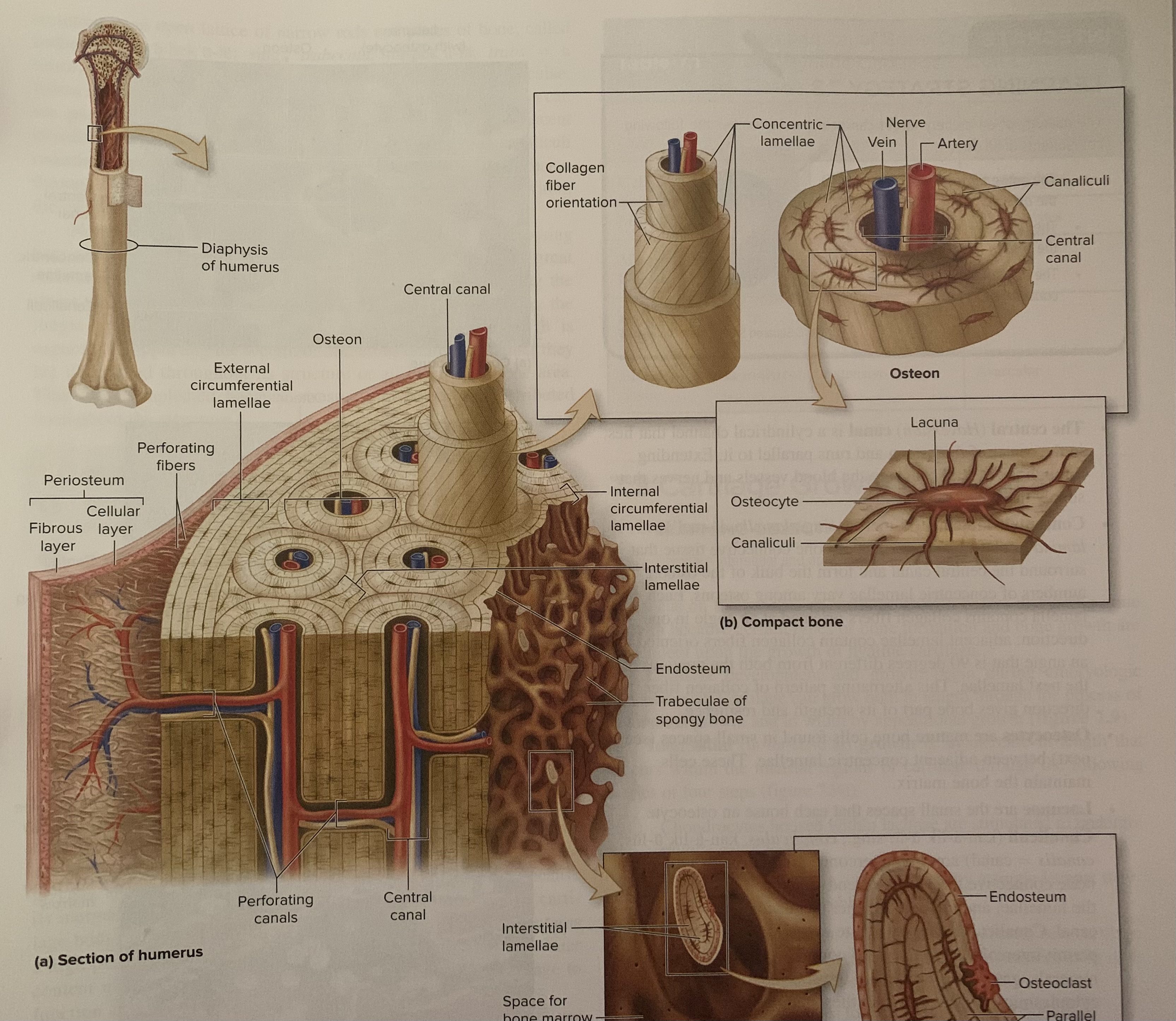
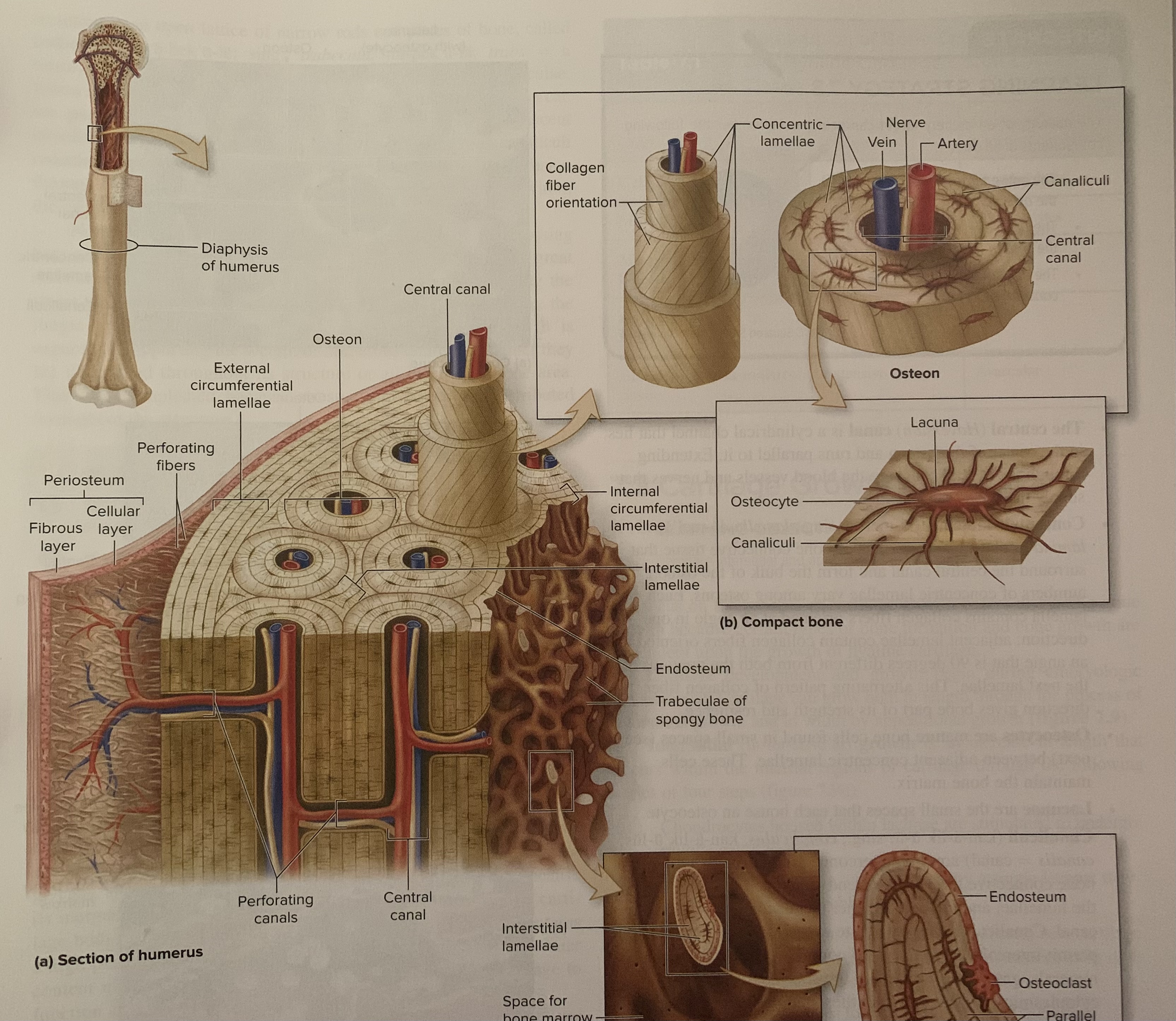
lacuna:
small, hollow spaces within compact bone tissue that house osteocytes, which are mature bone cells
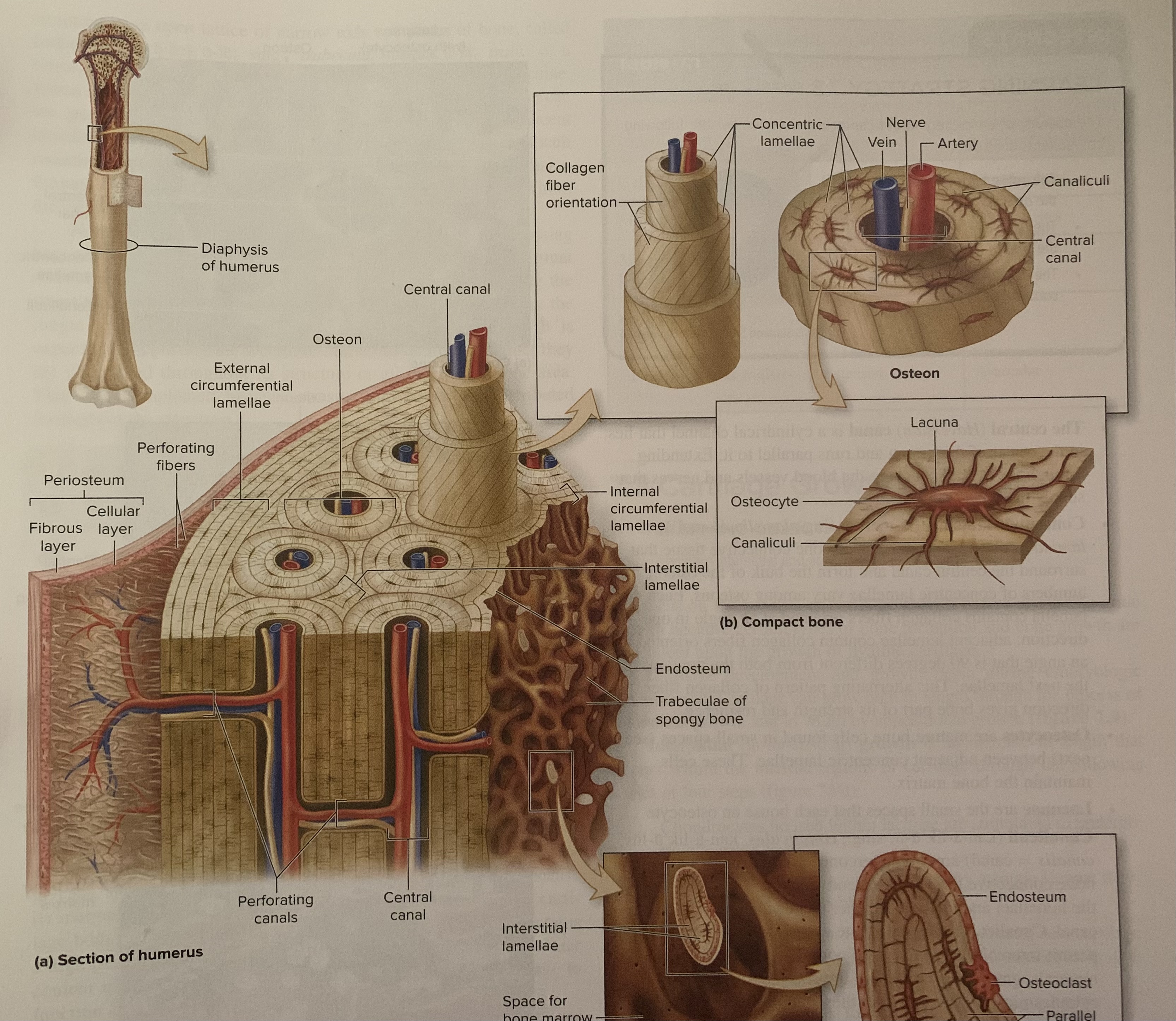
canaliculi:
Tiny, interconnecting channels within the bone CT that extend from each lacuna, through the lamellae, and connect to other lacunae and the central canal.
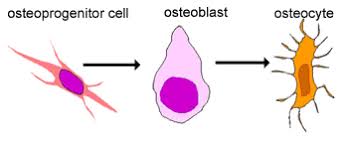
osteoprogenitor
Are stem cells derived from mesenchyme. When they divide through the process of cellular division, another stem cell is produced along with a “committed cell” that matures to become an osteoblast. these stem cells are located in both the periosteum and the endosteum
osteoblast
formed from osteoprogenitor stem cells. Often, osteoblasts are positioned side by side on bone surfaces.
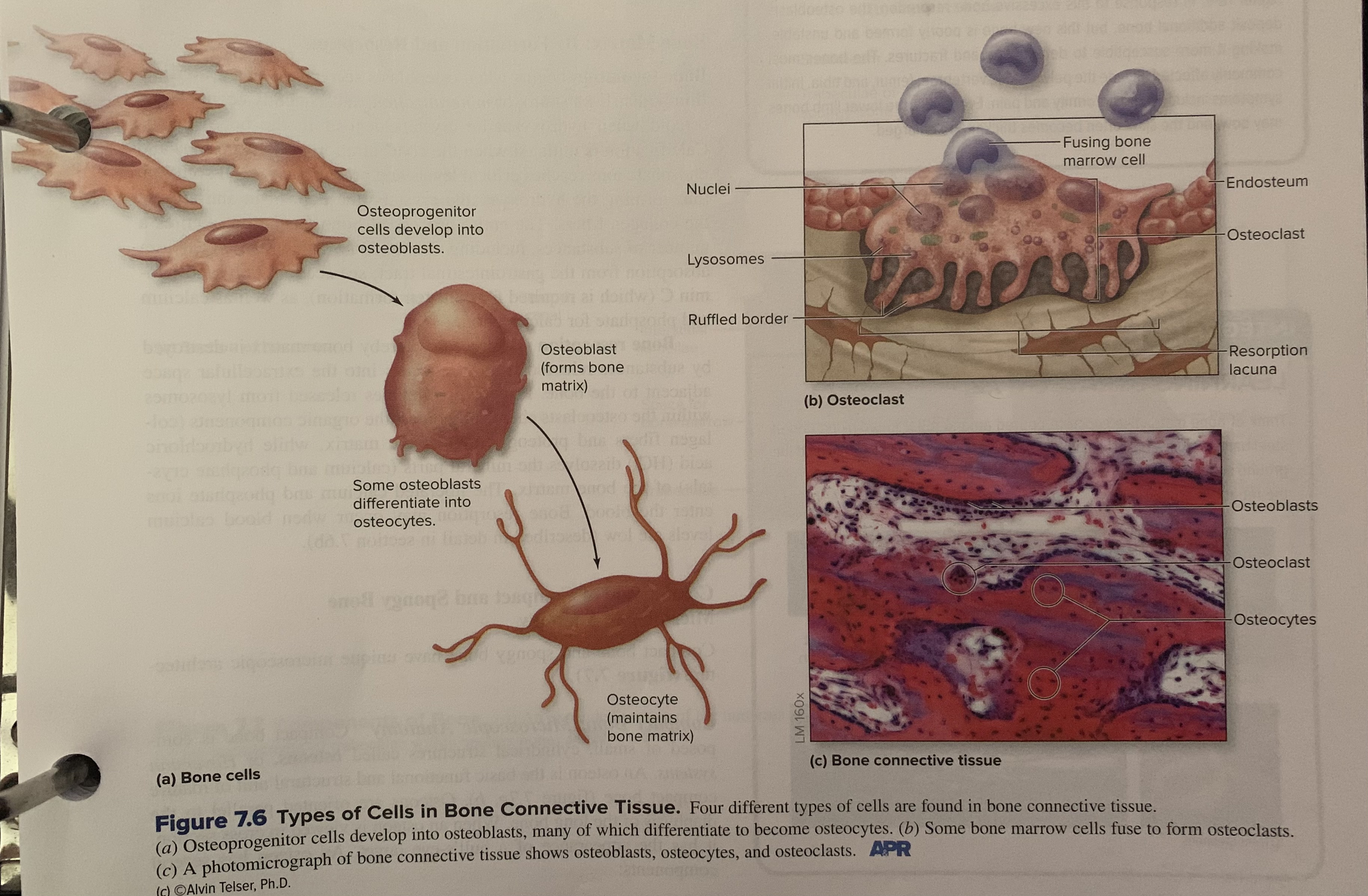
osteoclast
large, multinuclear, phagocytic cells. They are derived from fused bone marrow cells similar to those that produce monocytes. these cells exhibit a ruffled border where they contact the bone, which increases their surface area exposure to the bone. Often located within or adjacent to a depression or pit on the bone surface called resorption lacuna (Howship’s lacuna). Osteoclasts are involved in breaking down bone in an important process called bone resorption.
osteocyte
mature bone cells derived from osteoblasts that have lost their bone-forming ability when enveloped by calcified osteoid. Connections between some of the original neighboring osteoblasts are maintained by the cytoplasmic projections of the osteocytes. Osteocytes maintain the bone matrix and detect mechanical stress on a bone. If stress is detected, osteoblasts are signaled, and it may result in the deposition of new bone matrix at the surface.
