Essentials of Human Anatomy and Biology Ch 13
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
141 Terms
Pericardium
serous membrane that surrounds the heart. It is made of two layers: the outer, tough connective tissue fibrous pericardium surrounding a more delicate visceral pericardium (epicardium) that covers the heart.
visceral pericardium
(epicardium) membrane forming the outer layer of the heart
parietal pericardium
outer layer of the pericardium, At the base of the heart, the visceral pericardium folds back to become the ______ _________ that lines the fibrous pericardium
pericardial cavity
Between the parietal and visceral pericardium is a potential space ____________ filled with serous fluid that reduces friction.
epicardium
The outermost layer of heart wall, the _______, is made up of connective tissue and epithelium, and houses blood and lymph capillaries along with coronary arteries. It is the same as the visceral pericardium.
myocardium
The middle layer of heart wall called _______,consists of cardiac muscle and is the thickest layer of the heart wall.
endocardium
The inner layer of heart wall, _______ is smooth and is made up of connective tissue and epithelium, contains the Purkinje fibers (part of the conduction system).
epicardium, myocardium, endocardium
List layers of heart wall
Atria
heart chamber receives blood returning to the heart and have thin walls and ear-like auricles projecting from their exterior.
ventricles
Lower heart chambers, the thick-muscled _______ pump blood out of the heart.
septum
A ________divides the atrium and ventricle right and left chambers.Each also has an atrioventricular (AV)valve to ensure one way flow of blood from atria to ventricle.
chordae tendineae
The right AV valve (tricuspid) and left AV valve (bicuspid or mitral valve) have cusps to which _______ ________ attach.
papillary muscles
Chordae tendineae are, in turn, attached to _______ ________ in the inner heart wall that contract during ventricular contraction to prevent the backflow of blood through the AV valves.
superior and inferior vena cava
The __________ _____ ________ ________ bring blood from the body to the right atrium.
coronary sinus
The _________ ________ drains blood from the myocardium (coronary circulation) into the right atrium.
pulmonary valve
At the base of the pulmonary trunk leading to the lungs is the __________ ____________(semilunar), which prevents a return flow of blood to the right ventricle.
pulmonary veins
The left atrium receives blood from four ___________ _____ coming from the lungs.
mitral valve
Blood passes from the left atrium into the left ventricle through the _______ _______
Aorta
