34. Diseases of the shoulder joint. Aetiology, diagnosis and therapy.
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What type of joint is the shoulder?
Ball-and-socket synovial joint
Which bones make up the shoulder joint?
Scapula (glenoid cavity) and humerus (caput humeri)
Which muscles are associated with the shoulder joint?
Supraspinatus: Helps extend the shoulder.
Infraspinatus: Responsible for rotating the shoulder outward.
Subscapularis: Rotates shoulder inward.
Deltoid: Abducts shoulder (moves it away from body).
Biceps Brachii: Flexes elbow & assists in shoulder stabilisation.
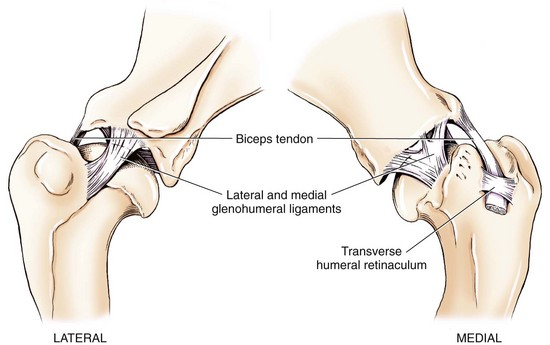
Which tendons and ligaments are associated with the shoulder joint?
Biceps Tendon: Runs through bicipital groove of humerus, helping stabilise shoulder.
Glenohumeral Ligaments: (lateral and medial) Provide stability to shoulder joint by connecting humeral head to scapula.
Transverse humeral ligament: stabilises biceps brachii tendon w/i bicipital groove of humerus ⤍ prevents tendon from slipping out during shoulder movement.
No collateral ligaments: tendons & muscles supports joint. Tendon of subscapularis muscle act as medial collateral ligament, & tendon of infraspinatus muscle act as lateral collateral ligament
What are examples of diseases of the shoulder joint?
Osteochondrosis dissecans (OCD)
Shoulder luxation
Shoulder instability/subluxation
Biceps brachii tendinopathy
Rupture of the tendon of origin of biceps brachii muscle
Incomplete ossification of the caudal glenoid (ICOCG)
What is osteochondritis dissecans (OCD)?
A disturbance of cell differentiation in metaphyseal growth plates and joint cartilage causing abnormal endochondral ossification of epiphyseal cartilage
What happens if OC results in a dissecting flap of cartilage?
It is termed osteochondritis dissecans (disseco = to separate)
Which joints are commonly affected by OCD?
Shoulder, stifle, hock, elbow, vertebral articular facets
Is the lesion in OCD usually unilateral or bilateral?
Bilateral
Which breeds are most commonly affected by OCD?
Large and giant breeds (rottweiler, labrador)
Which gender is more prone to OCD?
Males
What are some proposed aetiologies of OCD?
Trauma
Overfeeding during growing phase: high caloric diet, high protein
Hormonal: testosterone & GH stimulates epiphyseal growth
Increased Ca in diet: especially from commercial diets
What is the pathogenesis of OCD?
Thickening of articular cartilage → necrosis → horizontal fissure → vertical fissure → inflammation → degeneration, osteophytes, arthrosis, DJD, valgus/varus
Where are OCD lesions often located?
Caudal humeral head
Distal humeral/femoral epicondyle
Epiphysis of radius and ulna
What are the clinical signs of shoulder OCD?
Lameness (starting at 4-6 months), reluctance to move, stiffness, joint effusion, crepitus, swelling
How is shoulder OCD diagnosed?
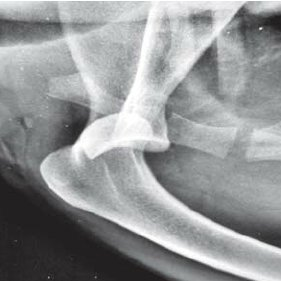
X-ray (flattening of subchondral bone, DJD), arthroscopy
Why is it important to X-ray both sides if an OCD lesion is found?
The lesion is usually bilateral
What are the treatment options for shoulder OCD?
Conservative (NSAIDs, rest, diet change, stem cell treatment)
Surgical (arthrotomy/arthroscopy, flap removal)
What are the types of shoulder luxation?
