Micro 29 | RNA Virus Infections III
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What is the genome structure of the Influenza virus?
It has a linear ssRNA genome, segmented into 8 segments, and is enveloped with a helical capsid.
How is Influenza virus transmitted?
Through respiratory droplets.
What cells does the Influenza virus target
The respiratory epithelium.
What are the major surface glycoproteins of the Influenza virus?
Hemagglutinin (HA) – serves as the viral attachment protein (VAP).
Neuraminidase (NA) – required for viral release.
How many serotypes does the Influenza virus have and which ones are significant to humans?
There are three serotypes – A, B, and C. Only A and B are significant human pathogens.
What is the role of HA (Hemagglutinin) in the Influenza virus?
HA is the viral attachment protein (VAP) that binds sialic acid on the host cell.
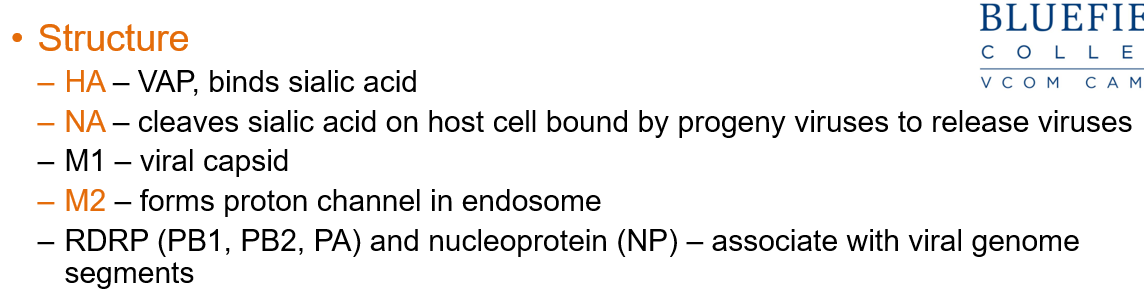
What does NA (Neuraminidase) do in the Influenza virus?
NA cleaves sialic acid on the host cell, allowing progeny viruses to be released.
What is the function of M2 in the Influenza virus?
M2 forms a proton channel in the endosome that helps uncoat the virus.
Which influenza type infects both animals and humans?
Only influenza A viruses infect both animals and humans.
What is the difference between antigenic drift and antigenic shift in influenza?
Antigenic drift: Small genetic changes causing minor variations.
Antigenic shift: Major genetic changes creating new viral strains.
Do both influenza A and B undergo antigenic drift?
Yes, both types A and B undergo antigenic drift.
Which influenza type undergoes antigenic shift, and why is it important?
Only influenza A undergoes antigenic shift when animal and human gene segments mix, creating new viruses that humans have no immunity against.
What happens when new viruses with different genetic makeups are generated in influenza A?
Antigenic shift, leading to a change in host tropism (which species it can infect) and disease severity.
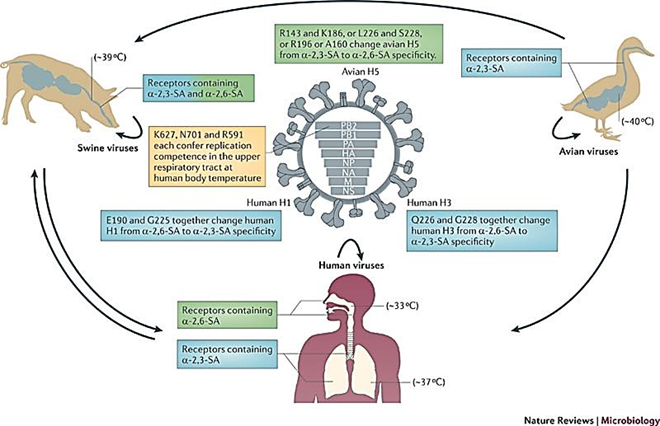
What factors enable antigenic shift in influenza A?