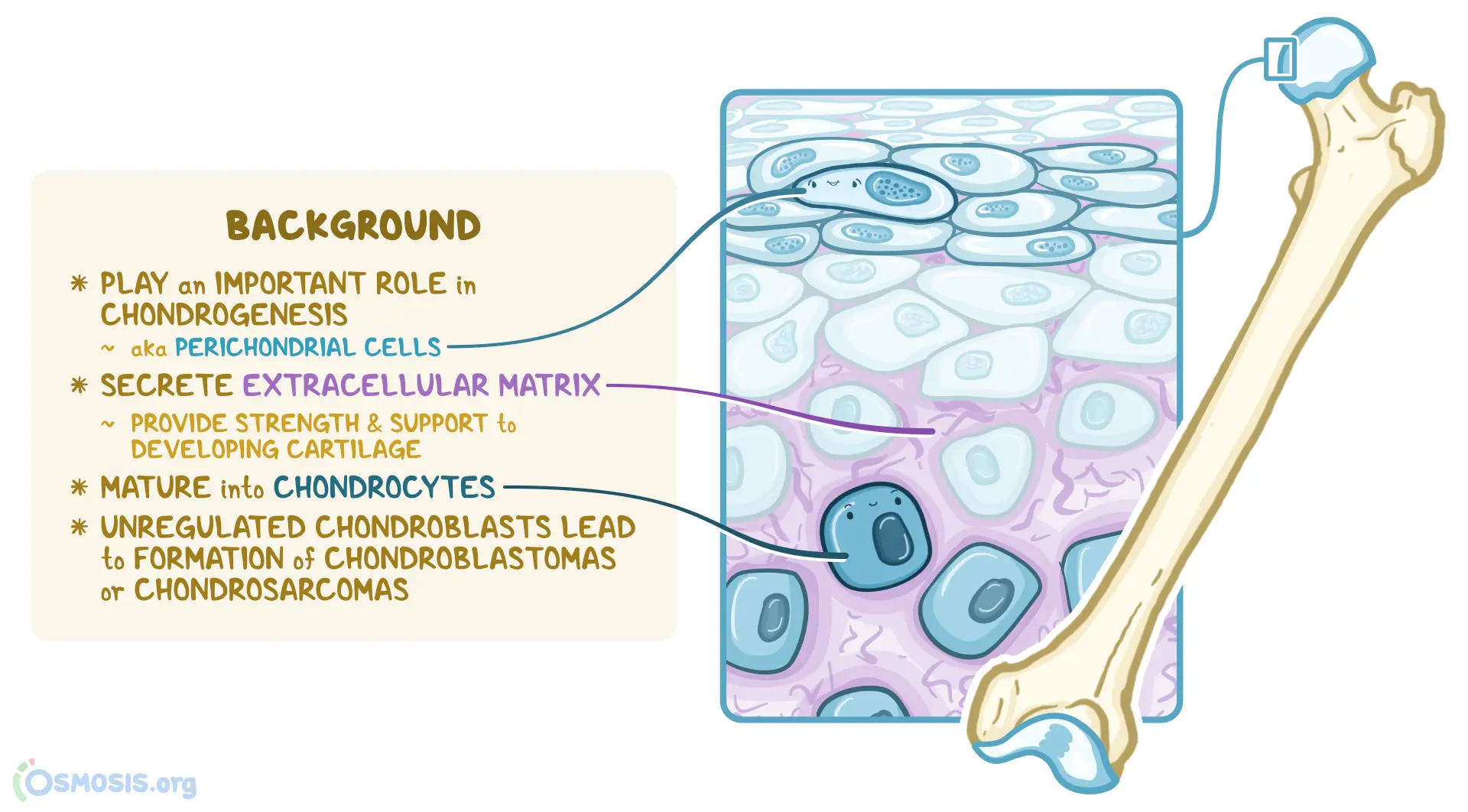
chondroblast
derived from mesenchymal cells and they produce the cartilage matrix
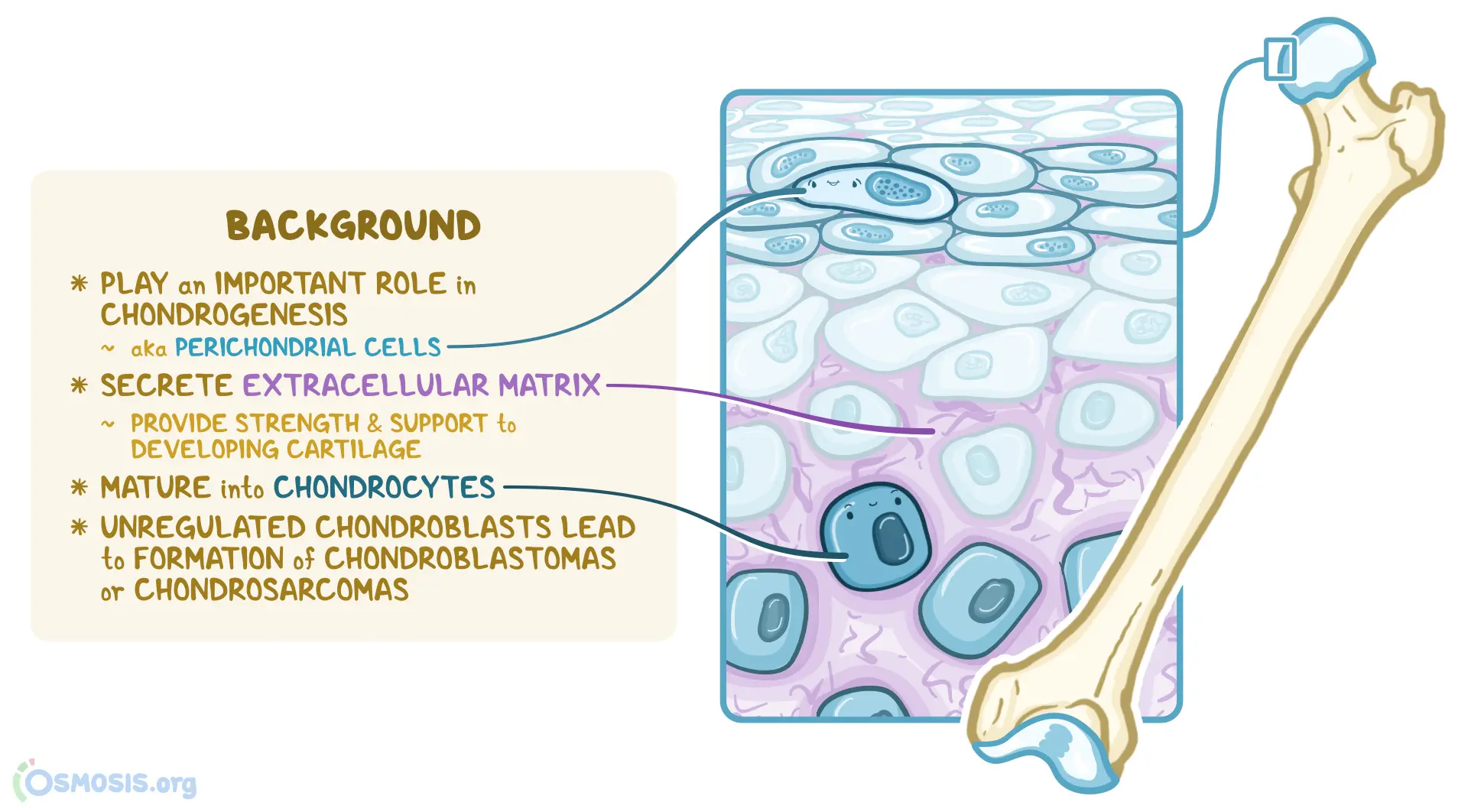
chondrocyte
Once chondroblast become encased within the matrix they have produced and secreted
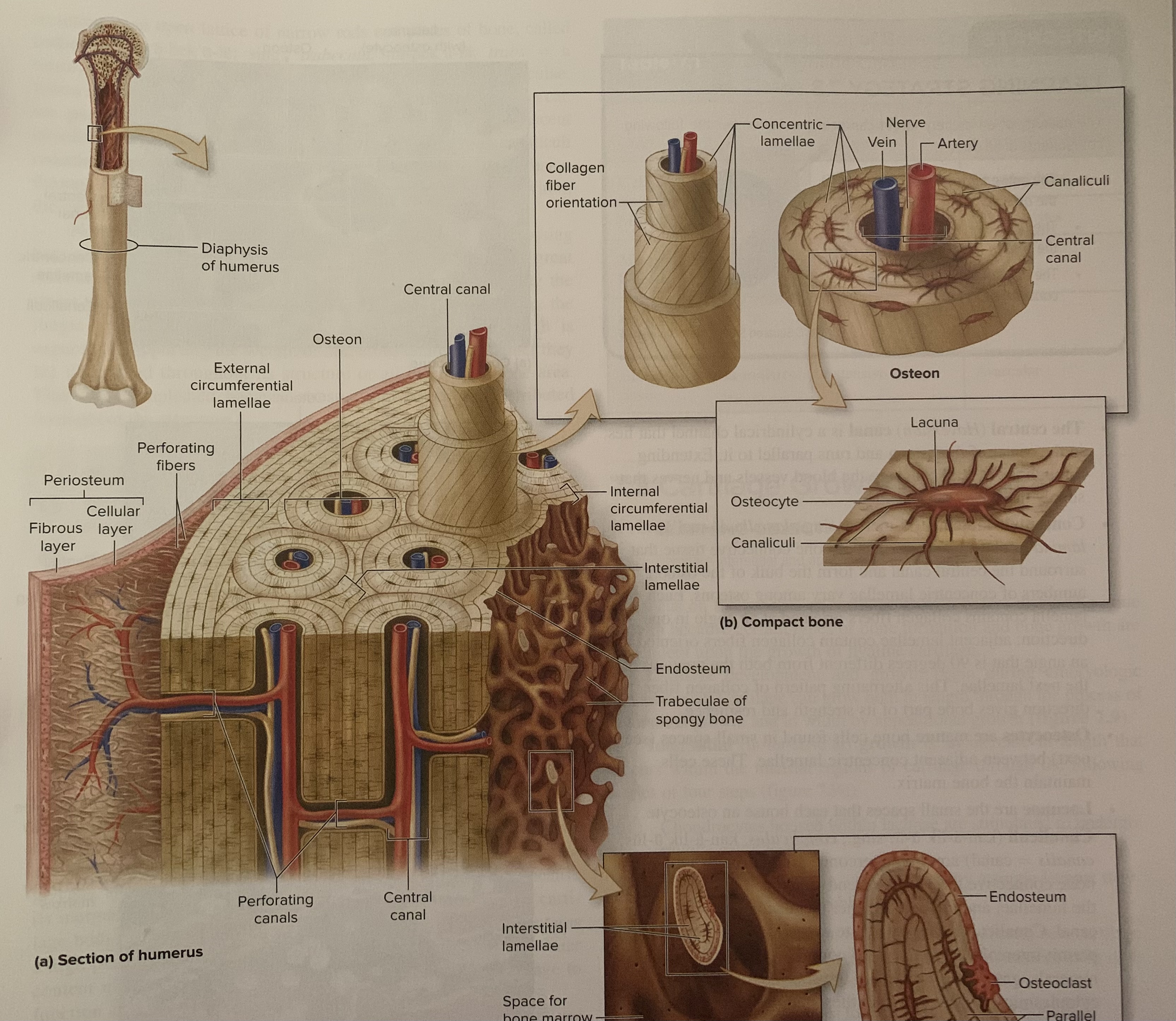
lamellae
thin, plated like layers of bone tissue that form the basic structural unit of compact bone (cortical bone)
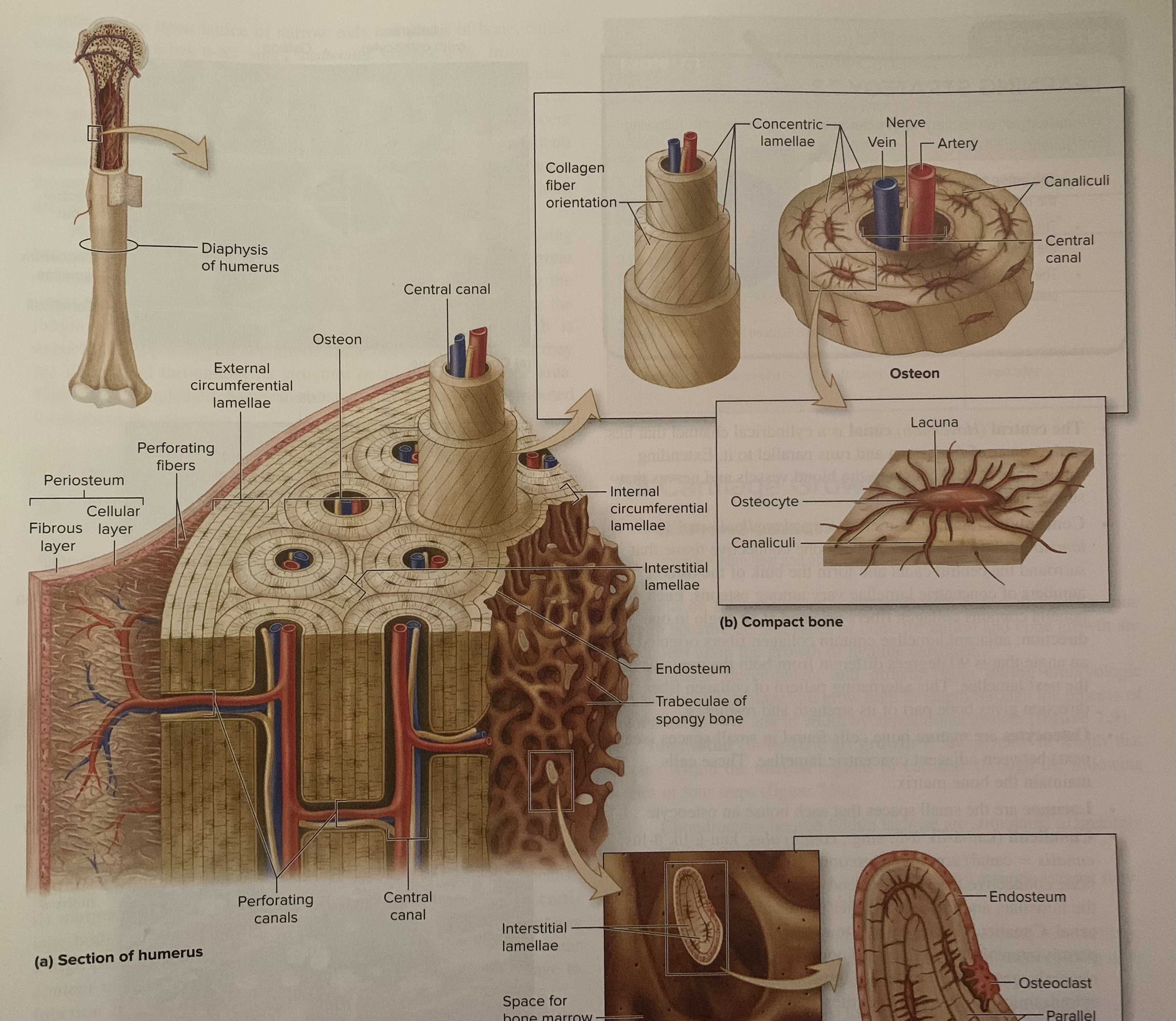
central (Haversian) canal
A cylindrical channel that lies in the center of the osteon and runs parallel to it. Extending through the canal are the blood vessels and nerves that supply the bone
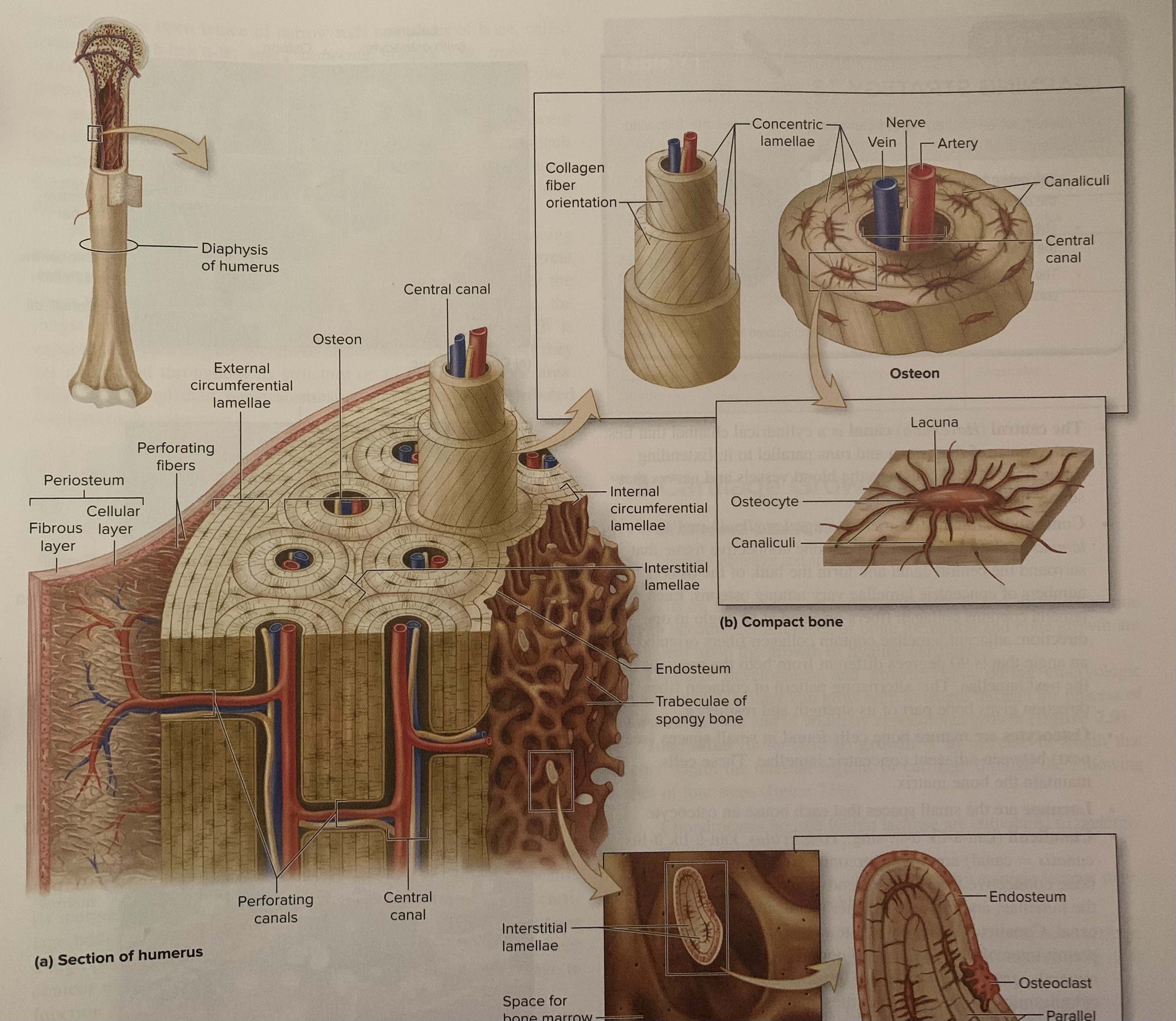
perforating canal
resemble central canals in that they also contain blood vessels and nerves. However, perforating canals run perpendicular to the central canals and help connect multiple central canals within different osteons, thus forming a channel for a vascular and innervation connection among the multiple osteons
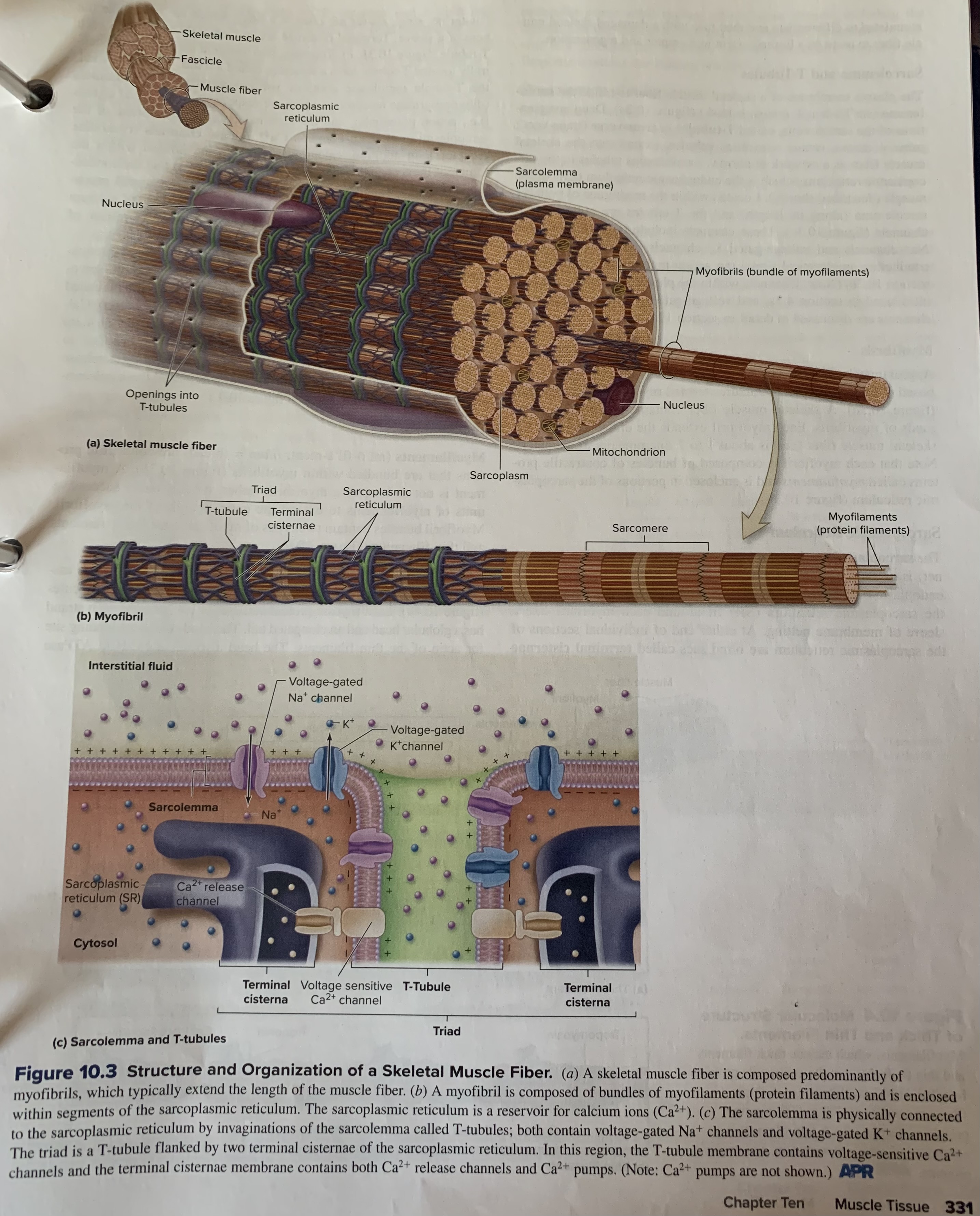
muscle fiber
A single muscle, such as the gracilis muscle on the medial thigh, may be composed of thousands of muscle cells that are typically as long as the entire muscle. Their potentially extraordinary length, skeletal muscle cells
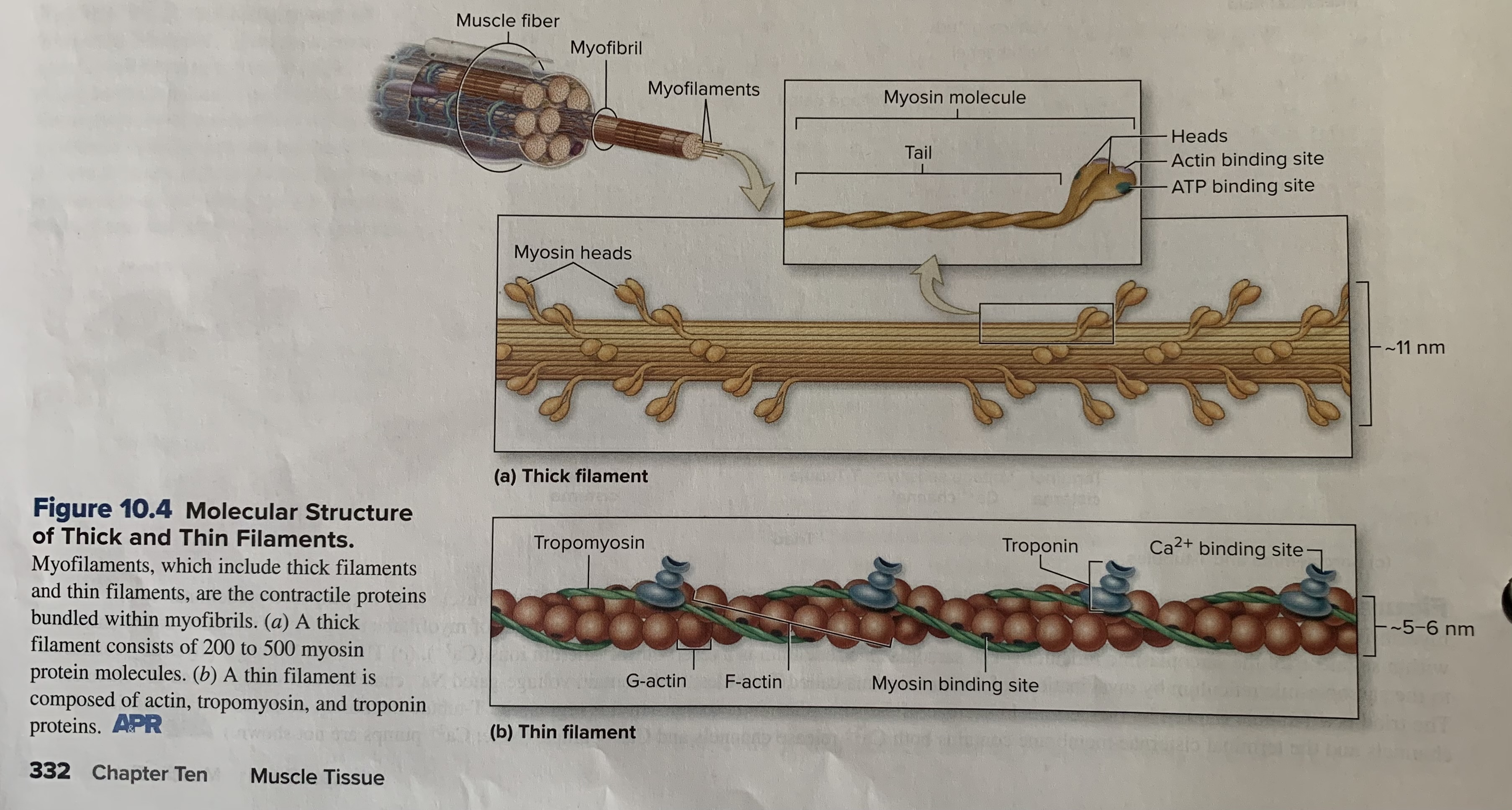
thick filaments (thick myofilaments) pp.332
Assembled from bundles of 200 to 500 myosin protein molecules.
