Lecture 14: Nerve Structure and Function
1/90
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
How many pairs of cranial nerves are there?
12 pairs of cranial nerves
How many pairs of spinal nerves are there?
31 pairs of spinal nerves (mixed nerve)
Define what a spinal nerve is.
A nerve that is….
Closer to the spinal cord
Connects the dorsal and ventral root
T/F: Both peripheral nerves and spinal nerves have connective tissue elements and vascular structures that encompass the nerve fibers
True
Peripheral nerve is a composite material meaning it contains….
Neural tissue
Connective tissue (collagen)
Blood vessels
T/F: Peripheral nerves are not well vascularized
False
They are highly vascularized
When compression and tension occur to a peripheral nerve, what components of the composite material does it impact?
Impacts the neural tissue as well as the vascular system
What are the most common types of injuries for peripheral nerves?
Trauma
Entrapment
What is another term for a compression force?
“Crushing”
Discuss the nerve fiber structure.
Axons covered by myelin sheath (which are formed by Schwann cells if the nerve is in the periphery)
What is the function of nerve fibers?
Transmit electrical signals (to target tissue)
Serve as a conduit to allow for axonal transport (nutrients ← → nervous system)
Various substances synthesized in the cell body (e.g., proteins) and are transported back and forth
Where is the interneural connective tissue located for a peripheral nerve?
Located outside of the myelin sheaths
What is the function of the interneural connective tissue?
Important to help the nerve fibers not be exposed to stretching and compression
Where is endoneurium located?
Inside the fascicle (around the axon)
What is endoneurium composed of?
FIbroblasts and collagen