Medial
Lateral
Cranial/caudal
What is the aetiology of medial shoulder luxation?
Trauma, congenital in some small breeds
How is medial shoulder luxation diagnosed?
X-ray
What are the treatment options for medial shoulder luxation?
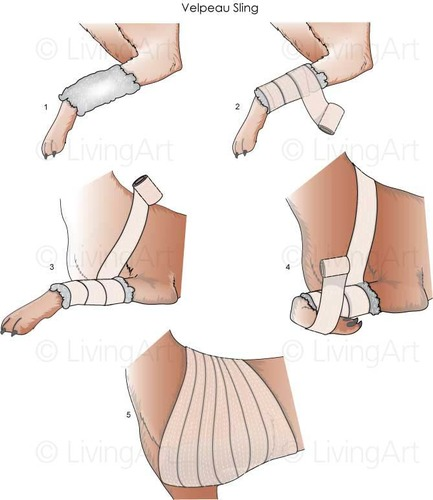
Conservative (Closed reduction & stabilisation under sedation or anaesthesia using velpeau sling, in distracts humeral head laterally)
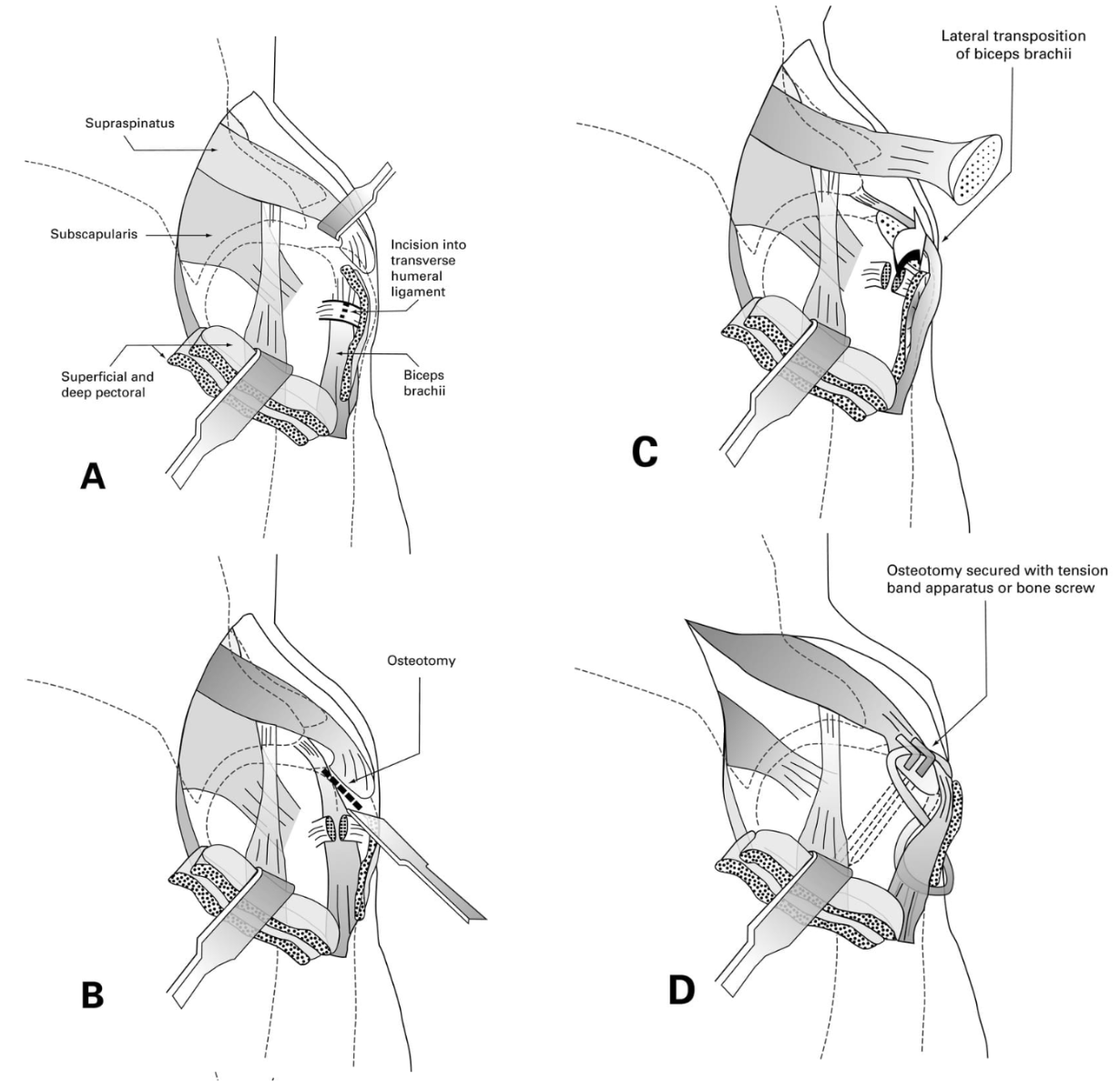
Surgical: Reconstruction of the glenohumeral ligaments and joint capsule. Transposition of either the biceps brachii tendon or supraspinatus tendon. Intraarticular pinning
