Med Comp Exam #2 (W5 IE and joint replacements) (w6 allergies and biphosphates)
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
What is infective endocarditis (IE)?e endocarditis
A microbial infection of the endocardium or heart valves
what 3 things cause IE
viral, fungal, or bacterial
what is Bacterial endocarditis(BE)?
caused by vascular system invasion by bacteria(bacteremia)
3 microorganism VIRUSES that cause IE and what parts of the body are they
Viridans group streptococci (alphahemolytic): microorganisms from the mouth and the pharynx
Staphylococcus aureus: inhabit the skin
Enterococci: from the G.I. tract
what happens if IE gets really bad? like what are the complications?
• Valvular dysfunction
• Myocarditis
• Heart failure
• Death (untreated, 6 months to a year)
if you’re on the oral health care team, what should you watch out for? what percentage should you know?
be aware of unnecessary antibiotic prophylaxis. Approximately 30% OF ANTIBIOTIC USE IS INAPPROPRIATE
why does the AHA keep revisiting the guidelines for antibiotics?
basically, why should we hesitate to give antibiotics to to IE patients who are worried about catching it from dental?
REASON 1 out of FOUR REASONS
IE is much more likely to result from frequent exposure to random bacteremia with daily activities than from bacteremia caused by a dental procedure
e.g. tooth brushing 2x daily for one year had 154,000 x greater risk of exposure to bacteremia than from single extraction
REASON 2 why does the AHA keep revisiting the guidelines for antibiotics?
basically, why should we hesitate to give antibiotics to to IE patients who are worried about catching it from dental?
antibiotic prophylaxis may prevent only an exceedingly small number of cases of IE, if any, in individuals who undergo dental treatment.
REASON 3 why does the AHA keep revisiting the guidelines for antibiotics?
basically, why should we hesitate to give antibiotics to to IE patients who are worried about catching it from dental?
the risk of antibiotic associated adverse events exceeds the benefit.
REASON 4 why does the AHA keep revisiting the guidelines for antibiotics?
basically, why should we hesitate to give antibiotics to to IE patients who are worried about catching it from dental?
maintenance of optimal oral health and hygiene may reduce the incidence of bacteremia from daily activities and is more important than prophylactic antibiotics for a dental procedure to reduce the risk of IE.
Approximately 30% OF ANTIBIOTIC USE IS INAPPROPRIATE. Why?
• Use in patients without infections
• Improper choice of agent
• Improper dose and duration
• Overuse for medical prophylaxis
NBNBNBNB List the cardiac conditions at highest risk of the adverse outcomes of IE and which antibiotic prophylaxis before treatment is recommended (FIVE OF THEM)
1. Prosthetic cardiac valve (including transcatheter-implanted prostheses and homografts) (VALVE COMPLETELY REPLACED)
2. Prosthetic material used for cardiac valve repair (such as annuloplasty rings and chords) (YOU ARTIFICIAL VALVE NEEDED REPAIR)
3. Previous history of IE
4. A cardiac transplant WITH valve regurgitation due to a structurally abnormal valve (DAMAGED VALVE IN TRASPLANTED HEART) (YOU HAD A HEART TRANSPLANT AND YOUR VALVE IS LEAKY BC ITS ABNORMAL)
5. Congenital (present from birth) Heart Disease (CHD):
a) Unrepaired Cyanotic CHD including palliative shunts and conduits If your heart defect (present from birth) hasn't been fixed, you need antibiotics. This includes if you have shunts or conduits (tubes to redirect blood flow).
b) Completely repaired defect with prosthetic material or device within 6 months of the procedure. If your defect was repaired with artificial material (like a patch or device) within the last 6 months, you need antibiotics.
c) Repaired CHD defect with residual shunts or valvular regurgitation at the site of or adjacent to the site of a prosthetic patch or a prosthetic device Even if your defect was repaired, if you still have leaks or narrowing where the repair was done, you need antibiotics.