What is the perineurium?
Lamellar sheath that encompasses each fascicle
What is the function of the perineurium?
Acts as a chemical barrier and has great mechanical strength
What is the epineurium?
Surround bundles of fascicles and is superficial in the nerve
What is the epineurium composed of?
Loose CT
T/F: Epineurium can vary in abundance between nerves or within nerves
True
Which layer of interneural connective tissue is the strongest?
Perineurium (but all layers help protect the nerve against compressive and tensile loads)
T/F: Spinal nerves do not have epineurium or perineurium
True
Are the layers of CT coverings of peripheral nerves vascularized?
Yes, peripheral nerves are highly vascularized within all layers of CT coverings
The vessels of peripheral nerves are very sensitive to _________ changes and are under a _________ amount of __________
The vessels of peripheral nerves are very sensitive to pressure changes and are under a constant amount of pressure
If the vessels of a peripheral nerve are closed off, what does this cause?
Nerve ischemia
Nerves are designed to communicate information via electrical _______________; to accomplish this nerve needs to be able to _______ through their ________ and relative to the ____________.
Nerves are designed to communicate information via electrical potentials / ion changes; to accomplish this, the nerve needs to slide through their sheaths and relative to the surrounding tissue
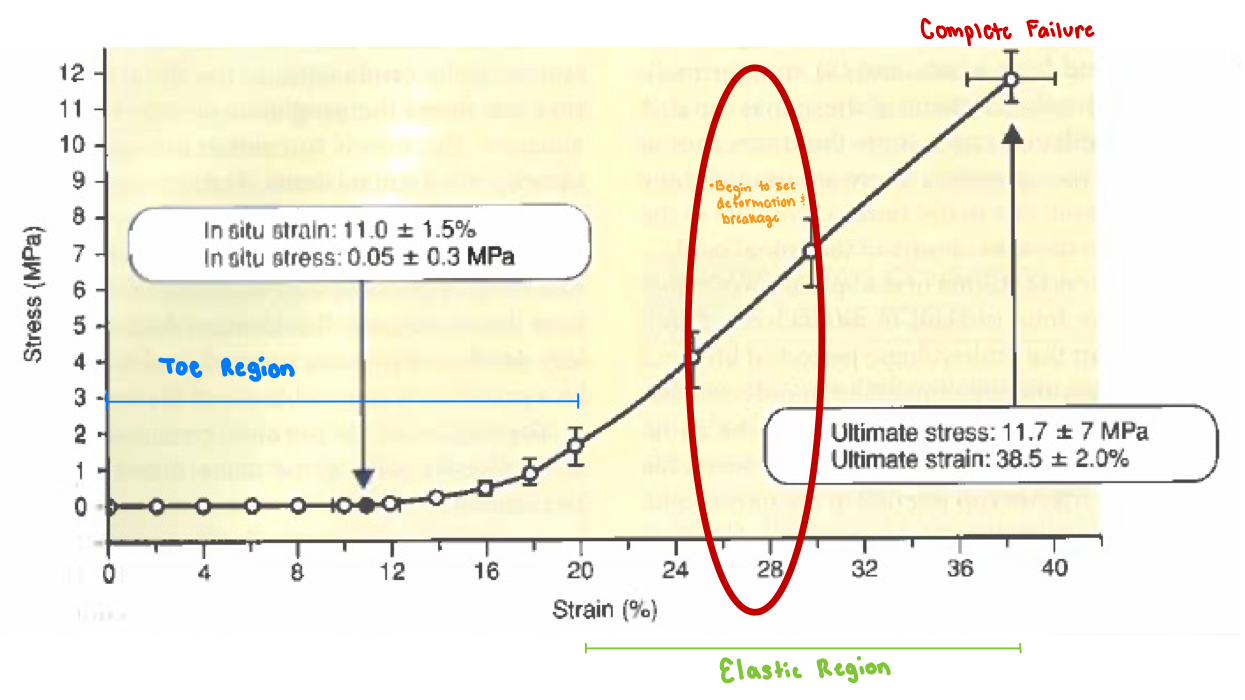
Discuss the stress-strain relationship of nerve?
Long toe region
Long elastic region
No plastic region
Basically goes straight to failure
However, deformation still occurs prior to failure, just within elastic region
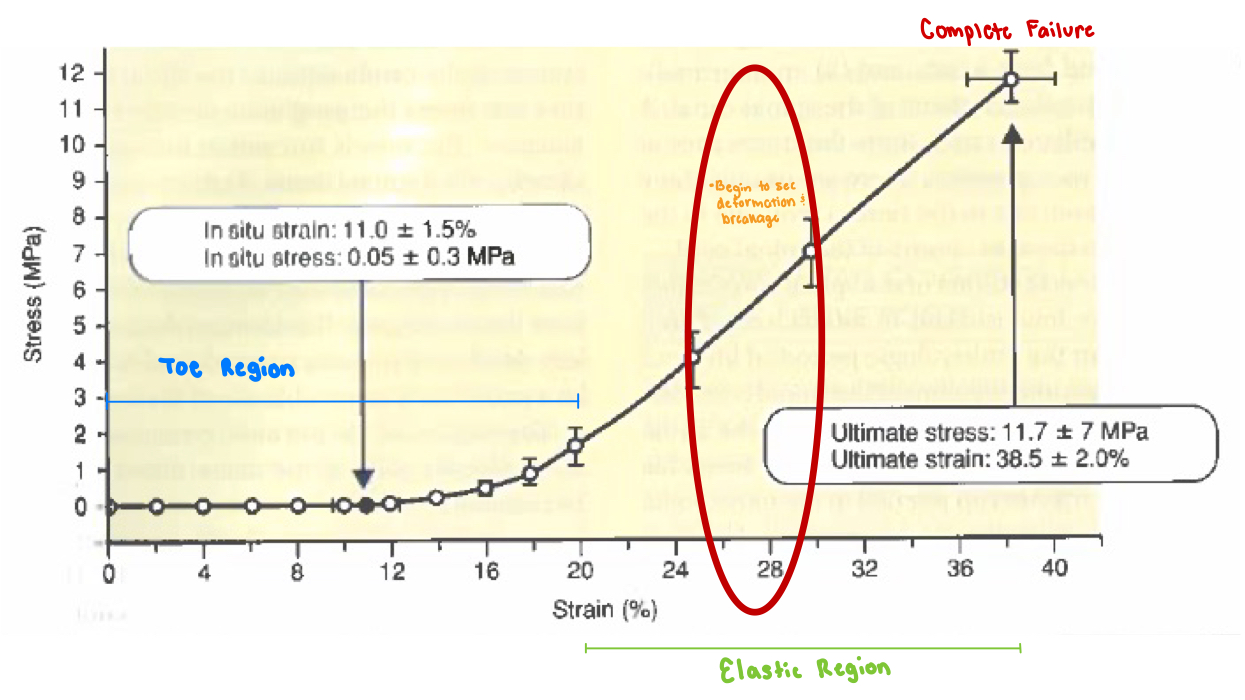
How much strain has occurred at the end of the toe region?