The left ventricle pumps blood into the entire body through the _________, guarded by the aortic valve(semilunar) that prevents backflow of blood into the left ventricle.
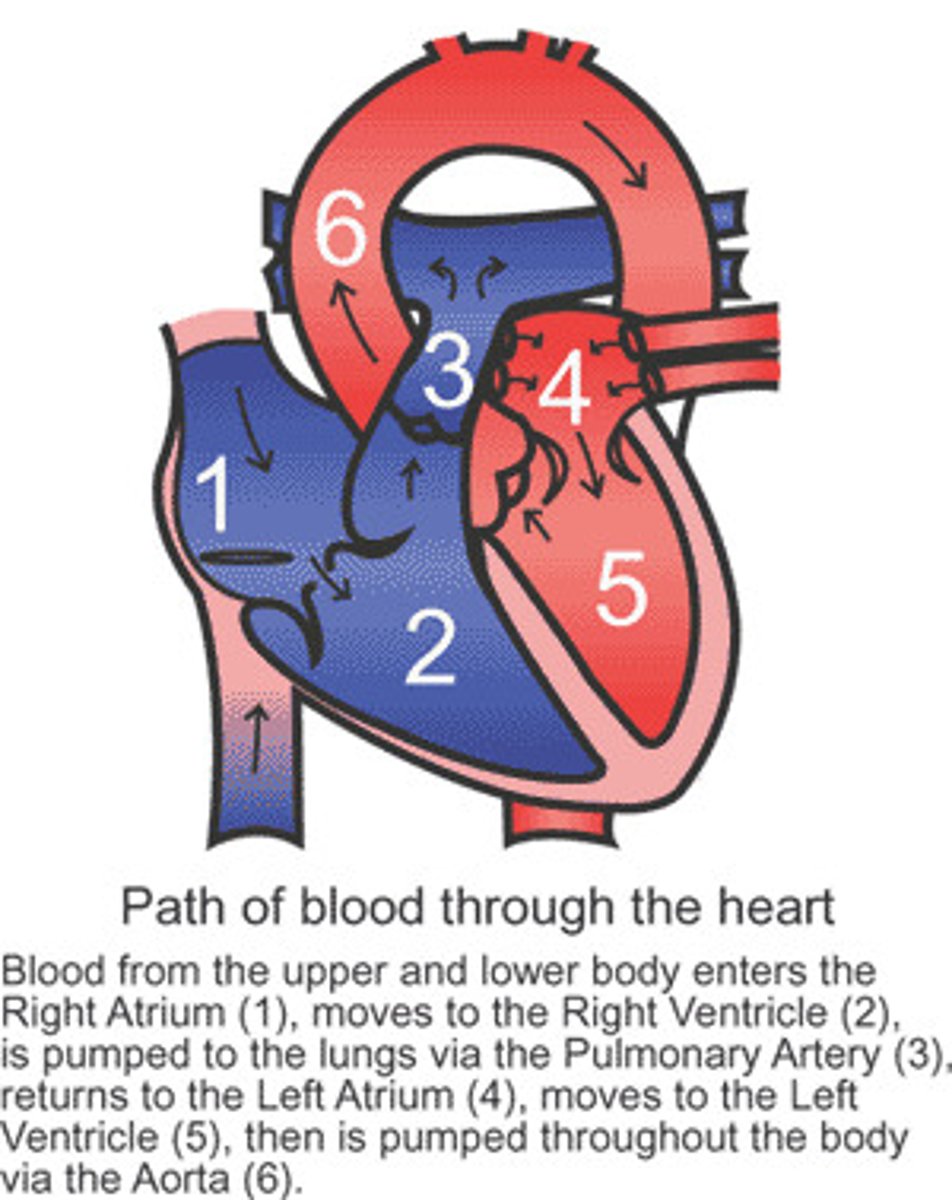
Blood Flow Through the Heart
1. Blood low in oxygen returns to the right atrium via the venae cavae and coronary sinus.
2. The right atrium contracts, forcing blood through the tricuspid valve into the right ventricle.
3. The right ventricle contracts, closing the tricuspid valve, and forcing blood through the pulmonary valve into the pulmonary trunk and arteries.
4. The pulmonary arteries carry blood to the lungs where it can rid itself of excess carbon dioxide and pick up a new supply of oxygen.
5. Freshly oxygenated blood is returned to the left atrium of the heart through the pulmonary veins.
6. The left atrium contracts, forcing blood through the left mitral (bicuspid) valve into the left ventricle.
7. The left ventricle contracts, closing the mitral valve and forcing open the aortic valve as blood enters the aorta for distribution to the body.
important to know the pathway of blood through the heart!!
Blood Supply to the Heart
1. The first branches off of the aorta, which carry freshly oxygenated blood, are the right and left coronary arteries that feed the heart muscle itself.
2. Branches of the coronary arteries feed many capillaries of the myocardium.
3. Blood flows best during the relaxation periods of the heart because contraction squeezes the blood vessels closed.
4. The heart muscle requires a continuous supply of freshly oxygenated blood, so smaller branches of arteries often have anastomoses as alternate pathways for blood, should one pathway become blocked.
5. Cardiac veins drain blood from the heart muscle and carry it to the coronary sinus, which empties into the right atrium.
coronary arteries
Branches of the _______ ________ feed many capillaries of the myocardium.
oxygenated
The heart muscle requires a continuous supply of freshly __________ blood, so smaller branches of arteries often have anastomosis as alternate pathways for blood, should one pathway become blocked.
coronary sinus
Cardiac veins drain blood from the heart muscle and carry it to the________ _______, which empties into the right atrium.
cardiac cycle
The ________ ________ consists of the atria beating in unison (atrial systole) followed by the contraction of both ventricles, (ventricular systole)then the entire heart relaxes for a brief moment (diastole).
systole
contraction phase of the heartbeat
Diastole
relaxation phase of the heartbeat
Cardiac Cycle
*KNOW WHAT HAPPENS WITH CHAMBERS DURING CYCLE
1. During the cardiac cycle, pressure within the heart chambers rises and falls with the contraction and relaxation of atria and ventricles.
