hemodialysis & peritoneal dialysis
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
dialysis - epidemiology
Incidence and prevalence of dialysis has increased over the years
Incidence: No. of new ESKD pts on dialysis in a year. Measure of development of kidney disease in the population
Prevalence: Total no. of pts on dialysis. Describes the burden of kidney disease in the population
dialysis - initiation
Elective vs emergent
Start planning early
GFR < 20-30 ml/min/1.73m 2
Patient/family education
Options: HD, PD, home HD(?). Access for HD or PD
K/DOQI guidelines
Non-diabetics: GFR < 15 ml/min/1.73m 2
Diabetics: GFR < 20 ml/min/1.73m2
Most pts start when GFR < 10 ml/min/1.73m 2 or when signs/symptoms of kidney failure are present
indications for chronic dialysis
Azotemia (lab anomalies) vs uremia (azotemia + symptoms)
Symptoms: Fatigue, weakness, SOB, mental confusion, N/V, bleeding, loss of appetite, itching, cold intolerance, weight gain, neuropathy, uremic breath
Signs: Edema, changes in urine output, abdominal distension, pericardial rub, asterixis, critical lab values (Urea, SCr, K)
indications for acute/emergent dialysis
Acid-base imbalance (acidosis)
Electrolyte abnormalities
Intoxication (drug overdose)
Overload (fluid)
Uremia
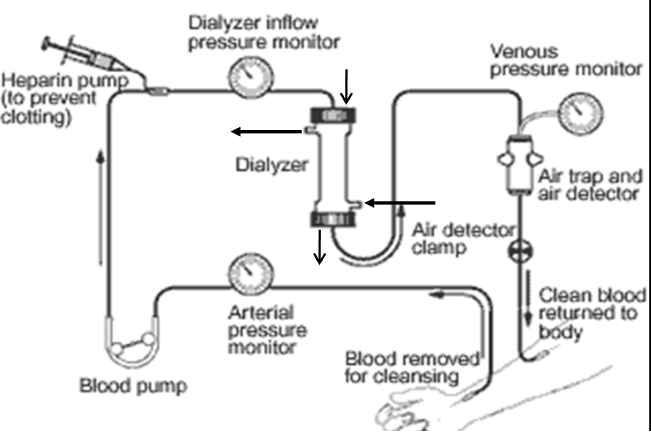
hemodialysis - principles
Perfusion of blood and dialysate on opposite sides of a semipermeable membrane
N2 waste products and uremic toxins move from blood to dialysate for removal

hemodialysis - movement mechanisms
Diffusion: Movement of substances along a conc gradient
Factors affecting diffusion rate
Solute conc -> blood vs dialysate
Solute characteristics: size, MW, protein binding (lesser better), solubility
Dialyzer composition -> membrane type
Blood and dialysate flow rate
Ultrafiltration: Movement of water across membrane due to hydrostatic/osmotic pressure
Primary means for removal of excess body water (depends on pt water content)
Convection: Dragging of solutes across membrane with fluid transport
Depends on hydrostatic pressure and pore size of dialyzer
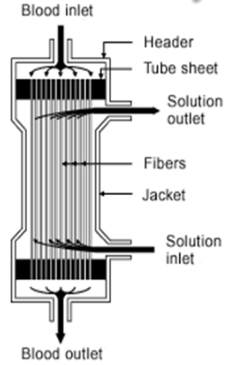
hemodialysis - dialyzer
Large canister with thousands of small fibers (semi-permeable membrane) that pts blood is passed through
Dialysate pumped around these fibers allowing wastes/toxins to pass into it for removal (countercurrent to blood flow)
3 types
Conventional: Small pores (urea, Cr)
High-efficiency: Larger surface areas (water, urea)
High flux: Large pores (high MW substances, drugs
hemodialysis - dialysate
Consists of purified water and electrolytes (isotonic)
Constituents conc set to approx normal values
Can be adjusted to meet specific pt needs
Pumped through dialyzer countercurrent to blood flow
Removes fluid, waste products, uremic toxins
hemodialysis - extrarenal vascular circuit
Typical schedule 3x/week (MWF/TTS)
4hr/treatment, depends on fluid status
hemodialysis - access
Allows permanent access to bloodstream for HD
Early referral to nephrology and vascular access
Preparation takes weeks to months before initiating dialysis
3 kinds of vascular access
Arteriovenous (AV) fistula, AV graft, venous catheter
hemodialysis - AV fistula
Preferred type
Advantages
Longest survival (years)
Lowest complication rate
Disadvantages
Requires >= 2 months to mature
May be difficult in certain pt (elderly, DM, PVD)
hemodialysis - AV graft
Use of synthetic graft (polytetrafluoroethylene)
Advantages
Requires 2-3 weeks
Disadvantages
Shorter survival
Higher rates of complications
hemodialysis - venous catheter
Temporary access -> should not be left inside for long
For AKI (short term HD), Planned for kidney transplant
When AV access not an option: Children, DM, severe PVD, obese, Failed multiple AVF, AVG attempts
Advantages: For emergent dialysis
Disadvantages
Short lifespan (weeks-months), Prone to complications
Low blood flow rates - compromise dialysis adequacy
Proper cleaning and care required -> cannot touch water
hemodialysis - goals
Desired dry weight (normotensive and free of edema/SOB)
Adequate removal of endogenous waste products
hemodialysis - urea reduction ratio (URR)