d) Surgical or transcatheter pulmonary artery
besides the adverse effects of congenital heart disease, can you take antibiotic prophylaxis for any other type of CHD
Except for the conditions listed above, antibiotic prophylaxis is NO LONGER recommended for any other form of CHD
What specific types of dental procedures are recommended to have antibiotic prophylaxis prior to performing?
all dental procedures that involve:
1. manipulation of gingival tissue or
2. the periapical region of teeth or
3. perforation (hole or puncture) of the oral mucosa
give some dental procedure examples where antibiotic prohy is recommended
• Extractions, dental implant
• Placement of orthodontic bands (not brackets)
• Periodontal procedures
• probing
• root planing or prophylaxis
• surgery
• Root canal or surgery beyond the apex
• Injection directly through the PDL (intraligamentary and intraosseous)
What types of procedures do NOT need antibiotic prophylaxis prior to treatment?
◦Routine anesthetic injections (through non-infected tissue)
◦Taking x-rays
◦Placement of removable prosthodontic or orthodontic appliances
◦Adjustment of orthodontic appliances & placement of orthodontic brackets
◦Shedding of deciduous teeth
◦Bleeding from trauma to the lips or oral mucosa
NBNBNBNB List the antibiotic prophylactic premedication recommendations (names and dosages) for an at-risk infective endocarditis patient using only oral meds
without an allergy to penicillin: Amoxicillin 2 g
with an allergy to penicillin: Azithromycin 500 mg
Clarithromycin 500 mg
*******Cephalexin 2g*******
Doxycycline 100 mg
Penicillin is in the same class as Amoxicillin!! If you are allergic to one you are allergic to the other!!
NBNBNBNB Which type of antibiotic should NOT be used when anaphylaxis, angioedema, or urticaria with penicillin has occurred ////////// if a patient has a hiiiistory with really bad allergic reactions (like anaphylaxis, angioedema, or hives) to penicillin/amoxicillin or ampicillin, you should not take ___________
cephalosporins. use another type.
List the four additional “dosing requirements” or the little procedure
◦Patients must take the antibiotic 30-60 minutes prior to dental treatment
◦If the antibiotic is inadvertently not administered before the procedure, it may be given up to two hours after the procedure. If you forget, you can take it up to 2 hours after.
◦Routine dental procedures should be scheduled at least 10 days apart if the same premedication is used. Wait at least 10 days between dental visits if you're taking the same antibiotic each time.
◦If shorter intervals must be scheduled, use another class of antibiotics (doxycycline, etc.) If you need to go sooner, you'll need a different antibiotic.
for example, over 10 days:
• First drug of choice: amoxicillin
• First debridement: macrolide (clarithromycin or azithromycin)
• Second debridement: doxycycline
• Third debridement: cephalosporin
• Fourth debridement: amoxicillin
EXTRA INFO ABOUT DOSING THAT IS NB
> even though the AHA says take it 30-60mins before treatment, IT TAKES AT LEAST 60MINUTES FOR ELEVATED AMOUNTS IN BLOODSTREAM
> 2g amoxicillin lasts 6hours, if its been longer, then give naother FULL dose
> If you know the patient has not taken their premed, you cannot work on them for a minimum of 30 minutes after premed taken
PART 2 !!!! Antibiotic Prophylaxis for Dental Patient with Total Joint Replacements
bacteremia in relation to joint replacement?
Bacteremia in the bloodstream may infect spaces in the area of a joint replacement
are invasive dental procedures associated with PJIs (prosthetic joint infection)?
no
invasive dental procedures are not associated with PJIs
do prophylactic antibiotics taken before dental treatment help prevent PJIs?
no.
prophylactic antibiotics taken before dental treatment do not help prevent PJIs
are antibiotics potentially harmful?
There are potential harms of antibiotics including risk for anaphylaxis, antibiotic resistance, and opportunistic infections
will the harms exceed the benefits or the benefits exceed the harms?
The benefits of antibiotic prophylaxis may not exceed the harms for most patients
Most people don't need antibiotics before dental work to prevent prosthetic joint infections (PJIs).