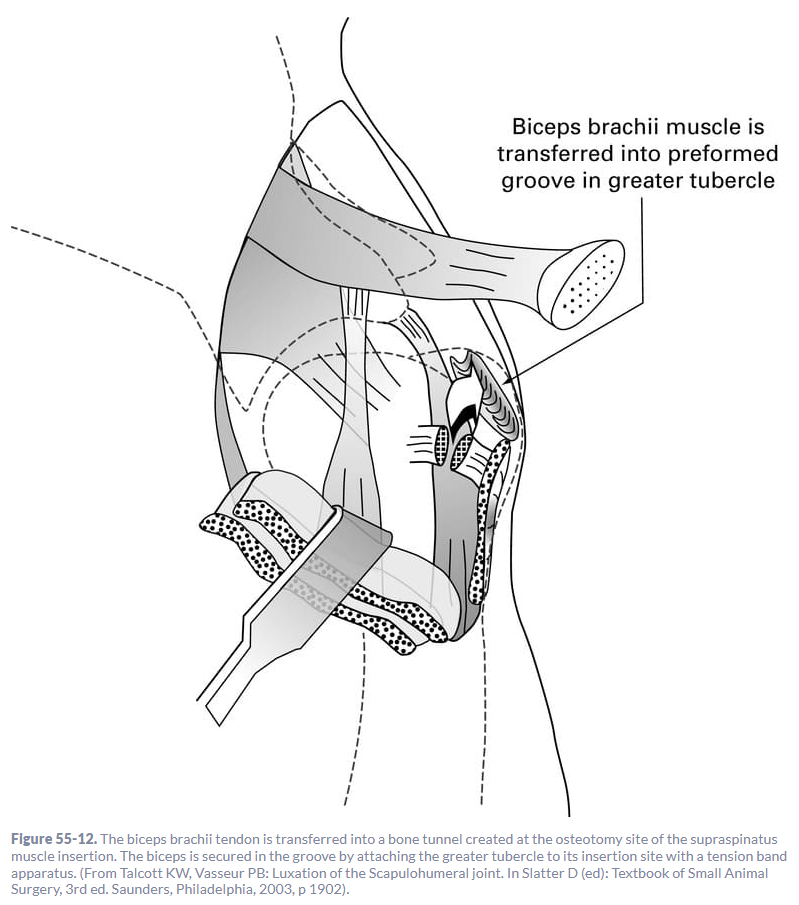
How is transpositioning of the biceps brachii tendon carried out?
Open joint capsule → osteotomy of greater tubercle of humerus (make deep groove) and move tendon medially to it → secure with lag screw/k-pins through tendon into the humerus
What are the clinical signs of lateral shoulder luxation?
Extreme adduction, flexed limb with medial rotation, greater tubercle is prominent & laterally displaced, pain & crepitus of shoulder.

What are the treatment options for lateral shoulder luxation?
Conservative: Closed reduction under general anaesthesia. Assess range of motion & stability, use splint for 2 weeks.