Goal URR > 65%
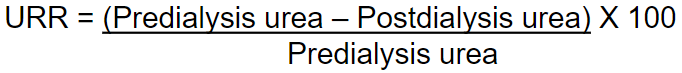
hemodialysis - Kt/V
Fraction of patient’s total body water that is cleared of urea during dialysis (fractional urea clearance)
where K = dialyzer clearance, t = time, V = distribution vol of urea
Usually calculated by dialysis machine
K/DOQI recommends goal Kt/V ~ 1.4 (min 1.2)
hemodialysis - complications
hypotension 20-30%)
cramps (5-20%)
N/V (5-15%): Causes: hypotension, dialyzer reaction
Headache (5%): Causes: disequilibrium syndrome, caffeine withdrawal (HD removal)
Chest/back pain (2-5%): Causes unknown, maybe dialyzer reactions
Fever/chills (<1%): Causes: endotoxin release, infection
Pruritus (5%): Causes: Inadequate dialysis (buildup of toxins on skin), Dry skin, Secondary hyperparathyroidism (high P + PTH), Electrolyte abnormalities, Histamine release, Mast cell production
HD complications - hypotension
Causes: Hypovolemia, Excessive ultrafiltration, Antihypertensive medications, Target dry weight too low, Diastolic dysfunction, Autonomic dysfunction, Low Ca, Na in dialysate, High dialysate temperature (low temp better, causes constricted vessels), Meal ingestion
Management
Place patient in Trendelenburg position, Reduce rate or turn off ultrafiltration
Administer fluids (NS): 100-200 ml bolus of IV NS
Increase dialysate Na conc, Switch to bicarbonate-buffered dialysate
Accurately set dry weight, Lower dialysate temp
Midodrine, α1 -adrenergic agonist 2.5-10 mg PO 30 min before HD (C/I in CVD)
Correct anemia, Administer O2, Avoid food before/during HD
HD complications - cramps
Causes: Muscle hypoperfusion, Hypotension, Electrolyte/acid-base imbalance
Management
Correct or prevent volume contraction and excessive ultrafiltration
Quinine (now not FDA approved)
Vitamin E 400 IU at bedtime
Other agents tried -> not much help
Skeletal muscle relaxants, Benzodiazepines, Pramipexole (restless leg syndrome)
hemodialysis - catheter related thrombosis
Catheter > grafts > fistulas
Intrinsic (within lumen) vs extrinsic (outside)
Suspected when blood cannot be aspirated from catheter yet saline flows in freely
Major cause of catheter failure
HD catheter related thrombosis - management
Non-pharmacological: Forced saline flush, Mechanical thrombectomy, Catheter stripping/removal, Exchange of catheter over guidewire
Pharmacological (intraluminal thrombolytics -> sits in catheter)
Alteplase (r-tPA): FDA approved for restoration of central venous catheter due to thrombosis
Instill 2 mg/2 ml per catheter port, attempt to aspirate after 30 min. May repeat if function not restored. Longer instillation duration may be required
Urokinase: Instill 1 ml (2000 units/ml); Aspirate after 5 min; aspiration attempts may be repeated every 5 min. Second injection may be necessary
Reteplase
hemodialysis - catheter related infections
Fever, chills, rigors, elevated white count
Obtain peripheral blood cultures and culture from catheter site before starting Abx
Those at risk for bacteremia (blood stream infection): DM, immunosuppressed, (+) history of cath-infections, S. aureus nasal carriage
Complications: Endocarditis, bacteremia, sepsis
HD catheter related infections - AV fistula and graft
AV fistula: Infections are race
Treat as subacute bacterial endocarditis x 6 weeks. May need to remove fistula if septic emboli
Synthetic AV grafts
Treat for 2-4 weeks
Resection of infected portion of graft may be required
HD catheter related infections - types
Exit site infections: May be with or without drainage
Topical antibiotics (mupirocin ointment) or IV (gram positive)
Proper local exit site care. No catheter removal unless infection fails to respond to therapy
Catheter-related bacteremia (with/without systemic signs/symptoms)
Gram-positive antibiotic (skin bacteria) coverage (cefazolin/vancomycin). Streamline therapy based on culture results
Remove catheter if symptomatic > 36 hr or clinically unstable
If stable and asymptomatic, provide culture-specific antibiotic coverage for a minimum of 3 weeks
Do not place new permanent access until blood cultures, performed after stopping antibiotics, have been negative for at least 48 hours