In medically compromised patients who are undergoing dental procedures that include gingival manipulation or mucosal inclusion, prophylactic antibiotics should be considered only after consultation with the patient and orthopedic surgeon.
AGAIN, No pre-med necessary after joint replacement EXCEPT for the patients with the following risk factors based on a med consult: 2TYPES, 2 and 4 total
NBNBNBNBNBNB No antibiotic prophylaxis is required for a TJR except for the high-risk conditions listed. These patients would require a med consult to determine whether antibiotic prophylaxis is necessary prior to oral treatment.
List the high-risk conditions
◦Immunocompromised/immunosuppressed patients:
>rheumatoid arthritis or systemic lupus
>drug (e.g. chemo or steroids)- or radiation-induced immunosuppression
◦Patients with co-morbidities
>history of previous joint infection or failure
>uncontrolled insulin-dependent diabetes NOT TAKING MEDICATIONSSS
>hemophilia
>HIV or malignancy
extra facts: Antibiotic prophylaxis is not recommended for dental patients with pins, plates, and screws.
NBNBNBNB List the antibiotic prophylactic premedication recommendations and dosages for an at-risk total joint replacement patient using only oral meds (there are less than the list for high-risk cardiac conditions):
without an allergy to penicillin: Amoxicillin 2g or Cephalexin 2g
with an allergy to penicillin: Doxycycline 100 mg
Antibiotic prophylaxis
The use of antibiotics to prevent infection in cardiac valves caused by bacteremia
Anaphylactic shock
A severe, and sometimes fatal, allergic reaction characterized by respiratory distress and hypotension, leading to cardiovascular collapse
Angioedema
Swelling of the lips, tongue and, in some cases, the larynx, leading to difficulty breathing.
Bacteremia
The presence of bacteria in the blood. It is when bacteria are in the circulating blood and capable of being transferred to distant sites within the body
Urticaria
Skin reactions characterized by itching, elevation of tissues (hives) with well-defined erythematous margins
Valvulopathy
a disorder of valve function causing a variety of cardiac disorders, such as arrhythmia, pulmonary hypertension, heart failure, and cardiogenic shock
ALLERGIESSSSS
Axium allergy question
“Are you allergic to or have you had a reaction to any of the following?”
Common allergies in dental practice (MAIN FIVE then etc.)
local anesthetics
aspirin
penicillin, antibiotics
Barbiturates, sedatives
Sulfa drugs
Codeine or other narcotics
Metals
Latex
Iodine
Pollen (hay fever, seasonal allergy)
Animal dander
Food
What IS an actual allergy - the immune system?
what is sensitization?
what happens with the antibodies, what’s the internal process of allergy ?
IT IS: Reaction of immune system to allergen >
Sensitization: formation of antibodies against allergen
Antigen stimulates production of antibodies
Memory cells develop
On re-exposure to allergen, antibodies bind to it
Antigen-antibody reaction occurs, leading to signs
Gives some examples of a mild allergy vs a severe allergy
Mild: Skin rash, Erythema (redness), Hives, Raised area, Urticaria (itching, hives)
Severe: Bronchiolar constriction, Asphyxiation, dyspnea (caused by angioedema), Reduction of blood pressure (vasodilation, shock), Cardiovascular collapse
LIST THE 4 TYPES OF HYPERSENSITIVTY REACTIONS with the nameee
a.) how rapidly they occur (if stated)
b.) one example of each:
Type I (immediate)
a) seconds to minutes after exposure
b) Hives, redness, itching Anaphylactic shock
Type II (cytotoxic)
a) not stated
b) HEMOLYTIC ANEMIA
Type III (arthus)
a) not stated
b) Arthralgia (joint pain), arthritis, lymphadenopathy, fever, urticarial skin lesions
Penicillin or Hep vaccine
(Arthus reaction refers to an acute, localized inflammatory response that typically occurs after vaccination)
Type IV (delayed)
a) days after exposure
b) latex allergy, poison ivy
Under a Type 1 hypersensitivity reaction, list the drugs used in dentistry that have caused fatal anaphylaxis and how quickly after exposure does a reaction happen?