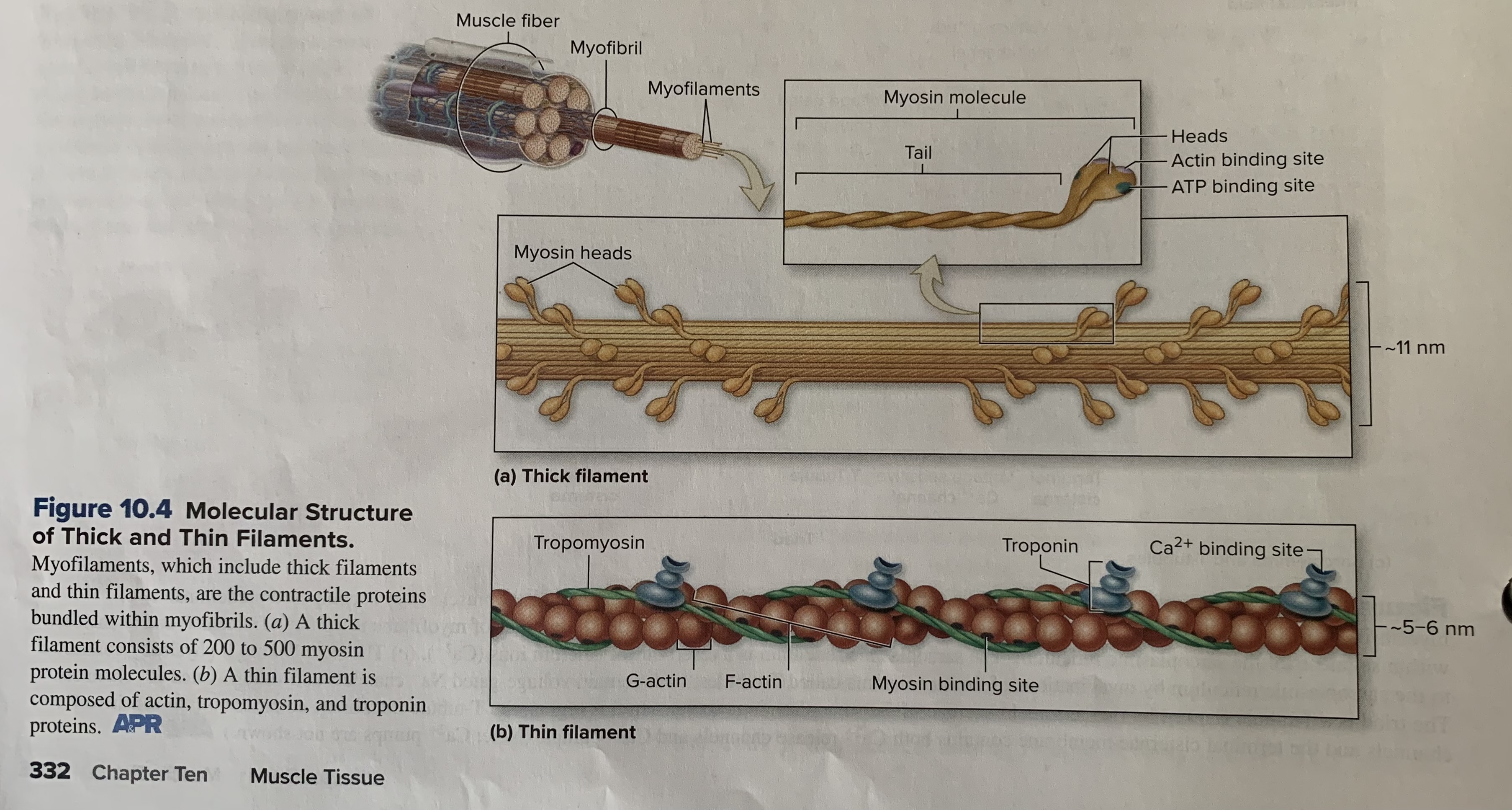
thin filaments (thin myofilaments)
Are approx. half of the diameter of thick filaments (about 5 to 6 nanometers)
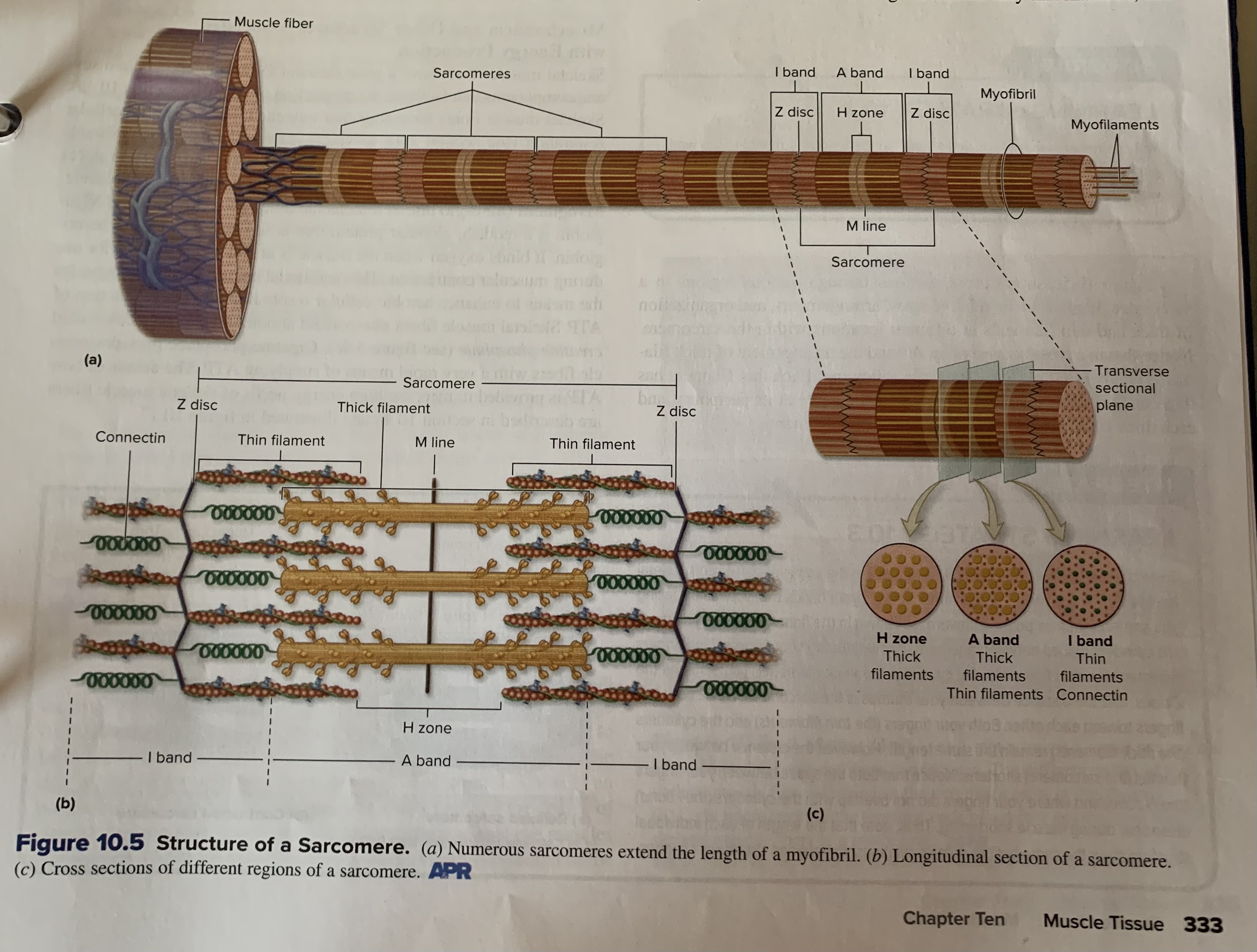
Z disc (z line)
Are composed of specialized proteins that are positioned perpendicular to the myofilaments and serve as anchors for the thin filaments. Although the Z disc appears as a flat disc when the myofibril is viewed in cross section, only the edge of the disc is visible in a longitudinal view, and it sometimes looks like a zigzagged line
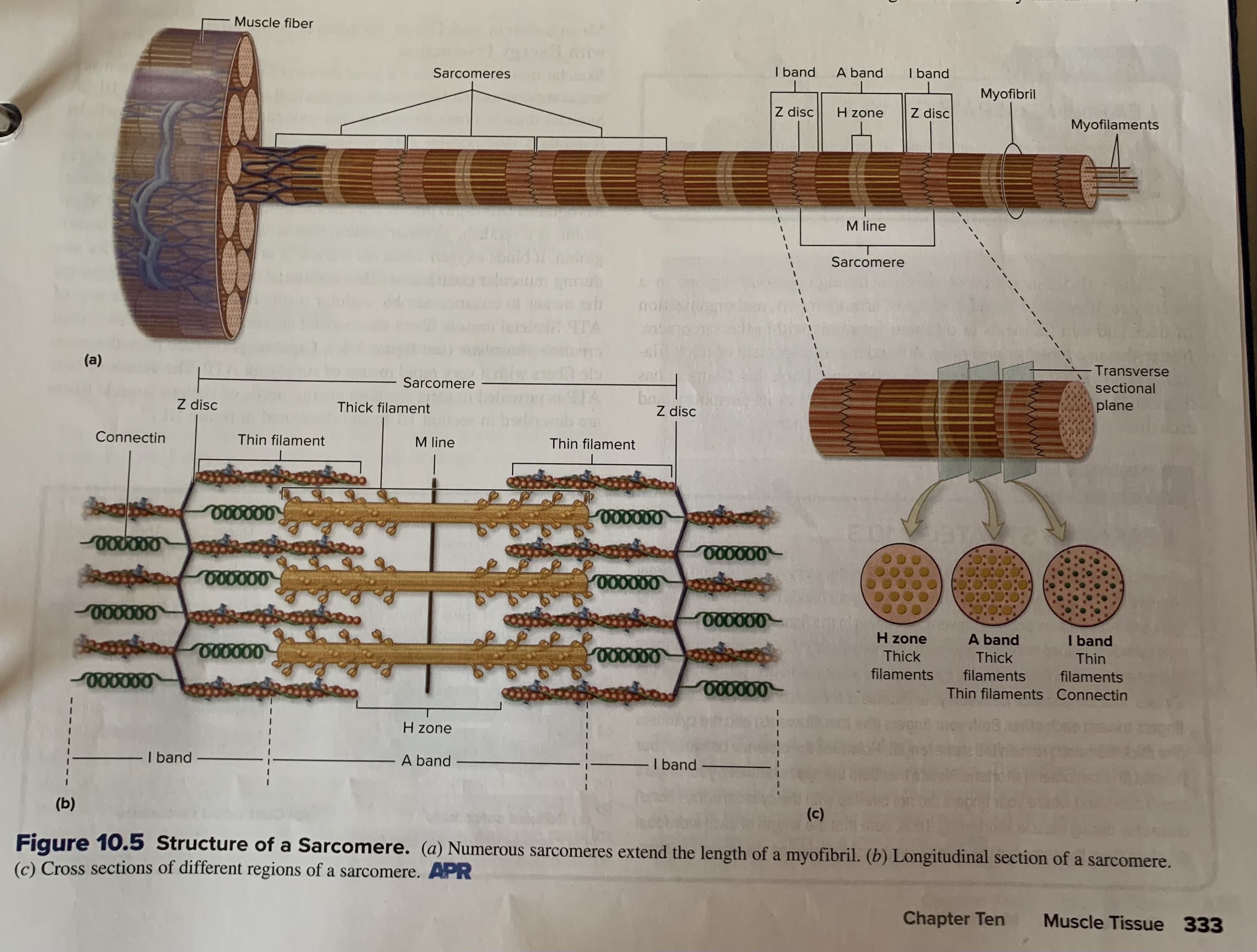
A band
The central region of a sarcomere that contains the entire thick filament. Thin filaments partially overlap the thick filament on each end of an A band. The A band appears dark when viewed with a microscope. The A band does not change in length during muscle contraction
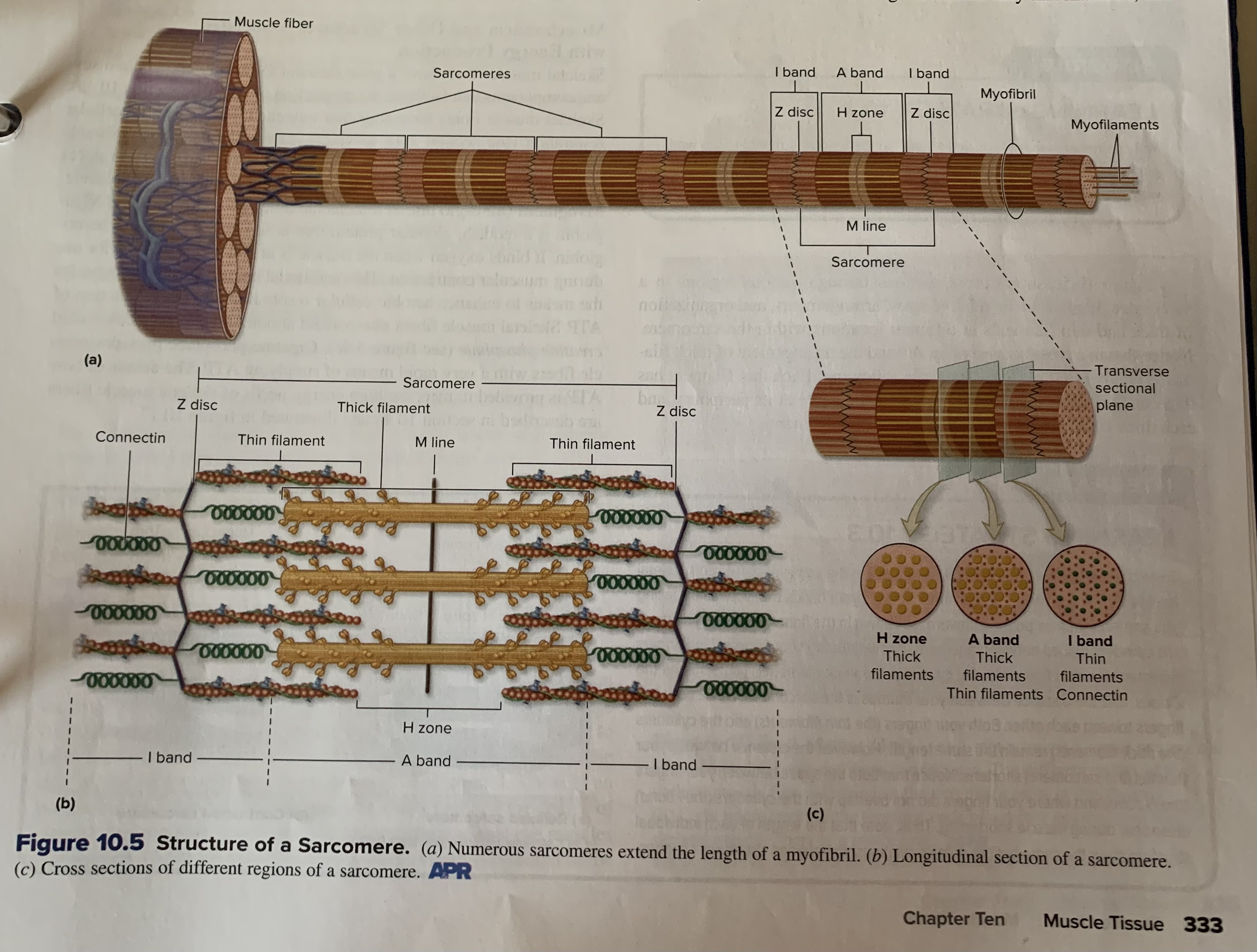
I band
extend from both directions of a Z disc and are bisected by the Z disc. These end regions contain only thin filament; this region appears light when viewed with a microscope. At maximal muscle shortening, the thin filaments are pulled parallel along the thick filaments, causing the I bands to disappear.
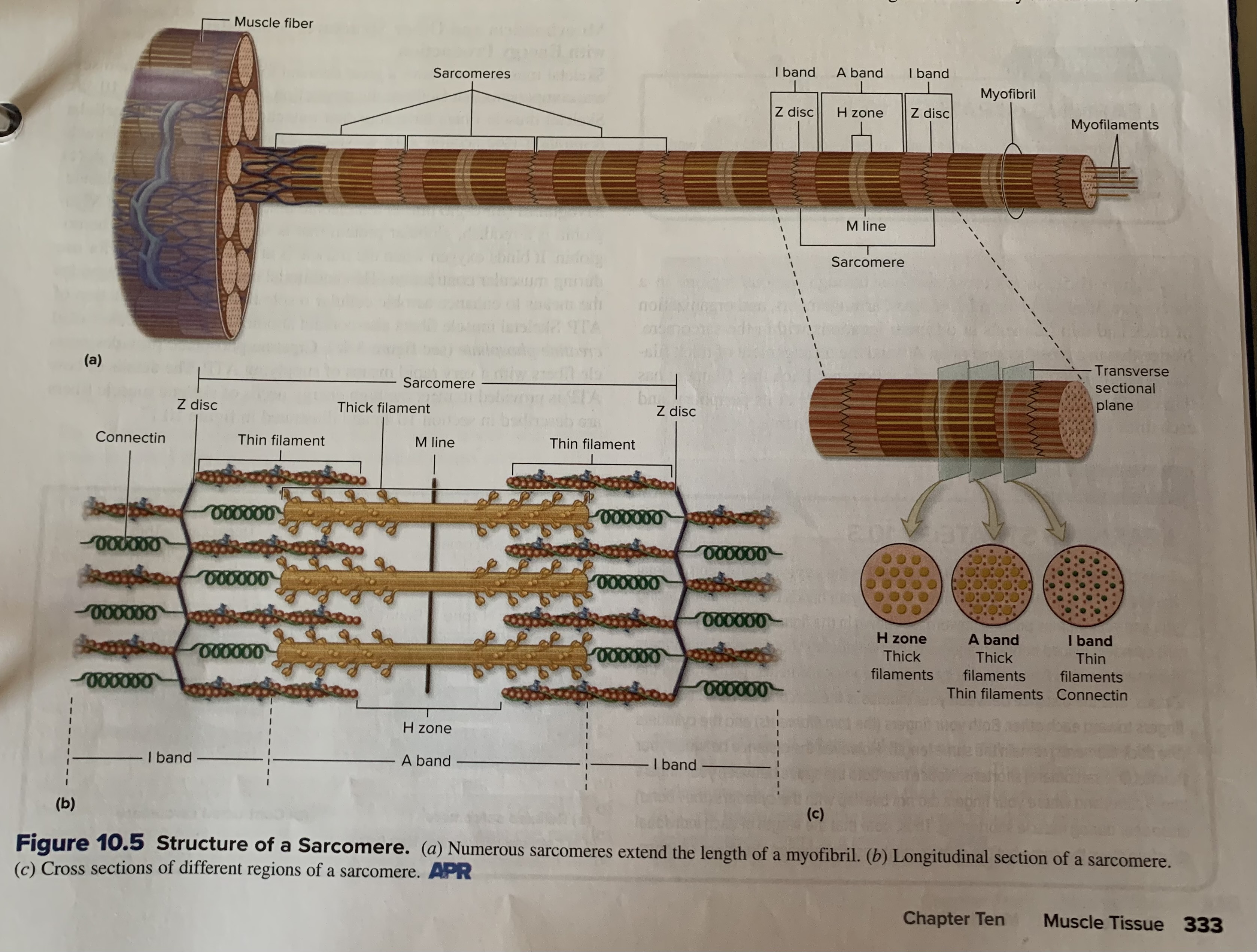
M line
Is a thin transverse protein meshwork structure in the center of the H zone. It serves as an attachment site for the thick filaments and keeps thick filaments aligned during contraction and relaxation events
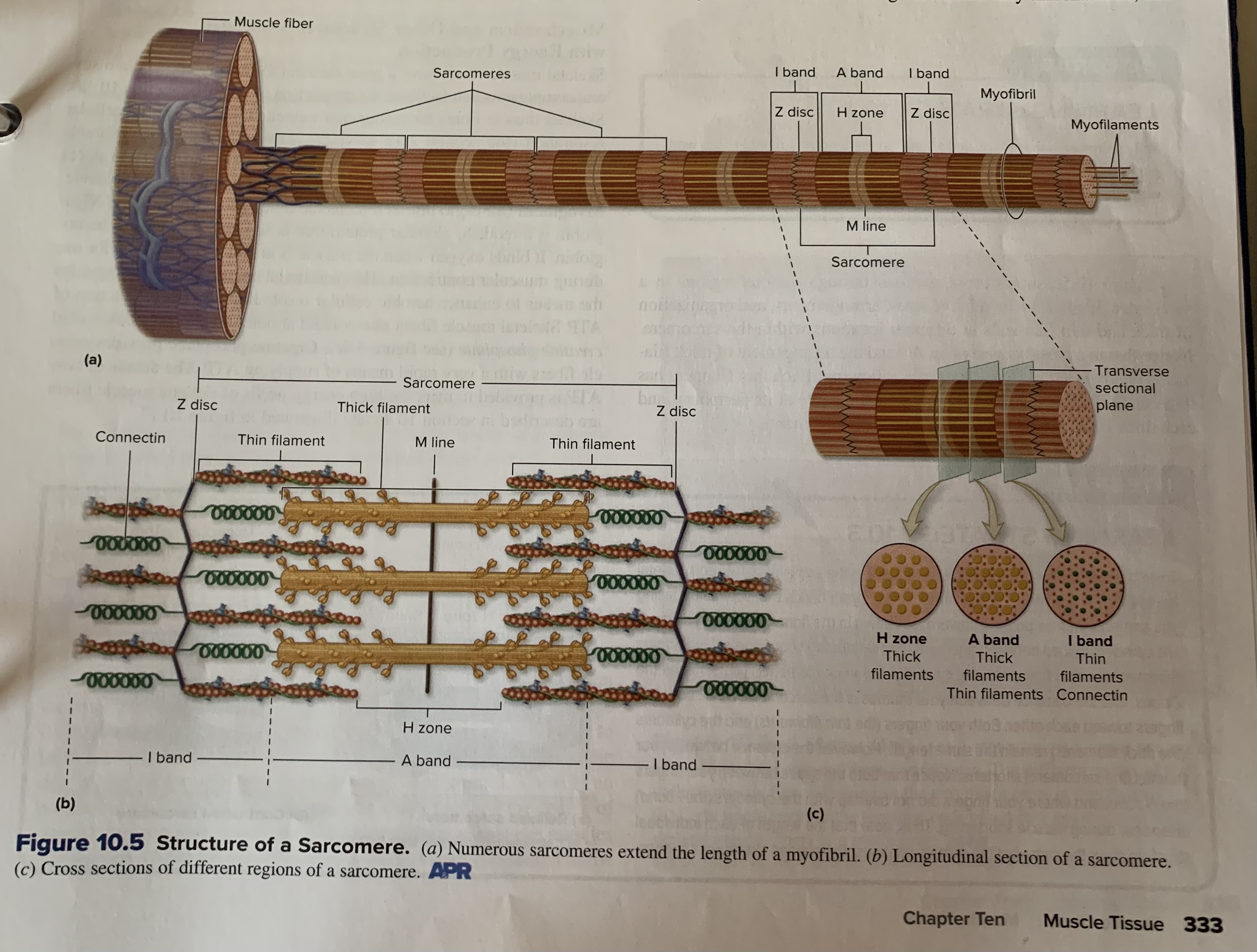
H zone (H band)
The most central portion of the A band in a resting sarcomere. This region does not have thin filament overlap; only thick filaments are present. During maximal muscle shortening, this zone disappears when the thin filaments are pulled past thick filaments
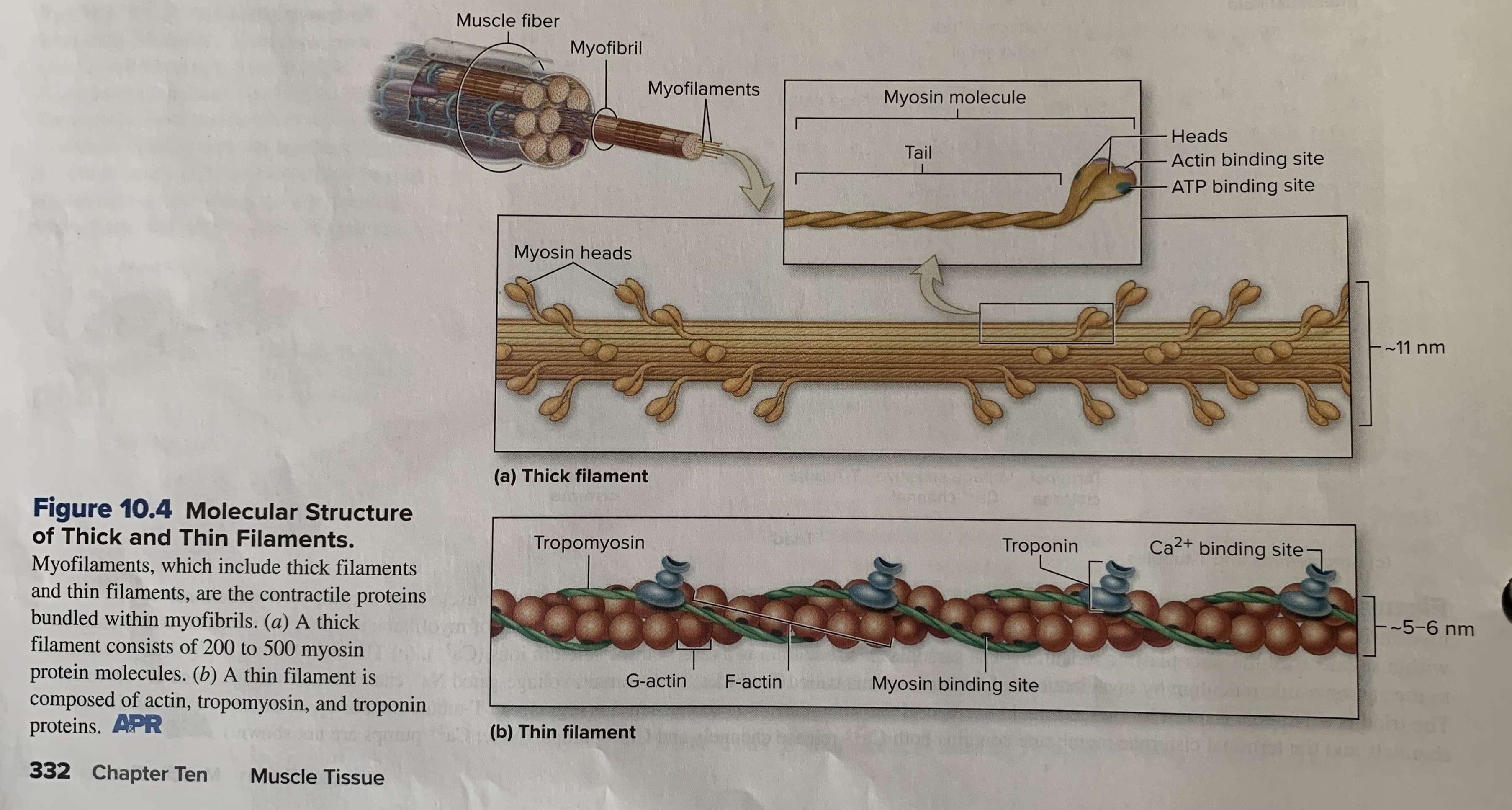
actin
Thin filaments are primarily composed of 2 strands of actin protein twisted around each other to form a helical shape. In each strand of actin, many (about 300 to 400) small, spherical molecules (G, or globular, actin) are connected to form a fibrous strand (F, or filamentous, actin). F actin resembles 2 beaded necklaces that are twisted and intertwined together, with G actin as the individual beads. Each G actin molecule has a significant feature called a myosin binding site. The myosin head attaches to the myosin binding site of actin during muscle contraction
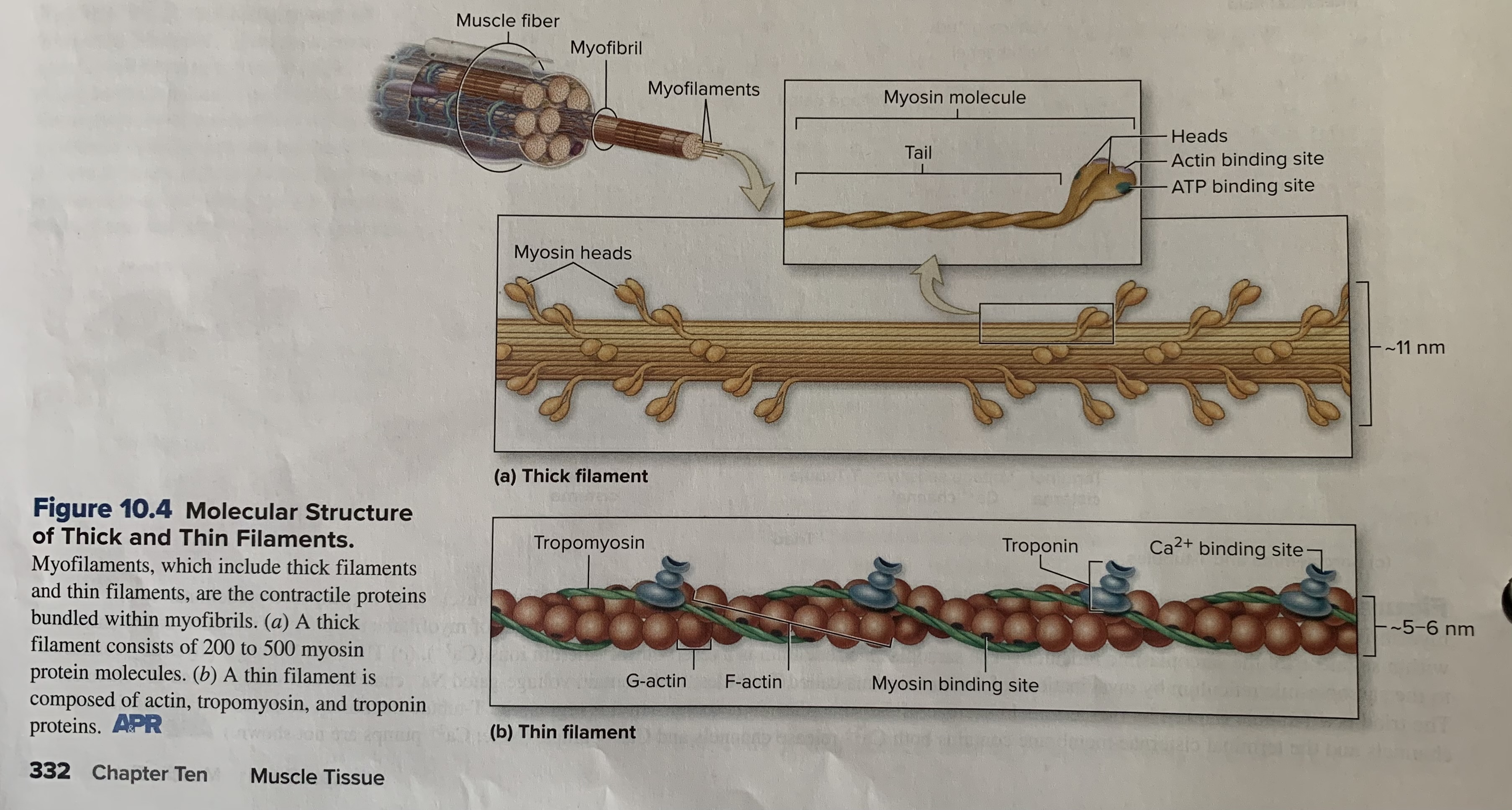
myosin
Each myosin protein consists of 2 strands; each strand has a globular head and an elongated tail. The head contains a binding site for actin of the thin filaments. The head also has a catalytic ATPase site where adenosine triphosphate (ATP) attaches and is split into adenosine diphosphate (ADP) and phosphate (Pi). (It is because the head of myosin functions as an ATPase enzyme that myosin is often referred to more specifically as myosin ATPase.) The tails of 2 strands of a myosin molecule are interwined. Each myosin molecule composing a thick filament is oriented so that its tails point toward the center of the thick filaments and its heads point toward the ends of the thick filaments. Think of the myosin protein molecules as 2 intertwined gold clubs, where many are grouped together with the golf shafts in the center and the club heads on each end