2. When the atria fill, pressure in the atria is greater than that of the ventricles, which forces the AV valves open.
3. Pressure inside atria rises further as they contract, forcing the remaining blood into the ventricles.
4. When ventricles contract, pressure inside them increases sharply, causing AV valves to close and the aortic and pulmonary valves to open.
a. As the ventricles contract, papillary muscles contract, pulling on chordae tendineae and preventing the backflow of blood through the AV valves.
b. The atria are filling in preparation for the next cycle.
5. As blood is pushed out of the ventricles, the pressure drops, and then drops more as the ventricles relax.
a. When the ventricular pressure is lower than the blood pressure in the aorta and pulmonary truck, the semilunar valves close.
b. Once ventricular pressure is less than atrial pressure, the AV valves open and the process begins again.
Heart Sounds
Heart sounds can be described as a "lubb-dupp"sound.
The first sound (lubb) occurs as ventricles contract and AV valves are closing.
The second sound (dupp) occurs as ventricles relax and aortic and pulmonary valves are closing
functional syncytium
A mass of merging fibers that act as a unit is called a ___________ _________; one exists in the atria (atrial syncytium) and one in the ventricles (ventricular syncytium).
cardiac conduction system
1. Specialized cardiac muscle tissue conducts impulses throughout the myocardium and comprises the ________ _________ ______.
2. A self-exciting mass of specialized cardiac muscle called the sinoatrial node(SA node or pacemaker),located on the posterior right atrium, generates the impulses for the heartbeat.
3. Impulses spread next to the atrial syncytium, it contracts, and impulses travel to the junctional fibers leading to the atrioventricular node(AV node) located in the septum.
a. Junctional fibers are small, allowing the atria to contract before the impulse spreads rapidly over the ventricles.
b. The delay through these fibers allows both atria to contract together.
4. From the AV node, the impulse passes to branches of the AV bundle and travel down the interventricular septum.
5. Purkinje fibers branch off the bundle branches and lead into the ventricular wall and papillary muscles.
6. These fibers stimulate contraction of the papillary muscles at the same time as the ventricles contract in a twisting, upward motion.
sinoatrial node
A self-exciting mass of specialized cardiac muscle called the __________ _________(SA node or pacemaker),located on the posterior right atrium, generates the impulses for the heartbeat.
atrioventricular node
Impulses spread next to the atrial syncytium, it contracts, and impulses travel to the junctional fibers leading to the __________ ________ (AV node) located in the septum. The delay through these fibers allows both atria to contract together.
atrioventricular bundle
From the AV node, the impulse passes to branches of the _______ ________ and travel down the interventricular septum.
Purkinje fibers
branch off the bundle branches and lead into the ventricular wall and papillary muscles. These fibers stimulate contraction of the papillary muscles at the same time as the ventricles contract in a twisting, upward motion
electrocardiogram(ECG)
is a recording of the electrical changes that occur during a cardiac cycle. The first wave, the P wave, corresponds to the depolarization of the atria which leads to the contraction of the atria.The QRS complex corresponds to the depolarization of ventricles that leads to contraction of the ventricles and hides the repolarization of atria. The T waves ends the ECG pattern and corresponds to ventricular repolarization and relaxation. The intervals between the waves as well as the size of the waves give information about the heart’s ability to conduct impulses.
P wave
The first wave, the _____ _______, corresponds to the depolarization of the atria which leads to the contraction of the atria.
QRS complex
The ________ ________ corresponds to the depolarization of ventricles that leads to contraction of the ventricles and hides the repolarization of atria.
T waves
The ___ _______ ends the ECG pattern and corresponds to ventricular repolarization and relaxation.
Regulation of the Cardiac Cycle
1. The amount of blood pumped at any one time must adjust to the current needs of the body (more is needed during strenuous exercise).
2. The SA node, AV node, and the myocardium are innervated by branches of the sympathetic and parasympathetic divisions of the autonomic nervous system.
a. Sympathetic impulses increase the speed and strength of heart contractions.
b. Heart rate is decreased by parasympathetic impulses.
3. The cardiac control center of the medulla oblongata maintains a balance between the sympathetic and parasympathetic divisions of the nervous system in response to messages from baroreceptors which detect changes in blood pressure.
4. Impulses from the cerebrum or hypothalamus may also influence heart rate through emotions.
5. Increased body temperature will increase heart rate.
6. Hyperkalemia (excess K+) will decrease rate and force of contraction; hypokalemia may cause life-threatening arrhythmias.