local anesthetics (LA's) (such as benzocaine, tetracaine, and lidocaine) and aspirin
seconds to minutes after exposure
what is Hemolytic anemia
a condition where red blood cells are destroyed faster than they can be produced, leading to a low red blood cell count
what is Arthus
An Arthus reaction refers to an acute, localized inflammatory response that typically occurs after vaccination
OTHER REACTIONS
Local Anesthetic Reactions! What are the reaction results and what is it in LA that causes allergies.
reactions are a range: Mild skin rash to severe anaphylaxis
Esters (topical)
Benzocaine (Hurricaine)
Tetracaine (Pontocaine)
are amide allergies common or esters?
ESTERS! amide allergies are rare
Aspirin Reactions! are they common? who are they common with?
Uncommon in general population. More common in those with asthma
symptoms: range from mild skin reactions to anaphylaxis/bronchospasm/CV collapse
It is estimated that between 15% and 19% of those with _____ are allergic to aspirin
asthma
Penicillin! or other antibiotics! what is penicillin known as NBNB
Penicillin is known as the most allergenic drug?
why would you use penicillin and what are the symptoms of the reaction.
Commonly used to treat oral infections, if you’re allergic to it you can use Azithromycin or Clarithromycin or Doxycycline
Symptoms range from mild skin reactions to anaphylaxis
Barbiturates, Sedatives, or Narcotics!
why do we use these?
Barbiturates and sedatives may be used in dental offices for stress reduction
Narcotics and codeine prescribed for oral pain in combination with other drugs
NBNBNBNB Distinguish Allergic Reaction from Side Effects (Allergy V. Sensitivity)
list some signs of allergy then list some signs of common side effects
Signs of allergy
Rash, hives, & itching
Common side effects
Nausea & vomiting, gastrointestinal complaints
NBNBNBNB what will reducing the dose alleviate?
Reducing dose will alleviate side effects but not allergy
2 MANAGMENTSS
Management of Latex Allergy. Signs? and Prevention NBNBNB
signs: Dermatitis
Dry, reddened skin
Vesicles
Crusted lesions
Itching
Difficulty breathing
Prevention:
