Exam 1
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Characteristics/principles of a therapeutic relationship
Therapeutic rather than Social
Client Focused
Goal Directed
Objective not subjective
Time-Limited
Phases of the therapeutic relationship
Preorientation Phase
Orientation Phase
Working Phase
Termination Phase
preorientation phase
Takes place prior to meeting with the client
1st gather data about the client, his or her condition, and the present situation
Nurse then examines his or her thoughts, feelings, perceptions, and attitudes about this particular client
orientation phase
The nurse-client become acquainted; build trust and rapport
A contract is established
Includes time and place for the meeting, as well as the purpose of the meetings
Dependability is imperative for both the nurse and the client
Client strengths, limitations, and problem areas are identified
Outcome criteria and a plan of care are established
working phase
Orientation phase ends and working phase begins when the client takes responsibility for his or her own behavior change
Client shows commitment to working on issues that have caused a life disruption
Clients’ needs are prioritized- safety and health come first
RN assists the client to change problematic behaviors in a safe environment
termination phase
Relationship comes to a close
This phase begins in the orientation phase when meeting times are established- lets the client know that the relationship will come to an end
Avoids confusing the client who may be unable to recognized boundaries in a relationship
Termination occurs when the client has improved or has been discharged
thought process
how thoughts are formed, organized, and expressed. It involves the flow and coherence of ideas.
Descriptors
Speed
Thought blocking
Flight of ideas
Too many thoughts
Organization (Severity from mild to severe)
Circumstantial
Tangential
Loose associations
Word salad
thought content
the themes, ideas, and beliefs that occupy a patient's mind. It includes the presence of any delusions, obsessions, or preoccupations.
Descriptors:
Logical vs. illogical
Abstract vs. concrete
Magical thinking
Obsessions
Ruminations
Delusions
Ideas of Reference
Thought Broadcasting
Thought Insertion
Thought Withdrawal
thought process vs content
Example for Thought Process:
Mr. X’s thinking was logical and goal-directed, with some circumstantiality when discussing suicidal thoughts.
Example for Thought Content:
Mr. X exhibited delusions of persecution, believing that people were conspiring against him
perception
Abnormalities in how one perceives their environment
Hallucinations: Perceptions without an external stimulus.
Auditory (AH): Hearing sounds or voices that are not present.
Visual (VH): Seeing objects or figures that are not there.
Olfactory (OH): Smelling odors that are not present.
Tactile (TH): Feeling sensations on the skin that are not real.
Gustatory (GH): Tasting flavors that are not there.
Illusions: Misinterpretations of real external stimuli.
Depersonalization/Derealization:
Depersonalization: Feeling detached from oneself, as if observing oneself outside the body.
Derealization: Feeling that the external world is unreal or distorted
Hallucinations vs Illusions vs Depersonalization
Hallucinations:
Mr. X reports experiencing auditory hallucinations, describing hearing voices that are not present. He also mentions occasional visual hallucinations, such as seeing shadows moving in his peripheral vision. There are no reports of olfactory, tactile, or gustatory hallucinations.
Illusions:
Mr. X describes experiencing illusions, such as misinterpreting the rustling of leaves as whispers. He states that these occurrences are infrequent but distressing when they happen.
Depersonalization/Derealization:
Mr. X reports feelings of depersonalization, stating, "I sometimes feel like I am watching myself from outside my body." He also describes episodes of derealization, where the world around him seems unreal or distorted
judgement and insight
Judgment
Ability to assess and evaluate situations, make rational decisions, understand consequences of behavior, and take responsibility for actions.
Key Questions:
Can the patient make sound decisions?
Do they understand the consequences of their actions?
Insight
Ability to perceive and understand the cause and nature of one's own and others’ situations.
Key Questions:
Do they understand their illness?
Do they have insight into their relationships with others?
judgement vs insight examples
Judgment:
Mr. X demonstrated poor judgment during the assessment. He reported that despite knowing the potential legal consequences, he frequently drives under the influence of alcohol. He also mentioned impulsively quitting his job without securing another source of income, reflecting an inability to evaluate situations and make rational decisions.