~15-20%
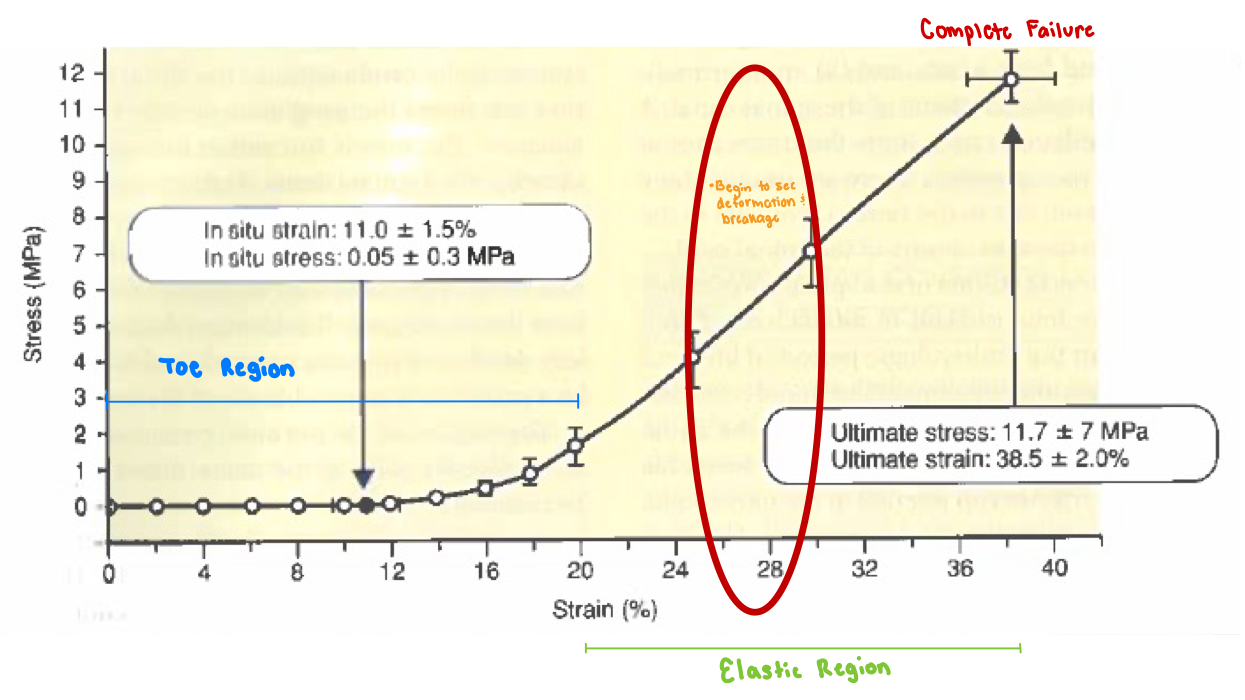
What percent of strain is the maximal elastic region at?