Cover latex stethoscope tube with a barrier
Use vinyl/non-latex gloves
Use latex-free injectable LA cartridges & polishing cups
Mark “LATEX WARNING” in chart
Dental products that contain latex include:
latex stethoscopes, gloves, injectable LA cartridges, and polishing cups
Management of Anaphylactic shock.
is it fatal?
Symptoms (signs)? and Management NBNB
Potentially fatal allergic reaction
Symptoms:
Immediate onset of skin reactions
Progression to respiratory & cardiovascular problems
Management:
Immediate injection of epinephrine
By dentist (sublingually)
By client (intramuscularly; EpiPen)
Call 911
Position patient upright & provide 100% oxygen
one more time, describe the 3 management strategies for anaphylactic shock:
◦Immediate injection of epinephrine
◦Call 911
◦Position patient upright and provide 100% oxygen
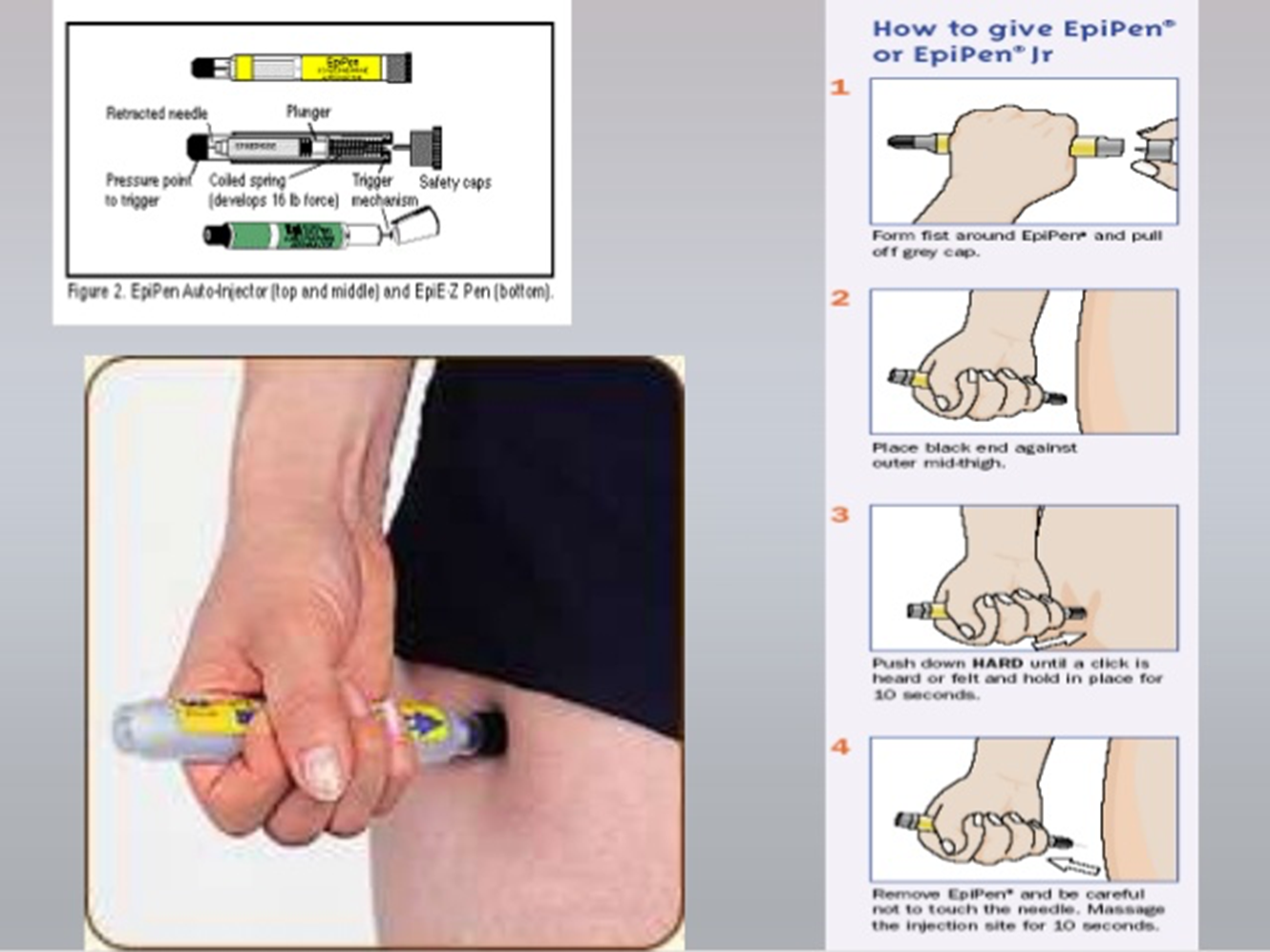
4 steps how to give epi pen
FINALLY TWO FOLLOW UP QUESTIONS NBNBNBNB
1.) Describe your symptoms (must ask!)
Nausea and vomiting or dizziness are side effects not allergic reactions
2.) Did your symptoms occur immediately or were they delayed? (very important to determine what type of allergy occurred)
when would you ask TH TWO MEGA FOLLOW UP QUESTIONSSSSSSSS NBNBNBNB
when a patient indicates a “positive” answer to having an allergy to a specific agent or substance to find out additional information to verify the severity of the allergy
what question do we ask to determine what type of allergy occurred? NBNB
Did your symptoms occur immediately or were they delayed?
fill in the blanks: “Hay fever or seasonal allergy, allergies to animals, and allergies to food are included because clients with a positive history of any allergy are at an _____ for having an allergy to products used as a part of ____ care…. “Usually the more _____the signs develop, the more _____ the situation.
increased risk
oral health
rapid
dangerous
Bisphosphonates and Antiresorptive Agents
ARONJ
List the 2 Axium questions relating to bisphosphonate use NB
HAVE YOU TAKEN, ARE YOU TAKING, OR ARE YOU SCHEDULED TO BEGIN TAKING ORAL
if this is a yes answer it will always be a yes. BISPHOSPHONATES?