HD catheter related infections - management
Start empiric therapy: Cover gram-positive (staph aureus) and gram-negative microorganisms
MSSA - sensitive
Cefazolin 20 mg/kg (to nearest 500 mg) IV with each dialysis (usual: 1g daily or 2 g 3x/week after HD)
MRSA - resistant
Vancomycin 20 mg/kg IV loading dose, then 500 mg with each dialysis (usual: 1 g then 500 mg, 750 mg or 1 g based on levels)
Gram-negative coverage
Gentamicin 1-2 mg/kg IV after each dialysis
Ceftazidime 1 g IV after each dialysis (usual: 1 g daily or 2 g 3x/week after HD)
Streamline therapy based on culture results
HD catheter related infections - antibiotic lock therapy
Used in treatment of uncomplicated tunneled catheter infections usually in combination with systemic Abx
Involves instilling each catheter lumen with antibiotic solution at the end of dialysis and allowing it to dwell for a period of time (usually ≤ 48 h)
Withdraw solution before next HD. Repeated after every HD session. Goal is to salvage the catheter
Mean success rate ~ 67%
Common used antibiotics: cefazolin, vancomycin, gentamicin
Usually mixed with heparin or normal saline in sufficient vol to fill catheter lumen (2-5ml)
Usually not used alone but in combination with systemic abx for 7-14 days
HTN management in dialysis pt
Predialysis < 140/90 mmHg
Postdialyisis < 130/80 mmHg
Appropriate measurement -> cuff size, supine vs sitting vs standing
Adjustment of dry weight
Consider giving anti-HTN drugs at night to reduce nocturnal surge of BP and minimize intradialytic hypotension
In some patients, hold AM dose of anti-HTN drugs
Consider dialyzability of drugs in patients with difficult-to-control HTN
HTN management - fluid accumulation
Management of excess fluid accumulation b/w dialysis sessions
Counseling by dieticians, Fluid restriction (~800 ml), Na restriction
Increase ultrafiltration, Longer dialysis
Increase frequency of dialysis
Drugs that reduce appetite
HTN management - ACEi/ARB
ACEi/ARB may be restarted (DHP-CCB often used also)
Cause greater regression of LVH
Reduce sympathetic nerve activity
Reduce pulse wave velocity
May improve endothelial function
May reduce oxidative stress
peritoneal dialysis - principles
Peritoneum serves as an inert semi-permeable membrane which allows movement of solutes and fluid between dialysate and peritoneal capillaries
Dialysate instilled into peritoneal cavity through trans-abdominal catheter and allowed to dwell
Diffusion and ultrafiltration take place during the exchanges to remove metabolic wastes
Dialysate is subsequent drained. Cycle is repeated
Types of PD: CAPD (multiple times/day) vs. APD (overnight)
peritoneal dialysis - precautions
PD dose may be altered to increase osmotic gradient across the peritoneum and in turn increases UF and diffusion
Increase no. of exchanges per day, volume of each exchange, dextrose concentration in dialysate
Increase dwell time -> may not be effective
Equilibrium may be reached, No further water or solute removal, Reverse water movement may occur
Adequacy: Kt/V = 1.7/week (KDOQI) -> higher kidney clearance
peritoneal dialysis - considerations
Importance of preserving residual kidney function
Associated with decreased mortality. Continue use of ACEi, ARB, avoid nephrotoxins
PD is much less efficient compared to HD:
Blood is not in direct contact with peritoneal membrane, metabolic waste products must travel some distances to the dialysate-filled peritoneal cavity. No method of regulating blood flow to surface of peritoneal membrane. No countercurrent blood flow and dialysate
Continuous procedure needed to achieve acceptable clearance of metabolic wastes
May be suitable for pts:
Hemodynamically unstable, With sig residual kidney function
Ambulant and who desire self-care
Supported by fam, with good personal hygiene
peritoneal dialysis - dialysate solutions
Varying concentrations of electrolytes (Na, Cl, Ca, Mg, lactate)
Dextrose solutions (1.5, 2.5, 3.86, 4.25% dextrose or 7.5% icodextrin, a glucose polymer)
Dextrose: Hyperosmolar dextrose solutions induce ultrafiltration by crystalline osmosis.