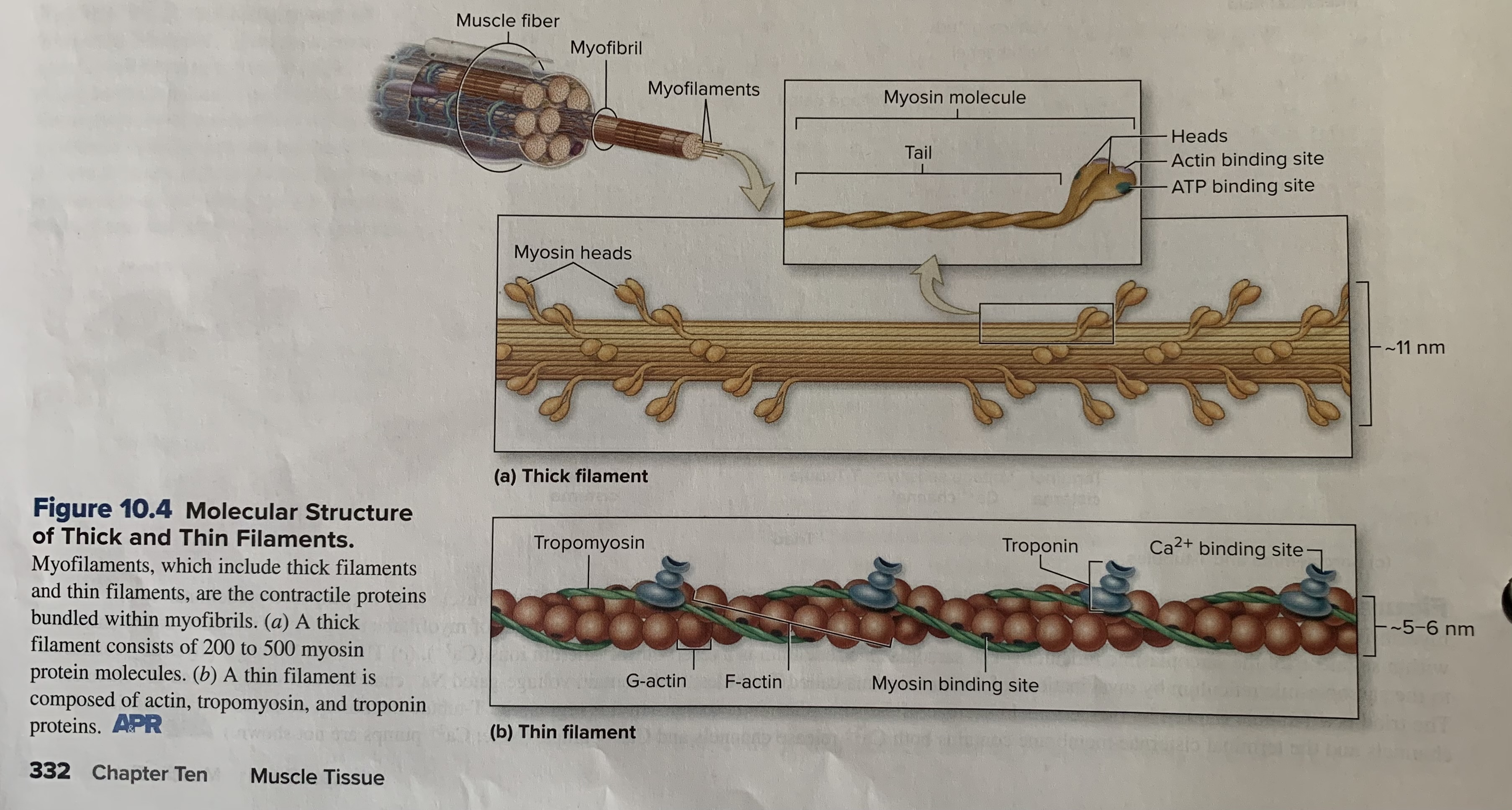
troponin
Is a globular, or “ball like,” protein attached to tropomyosin. Troponin contains the binding site for Ca2+
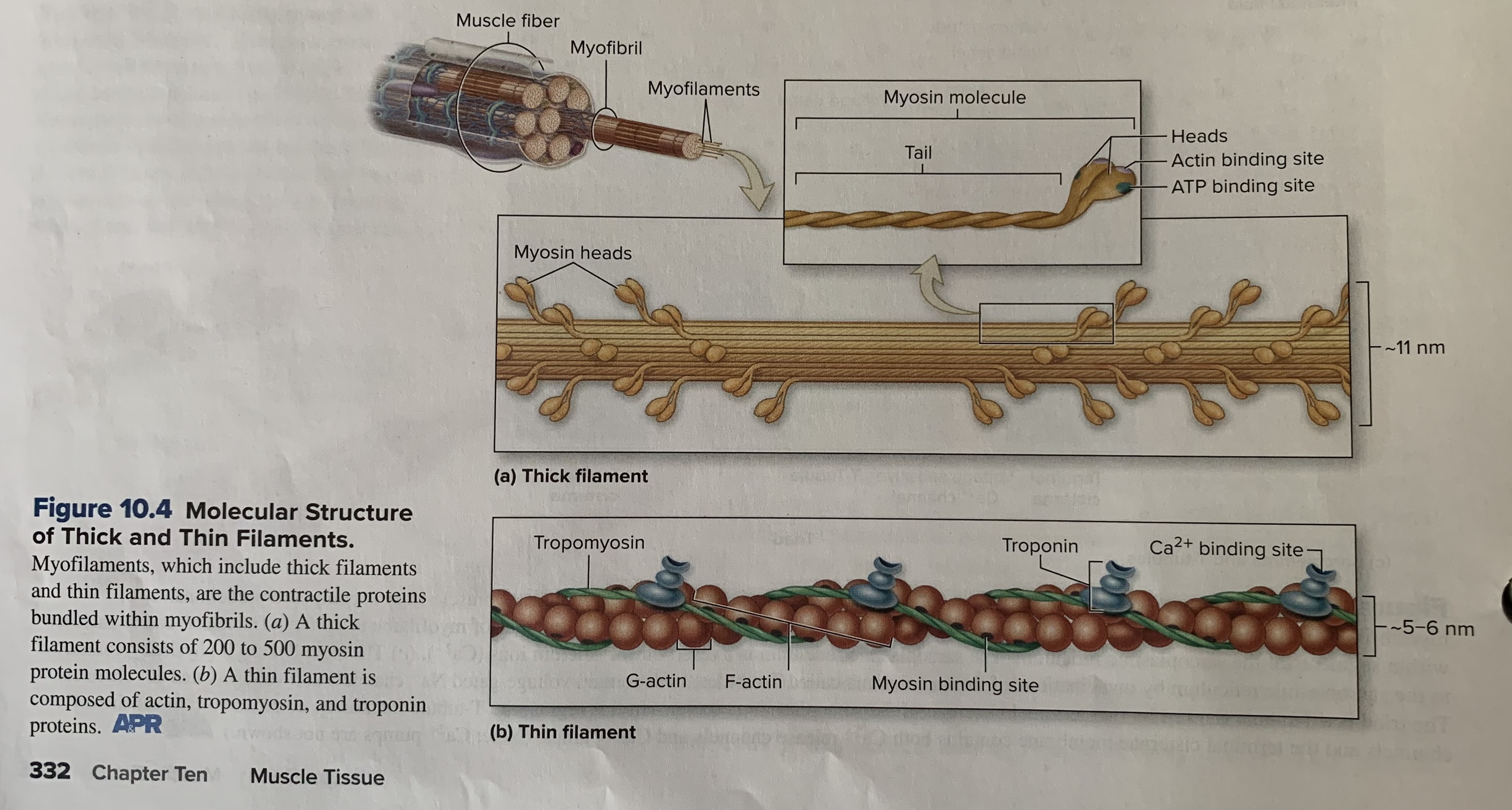
tropomyosin
Is a short, thin, twisted filament that is a “stringlike” protein. Consecutive tropomyosin molecules cover small regions of the actin strands, including the myosin binding sites in a noncontracting muscle.
parathyroid hormone
Increases blood calcium levels by encouraging bone resorption by osteoclasts
calcitonin
Promotes calcium deposition in bone and inhibits osteoclast activity
growth hormone
Stimulates liver to produce the hormone insulin like growth factor (IGF), which causes cartilage proliferation at epiphyseal plate and resulting bone elongation
Be able to explain the difference in primary and secondary ossification centers
The primary ossification center forms in the diaphysis. A growth of capillaries and osteoblasts, called a periosteal bud, extends from the periosteum into the core of the cartilage shaft, invading the spaces where the living chondrocytes had been. The remains of the calcified cartilage serve as a template on which osteoblasts begin to produce osteoid. This region is called the primary ossification center because it is the first major center of bone formation. Bone development extends in both directions toward the epiphyses from the primary ossification center. Healthy bone CT quickly displaces the calcified, degenerating cartilage in the shaft. Most, but not all, primary ossification centers have formed by the 12th week of development
Secondary ossification centers form in the epiphyses. The same basic process that formed the primary ossification center occurs later in the epiphyses. Beginning around the time of birth, the hyaline cartilage in the center of each epiphysis calcifies and begins to degenerate. Epiphyseal blood vessels and osteoprogenitor cells enter each epiphysis. Secondary ossification centers form as bone displaces calcified cartilage. Note that not all secondary ossification centers form before birth; some form later in childhood. As the secondary ossification centers form, osteoclasts resorb some bone matrix within the diaphysis, creating a hollow medullary cavity
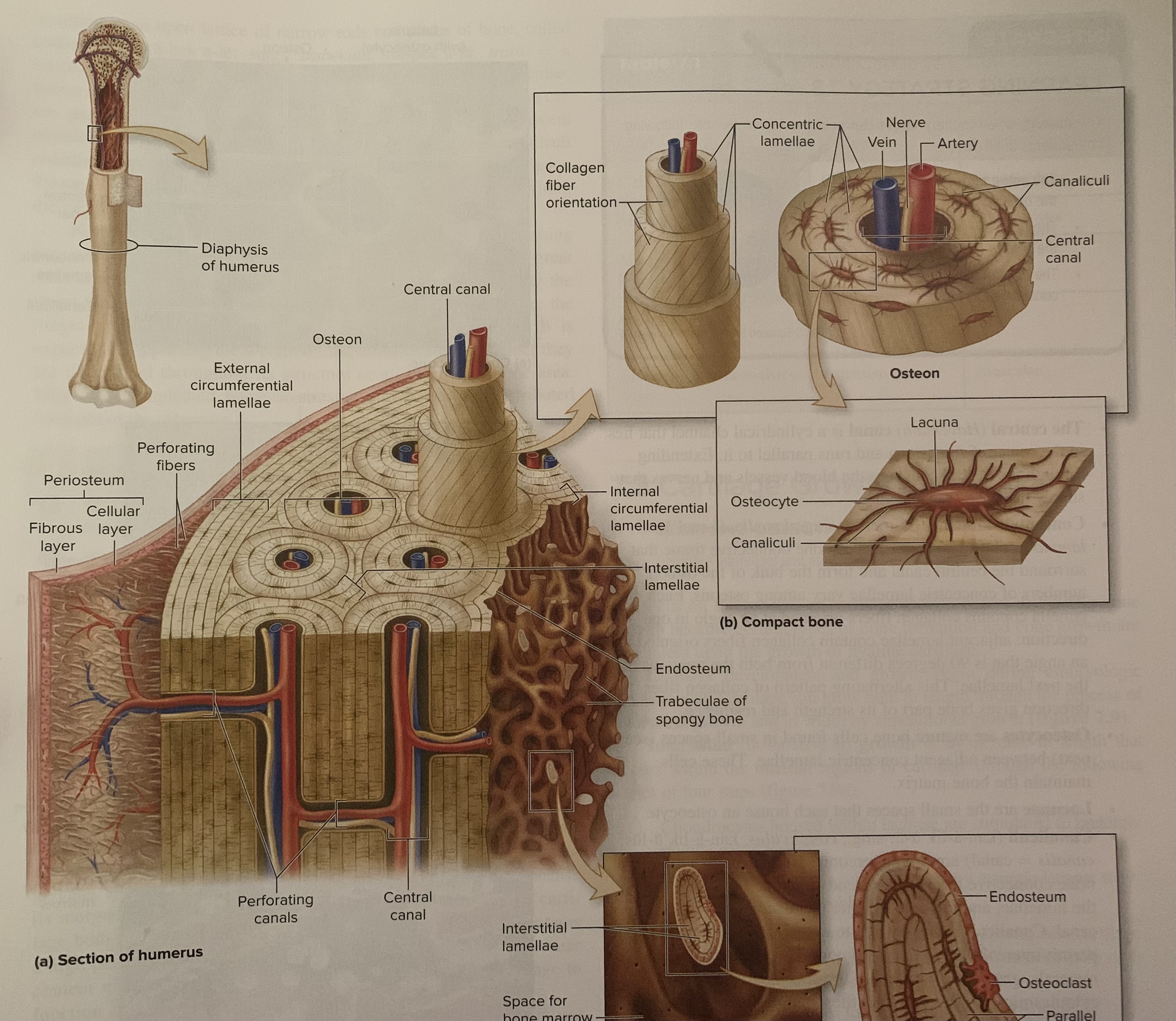
Be able to recognize the following: osteon, lacuna, canaliculi, lamellae
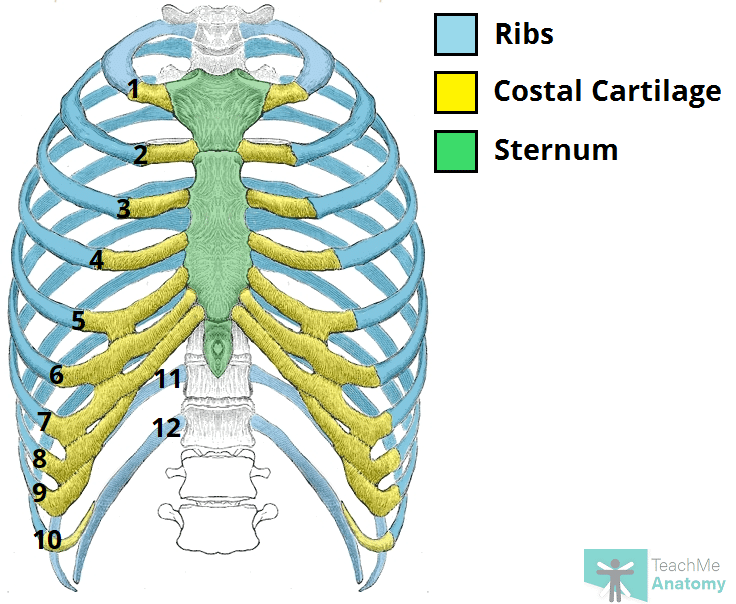
Explain how to differentiate between the three types of ribs:
The 2 types of ribs are differentiated by their anterior attachments to the sternum
True ribs (1-7):
articulate directly and individually to the sternum by separate cartilaginous extensions called costal cartilages. The smallest true rib is the first
False ribs (8-12):
their costal cartilages do not articulate directly to the sternum. The costal cartilages of ribs 8-10 fuse to the costal cartilage of rib 7 and thus indirectly articulate with the sternum.
