Respiratory Physiology
5.0(1)
Card Sorting
1/52
Earn XP
Description and Tags
Last updated 12:26 PM on 3/1/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
1
New cards
List the three stages of respiration.
1) Ventilation→ mechanical
2) Gas Exchange→ diffusion of O2 and CO2
3) Cellular respiration→ utilization of O2
2) Gas Exchange→ diffusion of O2 and CO2
3) Cellular respiration→ utilization of O2
2
New cards
Name the respiratory zones.
1) Conducting zone
2) respiratory zone
2) respiratory zone
3
New cards
List in order the sites of the conducting zone.
mouth
pharynx
larynx
trachea
primary bronchi
pharynx
larynx
trachea
primary bronchi
4
New cards
What is the function of the conducting zone?
1)raises temp
2)moistens air
2)moistens air
5
New cards
Distinguish between terminal and respiratory bronchiole.
Respiratory bronchiole branch out from terminal bronchiole.
6
New cards
What blood vessels are found on the alveoli?
capilaries
7
New cards
How does air move?
From high pressure area to low pressure areas
8
New cards
What is breathing in called?
Inspiration.
9
New cards
Describe lung air pressure during inhalation?
Reduction of air pressure in lungs to below atmospheric pressure due to volume increase.
10
New cards
What’s Boyle’s law?
P inversely proportional to Volume.
11
New cards
Describe the pleural membranes.
1)visceral→ tightly covers the lunds
2)pariental→ lines the
2)pariental→ lines the
12
New cards
Describe the relationship between the diaphragm and the thoracic cavity.
The diaphragm muscle lines the base of the thoracic cavity.
13
New cards
What holds the visceral and pariental pleura together?
Pleural fluid
14
New cards
Is there a space between the pleura?
There’s no interpleural cavity.
ONLY PLEURAL CAVITY!
ONLY PLEURAL CAVITY!
15
New cards
Distinguish between forced and normal inspiration.
**Normal** is caused by the contraction of the __diaphragm__ and the __external intercoastal__ muscles.
\
**Forced** inspiration is caused by secondary muscles → __scalenes__ and __pectoralis minor__
\
**Forced** inspiration is caused by secondary muscles → __scalenes__ and __pectoralis minor__
16
New cards
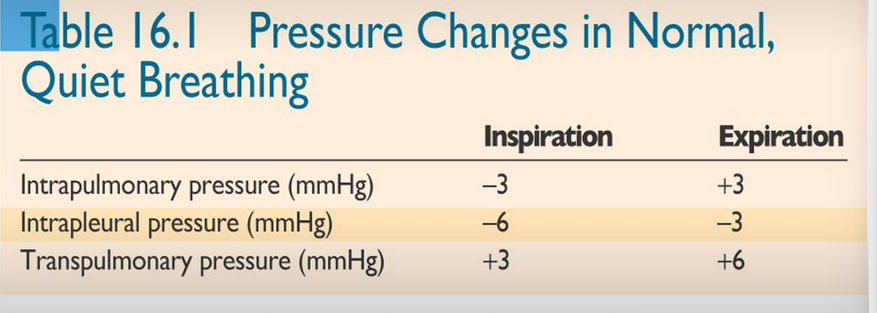
What’s the change in INTRAPULMONARY PRESSURE during normal inspiration?
\-3mmHg BELOW ATMOSPHERIC PRESSURE
17
New cards
What’s the change in INTRAPULMONARY PRESSURE during forced inspiration?
\-20mmHg
18
New cards
What contributes to normal expiration?
The elasticity of thorax and lungs that recoil after being stretched.
19
New cards
Is expiration passive or active?
Passive
20
New cards
What is the pressure increased to during normal expiration
\+3mmHg
21
New cards
What contributes to forced expiration?
Intercoastal muscles and abdominal muscles
22
New cards
What is the pressure change during forced expiration?
\+30mmHg
23
New cards
What type of mucles are respiratory muscles?
Skeletal- regulation of breathing!