Disadvantage: Incompatibility with peritoneal mesothelial cells or with peritoneal leukocytes
Icodextrin -> good for DM
Iso-osmolar. Produces prolonged ultrafiltration by “colloid osmosis”, Similar osmosis as 4.25% dextrose. Fewer metabolic effects such as hyperglycemia and weight gain
peritoneal dialysis - complications
Mechanical: kinking of catheter, inflow/outflow obstruction e.g. constipation
Infections: Peritonitis, catheter-related infections. Leading cause of morbidity, mortality, technique failure
Medical
glucose load
fibrin formation
PD complications - medical
Fluid overload (increase UF, diuretics if residual kidney function)
Electrolyte abnormalities ( or Ca, K ) esp if multiple times/day
Malnutrition (AA loss, muscle wasting, decreased appetite)
Glucose load
Fibrin formation in dialysate
PD complications - glucose load
Continuous supply of calories from dialysate containing dextrose
Exacerbation of DM; closer monitoring and adjustment of DM therapy may be required
IP administration of insulin (bioavailability 25-30%) -> not really in SG
Increase insulin requirements in PD patients due to:
Continued absorption of dextrose from peritoneal cavity
Adsorption of insulin to PVC bag and administration set
PD complications - fibrin formation
Fibrinogen secreted into peritoneal cavity results in fibrin formation (cloudy effluent)
Causes Intraperitoneal adhesions, outflow obstruction
Administer IP heparin 500 units/L (minimally absorbed due to high MW; limited systemic SE) to prevent catheter occlusion
peritoneal dialysis - peritonitis
Definition: Elevated dialysate WBC > 100/mm3 + > 50% PMN neutrophils
Clinical presentation: Abdominal pain, cloudy effluent, fever, nausea, vomiting, chills. Positive gram stain and culture of dialysate effluent
Sterile culture or culture-negative peritonitis may occur
40-60% of patients develop first episode within a year (incidence lower in APD)
Majority caused by gram(+) bacteria. No predominant gram(-) organism
Use of broad spectrum Abx for initial empiric therapy (near GIT which has gram (-) bacteria)
Modify therapy according to culture and sensitivities
peritonitis - prevention
Systemic prophylactic antibiotics should be administered immediately before catheter placement
Prophylactic therapy should include use of perioperative IV broad spectrum agents Gram(+): Cefazolin, vancomycin; Gram(-): AG (gentamicin)
Actual choice of prophylactic antibiotics should take into consideration institution’s local spectrum of abx resistance
Abx prophylaxis (broad spectrum coverage) also suggested prior to colonoscopy and invasive gynae procedures (mostly IV route)
Avoid/treat hypokalemia to reduce peritonitis risk. Avoid/limit use of H2RA to prevent enteric peritonitis
Avoid/treat GI problems e.g. constipation/enteritis (regular use of laxative to prevent constipation common in PD pts)
Use of anti-fungal prophylaxis during antibiotic therapy to prevent fungal peritonitis e.g. oral nystatin 500,000 units QID or fluconazole 200 mg q48h
peritonitis - treatment
Intra peritoneal (IP) administration of Abx preferred
Treatment duration: 14 to 21 days. Start as soon as possible
Intermittent (1 large dose into 1 exchange/day, min 6 h dwell) vs. continuous therapy (with each exchange)