Ability to infect different species
Co-infection of one host with multiple different viruses
Segmented genome that allows reassortment of genes in progeny viruses
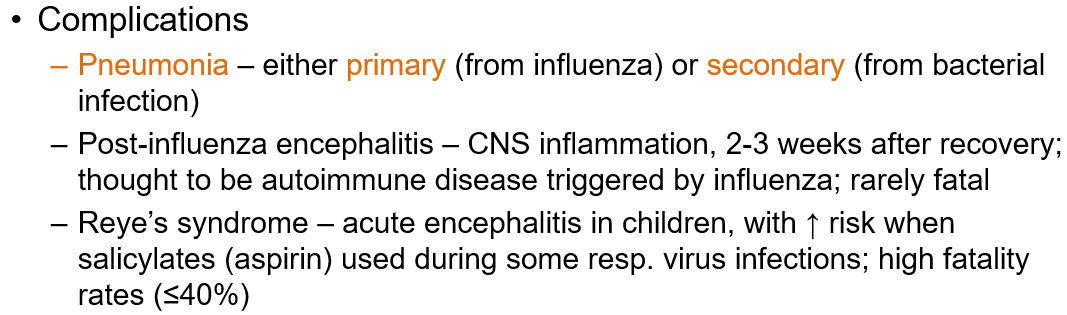
What are common complications of influenza?
Pneumonia (primary viral or secondary bacterial)
Post-influenza encephalitis (CNS inflammation, possibly autoimmune, rare)
Reye’s syndrome (acute encephalitis in children, especially with aspirin use during infection; high fatality rate)
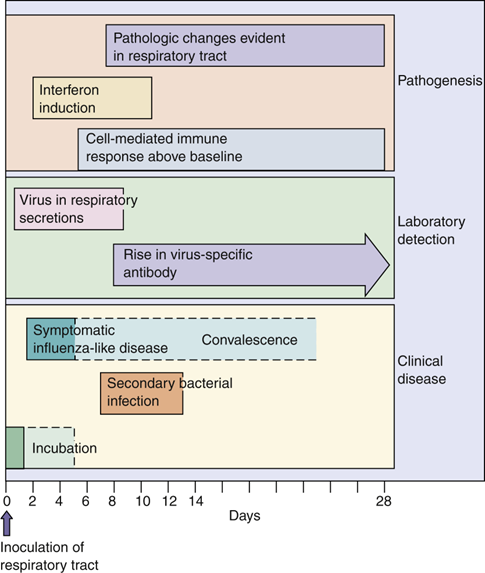
How is influenza attachment inhibited?
HA-specific antibodies produced by vaccines prevent viral attachment.
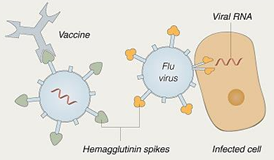
How is influenza prevented?
Vaccination
Inactivated or subunit vaccine: contains whole virus or purified HA/NA proteins from 3 strains, given intramuscularly.
What type of genome does Rubella virus have?
Single-stranded positive-sense RNA, enveloped, with an icosahedral capsid.
What disease does Rubella virus cause?
Rubella or "German measles."

How is Rubella virus transmitted?
Through respiratory secretions and droplets.
What is the disease progression of Rubella?
Replicates in the respiratory tract
Spreads to lymph nodes causing lymphadenopathy
Viremia spreads the virus throughout the body, leading to a rash
Describe the Rubella rash.
A pink rash lasting 3 days, starting on the face and spreading downward.

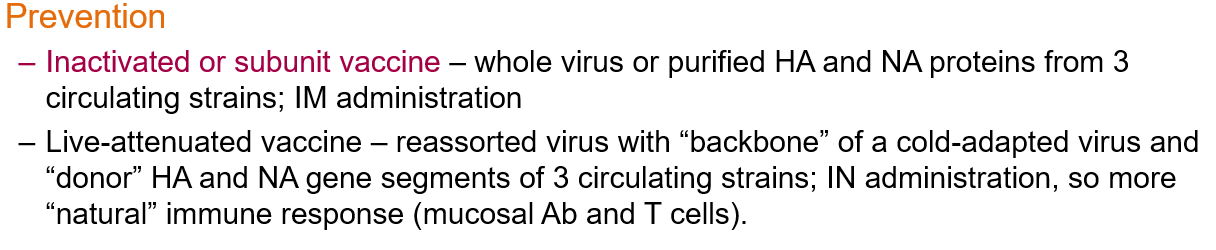
What is Congenital Rubella?