24
New cards
What’s pleural pressure? Ppl
Pressure of pleural fluid
25
New cards
What’s the relationship between intrapleural and intra alveolar pressure?
intrapleural pressure is LOWER than intra-alveolar
26
New cards
In which way are pariental and visceral pluera pulled?
Visceral is pulled inward
Pariental pulled outward (part of thoracic cavity)
Pariental pulled outward (part of thoracic cavity)
27
New cards
What’s the pressure gradient between intra-pleural and intra-alveolar pressure called?
Transpulmonary pressure
28
New cards
Why is transpulmonary pressure vital?
To keep pressure in lungs higher
29
New cards
Why is pressure in the intrapleural cavity so low?
The thoracic cavity stretches it outwards
The lunds stretch it in
Increase in volume due to
The lunds stretch it in
Increase in volume due to
30
New cards
Describe the intra-pleural pressure during inspiration and expiration
\-6mmHg during inspiration
\-3mmHg during expiration
\-3mmHg during expiration
31
New cards
What happens to transpulmonary pressure when pleural membranes are damaged and air flows in?
The air unsticks the pleural membranes
32
New cards
Define pneumothorax.
Collapsed lung.
33
New cards
What happens to lung volume due to pneumothorax?
Volume decreases as the visceral pleura no longer stretches the lung outward.
34
New cards
What’s the compliance of the lung?
Ability of the lung tissue to stretch and expand.
35
New cards
Define lung compliance.
The change in lung volume resulting from a change in TRANSPULMONARY PRESSURE
\
\
36
New cards
Equation for lung compliance
Cl= delta Volume / transpulmonary tissue
\
\
37
New cards
What’s the elasticity of the lung.
Ability of the lung to return rapidly to its original size.
38
New cards
What protein is responsible for the elasticity of lungs?
Elastin.
39
New cards
What happens to intrapulmonary (same as intralveolar pressure) during expiration.
Increased.
40
New cards
What happens to lung compliance in lungs with fibrotic tissue?
Compliance is reduced.
Less air moves in during inspiration.
= restrictive pulmonary disease.
Less air moves in during inspiration.
= restrictive pulmonary disease.
41
New cards
What is degenerated in a patient with emphysema?
alveolar septa and pulmonary capillaries
→ compliance is increased
→ volume increased but doesn’t snap back
→ elasticity lost
→ expirary diifult
→ compliance is increased
→ volume increased but doesn’t snap back
→ elasticity lost
→ expirary diifult
42
New cards
What else generates resistance to lung expansion?
Surface tension
43
New cards
What creates this surface tension?
SPHERICAL alveoli secrete a thin layer of fluid
→ presence of air increases surface tesnion
→ water molecules pull in towards the alveoli
→ opposed the expansion of lungs during inspiration
→ lung compliance decreased
→ presence of air increases surface tesnion
→ water molecules pull in towards the alveoli
→ opposed the expansion of lungs during inspiration
→ lung compliance decreased
44
New cards
Do smaller or larger alveoli have a greater surface tension?
smaller
45
New cards
What’s the law of laplace?
P= 2\* T/r
→ divided by the radius
→ inward pressure
→more work needed to increase the volume of air in alveoli that are pulled inward due to surface tension
→ divided by the radius
→ inward pressure
→more work needed to increase the volume of air in alveoli that are pulled inward due to surface tension
46
New cards
What does alveoli fluid contain to reduce surface tension?
Surfacts
47
New cards
What kind of biomolecule is a surfactant
Lipoprotein
48
New cards
What does the surfactant prevent?
Collapse ofsmaller alveoli during expiration
49
New cards
Do alveoli completely empty themselves?
No, there’s always residual volume
50
New cards
What type of alveoli produce surfactant?
Type II alveolar cells
51
New cards
When do type II alveolar cells develop?
Late foetal development
\-25th week
\-25th week
52
New cards
What do premature infants (before 34th week) suffer from due to low type II development?
Acute respiratory distress syndrome
53
New cards
Acute respiratory distress syndrome- what does that do to the lungs?
Decreases lung compliance
Collapses Alveoli
Collapses Alveoli