Alendronate (Fosamax), Etidronate (didronel), Ibandronate (boniva), risedronate (actonel), or Tiludronate (Skelid)
Have you taken, are you taking, or are you scheduled to begin taking intravenous (IV) bisphosphonates? Clodronate (bonefos), Pamidronate (aredia), or zoledronic acid (reclast, zometa)
What conditions are bisphosphonates prescribed for?
Ø Management of osteoporosis
Ø Cancer of the bone
Ø Paget’s disease: chronic bone disease in older people
Ø Bone pain
Ø Hypercalcemia
NBNBNBNBNB what is the most common condition they (bisphosphonates and AR Agents) are prescribed for
Osteoporosis
what 2 ways can you take BIS and ARA and give an example
Oral: Fosamax
IV: Zometa
antiresorptive agent: Denosumab
When do we use BIS IV form?
chemotherapy with metastasis to bone
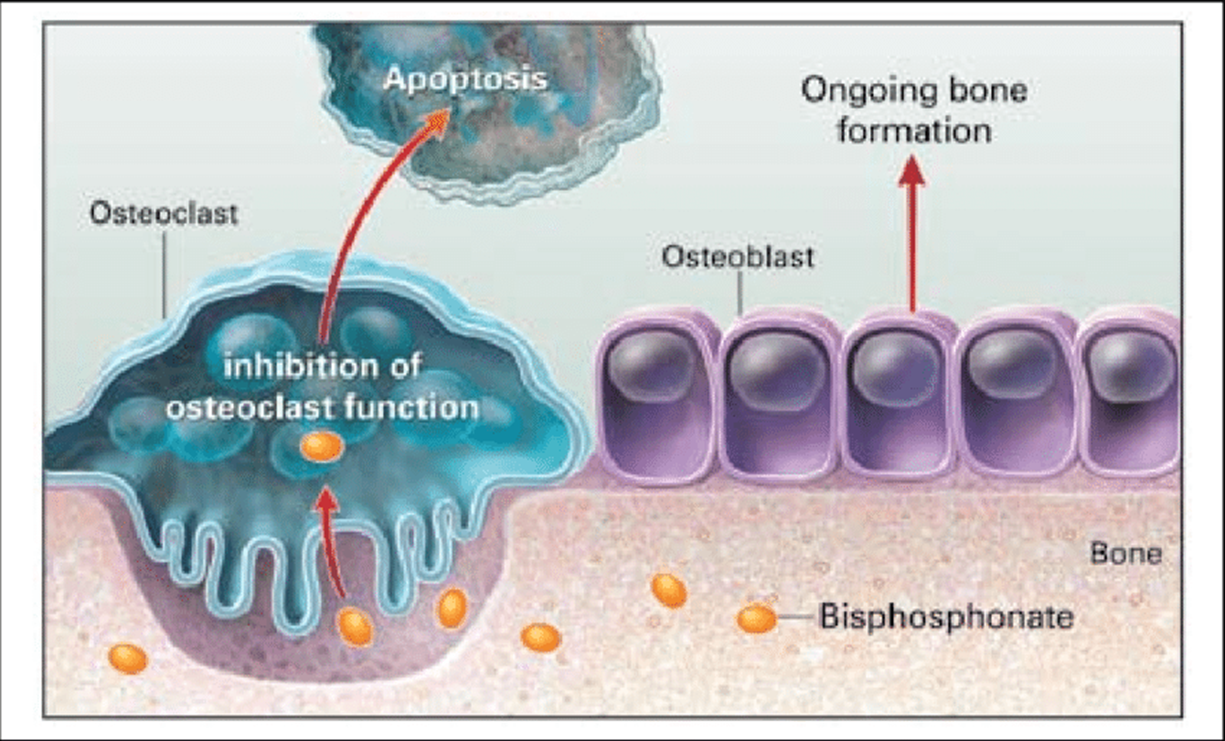
Mechanism of action for BIS and other AR agents
Powerful inhibitors of osteoclastic activity
> Bisphosphonates are drugs that target areas of higher bone turnover. (High bone turnover means your bones are breaking down and rebuilding themselves too quickly. This can lead to weaker bones and a higher risk of fractures)
> osteoclast cells, which break down old bone, absorb the bisphosphonate drug
> Their activity is slowed down
> This reduces bone breakdown
SIDE EFFECT: We know that bisphosphonates can:
interfere with the formation of osteoclasts
make osteoclasts self destruct or die early
change the signaling between osteoclasts and osteoblasts
normal bonce activity vs BIS
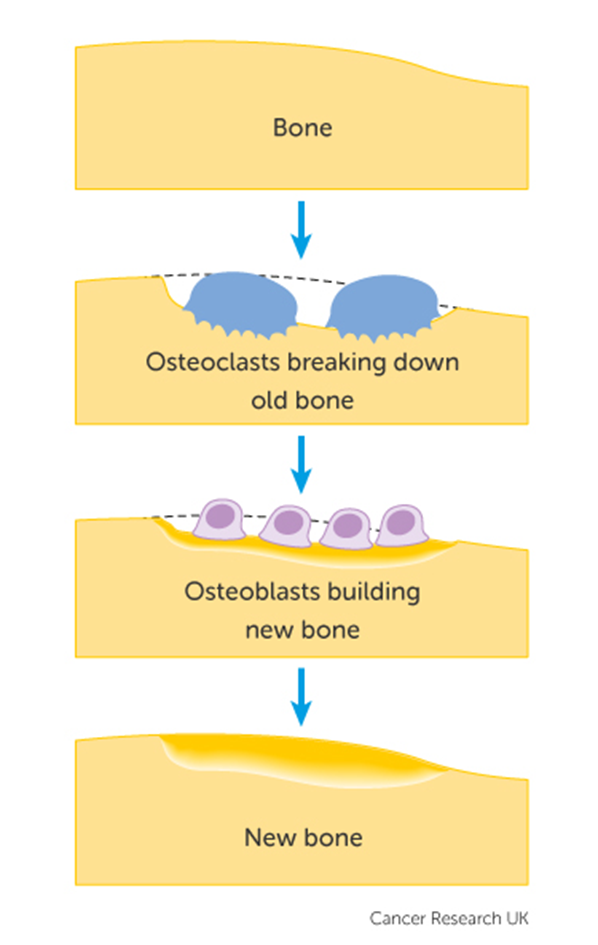