A condition where Rubella virus crosses the placenta during the viremic phase and infects the fetus.
What can Congenital Rubella cause?
Virus replicates in many fetal tissues causing teratogenic effects
Can alter fetal growth, mitosis, and chromosome structure
Infection during the first trimester may lead to cataracts, mental retardation, and deafness.
How does the immune system respond to rubella virus?
Antibodies protect and control the viremic spread.
Cell-mediated immunity is important in clearing the infection.
How is rubella prevented?
Live-attenuated vaccine (as part of the MMR: measles, mumps, rubella vaccine).
Measuring anti-rubella antibody titers early in pregnancy to check maternal immunity.
Vaccine campaigns, especially since the 1960s, aimed to immunize children to prevent transmission to pregnant women.

What does the term "blueberry muffin baby" refer to and what are its key features?
A newborn with purplish skin lesions caused by dermal hematopoiesis, often associated with congenital infections like congenital rubella.

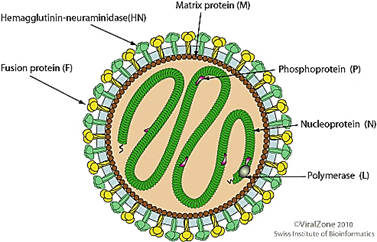
How are Paramyxoviridae and Pneumoviridae transmitted?
through aerosols, droplets, and fomites.
What are the viral attachment proteins for Paramyxoviridae and Pneumoviridae?
Paramyxoviridae: HN or H protein (with hemagglutination ability)
Pneumoviridae: G glycoprotein
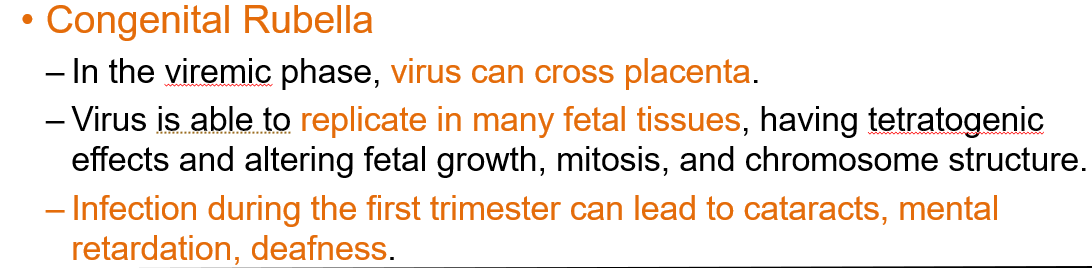
What is the role of the Fusion (F) protein in Paramyxoviridae and Pneumoviridae infections?
Helps the viral membrane fuse with the host cell membrane and promotes syncytia formation.

How does syncytia formation benefit Paramyxoviridae and Pneumoviridae viruses?
Allows the virus to spread from cell to cell and helps it evade the immune system.
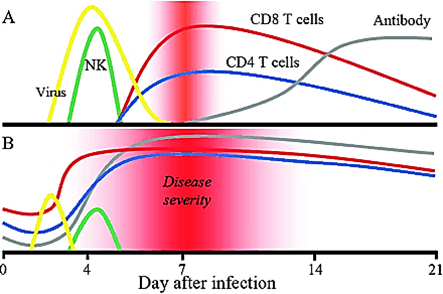
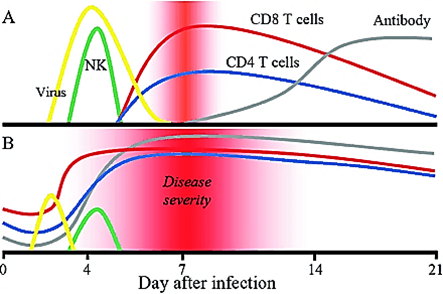
Why is cell-mediated immunity important in Paramyxoviridae and Pneumoviridae infections?