Insight:
Mr. X exhibited limited insight into his condition. When asked about his mental health, he denied having any problems despite exhibiting clear symptoms of depression and anxiety. He also showed a lack of understanding of how his substance use affects his relationships and overall well-being, indicating a significant lack of insight into his situation
capacity
the case of whether or not an individual is capable of making health care decisions
Based on if the patient has the ability to:
Communicate
Understand information
Understand situation and its consequences
Rationale for treatment options
Capacity is Fluid – not static
Capacity can change from time to time
No specific psychiatric disorder automatically reduces it
Patients with neurocognitive disorders, psychotic disorders, etc., can have capacity depending on the state of their illness
competency
a legal term – determined by courts, not medical professionals
Adults are assumed to be competent, but a hearing may be pursued if:
Significant psychiatric disorder
Judgment impaired
Disease that impedes an individual’s ability to reason
If it is deemed that an individual is unable to make a competent, informed, and voluntary decision re: treatment, courts have stated that the med determinations and treatment plans are best left to the professionals
veracity and fidelity
Veracity
Definition: Being truthful and transparent with patients.
Example: Fully explaining risks and benefits of treatments.
Application: Ensure patients can make informed decisions based on accurate information.
Fidelity
Definition: Loyalty and commitment to professional duties.
Example: Keeping promises, providing consistent care.
Application: Maintain trust by fulfilling professional obligations and providing reliable care
justice
Fair and equal treatment of individuals
Access to resources
Equity vs. equality
Equity – focuses on fairness by ensuring everyone has what they need to succeed, recognizing that individuals don’t start from the same place.
Same starting place
Equality – treats everyone the same, which doesn’t necessarily lead to fairness when people have different starting points or challenges
Same outcomes
right to refuse
Patients have the right to refuse medications. Even if:
Psychotic
Involuntary
“Forced medications” (MOO/FMP) require:
Two physicians to agree that the medication is needed for sanctity of life
Involuntary commitment
Forcible medications change from individual treatment to public protection when medication is used to
Prevent violence to third parties
To prevent suicide
To preserve security
Forced medications should be provided in the least restrictive method.
Offer oral first, if refused and safety risk remains, provide injection
Identify your needs and orders before starting the shift
informed consent
Informed consent is a documented agreement from the provider and patient identifying that information was provided and agreed
Adequate information on the risks and benefits of a given treatment modality
Should be educated on alternative modalities
Assumes patient has decision-making capacity and adequate information
Assumes voluntary decision in regard to treatment – but patient must still be provided with risks/benefits even in the case of involuntary treatment
involuntary commitment
Criteria
The person is unable without the care, supervision and assistance of others to satisfy his/her need for nourishment, personal or medical care, shelter or self-protection or safety and that death or serious physical debilitation would occur within 30 days unless treatment was provided
The person has attempted suicide, or the person has made threats to commit suicide and committed acts in furtherance of the threats
The person has mutilated himself/herself or the person has made threats to mutilate and committed acts in furtherance of the threats
Danger to others shall be shown by establishing that within the previous 30 days the person has inflicted or attempted to inflict serious bodily harm on another or has threatened serious bodily harm and has committed acts in furtherance of the threat to commit harm to another