Maximal elastic region is ~20% strain
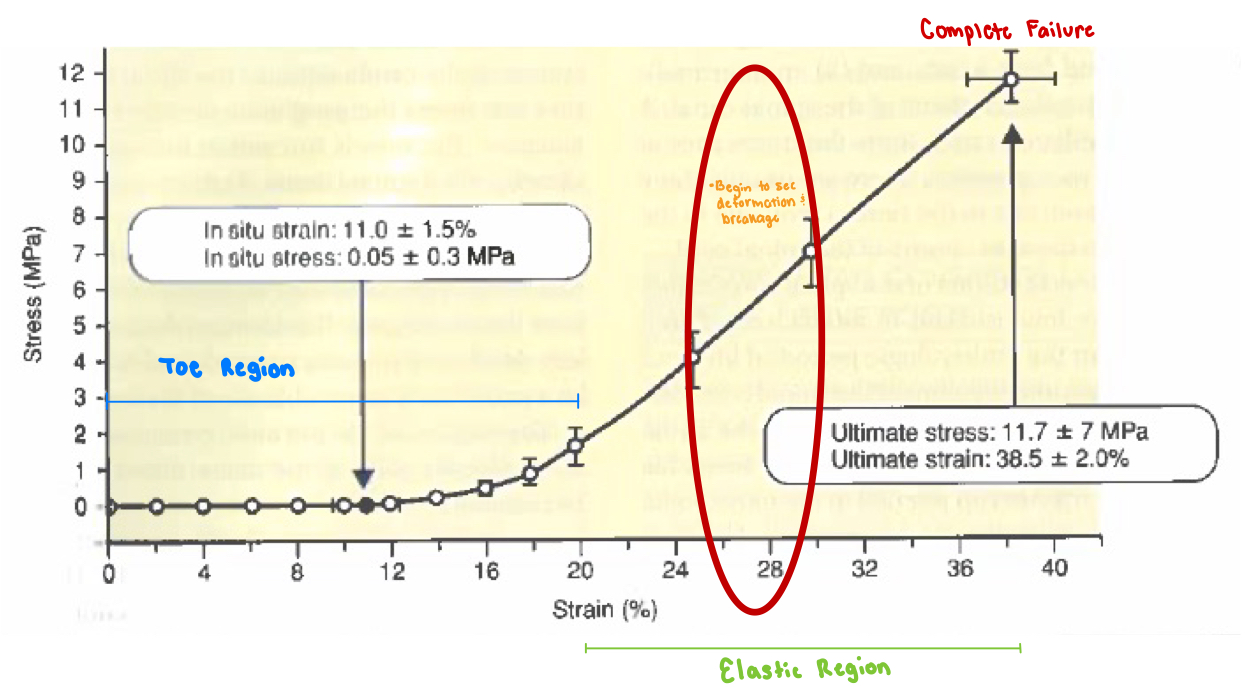
At what percent strain does complete structural failure occur?
25-30% strain
(Fibers of the perineural sheath endoneurium begin to break at 25-30% strain)
How does brachial plexus injury occur?
High energy injury (“stinger”)
Birth canal injury
What does the outcome of a nerve injury (e.g., brachial plexus injury) depend on?
Outcome depends on which tissue components are injured as well as the extent of the injury
T/F: There can be significant structural damage without visible damage to the nerve
True
How do we know when an individual who suffered a neural injury can return to activity?
The individual should not have any neural symptoms when returning to full activity (sensory and motor)
How much strain can occur before there are vascular effects?
Vascular impairment begins at 8% strain
Vascularization/blood supply completely ceases at 15% strain
How much strain can occur before there are neural effects?
Decreased action potential is identified at 6% strain
Action potential is completely blocked at 12% strain
Connective tissue (elastic region) of nerve remains intact until what percent strain?
20% strain
The connective tissue of nerve can remain intact at a greater percent strain compared to its vascularization and neural tissue. What does this mean?
The nerve could still be mechanically intact, but is not functionally intact
Shows the difference between mechanical abilities and physiological abilities
What is an example of a slower-tension injury?
Growth of a tumor
What occurs to the nerve with a growth of a tumor?
Fibers are forced into a circumferential course around the gradually expanding tumor
T/F: The effects of a tumor / slower tension injury can be minimal or non existent.
Why or why not?
True
This ie because the tumor growth / tension is slow enough that it has the ability to spread out (and not get compressed, etc.)
[However, once the tumor gets really big, then you can have issues with compression]
A double crush injury leads to…
Adhesions
What do adhesions leads to / cause?
Adhesions create anchors which create tension force on the nerve with limb movement
→ results in a combination of compression and tension injuries
How would you treat a double crush injury?
Treat by reducing adhesions
Surgical
Soft Tissue Mobilization (e.g., cupping)
Stretching
If a nerve is entrapped in two areas (e.g., double crush injury), it it “worse” if the areas are close together or far apart?
Worse if the areas are farther apart
Means that the nerve will be more affected (due to larger portion of the nerve being affected)
T/F: Neural tissue cannot be restored if pressure is relieved after 2 hours of compression
False!
Neural tissue can be restored if pressure relieved after 2 hours of compression
After how many hours of compression leads to permanent damage?