It is critical for clearing the infection but is also responsible for most disease symptoms.

What are the viral attachment proteins of the measles virus?
Hemagglutinin (H) and Fusion (F) proteins.
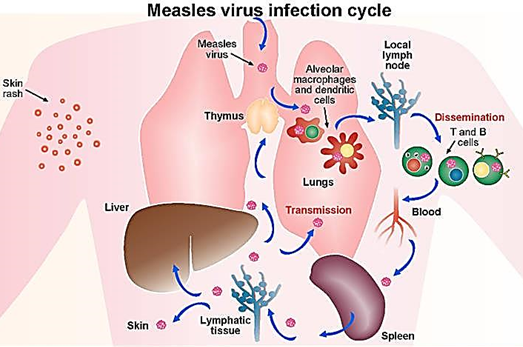
How does the measles virus spread in the body?
Viremic spread throughout the body.
From the upper respiratory tract lymph nodes, conjunctiva, urinary tract, small blood vessels, lymphatics, and the central nervous system
How is measles (Rubeola) transmitted?
By respiratory infection through aerosol droplets.
What are the symptoms of the measles prodrome phase?
The 3 C’s (cough, coryza, conjunctivitis), photophobia, and high fever.
What is the hallmark sign for diagnosing measles?
Koplik’s spots. Bluish-gray grains of salt with a red halo on the buccal membrane.

How does measles disseminate in the body?
By infection of lymphocytes and through viremia (free virus circulating in the blood).
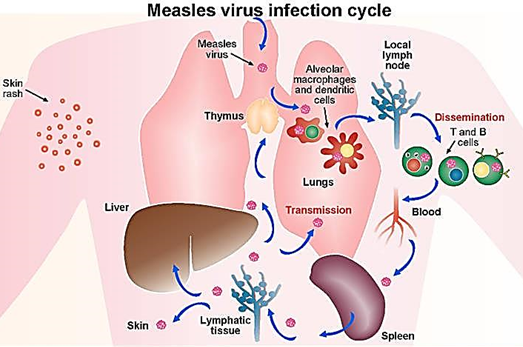
How does the measles rash develop?
The rash appears when the virus spreads to the skin and the immune system responds. It is caused by cytotoxic T lymphocyte destruction of infected endothelial cells lining small vessels.
What causes most measles-related deaths?
Giant cell pneumonia and secondary bacterial infections, especially in areas with severe malnutrition.
Interference with oxygen exchange due to synctia in the lungs
How can measles be prevented
MMR vaccine (Measles, Mumps, Rubella) — a live-attenuated vaccine that is highly effective.
What are the viral attachment proteins for the mumps virus?
Hemagglutinin-neuraminidase
Fusion proteins
What cells does the mumps virus target?
Epithelial cells of the upper respiratory tract, then spreads to the parotid glands
It can spread further to the testes, ovaries, pancreas, and thyroid.
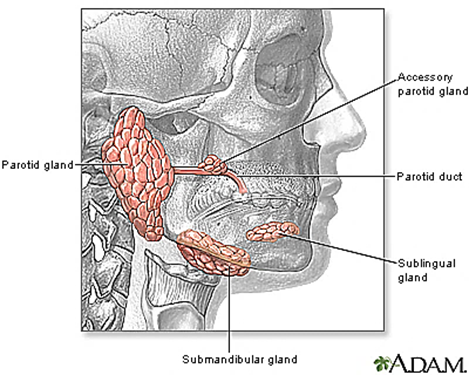
What are common clinical manifestations of mumps virus infection?