Abx generally stable in dextrose and icodextrin (refer to stability table)
Systemic toxicities of IP regimens likely similar to IV and oral
If WBC remains high or no clinical improvement by 5 days on appropriate abx, remove PD catheter, initiate HD and continue IV abx for 2 more weeks
peritonitis - empiric therapy
Initial empiric therapy should include use of broad spectrum agents; adjust therapy based on culture/sensitivities
Gram(+): Cefazolin, vancomycin
Gram(-): AG, ceftazidime, cefepime - gram (-) + (+) (monoTx possible)
Increase dose empirically by 25% in pts with significant residual kidney function (urine output >100 mL/day) and drug is renally eliminated
peritonitis - antibiotics
IP AG: Daily intermittent dosing recommended
Prolonged courses to be avoided due to risk of ototoxicity
Adjunctive oral N-acetylcysteine therapy may help prevent AG ototoxicity
Vancomycin, cephalosporins and AG can be mixed in same bag
Do not add AG and penicillin (PCN) to same bag due to chemical incompatibility -> PCN inactivates AG
peritoneal dialysis - fungal peritonitis
Less common but associated with poor prognosis and high morbidity, mortality
Remove catheter immediately
Treatment: azoles (fluconazole), echinocandins (caspofungin), amphotericin B
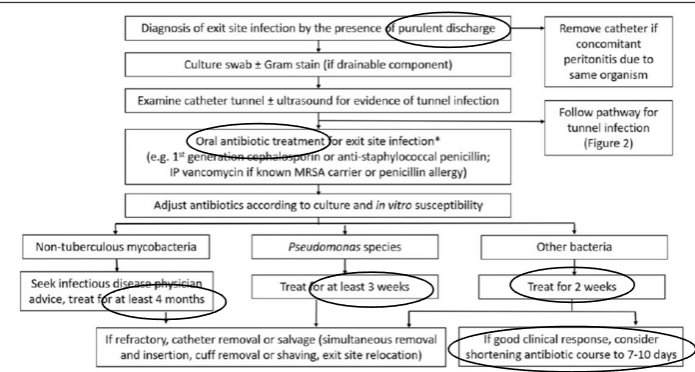
peritoneal dialysis - catheter related infections
2 types: exit and tunnel infection
Frequency of exit-site infection ~ every 24 to 48 months
Majority caused by staph aureus (S. epidermidis < common)
Pseudomonas less common but can result in significant morbidity
Increase risk in pts who are nasal carriers of S. aureus, diabetics, those receiving immunosuppressants
PD Catheter-related infections - clinical presentation
Purulent discharge (if present, consider definitive exit site infection)
Erythema at exit site (may or may not be present)
Fever, chills
PD Catheter-related infections - prevention
Administer prophylactic antibiotics before catheter insertion e.g. nasal antibiotics for nasal S. aureus carriers
Leave exit site dressing intact for 7 days after catheter insertion
Training and education of patients and caregiver on care of exit site
PD Catheter-related infections - management
Oral antibiotic treatment for exit site infection
HD - advantages
Higher solute clearance allows intermittent treatment
Dialysis adequacy parameters better defined
Low technique failure rate
Allows closer monitoring of pt
Allows IV administration of some drugs
HD - disadvantages
Requires multiple visits to center
Disequilibrium, hypotension, cramps are common; may take months to adjust
Infections and thrombosis from vascular access
Rapid decline of residual kidney function
PD - advantages
More hemodynamically stable
Suitable for elderly & young pts
Increased clearance of larger solutes
Preserve residual kidney function
IP drug administration
Less blood loss and Fe deficiency
No systemic heparinization
SC dosing of ESA possible
PD - disadvantages
Greater protein and AA losses, glucose load, peritonitis
Risk of obesity with glucose absorption
Mechanical problems, catheter malfunction, exit-site infections
Inadequate UF and solute removal in certain pts
Pt burnout and high technique failure rate
Extensive abdominal surgery may preclude PD
No convenient access for IV medications