Obtaining the Warrant:
Subjective belief that the individual has met the criteria for a commitment
Locate crisis center in counter and meet with case worker who will support call to country delegate
County delegate: 24-hour service of an appointed individual’s staff that can give the power of warrant for arrest
Review narrative with county delegate
Approval or denial of the warrant/petition
Hospitalization:
Petitioner must agree to keep the client's belongs secure
Fax or deliver the warrant to the police who will pick up the client and take to the nearest facility for evaluation
ER provider agrees with warrant (or doesn’t) and the patient is admitted
Post-Hospitalization
Within 5 days the patient will have a hearing to determine the validity of the need for treatment based on the 302 criteria
Involuntary Denial
If the county delegate at any time denies the petition the evidence use cannot be used for further petitions
If the patient isn’t found the 302 is canceled
Evidence use cannot be used for further petitions
If the judge for the inpatient hearing find no safety issue with the petition the patient is allowed to leave (no 48 hours)
Evidence use cannot be used for further petitions
issues with involuntary
Details
Anyone can 302 anyone
Practitioners and providers can call delegate directly; others must use emergency centers
Issues
If an individual is not found for admission the petition is ruined
If the petitioner does not present for the hearing
If the information provided in the narrative does not meet criteria for the delegate
Well known patients
Authoritarian vs Autonomy
Authoritarian – false imprisonment will occur if it means safety for others
Approved 302->303 prevents the patient from owning firearms in the future
voluntary commitment
To go into the psychiatric lock unit legal agreement to be in the hospital locked floor is required called a “Voluntary Agreement” (201 in PA)
Safety concerns are still required
This patient has identified themselves that they are unsafe
If the patient later requests discharge:
Patient can be held on the on the unit for up to 72 hours until evaluated for safety
The patient will be discharged if the provider determines that the patient is safe
If the provider identifies criteria leading to risk, the mental health professional can convert the admission to an involuntary. Involuntary legal process will occur after this decision is made
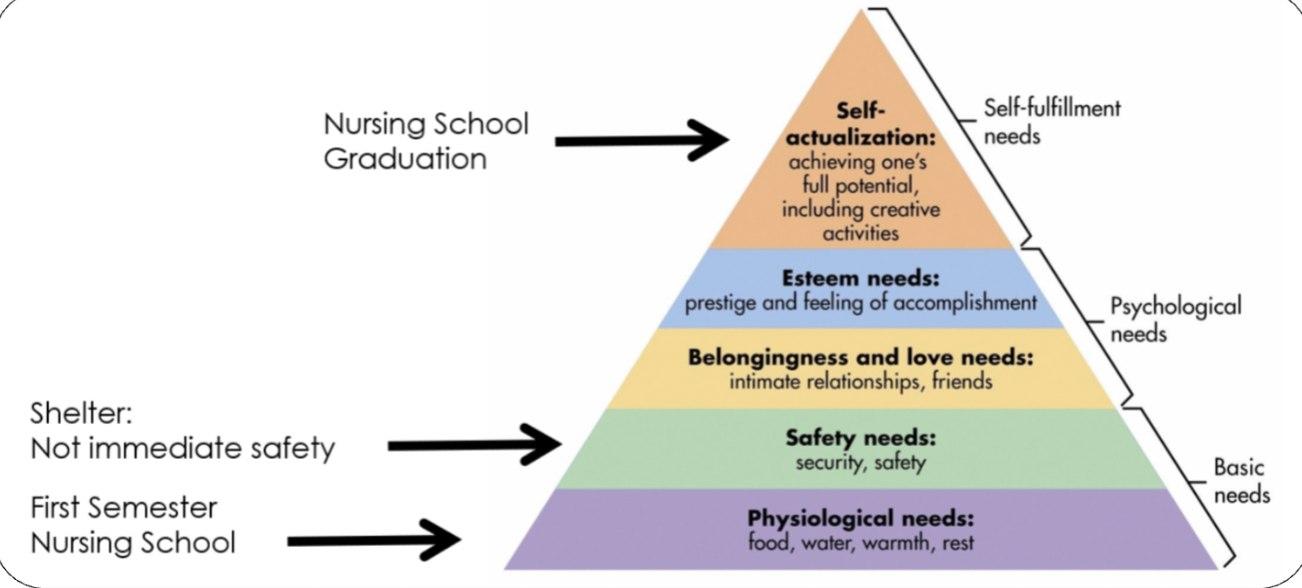
Maslow’s hierarchy of Needs
Abraham Maslow
Encourage us to look at the whole personality—not just the weaknesses (as past theories have focused on) but also the virtues
His theory proposes that humans have a hierarchy of 5 basic needs which are arranged in hierarchical order
CBT
Aaron Beck
Works to alter how we perceive the world to decrease a negative impact on our mood
most widely used therapy
The cognitive triad is Beck’s term to identify 3 common characteristics that distort the thinking of people with depression:
Negative Views of Self
Self image as defective/worthless
Negative views of the world
Evaluation of ongoing life events negatively
Negative Views of the future
“future holds no promise and that current difficulties will continue”
These cognitive distortions occur as automatic negative thoughts
The cognitive techniques help clients notice their own automatic negative thoughts and the connection of those thoughts to moods and actions
The behavioral techniques are used to show individuals that they are capable of interrupting/reframing dysfunctional patterns
DBT
Marsha Linehan
Psychotherapy to benefit characteristics of emotional distress for patient who
Difficult to think when affective
Difficulty with social situations
Conditioned for a chaotic environment
Deficit in coping skills to distress
Focus is on:
Mindfulness: Improving ability to accept and be present in the current moment.
