Lab Midterm (17)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
XLT
Extended length tracheostomy tubes used when regular one doesn’t fit well due to body shape or airway. Important to pick the right type and size for each pt. and be careful about correctly placing it (too deep, not deep enough, etc.).
Two types:
Proximal XLT: patients with thick necks or extra tissue around stoma. Proximal extends further at the neck of the tube.
Distal XLT: patients with long trachs, trach problems or airway swelling. Distal extends further at the end of the tube.
Percutaneous bedside tracheotomy
Establish airway via trachea and remove secretions from lungs through minimal invasive procedure at bedside, being utilized in ICUs for pts with prolonged mech. vent. or those with upper airway obstructions. Patient is supine w/ neck extension to expose trach. and sedated @ neck area. Syringe is attached to cannula needle which helps insert a guide wire into trachea. Incision is made around it and serial dilators are used to enlarge stoma enough to insert trach tube which passes over the dilator and into the trach.
Cook airway exchange catheters
Used to exchange ET tubes in difficult airways by inserting it into the ET tube to remove previous one and facilitate new one into correct position. Has soft edges but firmer than a bougie, so it has minimal damage and will not dislodge from the airway. It is disposable and single use.
Glidescope
Similar to laryngoscope but has a camera to give visuals of airway. Displace epiglottis directly or indirectly. Used for difficult airways, bariatric pts., pts w/ limited neck mobility, preference.
Comfit ET Tube Holder
Used to stabilize and hold ET tube to prevent extubation or movement of tube with its adjustable, velcro strap.
Bougie and Eschmann Stylets
Bougie is a broad term for a thin, flexible introducer while Eschmann is a type of bougie used in difficult airways when vocal cords are harder to visualize Eschmann creates a clicking feel when tip brushes against trach rings, confirming proper insertion. Indications are for difficult visualization of cords and confirming ET placement.
Retrograde intubation
Utilized to obtain definitive airway when normal intubation methods do not work (cervical spine injury, mouth tumors, bleeding etc.). Steps include identifying cricothyroid membrane and inserting a venous cannula needle in to then pass a catheter through it to advance into the upper airway. Guidewire/catheter is then retrieved through mouth/nose and a anterograde guide is advanced over that guide wire into the trachea, followed by placement of ET.
Fenestrated trach tube
Double cannulated tube w/ opening in posterior wall of outer cannula above the cuff in which the removal of the inner cannula would open the fenestration and allow air to pass into upper airway. Use this to transition pt. off ventilator by allowing them to try to start breathing on their own through a weaning process and enables speech and swallowing. Usually used with a PMV.C
Carlen’s tube
Dual ET tube with 2 distinct open passageways for each lung inside a single tube and two cuffs: one trach cuff to secure it and a bronchial cuff to plug left main bronchus. There is also a hook at end of tube to rest @ carina and keeps tube in place in left mainstream bronchus. Allows airflow to single lung and blocking off other to prevent cross-contamination to healthy lung. Laryngoscope blade guides tube into trach, placing it into left mainstream and inflating both cuffs to 20-30cmH2O to close passageways.
LMA and iGel
Standard Laryngeal Mask Airway and iGel LMA are supraglottic airway devices to maintain open airway during anesthesia or emergencies. Standard uses inflatable cuff to seal around larynx while gel uses gel-like cuff that conforms airway, with both allowing for effective ventilation, oxygenation and administration of anesthetic gases w/o intubation. Used in short-medium procedures under general anesthesia, as rescue airway during difficult intubation, or prehospital/emergency settings. Gel is useful in rapid insertion and has a gastric channel to reduce aspiration.
Passive (apneic) oxygenation during oral intubation
Method during oral intubation to continue delivering O2 to patient even when they are not breathing spontaneously to prevent critical hypoxia while we are securing airway. This is done by placing NC on pt @ 15LPM, a NR set @ 15LPM on top of that and keep it on while preparing and performing oral intubation. O2 continues to diffuse into lung even while not actively breathing. Done when quick oxygenation is critical like in ED and ICU. Downsides includes that it does not replace full oxygenation and that it requires two flowmeters.
Combitube
Used for emergent airway and/or when patient is difficult to intubate. CANNOT BE USED ON CONSCIOUS PATIENT due to gag reflex or tiny people. Has 2 external openings, 2 15mm adapters, 2 lumens, 2 cuffs (1 proximal cuff sealing oro/nasopharynx, 1 distal cuff sealing trach or esophagus to decrease regurgitation. There are vent. ports on side of the tube b/w proximal and distal cuff which allows for ventilation.
King LTS-D
Laryngeal Tube Suction - Disposable is a supraglottic airway device for airway management in emergency and controlled settings, being designed to secure a patent airway w/o need for laryngoscopy or ET intubation. It is inserted blindly into oropharynx and its cuffs seal esophagus and oropharynx once inflated. B/w the cuffs there is a ventilation opening to allow air to enter trachea, and also has a gastric access lumen to allow for suction of gastric contents to reduce aspiration risk.