Floating ribs (11 and 12):
They have no articulation with the sternum
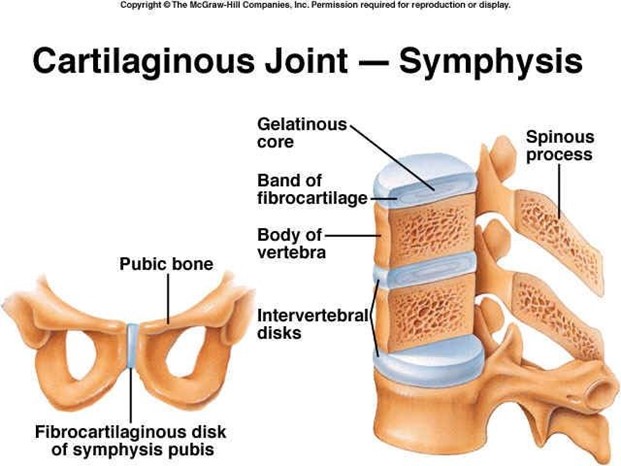
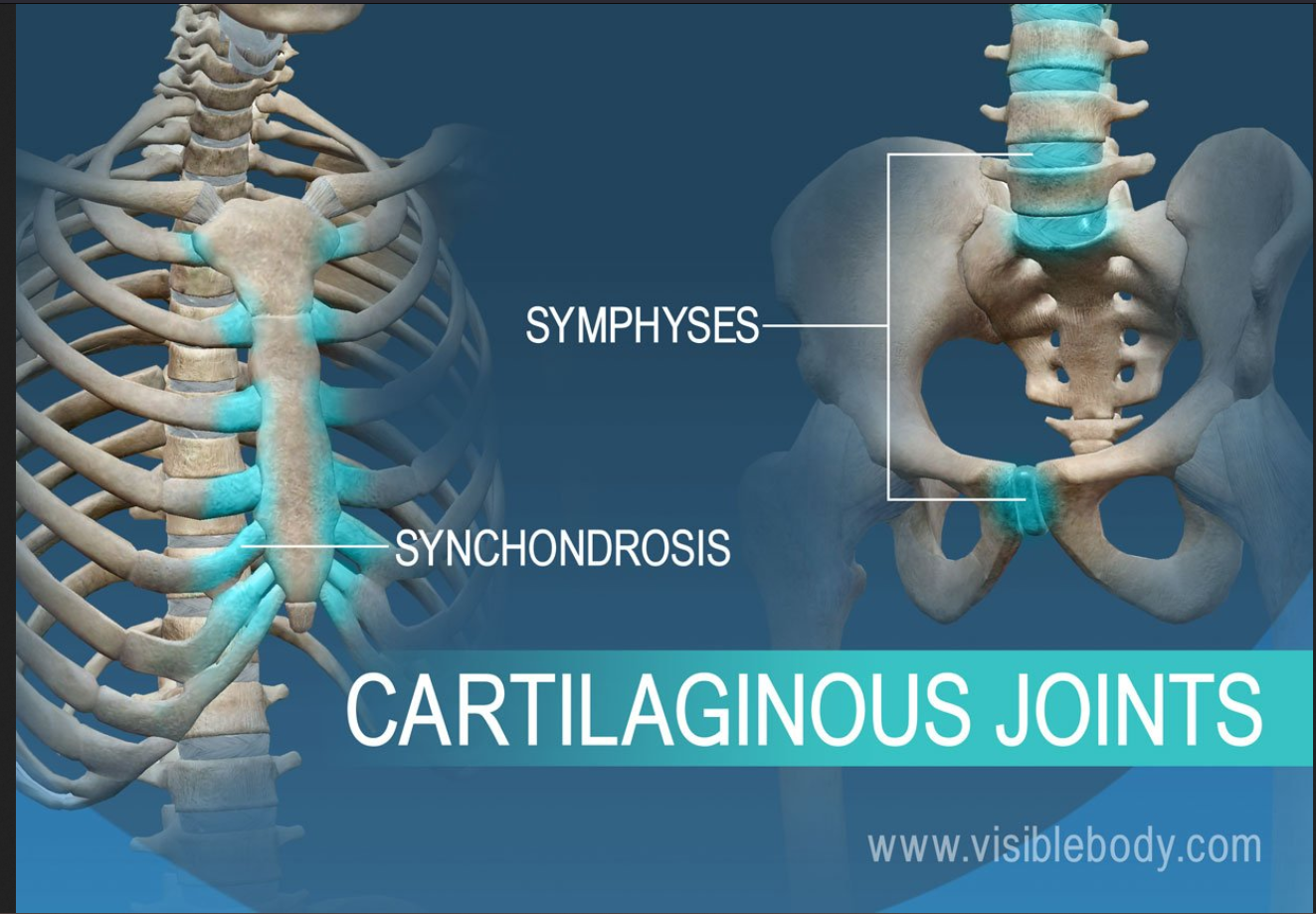
symphysis
has a pad of fibrocartilage between the articulating bones. The fibrocartilage resists both compression and tension stresses and acts as a resilient shock absorber. All symphyses are amphiarthroses-thus, they allow slightly mobility.
Example:
pubic syphysis and the intervertebral discs
Fibrous
Dense regular CT holds together the ends of bones and bone parts; no joint cavity
Structural classification:
Gomphosis, Suture, Syndesmosis
Functional Classification:
synarthrosis (immobile) or amphiarthrosis (slightly mobile)
Synovial
Ends of bones covered with articular cartilage; joint cavity separates the articulating bones; joint enclosed by an articular capsule, lined by a synovial membrane; contains synovial fluid
structural categories:
plane, hinge, pivot, condylar, saddle, ball and socket
Functional classification:
Diarthrosis (freely mobile)
cartilage (cartilaginous)
Pad of cartilage is wedged between the ends of bones; no joint cavity
Structural categories:
synchondrosis, symphysis
Functional classifcation:
synarthrosis (immobile) or amphiarthrosis (slightly mobile)
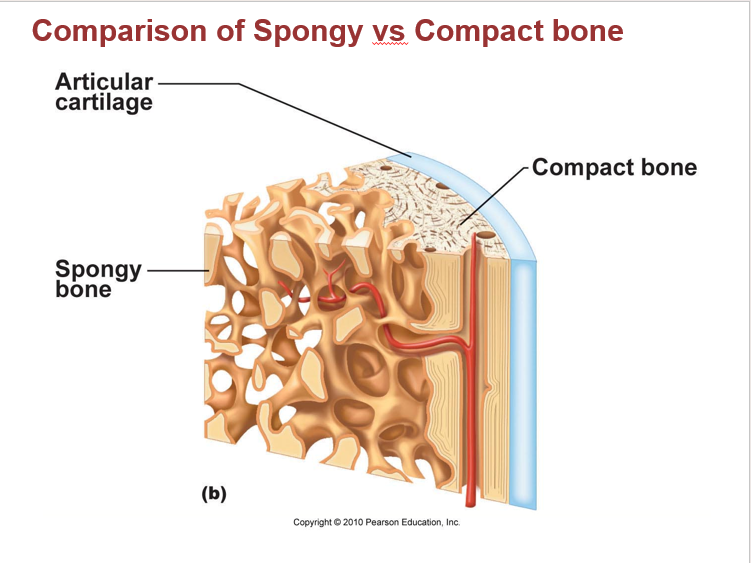
How are compact and spongy bone similar to each other? How are they different? Be sure your answers include resistance to force and types of marrow
Both compact and spongy bone are types of bone tissue, but they differ in structure, density, and function. Compact bone is (high) dense and strong, forming the outer layer, while spongy bone (low density) is lighter and porous, found internally and containing red bone marrow.
Compact bone: stronger and more resistant to compressive forces. Does not contain marrow directly, but it surrounds the medullary cavity, which contains bone marrow.
Spongy bone: lighter and can withstand forces from multiple directions. Contains red bone barrow in spaces between the trabeculae
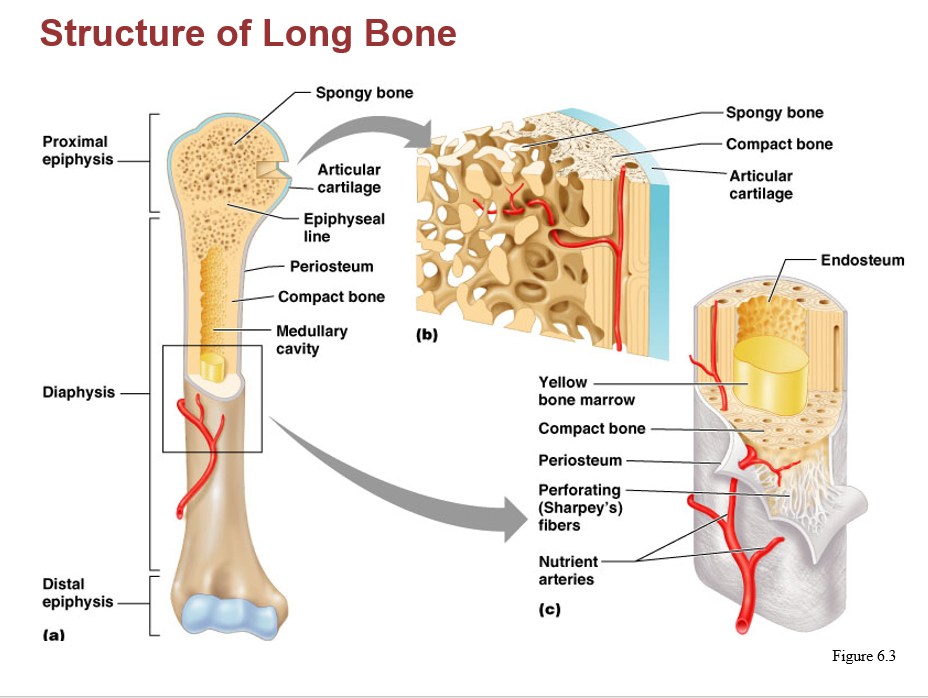
How are endosteum and periosteum similar to each other? How are they different? Be able to compare them to the perichondrium
They are all CTs involved in bone and cartilage growth, repair, and remodeling.
Periosteum is a tough sheath, covers the outer surface of the bone except for the areas covered by articular cartilage. Consists 2 layers: fibrous layer (outer) of dense irregular CT protects the bone from surrounding structures, anchors blood vessels and nerves to the surface of the bone, and serves as an attachment site for ligaments and tendons. Cellular layer (inner) includes osteoprogenitor cells, osteoblasts, and osteoclasts.
Endosteum is a very thin layer of CT containing osteoprogenitor cells, osteoblasts,and osteoclasts. it covers all internal surfaces of the bone within the medullary cavity.
Perichondrium is a dense irregular CT sheet that surrounds cartilage (specifically hyaline and elastic cartilage)
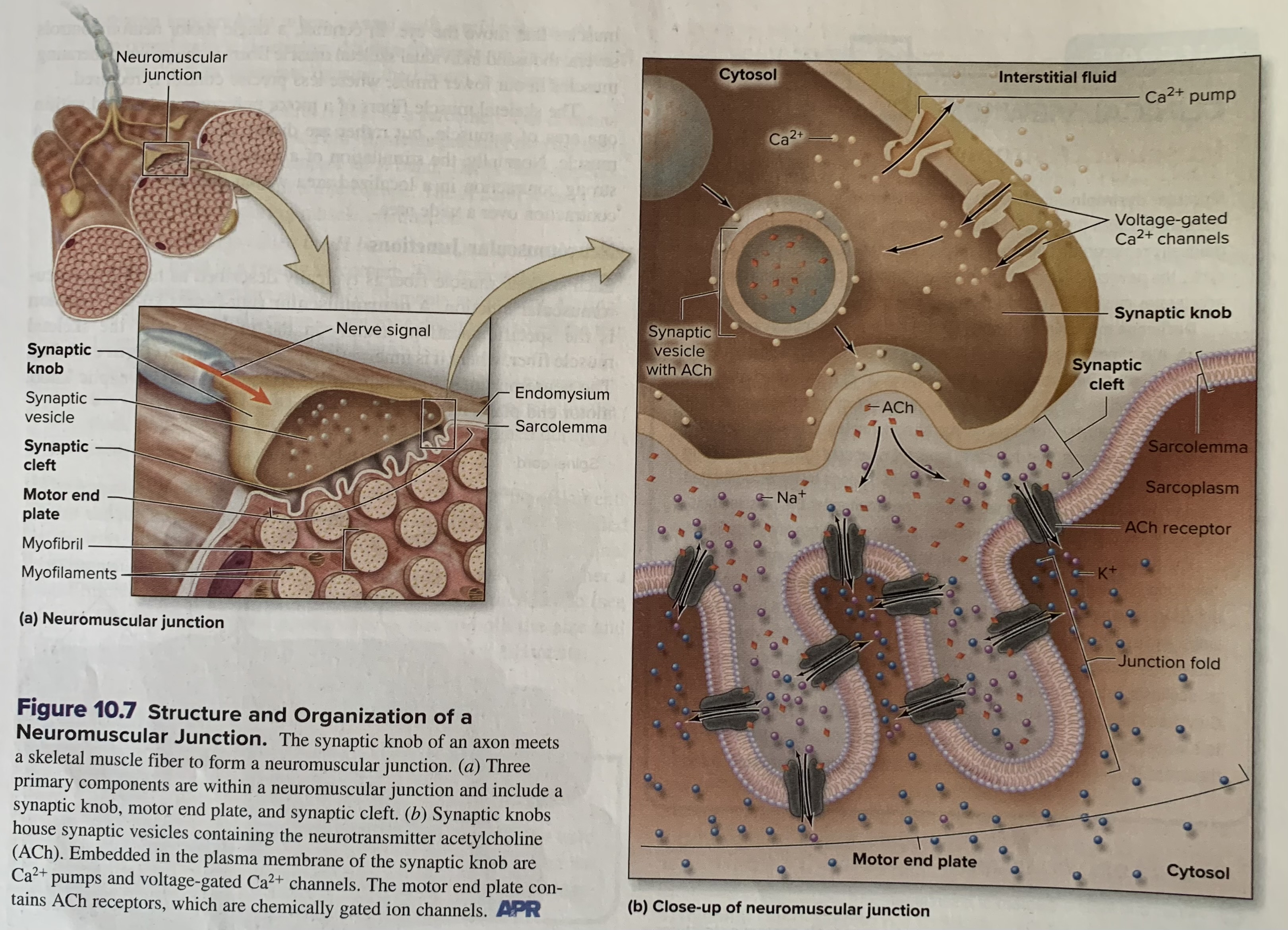
How is calcium used in the terminal branches of an axon?
In the terminal branches of axon, calcium ions play a crucial role in neurotransmitter release by triggering the fusion of synaptic vesicles with the cell membrane, a process known as exocytosis
How is calcium used in a contracting muscle?
Calcium plays a crucial role in muscle contraction by binding to regulatory proteins, exposing myosin binding sites on actin, and allowing the myosin heads to bind and initiate the sliding filament mechanism, leading to muscle contraction
Know the steps in the repair of a broken bone
A fracture hematoma forms
A fibrocartilaginous (soft) callus forms
A hard (bony) callus forms
The bone is remodeled
Sesamoid bone
small, sesame seed-shaped bones along the tendons of some muscles, are also classified as short bones. Acting as pulleys to redirect tendon forces and protect them from excessive wear and tear. They are composed of bone tissue.
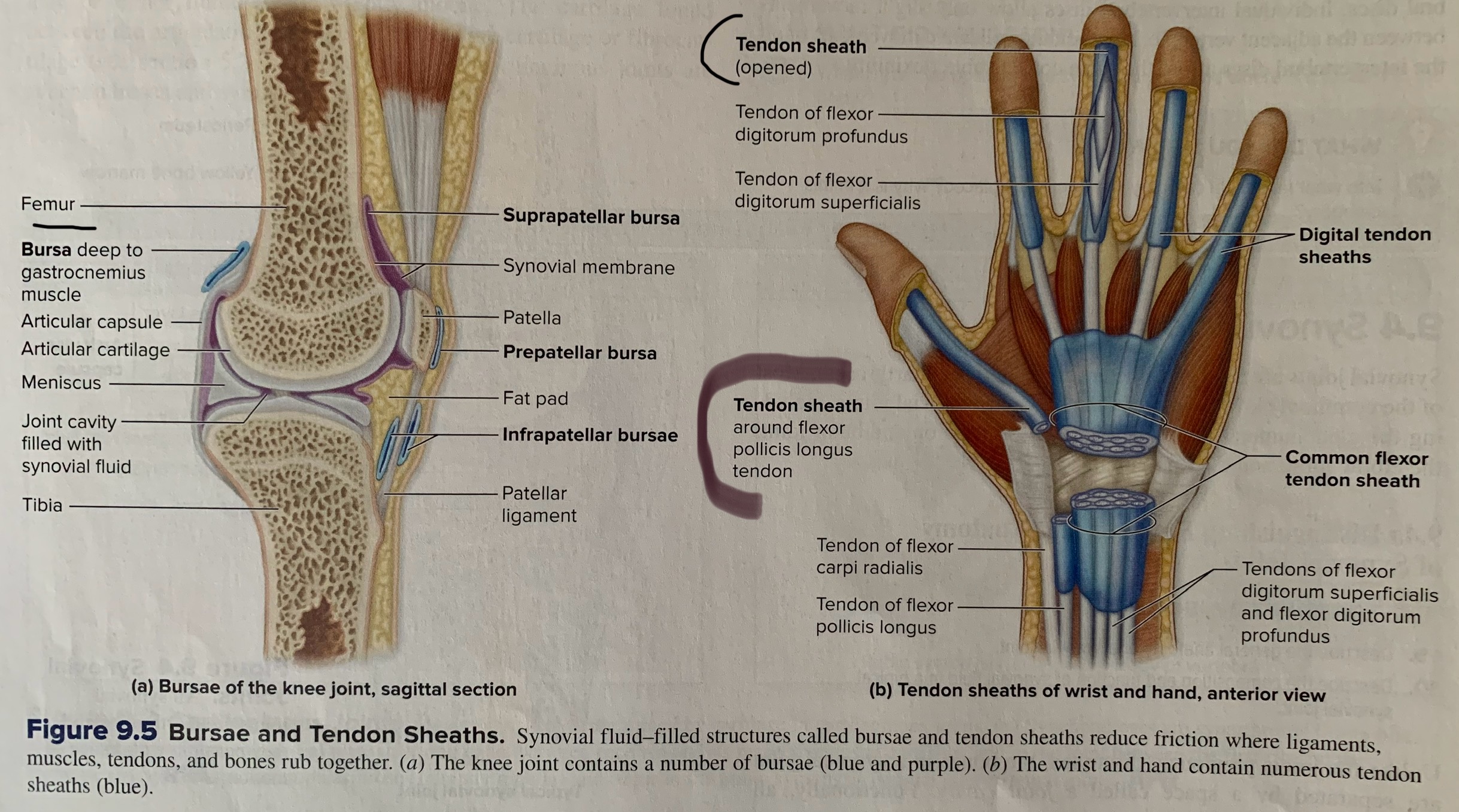
Bursa (bursae)
Is a fibrous, saclike structure that contains synovial fluid and is lined internally by a synovial membrane. Located between tendons, bones, and other tissues, acting as cushions and reducing friction between these structures during movement.
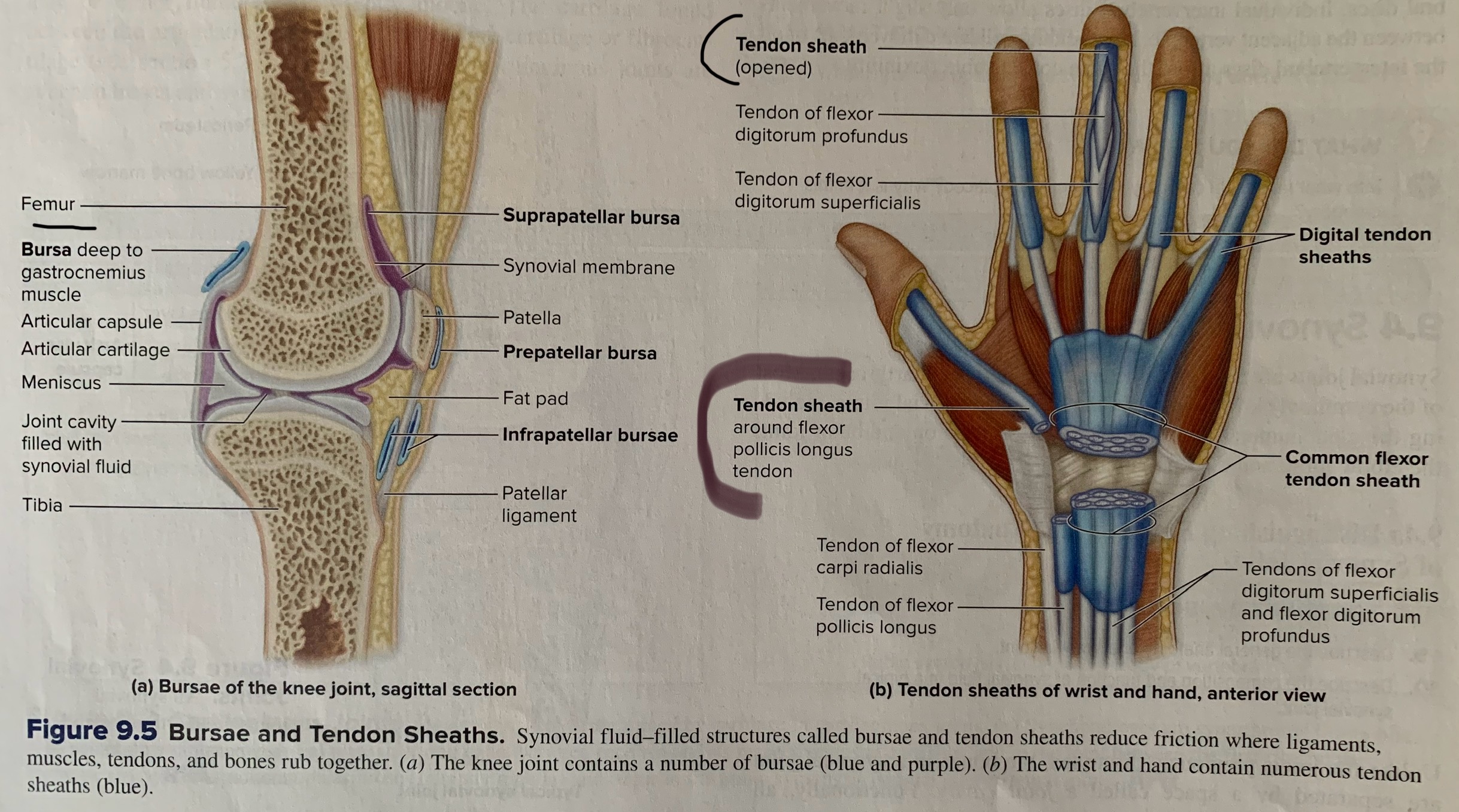
tendon sheath
An elongated bursa. Wraps around a tendon where there may be excessive friction. Tendon sheaths are especially common in the confined spaces of the wrist and ankle. They are composed of a fibrous layer and a synovial inner layer that secretes synovial fluid, which lubricates the tendon and allows for smooth gliding
What are the five functions of the skeletals (pg. 328)
Move the body
maintain posture
protect and support
regulate elimination of materials
produce heat
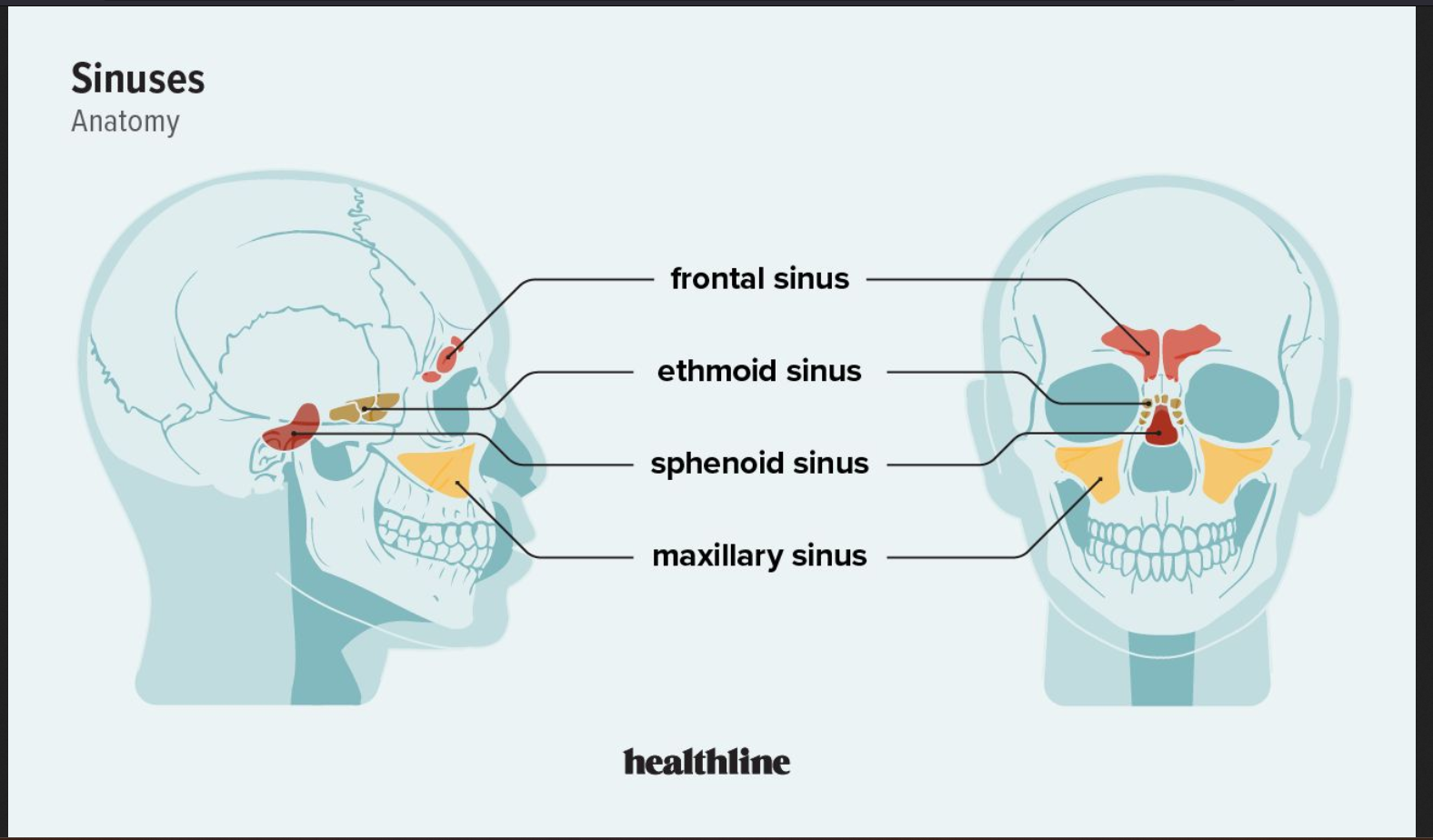
What are the paranasal sinuses, and which bones have them
Paranasal sinuses are air-filled spaces within the bones surrounding the nasal cavity, lined with a mucous membrane that produces mucus to keep the nasal passages moist.