what happens if you use BIS too long?
Prolonged use may suppress bone turnover & cause damage
NBNB How long can bisphosphonates stay in the bone?
10+ years
ARONJJJJJJJJ
what does ARONJ stand for ? what is it ?
Antiresorptive-agent induced Osteonecrosis of the Jaw
it is an adverse drug reaction described as osteonecrosis of the jaw (ONJ) that may be related to the use of antiresorptive-agents and bisphosphonates
osteonecrosis as necrosis of bone due to obstruction of blood supply
so in summary, ARONJ refers to a serious condition where the jawbone dies due to reduced blood supply, often linked to the use of bisphosphonates and other antiresorptive agents.
when is it called MRONJ? or BRONJ?
When onset is associated with the use of drugs such as bisphosphonates, the condition is known as “medication-related osteonecrosis of the jaw” or specifically in the case of bisphosphonates, BRONJ
does ARONJ happen more often in the mandible or maxilla? and what loc?
It occurs more often in the mandible. most common at the mylohyoid ridge.
NBNB What risk factors may initiate ARONJ? BIG 3, then othersss
> Greater risk associated with IV forms of BIS
> Greatest risk: use of BIS for >2 years
> Increased risk from tooth extractions
Denture irritations
Bone trauma
Trauma to tori
Age >65 years
Periodontitis
Smoking
Diabetes
NBNBNB what is the greatest risk for ARONJ ? its the most likely, when a pt does what, they are at the greatest risk for developing ARONJ?
you’ve been using BIS for 2+ years
if you have a tooth extraction, is your ARONJ more risky?