Above 4 hours will likely lead to permanent damage
HOWEVER can still be restored with healing (just not going to be restored from only relieving pressure)
For axonal transport, after __ mmHg of pressure, distal sites can lack _______ making it more susceptible for further _______
For axonal transport, after 30 mmHg pressure, distal sites can lack proteins making it more susceptible for further compression (double crush)
At what pressure can blood flow effects be observed?
30 mmHg pressure has been observed in carpal tunnel syndrome
80 mmHg can lead to complete blockage of intraneural blood flow
What pressure can cause structural nerve damage? What does this lead to?
Higher levels of compression of ~400 mmHg can cause structural nerve damage
Causes rapid deterioration of function
What fibers are affected first by compression?
Large diameter fibers are affected first (alpha motor neurons)
T/F: There is little deformation of nerve tissue prior to yield in compression
True
What factors are important regarding a nerve’s reaction to compression?
Amount of loading
Mode of application
(Not as rate sensitive)
The greatest effect that compression can have on the nerve “function” is…
Occluding blood supply
What mode of application is the most damaging to nerve tissue?
Direct pressure on nerve tissue is most damaging (rarely occurs unless it is internal)
T/F: Nerves can tolerate a lot of deformation prior to injury in compression
False!
Nerves tolerate very little deformation prior to injury in compression
T/F: Large diameter fibers undergo relatively greater deformation with force application than smaller fibers
True
Define uniform pressure. What does it cause?
Uniform Pressure - applied around the entire nerve
Causes…
The nerve to remain circumferential, but reduce the diameter in the loaded region
Radial pressure
Carpal Tunnel Syndrome
Define lateral compression. What does it cause?
Lateral Compression — when the nerve is placed between two flat surfaces and the are squeezed together
Causes…
Deformation of the cross-section (from circular to elliptical shape)
Sudden blow to nerve
Disc herniation
What is the root sleeve?
Connective tissue that separates axons from the CSF
Like pia mater proximally
Like arachnoid matter distally
What is the function of the inner layer of the root sheath/sleeve?
The inner layers of root sheath constitute a diffusion barrier between the endoneurium of the nerve roots around the CSF
(however, it is weak and only prevents macromolecules)
The spinal dura encloses what two structures?
Nerve Roots
CSF
What are the 2-layers of the spinal dura?
Inner Layer
Joins arachnoid and becomes spinal dura
Outer Layer
Adheres to the periosteum of the part of the laminae of the cervical vertebrae
What is the neurothelium?
An effective barrier between the dura and the archnoid (formed by the inner and outer layer of the spinal dura)
T/F: Neurothelium bests resists stress
True
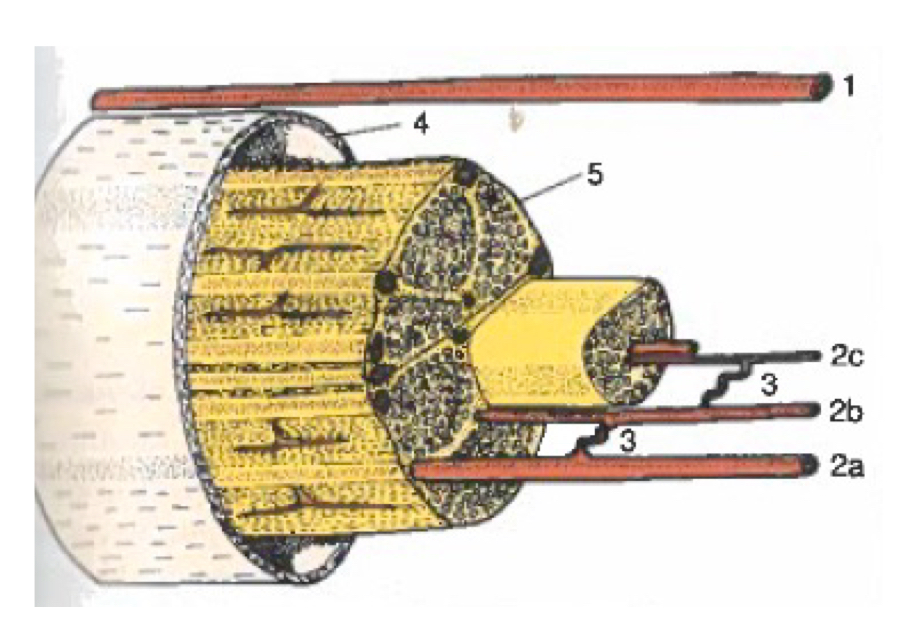
What does (1) in the photo depict?