7. Hypercalcemia (excess Ca2+) increases heart action while hypocalcemia depresses heart action.
8. Tachycardia –more that 100 beats/min
9. Bradycardia –less than 60 beats/min
Sympathetic
________ impulses increase the speed and strength of heart contractions.
parasympathetic
Heart rate is decreased by ___________ impulses.
baroreceptors
The cardiac control center of the medulla oblongata maintains a balance between the sympathetic and parasympathetic divisions of the nervous system in response to messages from ____________ which detect changes in blood pressure.
Hyperkalemia
(excess K+) will decrease rate and force of contraction; hypokalemia may cause life-threatening arrhythmias.
Hypercalcemia
(excess Ca2+) increases heart action while hypocalcemia depresses heart action.
Tachycardia
more that 100 beats/min
Bradycardia
less than 60 beats/min
Arteries and Arterioles
The arteries, which are strong, flexible, and resilient, carry blood away from the heart and bear the highest blood pressures. Because arteries are elastic, they narrow (recoil) passively when the heart is relaxing between beats and thus help maintain blood pressure. The arteries branch into smaller and smaller vessels, eventually becoming very small vessels called arterioles. Arteries and arterioles have muscular walls that can adjust their diameter to increase or decrease blood flow to a particular part of the body.
Arteries
_________ are strong, elastic vessels adapted for carrying high-pressure blood.
arterioles
Arteries become smaller as they divide and give rise to
endothelium, tunica media, tunica externa
The wall of an artery consists of an ___________ (tunica interna), _______ ______(smooth muscle), and a ______ _______(connective tissue).
tunica media
The _______ _______ ( has smooth muscle) is a thick layer
endothelium
is simple squamous epithelium; its creates a smooth surface to prevent clots; secretes biochemicals to prevent platelet aggregation; secretes substances to regulate blood flow.
tunica externa
The _______ _________ attaches the artery to surrounding tissues.
vasoconstriction, vasodilation
Arteries are capable of _______ ________as directed by the sympathetic impulses; when impulses are inhibited, _______ results; used to regulate blood flow and blood pressure.
Capillaries
____________are the smallest vessels, consisting only of a layer of endothelium through which substances are exchanged with tissue cells.
Precapillary sphincters
can regulate the amount of blood entering a capillary bed and are controlled by oxygen concentration in the area; if blood is needed elsewhere in the body, the capillary beds in less important areas are shut down.
oxygen
Blood entering capillaries contains high concentrations of __________ and nutrients that diffuse out of the capillary wall and into the tissues.
Hydrostatic pressure
________ __________drives the passage of fluids and very small molecules out of the capillary at the arteriole end by diffusion.
osmotic pressure
At the venule end, osmosis, due to the _______ _______ of the blood, causes much of the tissue fluid to return to the bloodstream.
Lymphatic vessels
collect excess tissue fluid and return it to circulation.
Blood Vessels
A. The blood vessels (arteries, arterioles, capillaries, venules, and veins) form a closed circuit that carries blood away from the heart, to the cells, and back again.
B. Arteries and Arterioles-know the pathway!
1. Arteries are strong, elastic vessels adapted for carrying high-pressure blood.
2. Arteries become smaller as they divide and give rise to arterioles.
3. The wall of an artery consists of an endothelium (tunica interna), a tunica media(smooth muscle), and a tunica externa(connective tissue).
a. The endothelium is simple squamous epithelium; its creates a smooth surface to prevent clots; secretes biochemicals to prevent platelet aggregation; secretes substances to regulate blood flow.
b. The tunica media ( has smooth muscle) is a thick layer
c. The tunica externa attaches the artery to surrounding tissues.
4.Arteries are capable of vasoconstriction as directed by the sympathetic impulses; when impulses are inhibited, vasodilation results; used to regulate blood flow and blood pressure.
5. Walls of arterioles get thinner as they approach the capillaries.
C. Capillaries ( site of gas exchange)
Capillaries are the smallest vessels, consisting only of a layer of endothelium through which substances are exchanged with tissue cells.
2. Capillary permeability varies from one tissue to the next due to the openings between cells, generally with more permeability in the liver, intestines, and certain glands, and less in muscle.