Suction pressure limits
Oral suction: no limit
Adult nasal/ET: <150mmHg
Neonatal: 80-100mmHg
OPA types
Oral pharyngeal airway types includes the Berman and Williams Airway Incubator.
Berman has center support and channels along each side that allow suction catheter or ETT to slide into pharyngeal space
Williams is proximal half is cylindrical and distal half is open on its lingual surface for blind orotracheal intubations
ETT
ET tube adaptor (15mm adaptor)
Pilot balloon and spring loaded valve
Murphy eye (hole at tip of ETT to prevent tube obstruction if end of tube is obstructed by secretions)
Tube shaft with size, depth and radiopaque markings
Tracheal cuff (seals off airway to prevent aspiration and positive pressure ventilation)
Self inflating bag vs flow inflating bag
Self inflating: NR, valved, O2 flow NOT required to function. Controllable pressures, delivers 1.0FiO2 @ >15LPM and has predictable VT
Flow inflating: No valves, O2 flow dependent, variable pressures and volumes.
Tools for intubation
ETT
slip tip syringe
stylet
water soluble lube
towel roll
CO2 detector
laryngoscope (handle + blade) or glidescope
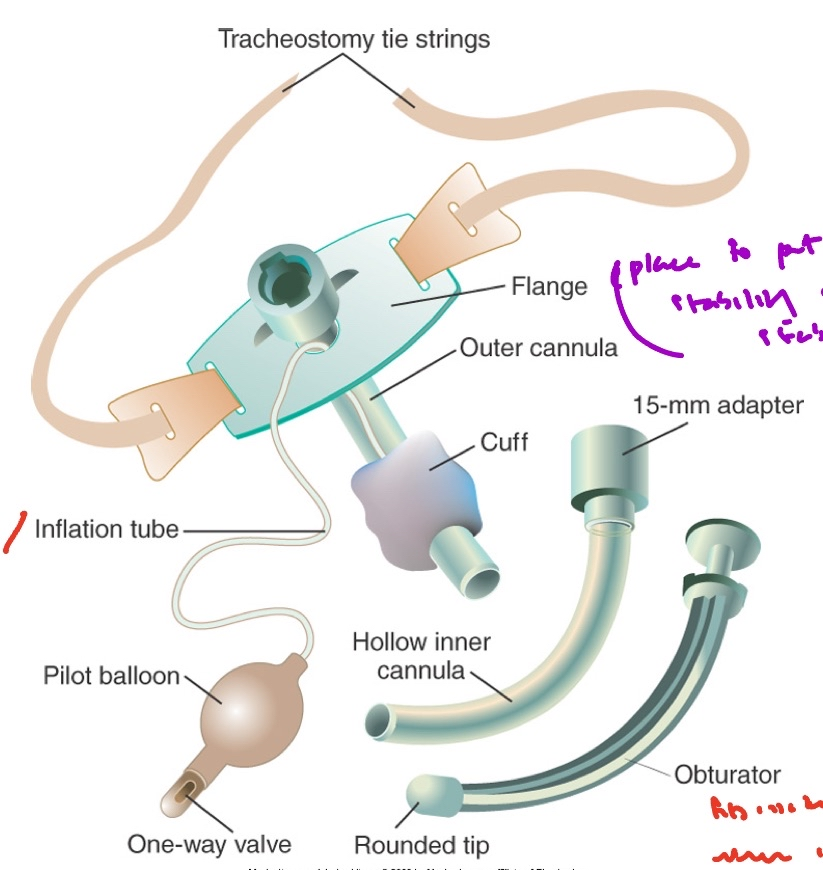
Tracheostomy tube parts
Flange is used to put string stability on to stabilize trach.
Obturator fits inside trach tube when inner cannula doesn’t fit, so it is used to only help put trach in and is immediately removed. DO NOT THROW AWAY RIGHT AWAY! Keep just in case of extubation.
Alternative cuff designs
Foam cuff designed to seal trach w/ atmospheric pressure in cuff
Tight-to-shaft cuff is low-volume, high-pressure cuff design maximizing airflow around tub when deflated, but inflated with sterile water only due to its porous silicone material
Fenestrated tube
Double-cannulated tube that has opening in postural wall of outer cannula above cuff that allows air to pass from lower to upper airway by reducing resistance to build strength back w/ using upper airway
Tracheostomy buttons
Not really a button but more like a hole (looks like an ear gauge), acting as a spacer to hold stoma open and closing it will have patient breathe through upper airway. Can pull it out to suction if need to, acting as an access point for trachea.
Can trachs be cuffless
Yes. Cuff facilitates positive pressure, so if only need to suction and reduce WoB, can have a cuff less one as it lowers resistance.