Extrinsic Vascular System

What does (2) in the photo depict?
Intrinsic Vascular System
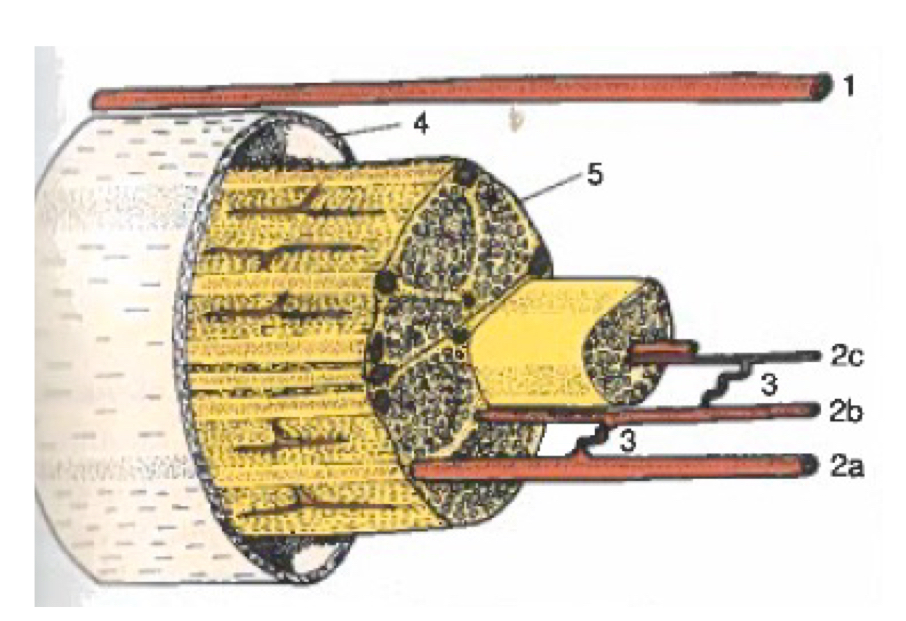
What does (3) in the photo depict?
Vascular Coils (connecting multiple intrinsic vessels)
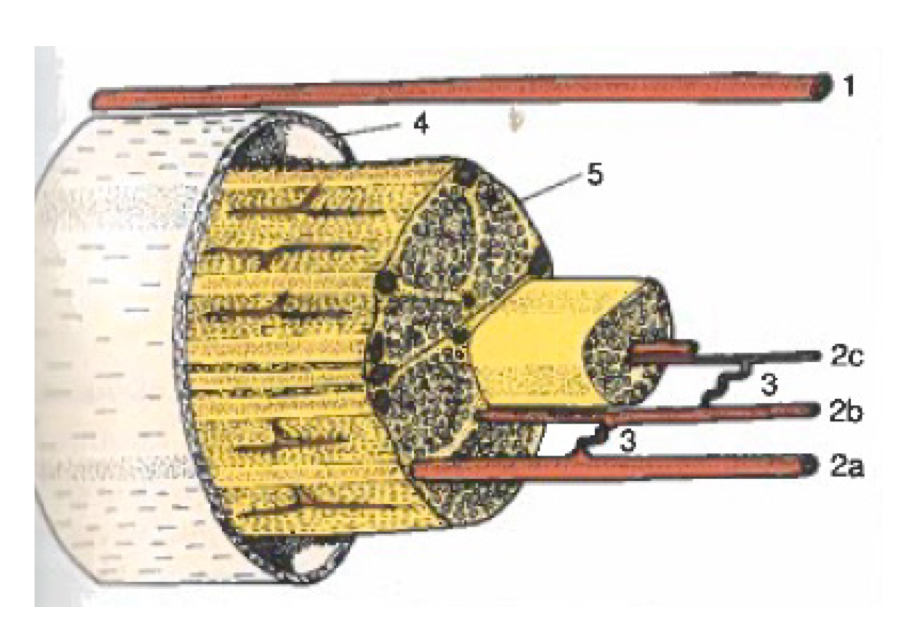
What does (4) in the photo depict?