Sudden onset of bilateral parotitis (swelling of the parotid glands) and fever
Swelling of other glands: orchitis, epididymoorchitis, oophoritis, mastitis, pancreatitis (with or without parotitis)
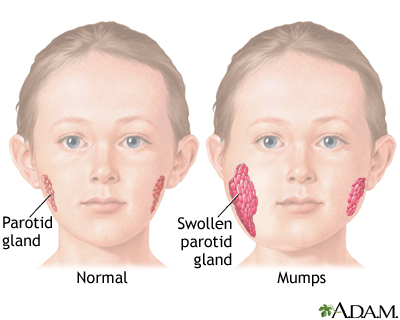
How can mumps virus infection be prevented?
MMR Vaccine (Live-Attenuated)
What are the viral attachment proteins of parainfluenza virus?
Hemagglutinin-neuraminidase
Fusion protein
Is parainfluenza virus infection systemic?
No, the infection is restricted to the respiratory tract, meaning there is no viremia.
How is parainfluenza virus transmitted?
Through large droplet aerosols and direct contact. It spreads rapidly in hospitals, causing nosocomial outbreaks in nurseries and pediatric wards.
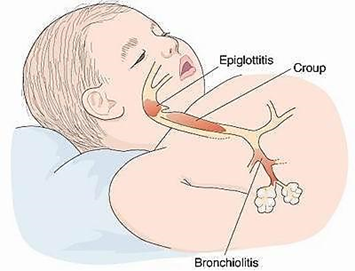
What diseases are caused by the parainfluenza virus?
Upper Respiratory Tract Infection: Causes mild cold-like symptoms (coryza, pharyngitis, wheezing, fever, mild bronchitis) limited to the URT; caused by all 4 serotypes.
Croup (laryngotracheobronchitis): Infection spreads to the lower respiratory tract, mainly in 2-5 year olds.

What are the hallmarks of croup caused by the parainfluenza virus?
Brassy "seal bark" cough
Steeple sign – tracheal/subglottal swelling that may block the airway
What is the leading cause of fatal acute respiratory infection in infants and young children?
Respiratory Syncytial Virus—RSV
What are the viral attachment proteins for RSV?
Attachment (G) glycoprotein – NO hemagglutinin activity
Fusion (F) glycoprotein
How is RSV transmitted?
Through large droplets and direct contact
Who are the high-risk populations for RSV?
Premature infants (weak lungs and low antibodies)
Elderly (weaker immunity, chronic diseases)
Bone marrow and heart-lung transplant recipients (immunosuppressed, severe infection risk)
What diseases does RSV cause?
RSV causes mild cold-like symptoms to severe pneumonia
Bronchiolitis in children, with 25-33% affected and 2-5% requiring hospitalization.
