Medicines reconciliation
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
what is a medication history
a list of what the patient is currently taking, recently stopped taking and other changes made to their regime
when is a medication history needed
during any patient encounter
GP appointment
Admission to hospital
Out-patient clinical appointment
Pharmacy first consultation
Request for OTC medicine / minor ailment advice
what is the importance of accurate medication histories
helps inform prescribing decisions
Avoid duplication of therapy
Avoid unnecessary polypharmacy
Avoid hazardous interactions
Adverse drug reactions may explain patient’s symptoms
Contribute to approximately 16.5% of hospital admissions
May be delayed – e.g. flucloxacillin-induced cholestasis
Some medicines need withholding prior to surgery
sources available for taking medication histories
Patient, relative or carer → patient may be interviewed, have their own list and / or be signed up to the NHS app
Patient’s own medicines
GP records / practice → can be accessed via the SCR or calling the surgery. Sometimes the information will sent with a GP referral letter.
Community pharmacist
Nursing / residential home MAR sheet
Recent discharge letter from hospital
Out-patient clinic letter
Transfer documentation from another hospital
what are the issues with patient/carer/relative interviews
May not be able to remember everything
May lie / fear Dr’s opinion?
Drugs with abuse potential
Borrowing” a friend’s / relative’s medicines
Self-adjustment of dosages
Poor / non-adherence
Potential language barriers
Safeguarding issues
When patients struggle to remember the names of their medicines and mispronounce them, be wary about correcting them as there are some similar sounding medicines
tips for conducting a patient/carer/relative interview
Introduce yourself and explain purpose of consultation
Positive patient identification
Structured approach
Open followed by closed questions
Don’t intimidate the patient
Don’t use medical jargon
Don’t use leading questions (phrases used to prompt a specific/biased answer)
questions to ask during a patient/carer/relative interview
Do you take any regular medication prescribed by your Dr?
Does your Dr prescribe anything else for you, e.g. inhalers, eye drops, creams / ointments, patches, injections?
Ask females about oral contraceptives or hormone replacement therapy as appropriate
Ask about vaccines for relevant groups
Ask about recent medication changes and why → changed by prescriber or patient
Ask about recent short courses of medicines, e.g. antibiotics, steroids
Do you take anything prescribed for anyone else (e.g. a relative)?
Ask about medicines from internet pharmacies
Ask about OTC / herbal / complimentary medicines
Ask about recreational drugs use (substances taken for enjoyment)
Confirm allergies and previous intolerances
Ask about smoking and alcohol
give examples of interactions with some OTC medicines
Fluconazole inhibits CYP450 enzymes
Pholcodine linctus → increases risk of anaphylaxis to neuromuscular blocking agents → withdrawal of all pholcodine containing products in 2023
dangers of herbal medicines
ADRs well recognised with some e.g. hepatotoxicity with black cohosh
Potential for interactions e.g. St John’s Wort
what is adherence and why do we need to enquire about it
the extent to which a patient takes their medication or follows recommendations from a healthcare professional
Poor adherence may explain a patient’s hospital admission
Need to identify early on → may avoid unnecessary additional medicines
Some patients may only take medicines when symptomatic
Potential opportunity for patient education
things to consider when patient brings in their own medicine
Have they brought them all in?
Are they this patient’s medicines?
Check dates of dispensing
Check label and packet match
Check expiry date
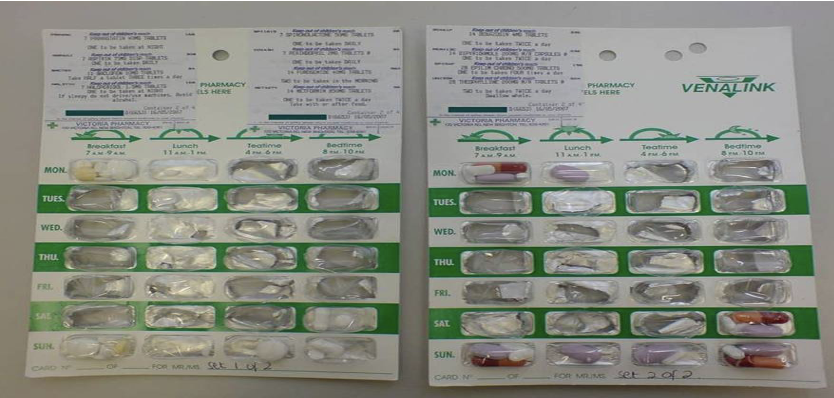
multi-compartmental compliance aids / blister pack
a device designed to contain individual doses of medicines in separate compartments or blisters.
what do you need to consider when using GP records a a source
Is it complete and up-to-date?
No record of OTC or herbal meds
What about medicines from specialists?