Spinal dura
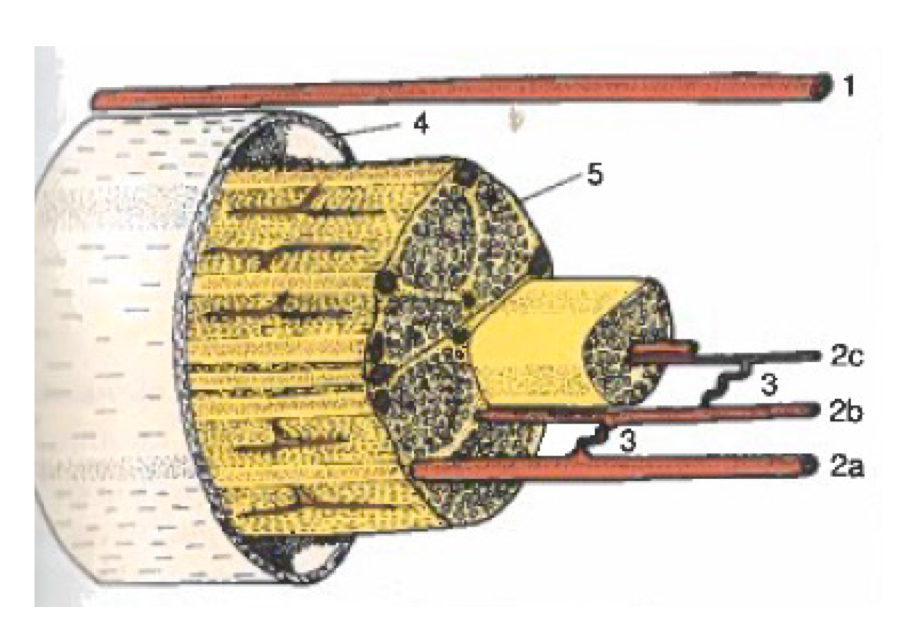
What does (5) in the photo depict?
Root sheath
T/F: Within the thecal sac, there are neural sheaths surrounding the spinal roots
False
Within the thecal sac, there are no neural sheaths surrounding the spinal roots
→ this causes mechanical properties to be greatly lowered
What is the function of bone that surrounds spinal nerve roots?
Helps prevent excessive compression/tensile loads from occurring
Once a spinal nerve root is out of the ___________ the strength of the nerve fiber is ________.
Once a spinal nerve root is out of the intervertebral foramen sheaths (e.g., intrathecal sac) the strength of the nerve fiber is increased
Does failure in spinal nerve roots occur at higher or lower stress values (compared to peripheral nerve)?
Failure of spinal nerve roots occurs at lower stress values
Does failure in spinal nerve roots occur at higher or lower strain values (compared to peripheral nerve)?
Failure of spinal nerve roots occurs at lower strain values
T/F: The mechanical properties of a spinal nerve depends on its location in the spinal cord.
True!
(e.g., spinal nerve at S1 can undergo more strain than the L5 spinal nerve)
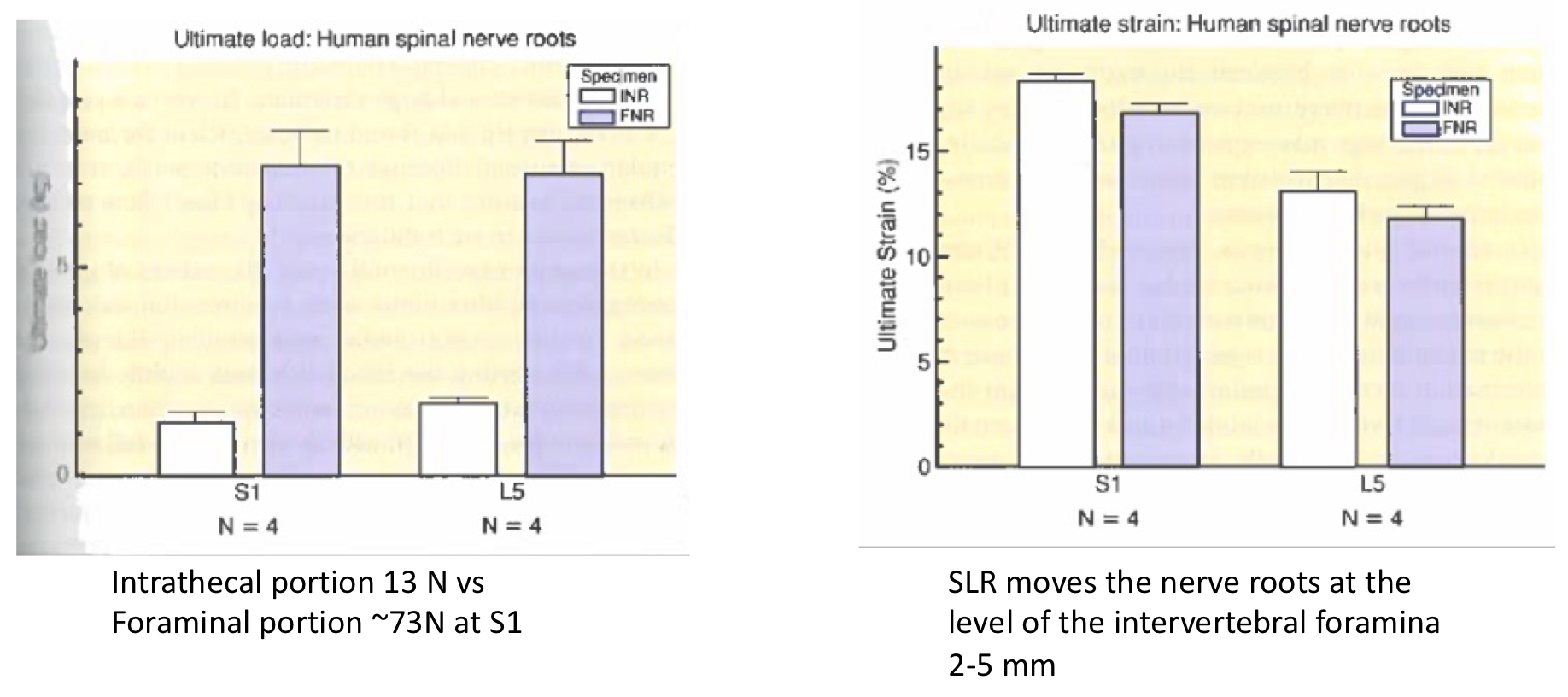
Is stress or strain more protected/resisted in spinal nerve roots?
Strain
What are some examples of nerve injuries?
Disc herniation
Local peripheral entrapments
Tension injuries (e.g., brachial plexus)
Neuropathy
What happens with disk herniation?
Unilateral compressive load → creates bending force
Tension → leads to vascular effects
With disc herniation, 5-10 mmmHg of pressure leads to…
Venous stasis (which has upstream effects on capillaries)
With disc herniation, compression will lead to _____ and ______ effects to the _____ axons first