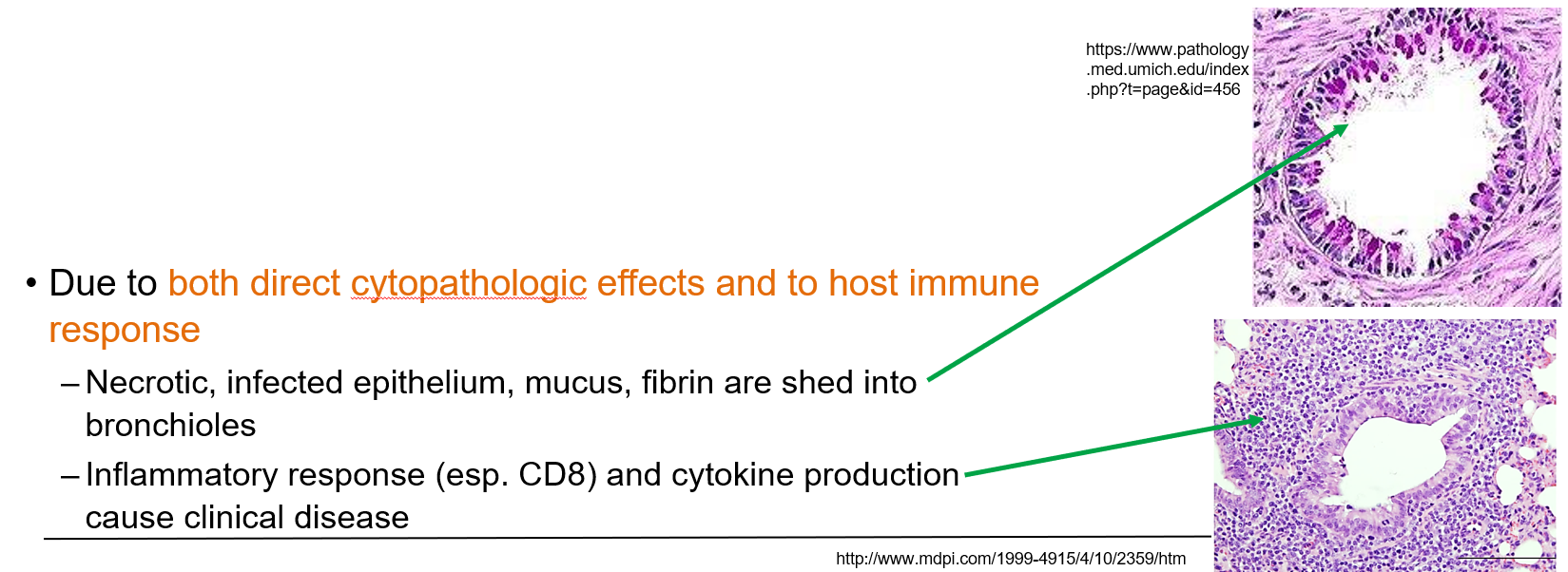
What causes clinical disease in RSV?
Both direct cytopathic effects (epithelial cell death, mucus, fibrin) and the host immune response (CD8+ T cells, cytokines) lead to airway damage and disease.
Is antibody protection effective against RSV?
Yes, but only during the initial infection. It is limited due to RSV spreading from cell to cell.
Does maternal antibody protect infants from RSV?
It offers some protection but is usually too low to be fully effective.
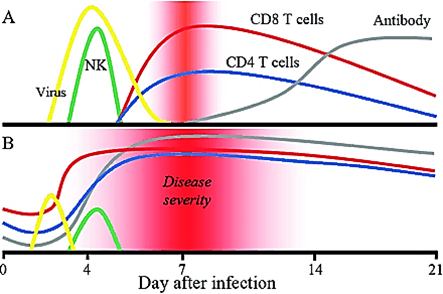
What is required to clear an RSV infection?
Cell-mediated immunity
Why do people get reinfected with RSV?
Naturally induced immunity is short-lived, causing reinfections every 2-5 years.
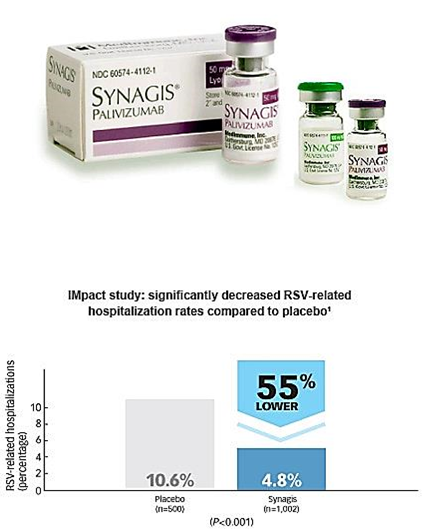
How can RSV be prevented?
Passive antibody (monoclonal antibody against RSV F protein)
Maternal antibody: Protects the infant if mom’s antibody levels are high (pregnant moms can be vaccinated).
Vaccination:
Arexvy® (GSK): for elderly (licensed 2023)
Abrysvo® (Pfizer): for elderly and pregnant women (licensed 2023)