Distress Tolerance: Increasing tolerance of negative emotion, rather than trying to escape from it.
Emotion Regulation : Skills to manage and change intense emotions
Interpersonal effectiveness: Techniques that improve communication in a way that is assertive, maintains self-respect, and strengthens relationships
Although considered an individual therapy it is recommended that it is provided in a comprehensive setting
Individual therapy
Group Therapy
Individual psychiatry
Work book homework
24-Crisis supports
Providing requires certification by Dr. Linehan
interpersonal therapy
Focus is on interpersonal problems rather than on personality reconstruction
Therapist identifies the nature of the problem that needs resolved
#1 intervention for adolescents
4 problem areas have been identified:
Grief
Role disputes
Role transitions
Interpersonal deficit
Identification of Interpersonal Issues:
Identification of specific interpersonal issues/problems that are contributing to their emotional distress
Communication Analysis:
Identification of communication styles and patterns that may be contributing to misunderstandings or conflicts in relationships
Role Play:
Exercises to help clients practice and develop better interpersonal skills.
Clients may reenact specific interpersonal situations or conversations, allowing them to gain insight into their behavior & responding.
Grief and Loss Work:
Techniques to help process emotions and adapt to these losses.
A supportive space to express grief and explore the impact of the loss on their relationships and sense of self
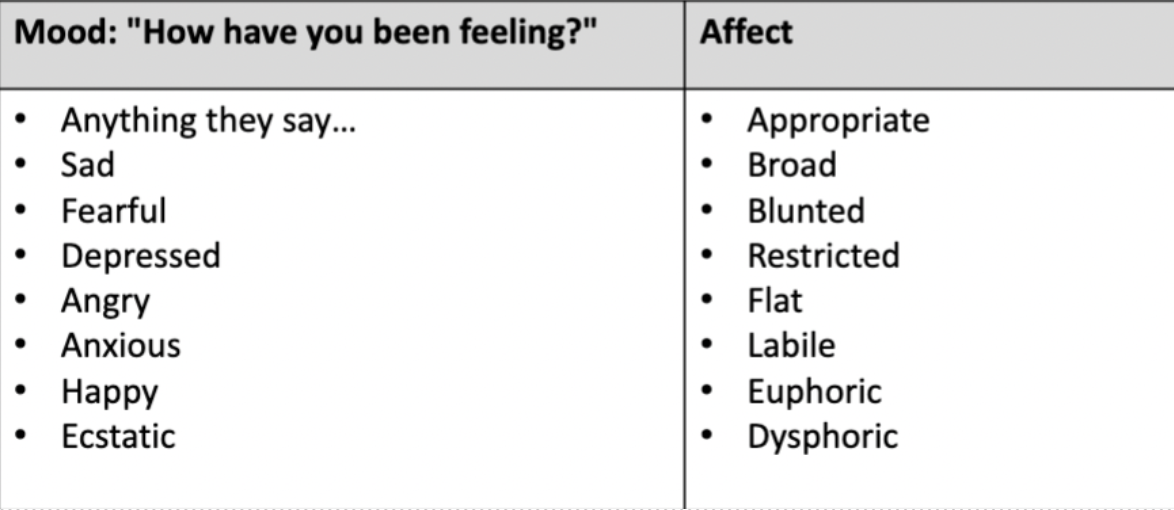
mood vs affect
Mood
what the patient says they are feeling. This is the only subjective part of the MSE.