With disc herniation, compression will lead to neural and vascular effects to the motor axons first
(may not notice the symptoms unless tested)
With disc herniation, faster onset rates of compression leads to…
More pronounced effects on
Edema formation
Methyl glucose transport
Impulse propagation
With disc herniation, compression of nerve roots causes an increase in what neurotransmitter?
Substance P (a neurotransmitter related to pain perception)
T/F: Lower/less compression (e.g. 10 mmHg) at multiple levels typically leads to greater impairments than higher compression (e.g., 50 mmHg) at one level
True!
(may be due to the fact that blood is impacted all the way between the areas of compression, from 10mm to 30mm)
What are the clinical signs and symptoms of nerve injury (both spinal or peripheral nerve)?
Paresthesia (pins and needles)
Pain
Numbness
Muscle weakness (motor nerves)
Is it likely that an individual will notice muscle weakness due to nerve injury?
Not likely until they notice the other symptoms (typically don’t even notice muscle weakness until doing testing)
T/F: Physiologic function of a nerve will fail first before the material of a nerve will
True!
Therefore we are more concerned with the sheaths and vascular supply
What is the most common clinical concern?
That the nerve needs to be able to slide during function
When a nerve is severed, what component of nerve is hard to “heal” or “regenerate”?
Hard to regenerate the conduction properties
→ when a nerve is severed, healing the soft tissue is not a problem (conduction is)
When considering treatment, what are we most concerned about and why?
More concerned with the sheaths and vascular supply
We are more concerned about this because physiological function of a nerve will fail first (before material itself)