Increased risk from tooth extractions
ARONJ is more prevalent in which form of BIS (oral or I.V.)
IV forms of BIS
what is this
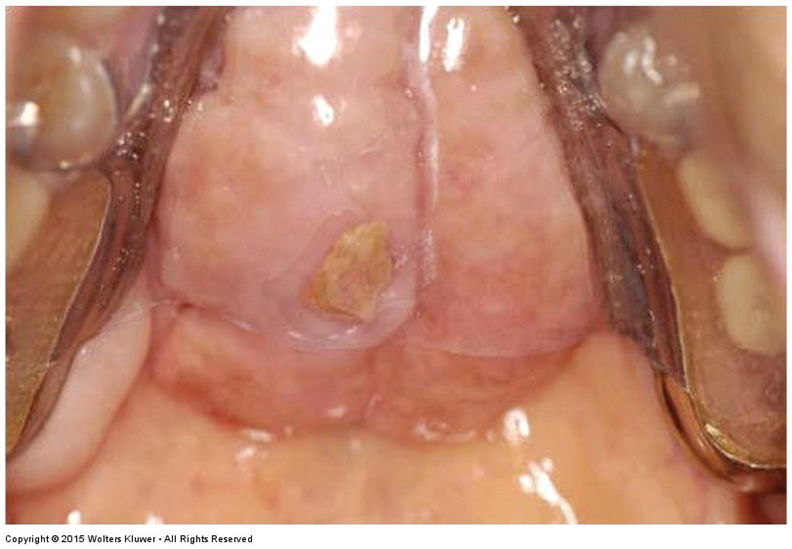
palatal tori
Signs and Symptoms of ARONJ ?
Spontaneous exposure of the jaw
Surgical site fails to heal
Pain
Tooth mobility
Ulceration of mucosa
Widening of periodontal ligament
NBBBB WHAT IS ORN ????? DIFFERENT TO ONJ
and What is ORN caused by?
Radiation induced Osteoradionecrosis (ORN) of the Jaw
vs osteonecrosis
high doses of radiation to the head and neck area
Prevention and treatment of BRONJ (4)
Extractions done prior to BIS therapy
Educate the patient regarding prevention of oral disease and infections (Good OHI)
Refer to oral and maxillofacial surgeon
Current recommendations based on experience of oral surgeons not on randomized studies due to the limited research on the subject.
if a pt is coming in for routine dental treatment—such as PROPHYLAXIS, fluoride carriers, dental restorations, or dentures— should we give special care?
NO special precautions are required for these patients.
is it better to give bisphosphonate therapy before or after there oral health treatments?
AFTER
what kinds of procedures should be done before bisphosphonate therapy?
invasive procedures - EXTRACTING TEETH, IMPALNTS
should BIS therapy be done before or after OSSEOUS HEALING, and is oral hygiene necessary?
AFTER optimum osseous healing is achieved
Maintenance of oral hygiene and follow-up are necessary.
for MRONJ, Which route of entry causes a higher risk?
IV
for MRONJ, How does duration of therapy affect the risk?
A longer duration of therapy with bisphosphonates is associated with an increased risk of MRONJ
Individuals who have taken oral BIS for over 2 years are at the greatest risk for developing ARONJ
What type of treatment is more likely related to ONJ?
Dentoalveolar surgeries, such as extractions, periodontal surgeries, or dental implants, are more likely related to MRONJ
What anatomical regions are at a higher risk for MRONJ?
mandible
palatal tori
mylohyoid ridge
Which arch is 2 x higher increased risk?
mandible
for MRONJ List Demographic and Systemic Risks:
◦Patients with a history of periodontal disease and dental abscess
◦Increased age; risk increases with each passing decade
◦Caucasians are at a higher risk
◦Malignancy diagnosis: patients with multiple myeloma, breast cancer or prostate cancer are at higher risk
◦Osteopenia/osteoporosis diagnosis