Affect
the observable expression of emotion. It is what you observe
major depressive episode symptoms
1. Depressed mood most of the day, nearly every day,
2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month) or decrease or increase in appetite nearly every day.
Rule out: cancer, eating disorder, thyroid issues, T1DM
4. Insomnia or hypersomnia nearly every day
Psychomotor agitation or retardation nearly every day
6. Fatigue or loss of energy nearly every day.
7. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day
8. Diminished ability to think or concentrate, or indecisiveness, nearly every day
9. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
Major depressive disorder vs. Persistent depressive disorder (dysthymia)
Essentially prolonged, subthreshold depressive symptoms
Duration
2 years in adults
1 year in children/adolescents
Two (or more) of the following symptoms must be present
Poor appetite or overeating
Insomnia or hypersomnia
Low energy or fatigue
Low self-esteem
Poor concentration or difficulty making decisions
Feelings of hopelessness
Does NOT need to present dysfunction
SSRIs
examples
Fluoxetine (Prozac)
Paroxetine (Paxil)
Strong side effect profile limits patient profile, strong meds for OCD
Sertraline (Zoloft)
Citalopram (Celexa)
Escitalopram (Lexapro)
Fluvoxamine (Luvox) – OCD only
side effects
Many side effects are transient – provide patient education: Due to increase in serotonin
Headache
Nausea, vomiting, GI distress
Increases in anxiety/activation
Sexual side effects may be problematic and may not resolve with time.. This is from agonizing the 5ht-2A receptor
Other considerations:
QT interval prolongation (caution in the elderly)
Increased risk for bleeding/thrombocytopenia
Potential for hyponatremia
Increases in suicidality – Black Box Warning for children and adolescents
SNRI
examples
Duloxetine (Cymbalta)
Used for pain as well
Venlafaxine (Effexor)
Desvenlafaxine (Pristiq)
side effects
Headaches (transient)
Nausea, vomiting, GI distress (transient)
Increased anxiety/activation (transient)
Sexual dysfunction (typically persists with therapy)
Increased risk for suicidality
Major side effect that differs from SSRIs is dose-dependent increases in blood pressure during rapid titration
Must monitor blood pressure in these patients as a nursing intervention
TCAs
Examples
Amitriptyline (Elavil)
Amoxapine (Asendin)
Clomipramine (Anafranil)
Desipramine (Norpramin)
Dothiepin (Prothladen)
Doxepin (Sinequan)
Imipramine (Tofranil)
Lofepramine (Deprimyl)
Nortriptyline (Pamelor)
Protriptyline (Triptil)
Trimipramine (Surmontil)
Side Effects
Antagonists at serotonin transporter and norepinephrine transporter
Significant anticholinergic side effects – dry mouth, constipation, urinary retention
Anti-histamine properties – sedation and weight gain
Antagonist at alpha adrenergic 1 receptors – dizziness, sedation, hypotension
Risk for both cardiac arrhythmias (QTc prolongation) and seizures
Lethal in overdose
MAOIs
examples
Isocarboxazid (Marplan)
Phenelzine (Nardil)
Tranylcypromine (Parnate)
Selegiline (Emsam)
Does come in patch form – better side effect profile
CYP450 receptors exist in the small intestine, patch bypasses this
Side effects
significant issue with drug-food interaction, limiting patient tolerability and acceptability
Tyramine must be avoided -> if consumed, can lead to hypertensive crisis
Cured meats, red wine, aged cheese, beer
Grapefruit
Other notable side effects include sedation, anticholinergic side effects, and orthostatic hypotension
bipolar I vs bipolar II
I
The presence of 1 MANIC episode
Typically, even depression is more profound and severe
Suicidality Risk
Impulsivity associated with the diagnosis
Risk of suicide is 15x greater than that of the general population
Rapid cycling
Four or more episodes in 12 months
Associated with poorer outcomes