3. The pattern of capillary density also varies from one body part to the next; areas with a great deal of metabolic activity (leg muscles, for example) have higher densities of capillaries.
4. Precapillary sphincters can regulate the amount of blood entering a capillary bed and are controlled by oxygen concentration in the area; if blood is needed elsewhere in the body, the capillary beds in less important areas are shut down.
5. Exchanges in Capillaries
a. Blood entering capillaries contains high concentrations of oxygen and nutrients that diffuse out of the capillary wall and into the tissues.
b. Plasma proteins remain in the blood due to their large size.
c. Hydrostatic pressure drives the passage of fluids and very small molecules out of the capillary at the arteriole end by diffusion.
d. At the venule end, osmosis, due to the osmotic pressure of the blood, causes much of the tissue fluid to return to the bloodstream.
e. Lymphatic vessels collect excess tissue fluid and return it to circulation.
Venules
_________ leading from capillaries merge to form veins that return blood to the heart.
Veins
_______ have the same three layers as arteries have, except that the muscle layer is thinner, and have a flap-like valve inside to prevent backflow of blood. They do not carry high-pressure blood
Blood Pressure
usually refers to arterial pressure,
Arterial blood pressure rises and falls following a pattern established by the cardiac cycle.
a. During ventricular contraction, arterial pressure is at its highest (systolic pressure).
b. When ventricles are relaxing, arterial pressure is at its lowest (diastolic pressure).
c. Pressure decreases as distance from the left ventricle increases.
d. A sphygmomanometer is used to measure arterial blood pressure; 120/80 (systolic/diastolic) is considered normal.
2. The surge of blood that occurs with ventricular contraction can be felt at certain points in the body as a pulse.
Factors that Influence Arterial Blood Pressure
1.Arterial pressure depends on cardiac output, blood volume, peripheral resistance, and blood viscosity.
2.Cardiac output -directly affects blood pressure
a.Cardiac output is equal to stroke volume times heart rate.
b.Stroke volume is the amount of blood discharged from the ventricles with a contraction (about 70 mL).
c.Heart rate is the beats per minute (average is 72 beats/min).
Blood Volume
a.Blood pressure is normally directly proportional to the volume of blood within the cardiovascular system.
b._____ _____ varies with age, body size, and gender.
Peripheral Resistance
a. Friction between blood and the walls of blood vessels is a force called peripheral resistance,which hinders blood flow.
b. As peripheral resistance increases, such as during sympathetic constriction of blood vessels, blood pressure increases.
c. Dilation of blood vessels causes blood pressure to decrease.
Blood Viscosity
a.Viscosity is the ease of blood flow due to the thickness of the blood.
b. The greater the viscosity of blood, the greater its resistance to flowing, and the greater the blood pressure.
Control of Blood Pressure
Blood pressure is determined by cardiac output times peripheral resistance; BP = CO x PR
Baroreceptors Sense change in BP
a. The volume of blood that enters the right atrium is normally equal to the volume leaving the left ventricle.
b. If arterial pressure increases, the cardiac center of the medulla oblongata sends parasympathetic impulses to slow heart rate (cardioinhibitor reflex).
c. If arterial pressure drops, the medulla oblongata sends sympathetic impulses to increase heart rate to adjust blood pressure (cardioaccelerator reflex).
Other factors, such as emotional upset, exercise, and a rise in temperature can result in increased cardiac output and increased blood pressure.
6. Peripheral resistance also controls blood pressure
a. Sympathetic nerves change the diameter of arterioles in response to blood pressure changes.
b. Vasodilation will decrease PR and BP.
c. Vasoconstriction will increase PR and BP.
The vasomotor center of the medulla oblongata can adjust the sympathetic impulses to smooth muscles in arteriole walls, adjusting blood pressure.
Venous Blood Flow
1. Blood flow through the venous system is only partially the result of heart action and instead depends on skeletal muscle contraction, breathing movements, and vasoconstriction of veins (venoconstriction).