They types of bones that have paranasal sinuses:
Frontal sinuses, maxillary sinuses, ethmoid sinuses, sphenoid sinus
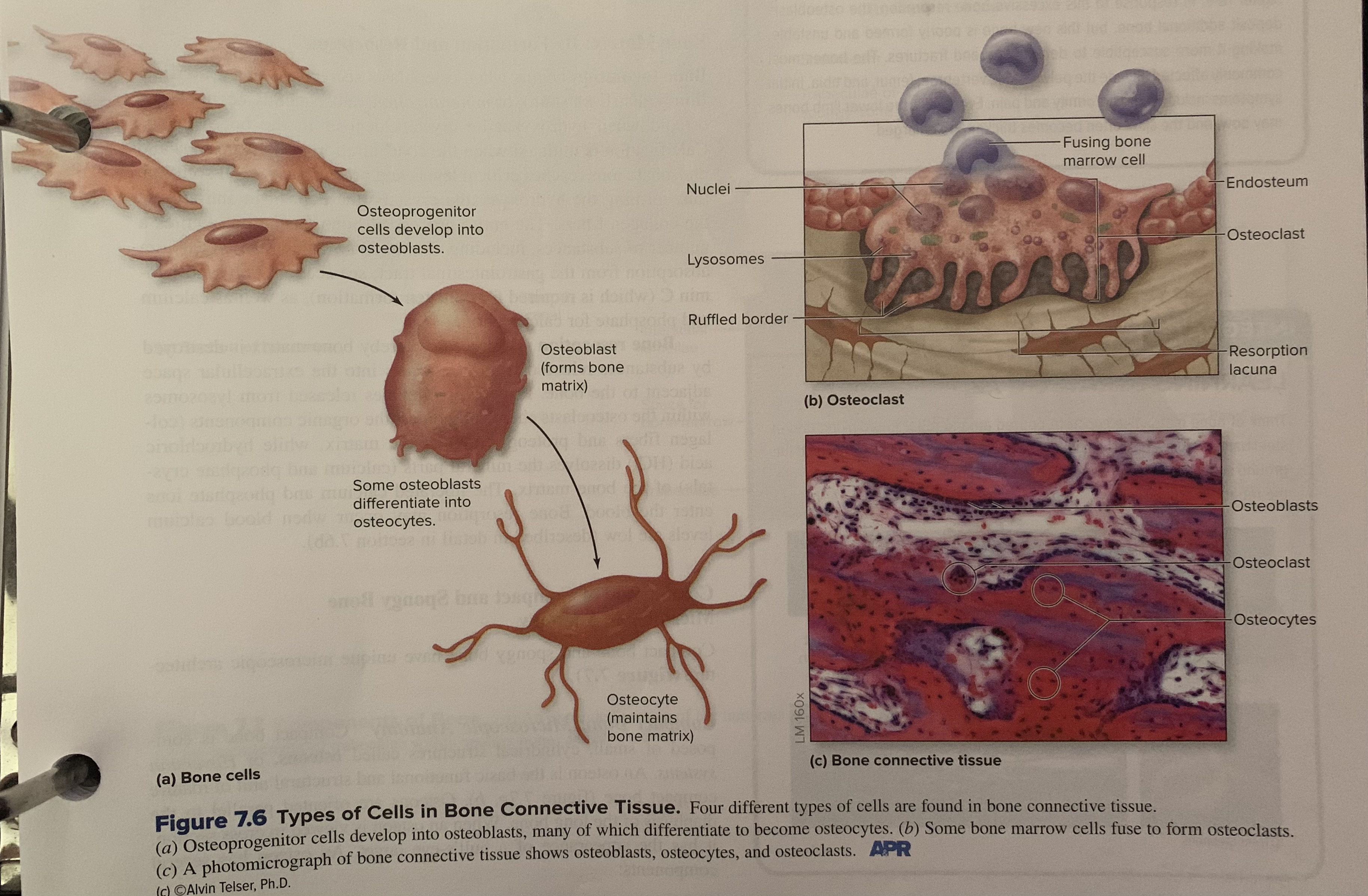
What are the roles of these cells in bone: osteoprogenitor, osteoblast, osteoclast, osteocyte
Osteoprogenitor Cells (Osteogenic Cells):
These are the stem cells of bone, residing in the bone marrow and serving as the precursors to osteoblasts. They are responsible for bone repair and growth.
Osteoblasts:
These cells are responsible for synthesizing and storing new bone tissue, forming the organic matrix (osteoid) of bone, which then mineralizes to form hard bone. They also regulate osteoclasts.
Osteoclasts:
These are large, multinucleated cells that break down bone tissue (bone resorption) to release minerals, like calcium and phosphate, back into the bloodstream.
Osteocytes:
These are mature bone cells that are derived from osteoblasts that have become trapped within the bone matrix. They maintain bone structure by regulating mineral concentration, and they act as mechanosensors, detecting stress and damage to bone, which can trigger bone remodeling.
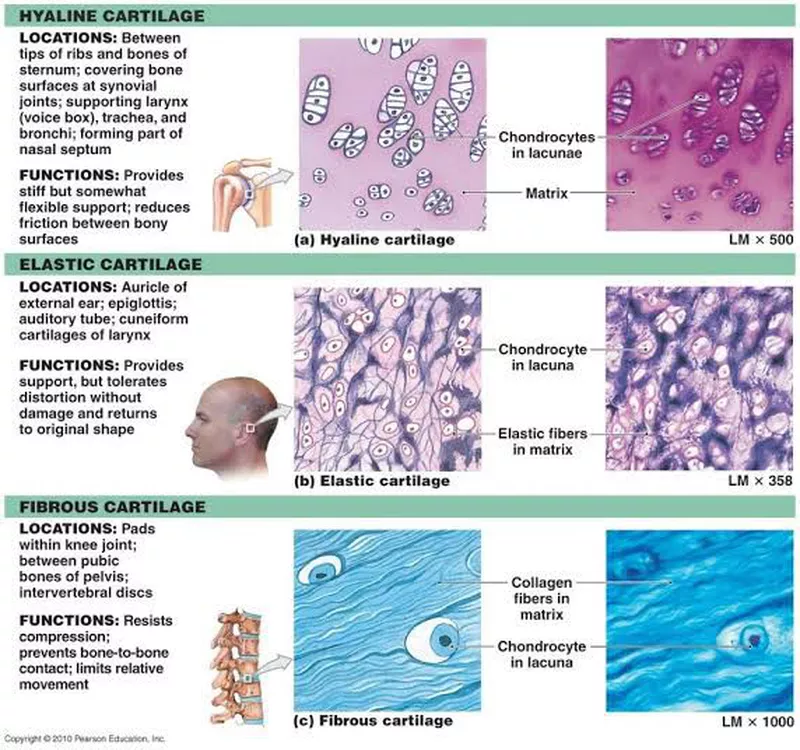
What are the three types of cartilage? Which is the most common? Which is best at shock absorption? Which is best at springing back after it Is bent?
Hyaline cartilage: The most common type, found in areas like the trachea, rib tips, and articular surfaces of bones.
Elastic cartilage: Provides flexible support, found in the external ear, epiglottis, and larynx. Is best at springing back after bending.
Fibrocartilage: The toughest type, found in areas like the intervertebral discs and menisci of the knee, providing shock absorption and support. Is best at shock absorption.
What are the two ways that bone forms? Which method forms our flat bones?
The 2 ways bone form are:
intramembranous ossification: Involves the direct transformation of mesenchymal tissue into bone. Forms the flat bones of the skull, clavicle, and some facial bones. Also plays a role in bone healing and remodeling.
endochondral ossification: Involves the formation of a cartilage model that is then gradually replaced by bone. Forms most of the long bones and some irregular bones. This process is essential for the growth of log bones during childhood and adolescence.
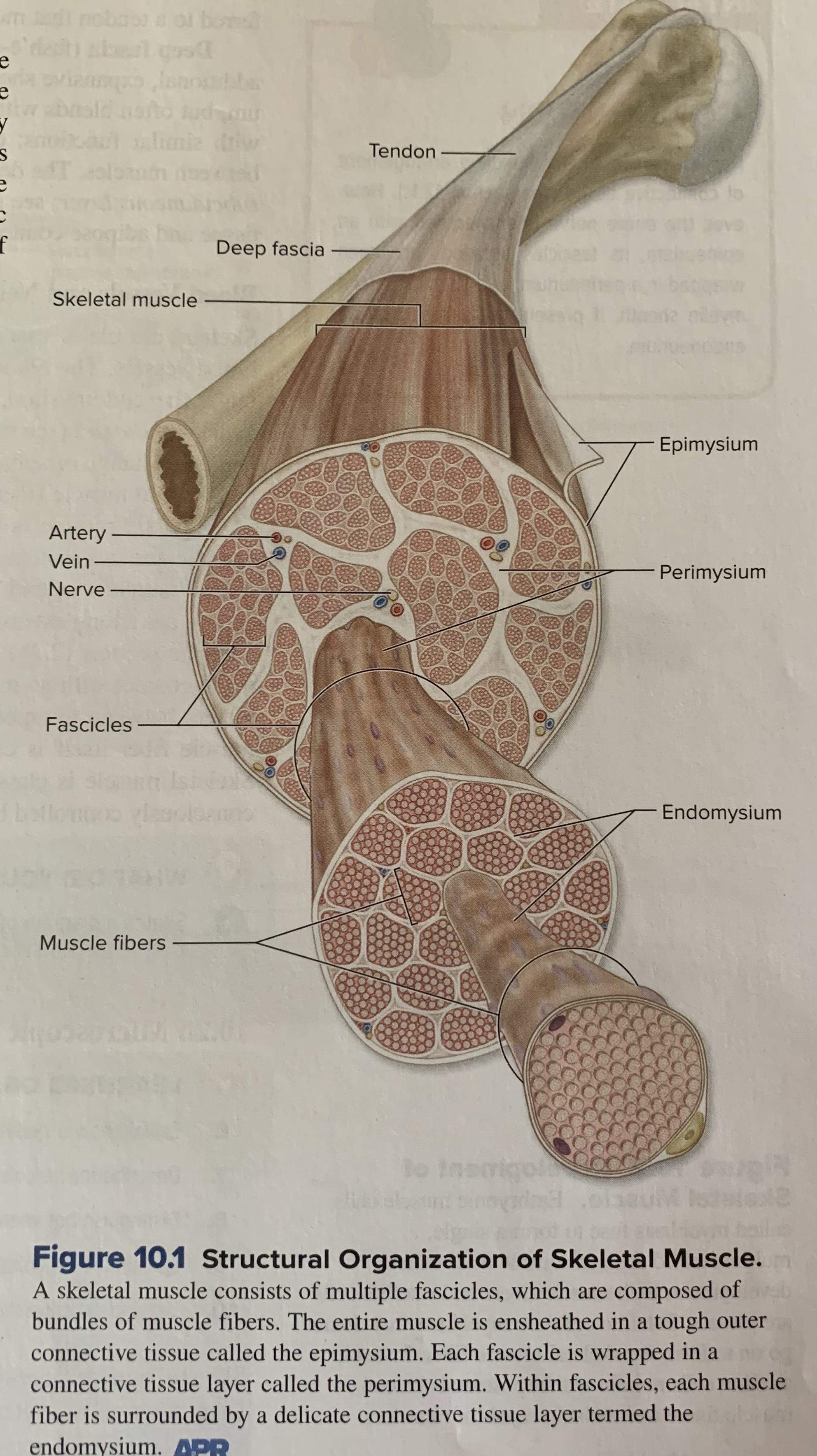
Epimysium
Is a layer of dense irregular CT that surrounds the whole skeletal muscle. This fibrous tissue ensheathes the entire skeletal muscle to protect and support it like a tough leather sleeve.
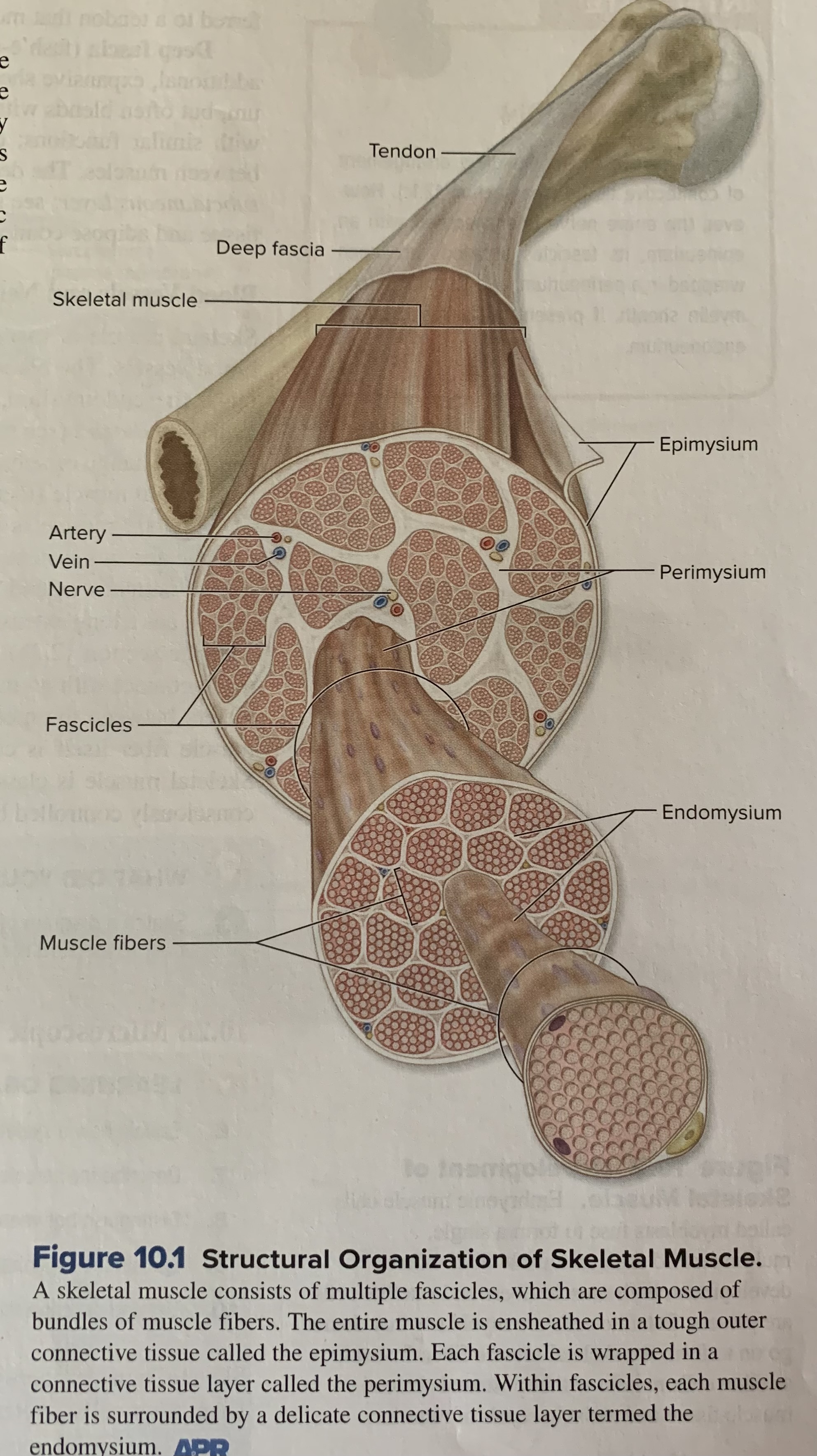
perimysium
Is a layer of dense irregular connective around each fascicle. These tough, fibrous CT sleeves also provide protection and support, but to each bundle of muscle fibers.
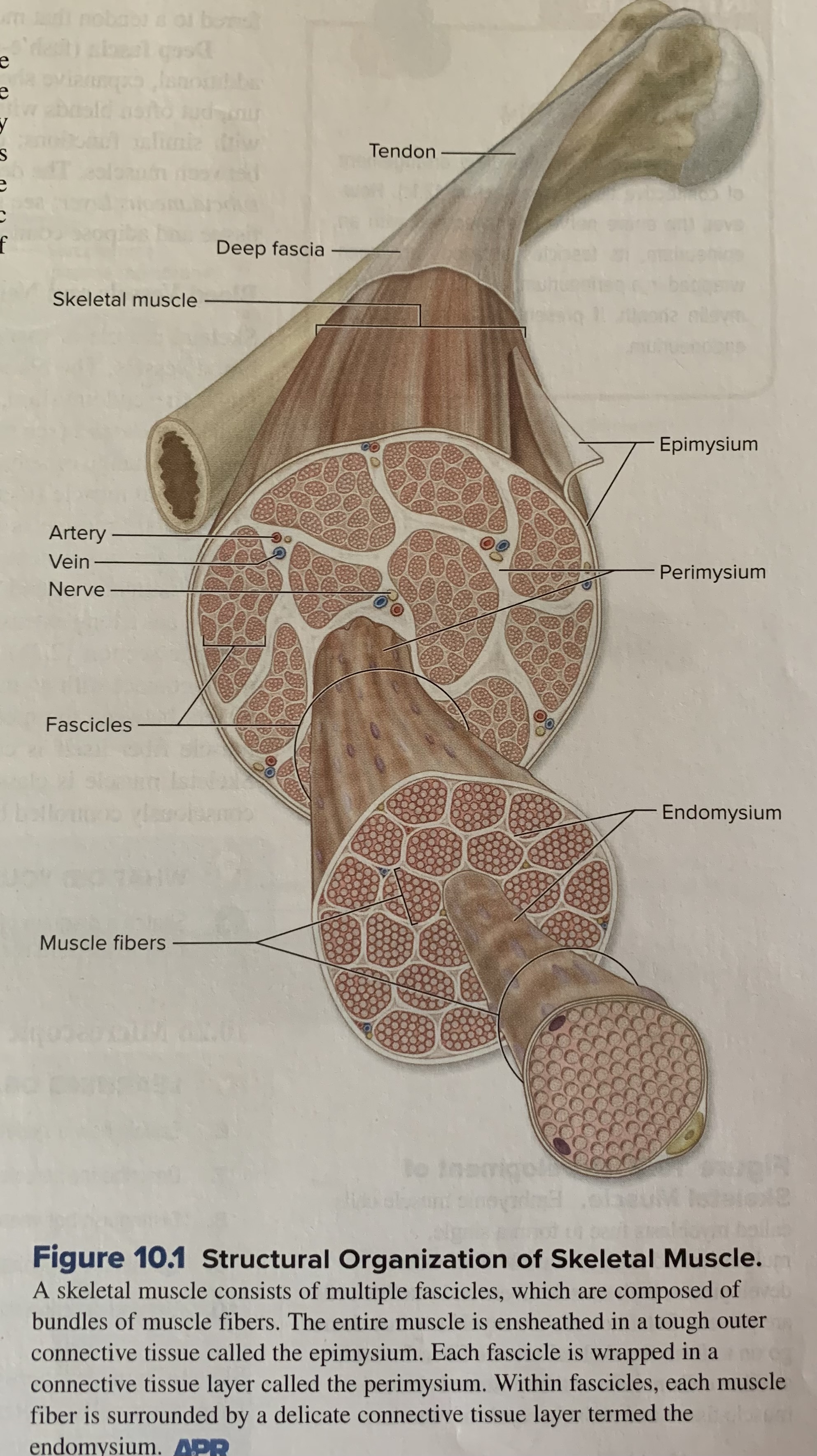
endomysium
Is composed of areolar CT that surrounds each muscle fiber. These more delicate coverings function to electrically insulate the muscle fibers
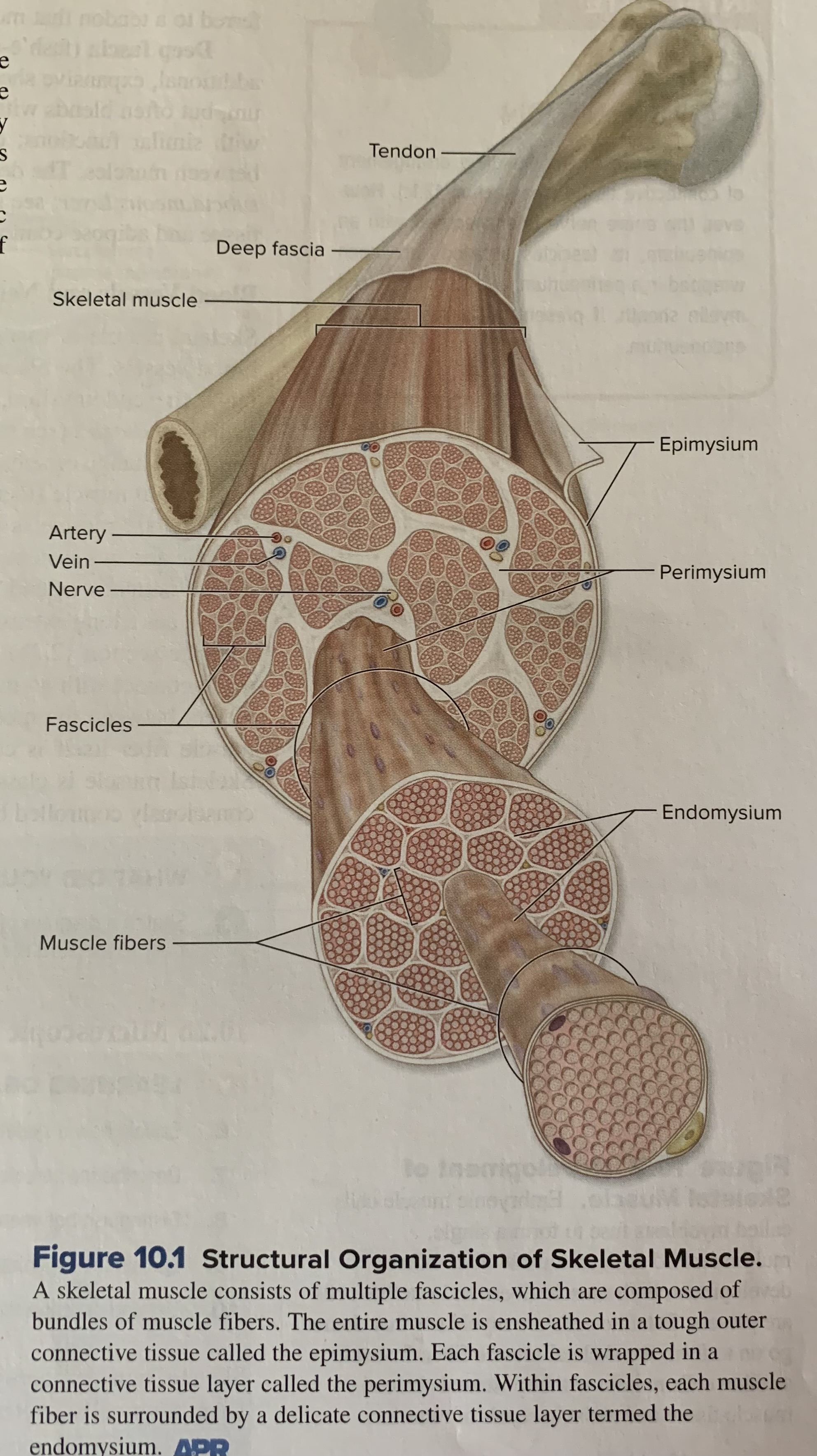
fascicle
Many muscle fibers are bundled within a fascicle and many fascicles are bundled within the whole skeletal muscle.