II
The presence of
Hypomanic episode
One major depressive episode
A manic episode excludes this diagnosis
Diagnosing
Very difficult to recognize, and can incorrectly be treated with SSRIs which may worsen disease trajectory
Years of evaluation before eventual identification
mood stabilizers
Lithium
Anticonvulsants
• Valproate (Depakote)
• Depakote (ER, Sprinkles etc)
• Divalproex Sodium
• Valproic Acid
• Lamotrigine (Lamictal)
• Carbamazepine (Tegretol)
• Oxcarbazepine (Trileptal)
Medications previously thought to work for bipolar
• Topiramate (Topamax)
• Neurontin
lithium
Short Term
• Polyuria and polydipsia (nephrogenic diabetes insipidus)
• Diarrhea, nausea, weight gain
• Acne, rash, alopecia
• Leukocytosis – False Positive
• Arrhythmia
• Toxicity - to be discussed on following slide
Long Term
• Goiter (euthyroid or hypothyroid)
• Renal impairments (10+ years)
• Hypercalcemia related to alterations of parathyroid functioning
0.6 – 1.2 mEq/L
NARROW THERAPEUTIC RANGE
Early signs of toxicity *
• Tremor: Can be a normal side effect
• Ataxia,
• Vomiting (very fine tremor may occur even at
therapeutic levels)
Profound signs of toxicity
• Mental status changes,
• Confusion,
• Coma
valproate
side effects
Common: Nausea, vomiting, abdominal pain, dizziness, tremor, weight gain
Hepatotoxicity
Incidence: Higher in children under 2 years and patients on multiple anticonvulsants
Action: Monitor liver function tests, watch for symptoms like jaundice, fatigue, and abdominal pain
DRESS Syndrome
Incidence: Rare but serious
Action: Report any signs of rash, fever, swollen lymph nodes, or other symptoms of systemic illness;
seek immediate medical attention
Thrombocytopenia
Incidence: Monitor platelet counts
Action: Watch for signs of bruising, bleeding, and report to a healthcare provide
Monitoring
Liver Function: Regular liver function tests
Platelet Count: Monitor for thrombocytopenia
Skin Reactions: Monitor for signs of DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms)
Caution in PCOS
lamotrigine
side effects
Common
Dizziness, headache, blurred vision, coordination problems, GI disturbances
Serious
Severe skin rashes (Stevens-Johnson syndrome, toxic epidermal necrolysis)
Multi-organ hypersensitivity reactions
Aseptic meningitis
Monitoring
Skin Reactions: Watch for rashes, especially initially
carbamazepine and oxcarbazepine
Side Effects
Common: Dizziness, drowsiness, nausea, vomiting, ataxia, visual disturbances
Monitoring
Liver Function: Regular liver function tests
Sodium Levels: Monitor for hyponatremia
Complete Blood Count (CBC): Watch for signs of blood dyscrasias (e.g., agranulocytosis, aplastic anemia)
Skin Reactions: Monitor for signs of SJS/TEN and DRESS syndrome
Blood Dyscrasias
Incidence: Rare but serious
Action: Monitor CBC; watch for signs of infection, unusual bleeding, bruising, and fatigue
Hyponatremia
Incidence: More common with oxcarbazepine
Action: Monitor sodium levels; watch for symptoms like nausea, headache, confusion, and seizures
Teratogenicity:
Risk of birth defects; contraindicated in pregnancy unless absolutely necessary
lithium tests
Renal function tests
Thyroid function
Serum electrolytes with special consideration for serum calcium
EKG
Weight/BMI
Beta-hCG pregnancy tests in all women of childbearing age
Serum lithium levels
Draw trough just before next dose (8 to 12 hours after previous dose) → usually first thing in the AM
steven johnson syndrome
Stevens-Johnson Syndrome (SJS)
Incidence: Approximately 0.04% of patients
Action: Any rash should be immediately evaluated; stop medication and seek emergency care.
SJS Progression
Prodromal Phase
Fever >102°F
Flu-like symptoms
Photophobia
Mucosal lesions
Cutaneous Phase
Widespread skin rash, often starting on the face and thorax
Blistering and peeling of the skin
Recovery Phase
Re-epithelialization (new skin formation)