2. Contractions of skeletal muscle squeeze blood back up veins one valve section at a time.
3. Differences in thoracic and abdominal pressures due to respiration draw blood back up the veins.
4. Constriction of veins returns blood to the heart.
systolic pressure
During ventricular contraction, arterial pressure is at its highest
diastolic pressure
When ventricles are relaxing, arterial pressure is at its lowest
sphygmomanometer
A ______________ is used to measure arterial blood pressure; 120/80 (systolic/diastolic) is considered normal.
pulse
The surge of blood that occurs with ventricular contraction can be felt at certain points in the body as a _______
Arterial pressure
______ _______depends on cardiac output, blood volume, peripheral resistance, and blood viscosity.
Cardiac output
directly affects blood pressure, is equal to stroke volume times heart rate.
Stroke volume
is the amount of blood discharged from the ventricles with a contraction (about 70 mL).
Heart rate is the beats per minute (average is 72 beats/min).
Blood volume
varies with age, body size, and gender.
peripheral resistance
Friction between blood and the walls of blood vessels is a force called ________ _______,which hinders blood flow.
as it increases, such as during sympathetic constriction of blood vessels, blood pressure increases.
Vasodilation will decrease PR and BP.
Vasoconstriction will increase PR and BP.
viscosity
The greater the _________of blood, the greater its resistance to flowing, and the greater the blood pressure.
Baroreceptors
sense change in BP.
cardioinhibitory reflex
If arterial pressure increases, the cardiac center of the medulla oblongata sends parasympathetic impulses to slow heart rate
cardioaccelerator reflex
If arterial pressure drops, the medulla oblongata sends sympathetic impulses to increase heart rate to adjust blood pressure
vasomotor center
The ________ _________ of the medulla oblongata can adjust the sympathetic impulses to smooth muscles in arteriole walls, adjusting blood pressure.
venoconstriction
Blood flow through the venous system is only partially the result of heart action and instead depends on skeletal muscle contraction, breathing movements, and vasoconstriction of veins
pulmonary circuit
including vessels carrying blood to the lungs and back, is made up of vessels that convey blood from the right ventricle to the pulmonary trunk and pulmonary arteries to the lungs, alveolar capillaries, and pulmonary veins leading from the lungs to the left atrium.
systemic circuit
made up of vessels carrying blood from the heart to the rest of the body and back, including coronary circulation; includes the aorta and its branches leading to all body tissues as well as the system of veins returning blood to the right atrium.
path of circulation
The body's blood vessels can be divided into a pulmonary circuit, including vessels carrying blood to the lungs and back, and a systemic circuit made up of vessels carrying blood from the heart to the rest of the body and back, including coronary circulation.
aorta
the body's largest artery.
Arterial System
Principal Branches of the Aorta
1. The branches of the ascending aorta are the right and left coronary arteries that lead to heart muscle.
2. Principal branches of the aortic arch include the brachiocephalic, left common carotid, and left subclavian arteries.
brachiocephalic, left common carotid, left subclavian arteries
Principal branches of the aortic arch
common carotid
The right and left _______ ______ arteries diverge into the external carotid and internal carotid arteries (the internal carotids are the major blood supply to the brain).
carotid sinuses
Near the base of the internal carotid arteries are the _________ ___________that contain baroreceptors to monitor blood pressure.
descending aorta
(thoracic aorta) gives rise to many small arteries to the thoracic wall and thoracic viscera.
abdominal aorta
gives off the following branches: celiac, superior mesenteric, suprarenal,renal, gonadal, inferior mesenteric, and common iliac arteries.
subclavian artery
The ______ _______ continues into the arm where it becomes the axillary artery.
axillary artery
In the shoulder region, the ______ _____ becomes the brachial artery that, in turn, gives rise to the ulnar and radial arteries.
Arteries to the Thoracic and Abdominal Walls
1.Branches of the thoracic aorta and subclavian artery supply the thoracic wall with blood. (internal thoracic artery, anterior intercostal arteries and posterior intercostal arteries)
2. Branches of the abdominal aorta, as well as other arteries, supply the abdominal wall with blood. (internal thoracic, external iliac, phrenic and lumbar arteries).
Arteries to the Pelvis and Lower Limb
1.At the pelvic brim, the abdominal aorta divides to form the common iliac arteries that supply the pelvic organs, gluteal area, and lower limbs.
2.The common iliac arteries divide into internal and external iliac arteries.
a.Internal iliac arteries supply blood to pelvic muscles and visceral structures.
b.External iliac arteries lead into the legs, where they become femoral, popliteal, anterior tibial, and posterior tibial arteries.