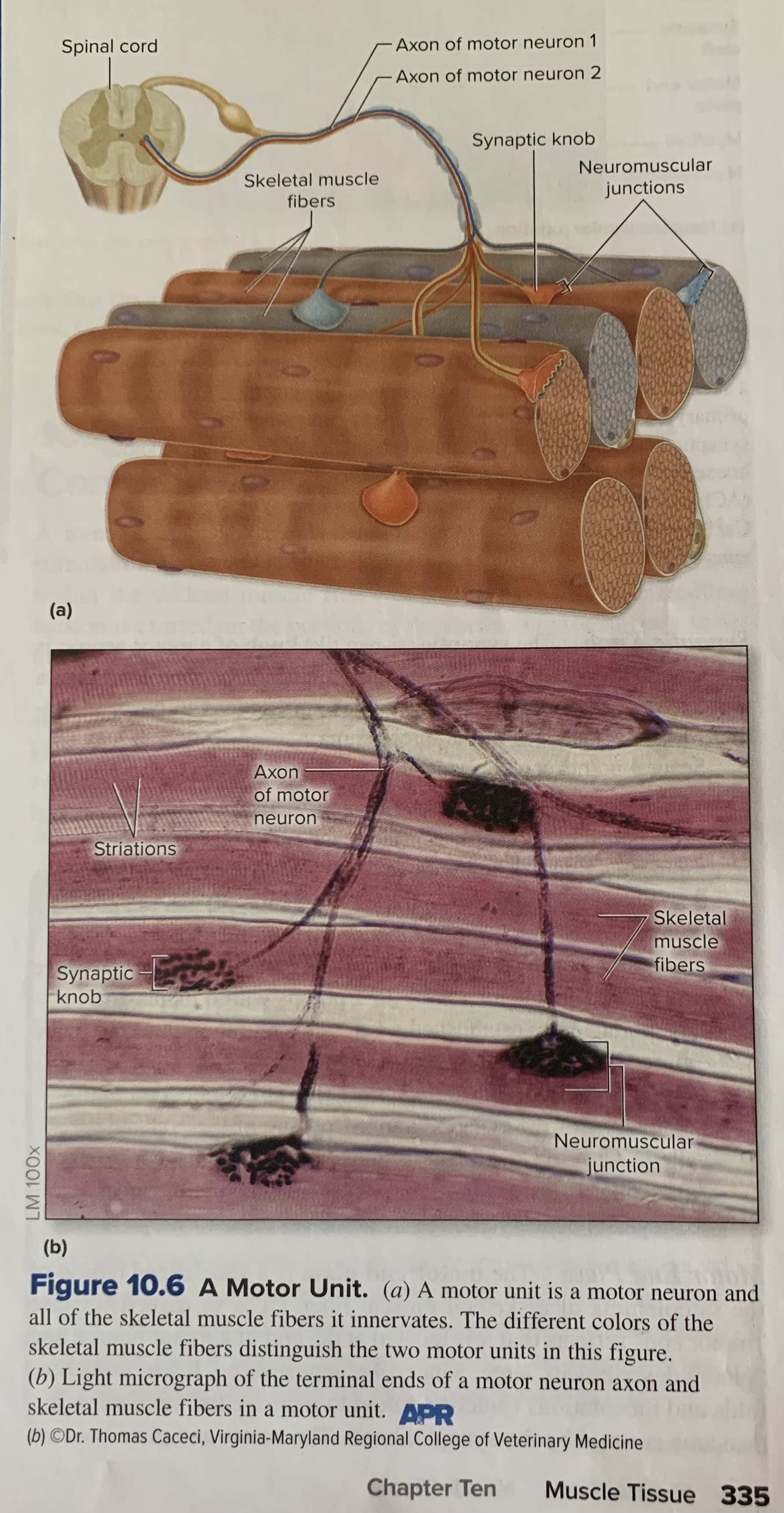
motor unit
A single motor neuron and the skeletal muscle fibers it controls
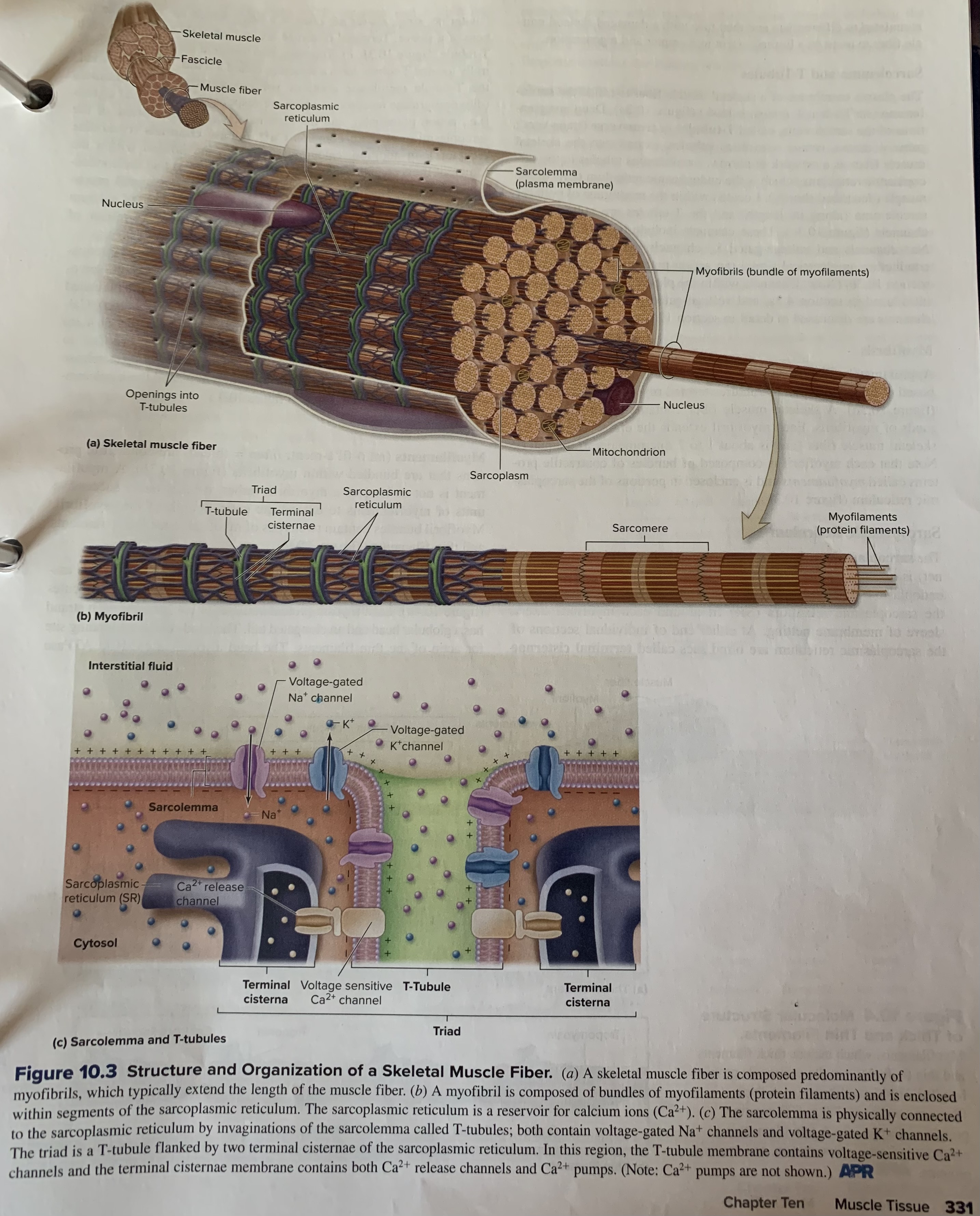
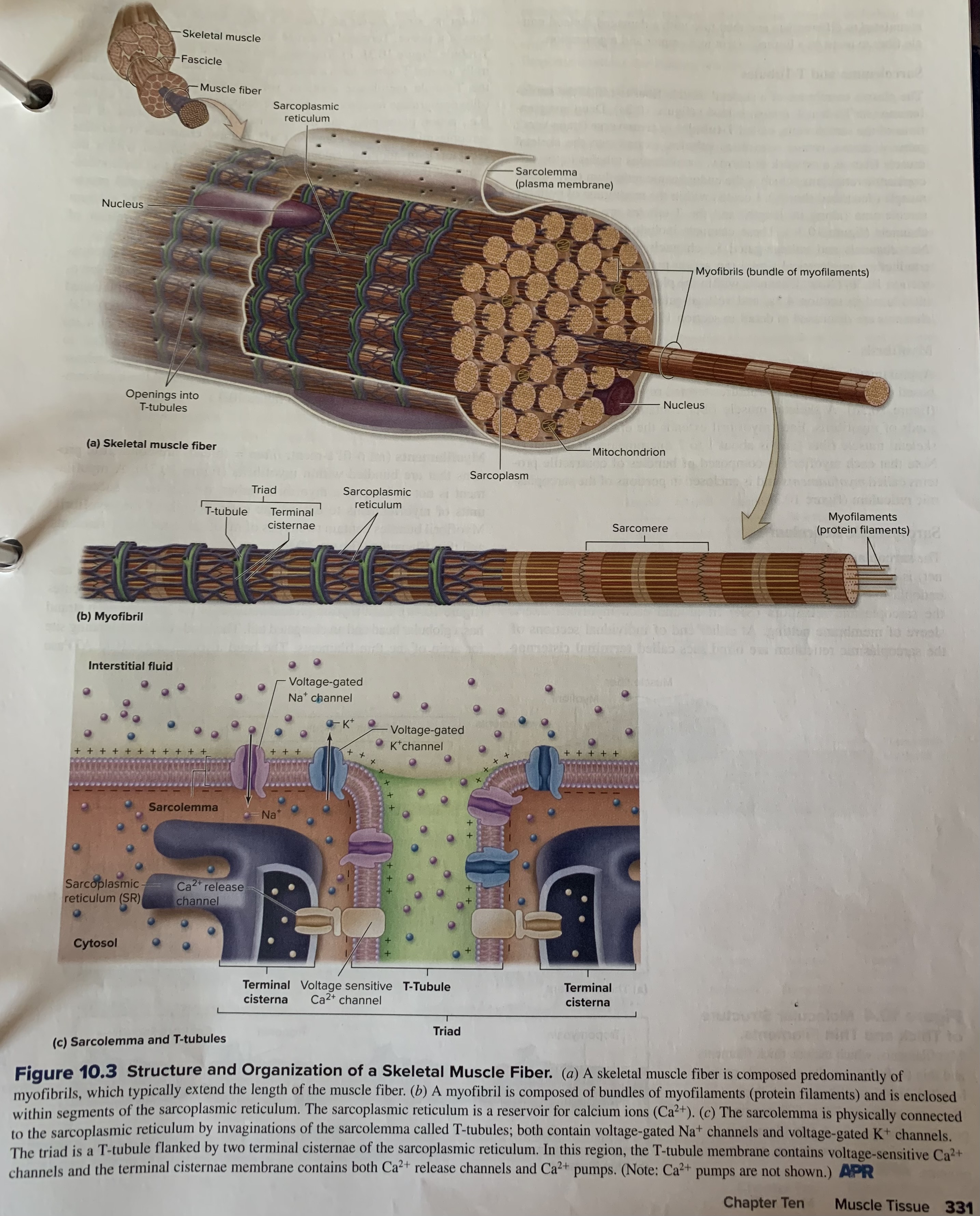
sarcolemma
The plasma membrane of a skeletal muscle fiber
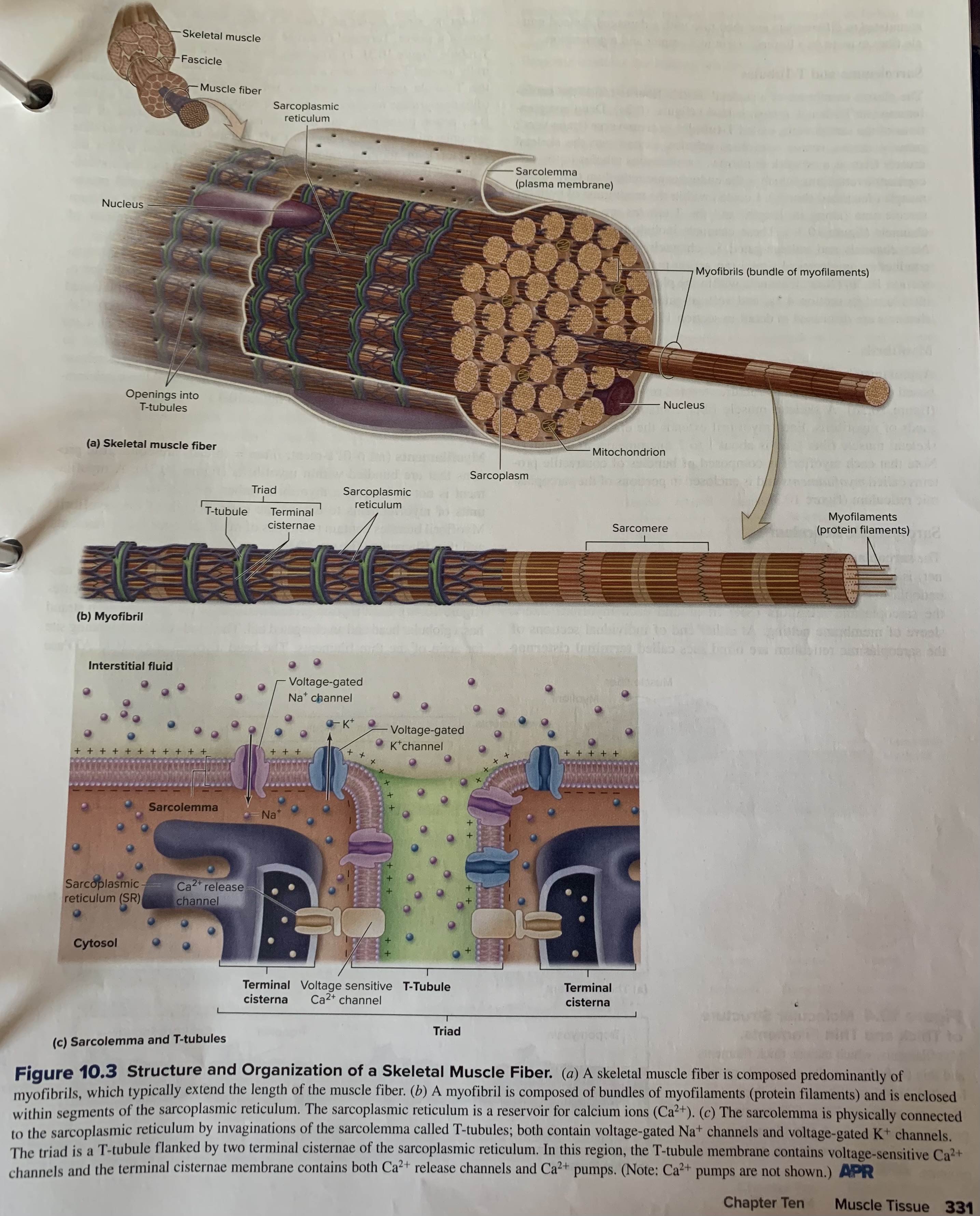
sarcoplasmic reticulum
Is an internal membrane complex that is similar to the smooth endoplasmic reticulum of other cells. Is a specialized form of the endoplasmic reticulum found in muscle cells, primarily responsible for storing and releasing calcium ions, which are crucial for muscle contraction and relaxation.
The SR is a network of tubules and cisternae that surrounds each myofibril (the functional unit of a muscle cell)
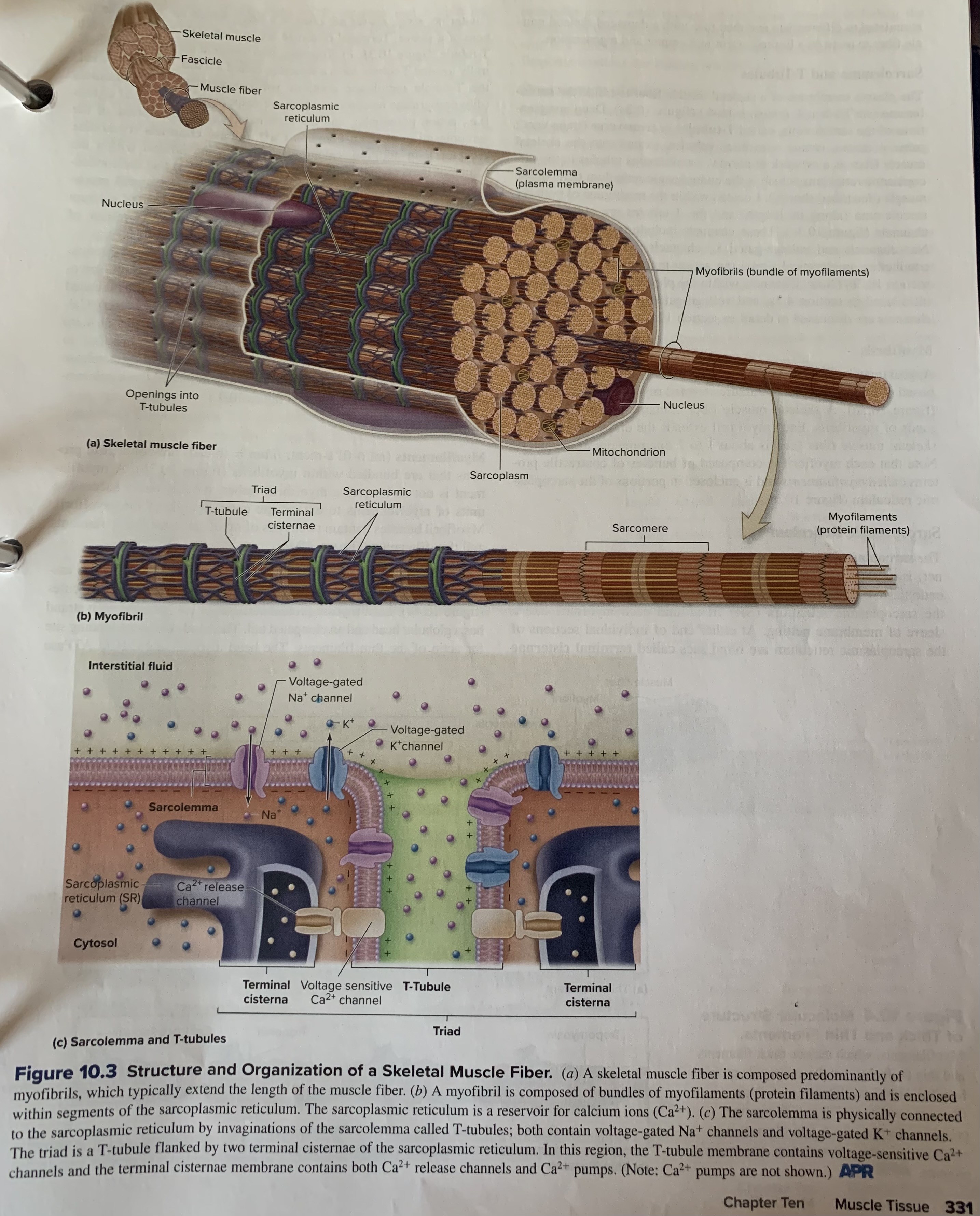
T-tubules (or transverse tubules)
Deep invaginations of the sarcolemma. Extend into the skeletal muscle fiber as a network of narrow, membranous tubules to the sarcoplasmic reticulum, which is the endoplasmic reticulum (ER) of the muscle (describe shortly).
sarcoplasm
Cytoplasm in skeletal muscle fibers.