Surgical: lateral transposition & tenodesis of biceps tend, trans-articular pinning, glenoid excisional arthroplasty, arthrodesis chronic
What is the aetiology of cranial/caudal luxation?
Rare, trauma
How is cranial/caudal luxation diagnosed?
Physical exam to rule out brachial plexus neuropathy, X-ray to determine cause of luxation
How is a craniolateral osteotomy carried out?
A deep groove is made in greater tubercle for biceps tendon → cut tendon → move tendon → tubercle replaced over tendon secured w/ screw or pin/tension band
Which dogs are most commonly affected by shoulder instability?
Small dogs with congenital laxity (3-10 months), medium/large active dogs with trauma/overuse
What pathology can occur from shoulder instability?
Abnormal movement of the humeral head in the joint → tearing/stretching of supporting structures
Which is the most common form of shoulder instability?
Medial
How is shoulder instability diagnosed?
Palpation & manipulation under sedation: Increased angles of abduction (should be less than 30), often w/ pain present. Positive shoulder-drawer test
X-Ray. Measuring the abduction angle.
Arthroscopy for definitive diagnosis: Show tearing & laxity of tendons
What are the treatment options for shoulder instability?
Conservative: Stabilisation of shoulder joint → treatment of choice. Forelimb hobbles, anti-inflammatory drugs (intraarticular steroids), exercise modification, physiotherapy
Surgical: Ligament reconstruction, joint capsular imbrication (overlapping), joint capsular shrinkage, simple debridement of damaged tissues, prosthetic stabilisation, shoulder fusion, or total shoulder replacement
What is biceps brachii tendinopathy?
Tearing, trauma, and inflammation of the biceps tendon and sheath, usually accompanied by bicipital tenosynovitis (biceps brachii tendon + synovial sheath).
Chronically, synovial hyperplasia with dystrophic mineralization may occur.
What are the clinical signs of biceps tendinopathy?
Variable lameness, intermittent/progressive, often worse after exercise
Tearing of tendon: acute lameness
Chronic inflammation: progressive lameness
How is biceps tendinopathy diagnosed?
Direct palpation of origin of biceps brachii muscle (BBM). BBM retraction test.
Radiography (see irregularity of intertubercular groove. Mineralisation of tendon), USG, MRI, Arthroscopy.

What are the treatment options for biceps tendinopathy?
Medical: long acting corticosteroids into scapulohumeral joint, weight loss, strict cage rest w/ gradual exercise gradually after 6 weeks post injection. Omega 3 FA → inflammatory affect (good supplement)
Surgery: Recommended for cases linked to mechanical problem or when the dog does not respond to medical treatment.
Arthroscopy/arthrotomy
Bicipital Tenotomy: Tendon is released from its origin near supraglenoid tubercle (works in dogs because they do not lift loads)
Bicipital Tenodesis: Moving the origin of tendon and stabilising it to the humerus.
What is the aetiology of biceps tendon rupture?
Direct laceration of the tendon
Avulsion from supraglenoid tubercle
As an intrasubstance tear of the tendon
Rupture of the tendon is connected with traumatic shoulder joint luxation. Large dog breeds are inclined.
What are the clinical signs of biceps tendon rupture?
Lameness, pain, muscle atrophy, limited range of movement, abnormal gait
How is biceps tendon rupture diagnosed?
Direct palpation of the origin BBM
M.biceps brachii retraction test
Radiography (show irregularity of the supraglenoid tubercle, calcification. General arthritis signs. Caudal glenoid rim is arthritic w/ osteophytes). Contrast arthrography.
USG, MRI.
Arthroscopy
What is incomplete ossification of the caudal glenoid (ICOCG)?
Incomplete fusion of the accessory caudal glenoid ossification centre, also known as Ununited Caudal Glenoid (UCG)
What are the clinical signs of ICOCG?
Usually asymptomatic, pain if the caudal fragment is mobile, mild/moderate shoulder pain, regional muscle atrophy
How is ICOCG diagnosed?
X-Ray: easily demonstrated by a mediolateral radiograph (small caudal glenoidal fragment)
Arthroscopy.

Arthrotomy, fragment removal