Access via SCR, but:
Patients can opt out (may not have their consent)
England only
Check date of last prescription issue
why are community pharmacies helpful
for confirming if prescribed medicines have been dispensed
for confirming what goes in multi-compartmental compliance aid
when methadone last picked up
Patients often use same pharmacy but do not have to register with a single community pharmacist
what are considerations when using nursing / residential home MAR sheet as a source
reflects the items prescribed and administered in a nursing/care home
Check all sheets have been sent
Check carefully for stop dates
Read directions carefully
Has it been accurately transcribed from the prescription?
how useful are discharge letters as a source
useful if patient discharged in last couple of weeks
Check with them if they’re aware of any changes between date of discharge and re-admission
Was medicines reconciliation completed during that admission?
how useful are out-patient clinic letter as a source
a summary of a patient's visit to a hospital clinic, written by a healthcare professional to their GP and often copied to the patient
May include information about medicines changes that have not been updated on GP record
Information about medicines prescribed by specialist only
May only focus on a single condition’s treatment
how useful is a transfer documentation form another hospital as a source
Transfer to specialist centre and back
Can see what the patient has been receiving before transfer
Is documentation complete?
Unfamiliarity with another system’s paperwork
Was medicines reconciliation completed during admission at transferring hospital?
how many sources are needed
Usually recommend two sources, but have to consider
Acceptable to use one for a patient with no co-morbidities?
Acceptable to use one for a patient who is knowledgeable about their medicines?
May only have one source available at the time
May need more for complex patients (e.g. those that get medicines from different clinics)
no source is 100%
considerations when patients are prescribed insulin
Dose not stated on GP record, prescription or dispensing label
Who administers it?
If patient’s unsure of dose:
Relative / carer
District nurse (if they administer)
Recent discharge letter / admission notes
considerations when patients prescribed opiate substitution
Must confirm dose with 2nd source before prescribing in hospital
Community drugs service:
Confirm drug, form, dose, frequency of pick-up, date of last pick-up, whether supervised consumption
Details of key worker
Details of any other medicines (e.g. benzodiazepines) prescribed by the service
They’ll usually contact community pharmacy to pause dispensing
Contact when patient discharged
considerations for patients with schizophrenia
May deny taking medicines (if have no insight into condition)
Clozapine is hospital only prescription but only registered community pharmacies can dispense
role of Community psychiatric nurse:
provide information on depot antipsychotics
If procyclidine listed on GP records, but no oral antipsychotics, question whether they are receiving depot antipsychotics administered elsewhere
what to include when documenting medication histories
Patient demographics
Allergies / ADRs (+ description)
Source(s) used to obtain history
Current medication patient is taking – prescribed and purchased
Name, formulation, strength
Dose, frequency, timing
+/- indication, duration
Medicines stopped / changed recently
Vaccines?
Potential or actual adherence problems
what is medicines reconciliation
process of identifying an accurate list of a person’s medicines and comparing them with the current list in use
helps to recognise any discrepancies, and document any changes, resulting in a complete list of medicines
Process followed depends on setting patient transferred to
when should you complete medicines reconciliation
Upon admission to hospital
Transfer between hospital wards (sometimes)
Transfer between hospitals
Upon discharge from hospital
When GP practice receives hospital discharge or out-patient clinic letter
how does medicines reconciliation occur on admission
take patients’ medicines list right early in their stay
Obtain accurate medication history, often need at least two sources
Compare with medicines prescribed on in-patient chart
Identify discrepancies (differences found)
Document reasons if intentional
Resolve unintentional ones
why is medicines reconciliation important
Reduces missed / wrong / delayed doses
Potentially reduces ADRs
Managing medicines in peri-operative period
Influences decisions made and information sent to GP after discharge
Medicines reconciliation should be completed within 24hrs of admission
how do errors occur when taking medicines reconciliation
Inaccurate / incomplete medication history documented
Transcription errors between documented history and in-patient prescription
Absent or incomplete documentation of reasons for changing pre-admission medicines
steps to ensure that a patient’s medications are accurately managed and documented when they are discharged from the hospital
Discharge prescription written / transcribed → forms part of discharge letter
Compare with medicines prescribed on hospital in-patient prescription (chart)
Identify discrepancies and resolve errors (some medicines will be hospital only)
Ensure appropriate course lengths and state if GP to continue
communicate discharge letter to GP surgery → Need to explain changes made to pre-admission medicines and why new medicines started
steps to ensure a patient’s medications are accurately managed and documented in primary care
GP surgery receives copy of discharge letter or out-patient clinic letter
Medicines listed on letter compared with GP record
GP record updated with new medicines to add to repeats and remove those discontinued in hospital
Ensures GP records are accurate and up-to-date before next repeat prescription is issued
Medicines reconciliation should be completed in primary care within one week of GP practice receiving discharge information