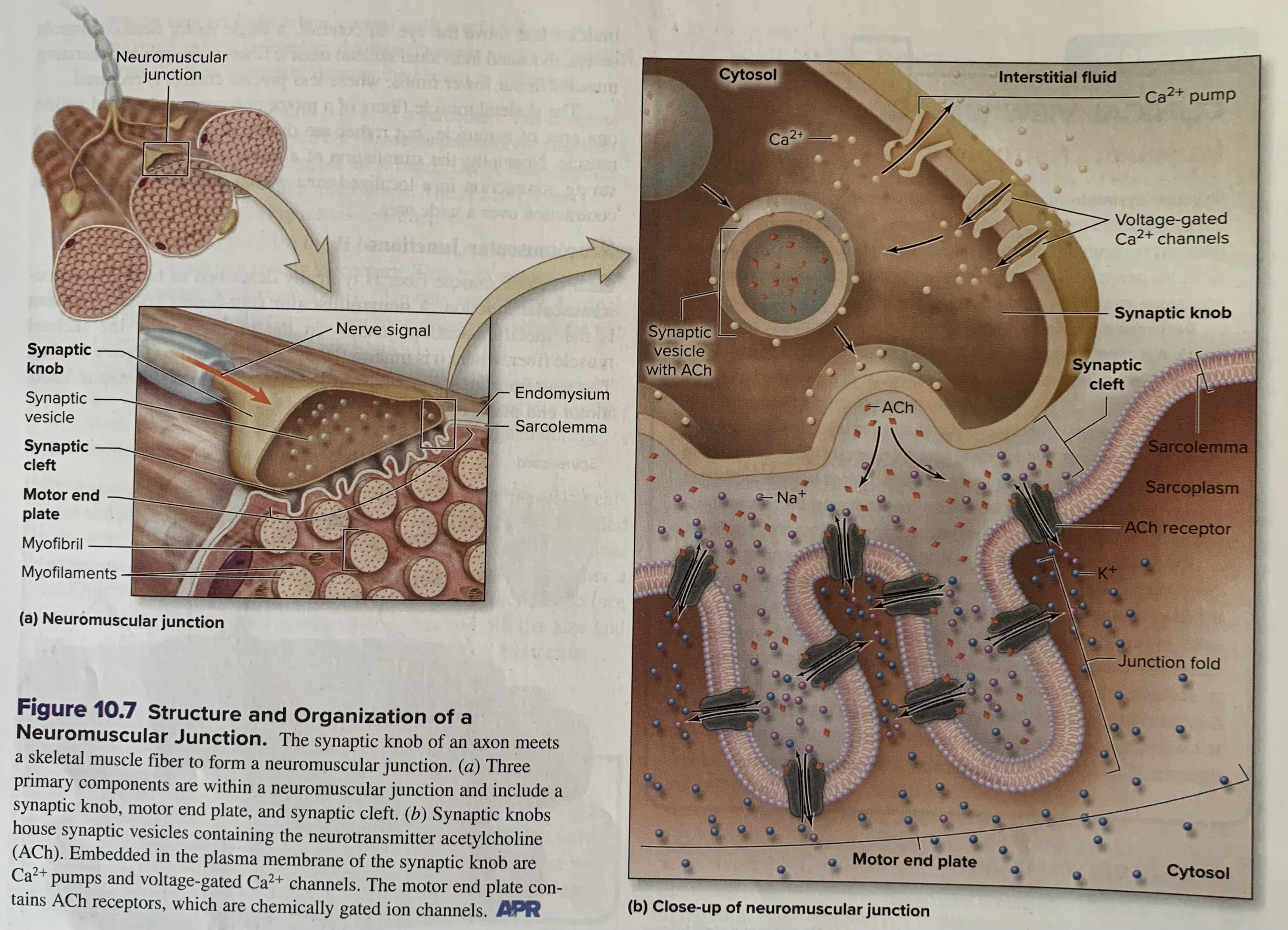
neuromuscular junction
Each skeletal muscle fiber is typically described as having one neuromuscular junction. Is the specific location, usually in the mid-region of the skeletal muscle fiber, where it is innervated by a motor neuron. The nueromuscular junction has the following parts: synaptic knob, motor end plate, and synaptic cleft.
synapse
Is a junction where a neuron (or nerve cell) communicates with another neuron, a muscle cell, or a gland cell, transmitting electrical or chemical signals.
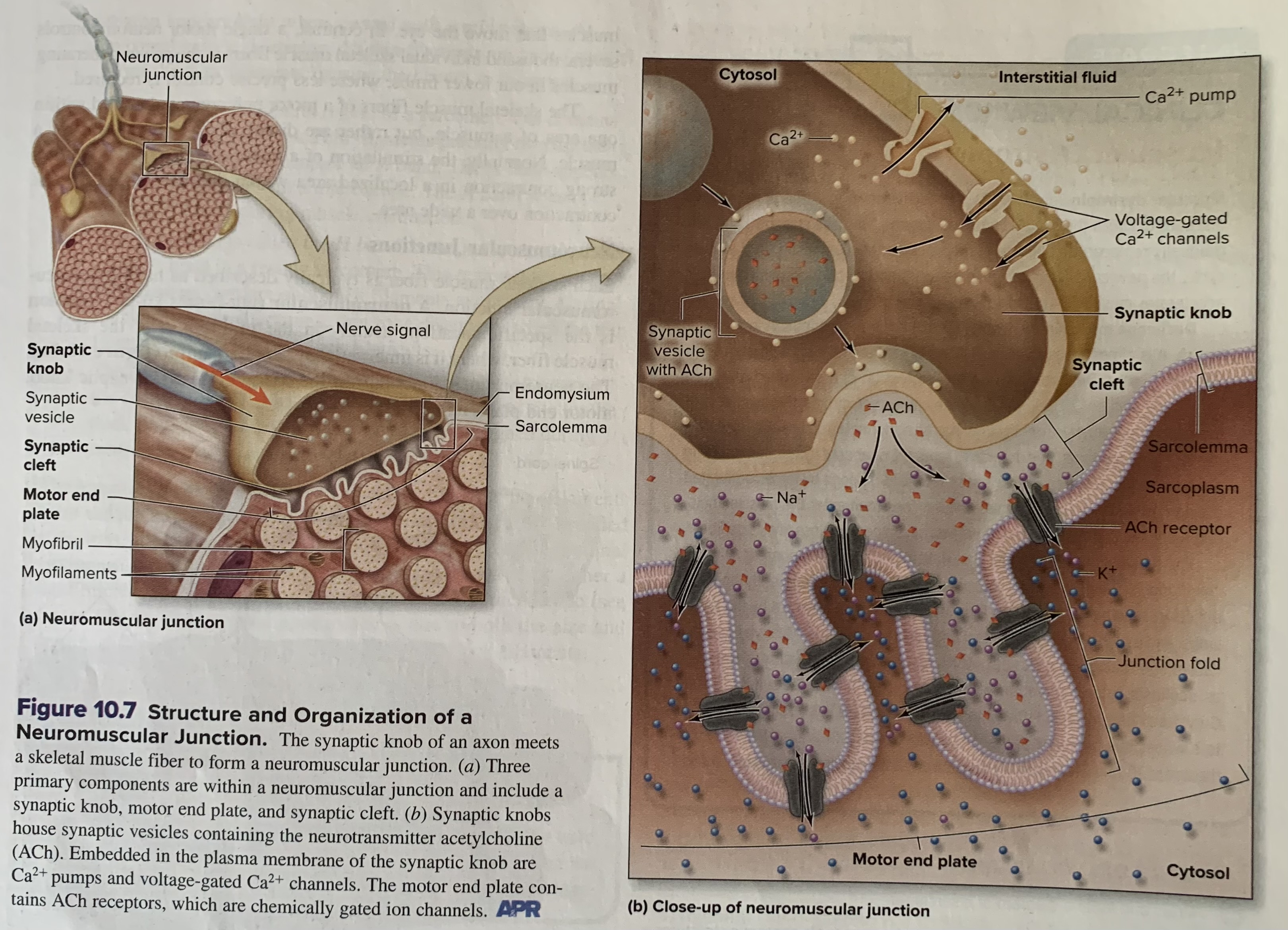
synaptic cleft
Is an extremely narrow (30 nanometers), fluid filled space separating the synaptic knob and the motor end plate.
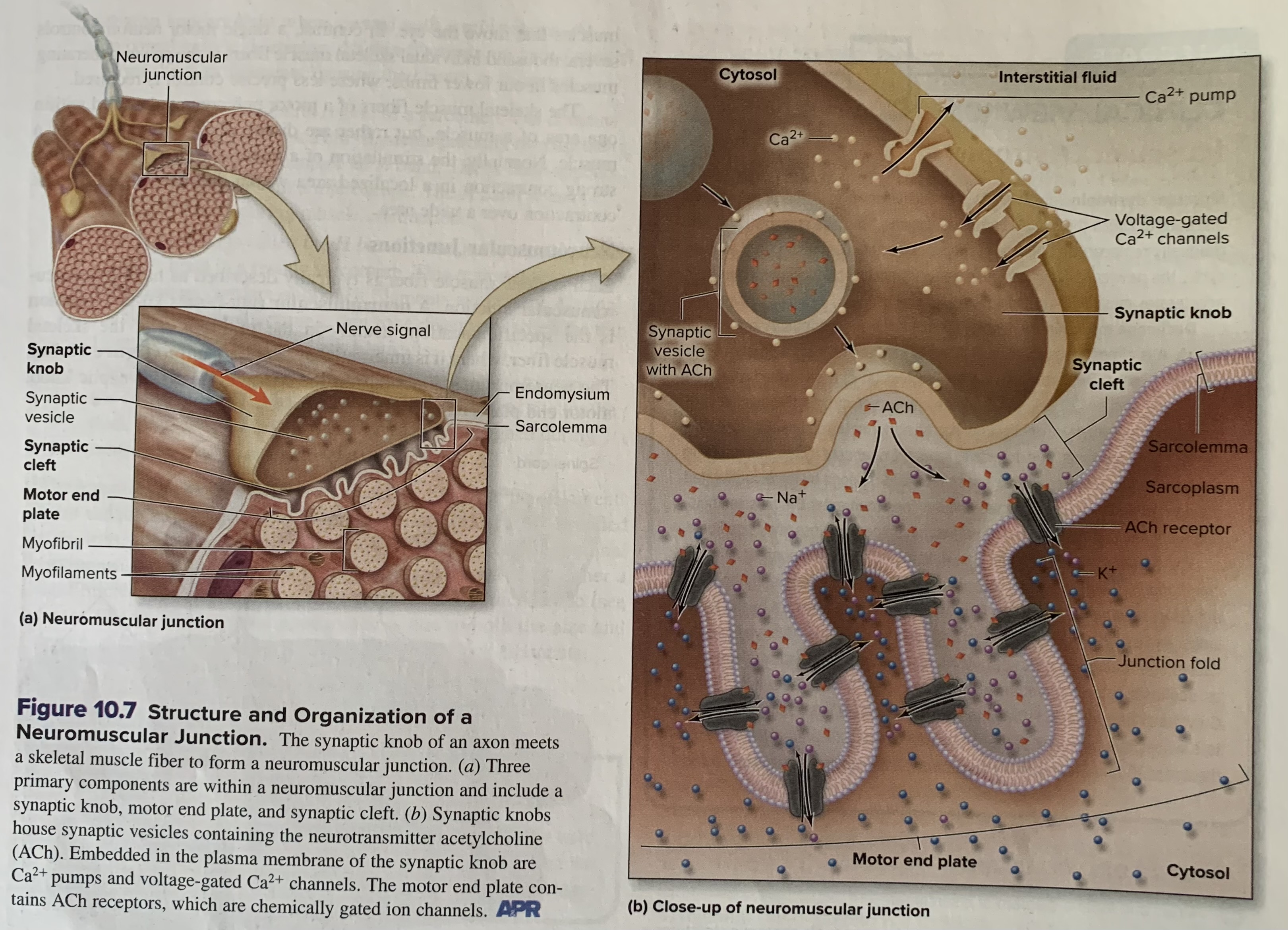
Acetylcholine (ACh)
Acts as a neurotransmitter, meaning it’s released by motor neurons to stimulate muscle contraction by biding to nicotinic acetylcholine receptors (nAChRs) on the muscle cell membrane, leading to muscle fiber depolarization and contraction
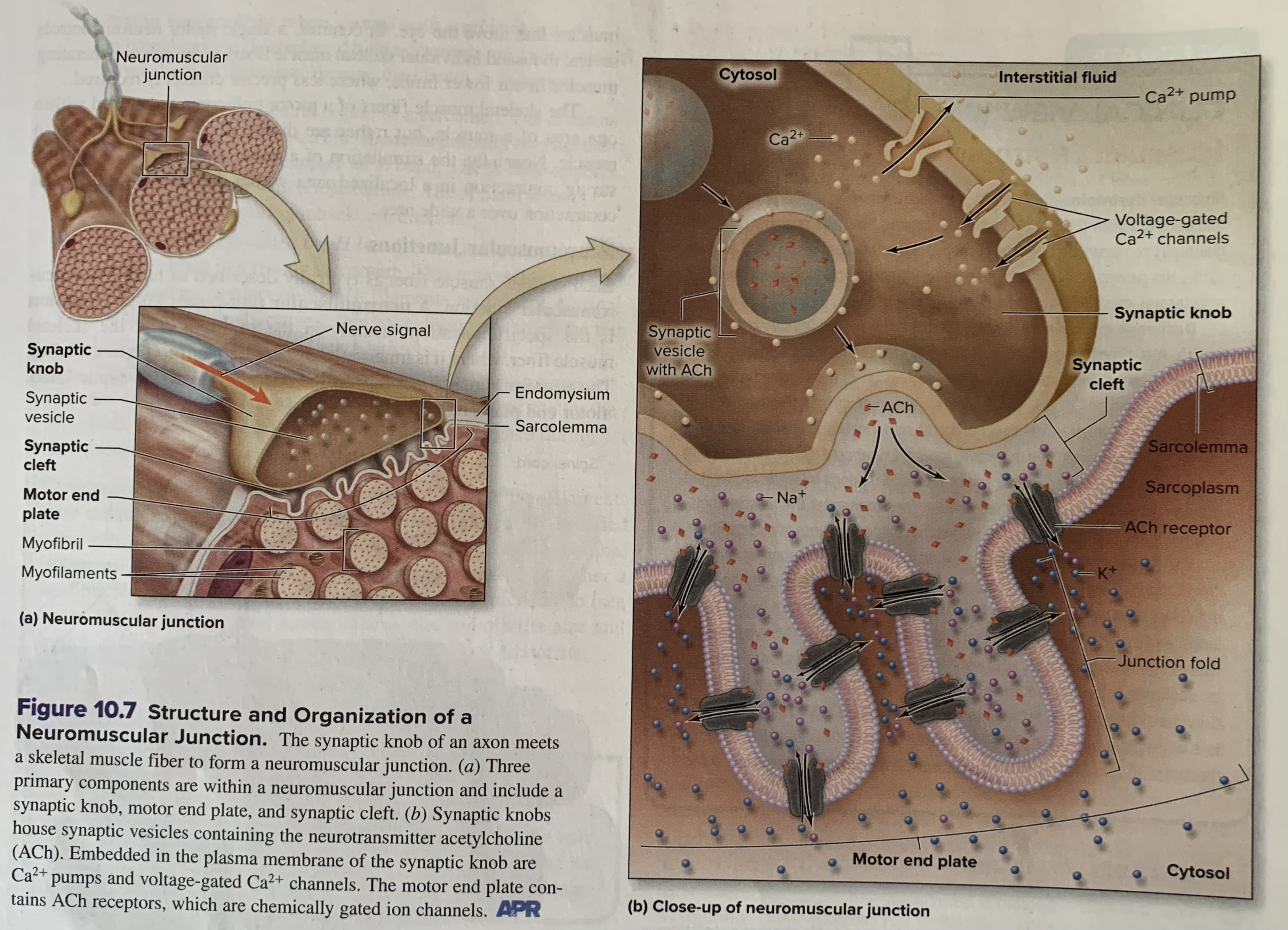
acetylcholinesterase (AChE)
(AChE) resides within the synaptic cleft and quickly breaks down ACh molecules following their release into the synaptic cleft.
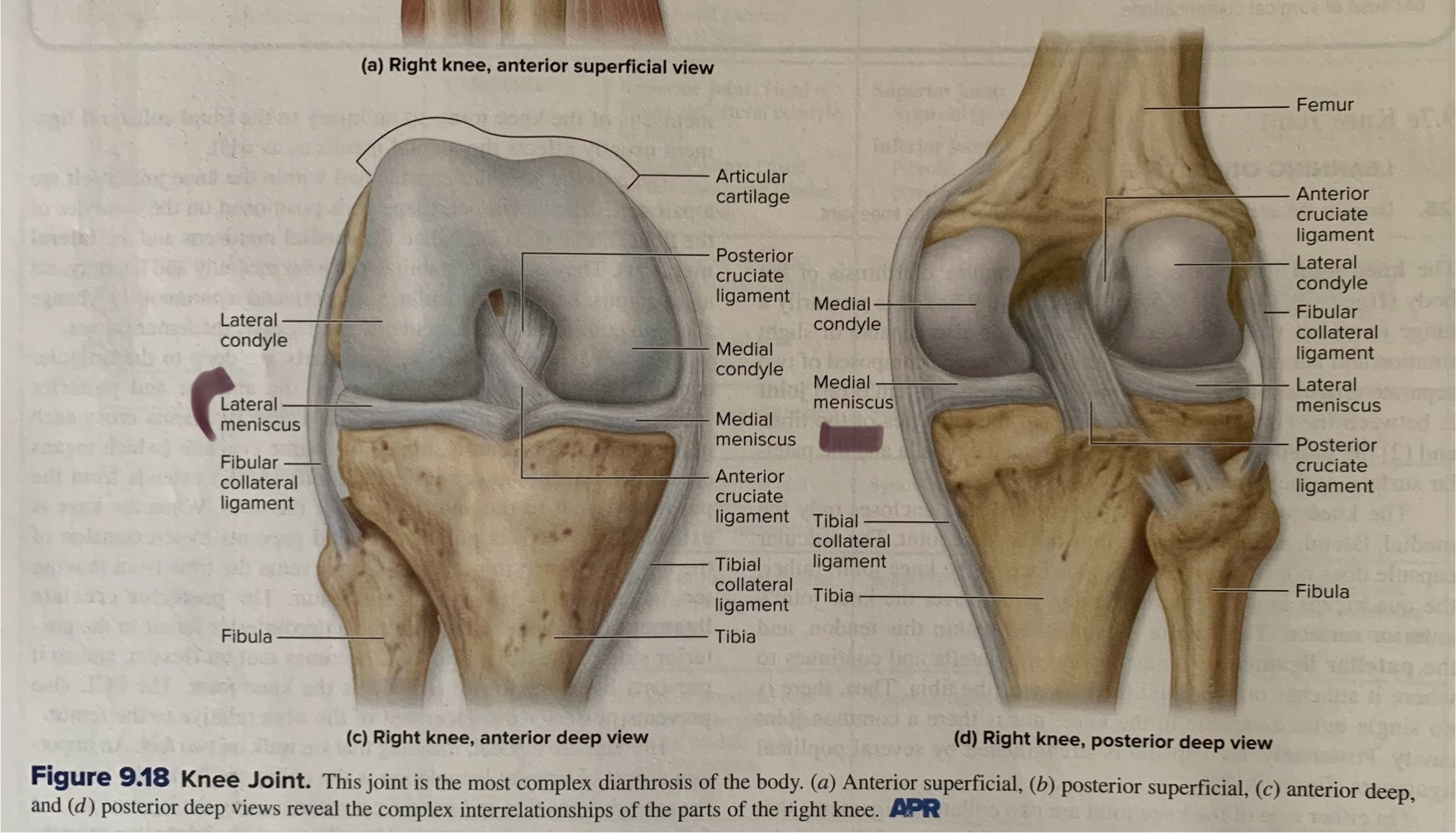
What is a meniscus
Deep to the articular capsule and within the knee joint itself are a pair of C shaped fibrocartilage pads positioned on the condyles of the tibia. These pads are called medial meniscus and the lateral meniscus. They are partially stabilize the joint medially and laterally, act as cushions between articular surfaces, and continuously change shape to conform to the articulating surfaces as the femur moves

What is osteoporosis? Be able to describe some of the symptoms. What vitamin(s) are usually prescribed to patients with osteoporosis?
meaning porous bone, is a disease that results in decreased bone mass and leads to weakened bones that are prone to fracture. The most common fracture sites are the wrist, hip, and vertebral column.
Osteoporosis is often called a “silent disease” bc there are usually no symptoms until a bone is broken.
Vitamin D and calcium supplements are frequently prescribed to help manage osteoporosis.
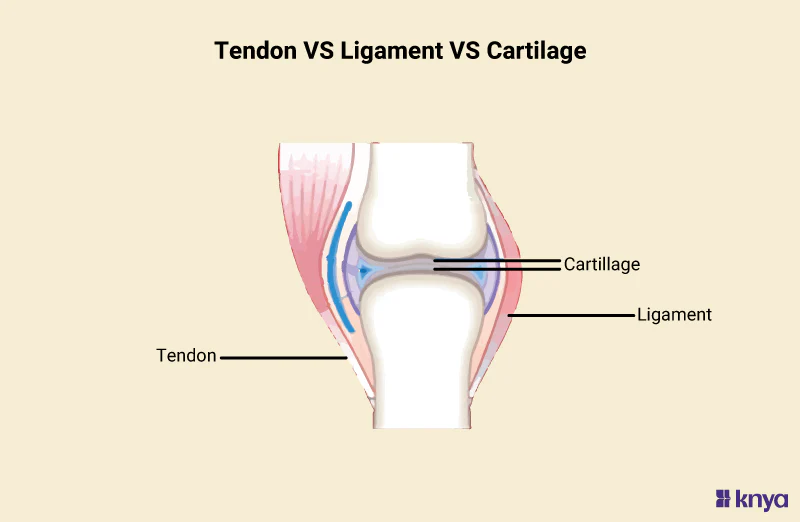
What is the difference between a tendon and a ligament
Ligaments are composed of dense regular CT, and they connect 1 bone to another bone. Ligaments function to stabilize, strengthen, and reinforce most synovial joints.
Tendons are like ligaments and are composed of dense regular CT, but they are not part of the synovial joint. A tendon attaches a muscle to a bone. When a muscle contracts, the tendon from that muscle moves the bone to which it is attached, thus causing movement at the joint.
What role do chondroblasts play in cartilage?
Chondroblasts are immature cartilage cells that play a crucial role in cartilage development and growth by secreting extracellular matrix components, including collagen and proteoglycans, which form the cartilage matrix
What cell type is found in the lacunae of hyaline cartilage?
The chondrocyte, a specialized cartilage cell, is found within the lacunae of hyaline cartilage, where it plays a crucial role in synthesizing and maintaining the extracellular matrix
Where is an epiphyseal growth plate found? What is it made of? How are growth plates related to gigantism and acromegaly? What hormone is involved in these conditions?
The epiphyseal growth plate is a hyaline cartilage plate found in the metaphysis (the area between the diaphysis and epiphysis) at each end of long bones in children and adolescents, where bone lengthening occurs.
Gigantism, characterized by excessive height in children, and acromegaly, involving abnormal bone and tissue growth in adults, are both linked to excessive growth hormone (GH) production, with the key difference being the timing of GH excess relative to the closure of growth plates.
Hormone involved: Both conditions are caused by excessive secretion of growth hormone (GH)
Be able to explain the steps in muscle contraction and place them in correct order. When is ATP used? When is calcium used? (pg. 344)
Muscle contraction involves a series of steps: a nerve signal triggers calcium release, which binds to troponin, exposing binding sites on actin, allowing myosin heads to bind, forming cross-bridges. Myosin then pulls actin, shortening the muscle, and ATP provides the energy for this process, while calcium is crucial for initiating the contraction and breaking the crossbridges.
The roles of the following chemical in muscle contraction: sodium ions (Na+):
When an action potential reaches the muscle fiber, sodium ions rush into the cell, depolarizing the membrane and triggering the release of calcium ions from the sarcoplasmic reticulum
The roles of the following chemical in muscle contraction: potassium ions (K+):
After the muscle fiber is depolarized by sodium influx, potassium ions move out of the cell, helping to restore the membrane potential and prepare for the next contraction.
The roles of the following chemical in muscle contraction: calcium ions (Ca2+):
Calcium ions bind to troponin, causing a conformational change that shifts tropomyosin away from the actin binding sites, allowing myosin to bind and initiate muscle contraction.
The roles of the following chemical in muscle contraction: troponin
This protein complex is attached to tropomyosin and acts as a calcium sensor. When calcium binds to troponin, it undergoes a conformational change that moves tropomyosin.
The roles of the following chemical in muscle contraction: tropomyosin
A protein molecule that covers the actin binding sites, preventing myosin from binding to actin when the muscle is relaxed.
The roles of the following chemical in muscle contraction: actin
The thin filament in a muscle fiber that myosin binds to during contraction.
The roles of the following chemical in muscle contraction: myosin
The thick filament in a muscle fiber that pulls on the actin filaments to cause contraction.