Lecture 15 Ocular Manifestations of CNS
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Cranial Meneinges
-Dura Mater
-Arachnoid Mater
- Pia Mater
Dura mater
outer tough coating, large blood vessels, surround and supports dural venous sinuses, attached to skull
Arachnoid Mater
intermediate layer, trabeculae, cushions the CNS
Pia Mater
thin, delicate, vascularized
Ventricular System
a system of fluid-filled cavities inside the brain
lateral ventricles (2) ->Interventricular Foramina (2) -> 3rd Ventricle -> Cerebral Aqueduct -) 4th Ventricle -> Central Canal
Cerebrospinal fluid
produced by the choroid plexus in the ventricles
-Flows out of the 4th ventricle via smaller foramina into cisterns
-Cisterns communicate with subarachnoid space between arachnoid and pia mater
-CSF circulates in subarachnoid space and bathes CNS
-Exits via arachnoid granulations into dural venous sinuses
Increased Intracranial Pressure (ICP)
abnormal increased intracranial pressure (normal adult 10-15 mmHg)
cane be caused by head injury, cerebral edema, intracranial space occupying lesion, increased CSF production, obstruction, Decreased CSF absorption, venous outflow obstruction, brain herniation, and Idiopathic Intracranial Hypertension
Monroe-Kelli Hypothesis
if 1 of the 3 components inside the cranium increase in volume, the other 2 must decrease in volume
INCREASED ICP IS THE RESULT IF NOT!!
Idiopathic Intracranial Hypertension (IIH)
AKA Pseudotumor Cerebri
-chronic elevated intracranial pressure with no obvious cause
-Risk factors include overweight, biologically female and fertile
-CSF in subarachnoid compresses optic nerve and central retinal vessels leading to visual impairment
-signs and symptoms include: headache, papilledema, diplopia, nausea, vomiting, CN Palsies (CN VI), retrobulbar pain, photopsia, elevated pressure on lumbar puncture
papilledema
compression of optic nerve and retinal vessels crossing the subarachnoid space causes bilateral edema of the optic nerves
-typically presents with indistinct margins of the optic disc, engorged venous blood vessels, small peripapillary hemorrhages, and loss of spontaneous venous pulsation
-can cause enlarged blind spot in visual field
management of IIH
consult neurology and neurophthalmology
-get CT scan, MRI, lumbar puncture
-weight loss
-medications
Carbonic Anhydrase Inhibitors (Diamox) to decrease CSF production
Loop Diuretics (Furosemide) to decrease sodium reabsorption in Loop of Henle
-Surgery -Optic Nerve Sheath Fenestration
Increased Intracranial Pressure
abnormal increase intracranial pressure (Normal adult 10-15 mmHg)
-can be caused by head injury, cerebral edema, intracranial space occupying lesion (tumor, aneurysm, hemorrhage), increased CSF production, obstruction, decreased CSF absorption, venous outflow obstruction, brain herniation, idiopathic intracranial hypertension
Cranial Hematomas
bleeding inside of the cranium is a medical emergency!
-Commonly caused by trauma, hemorrhagic stroke, ruptured aneurysm
-Increased ICP results from hemorrhage, surrounding edema or hydrocephalus due to obstruction of CSF
-Three types: Epidural, Subdural, and Subarachnoid
- may affect vision causing diplopia, blurred vision, photophobia
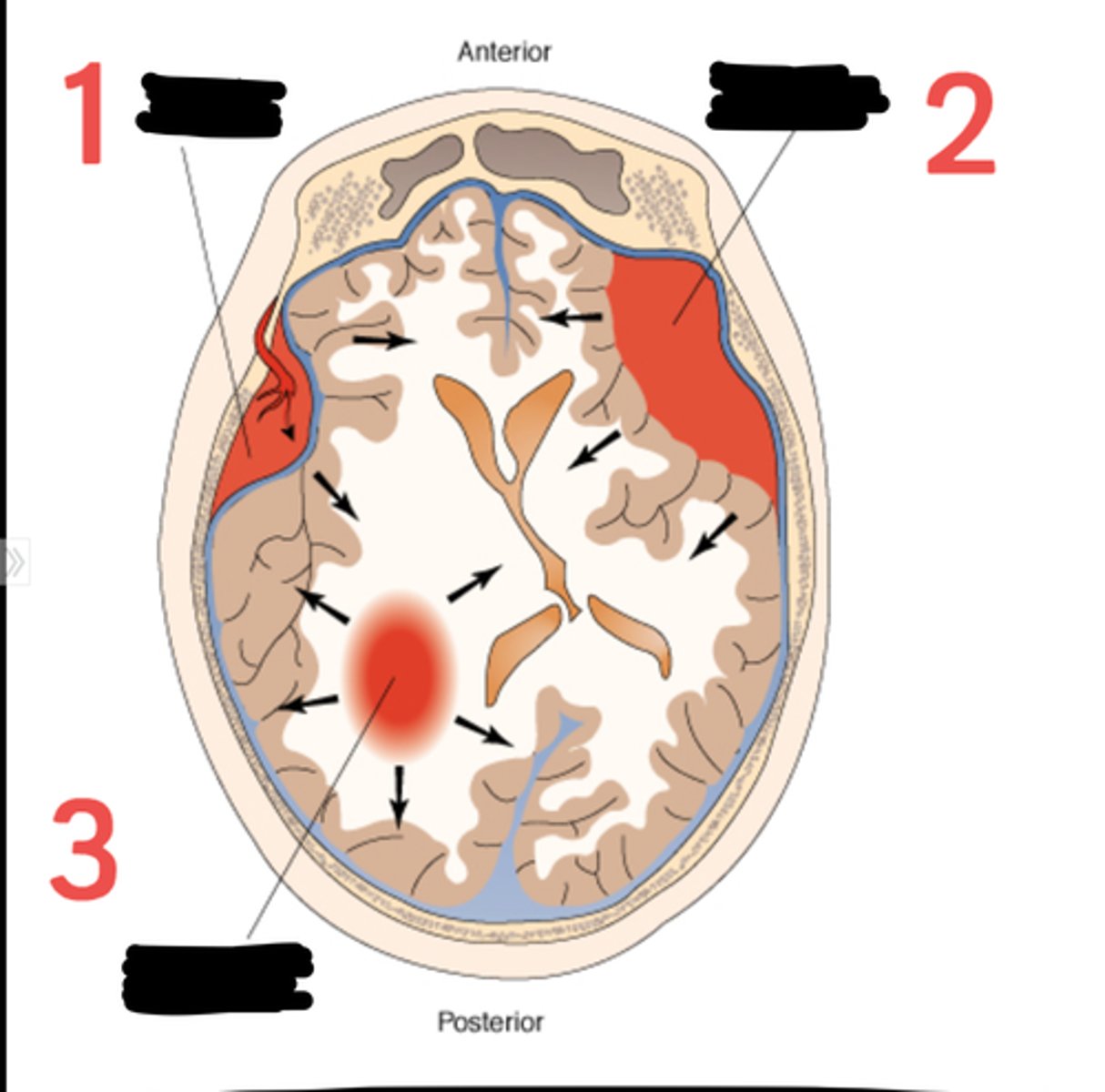
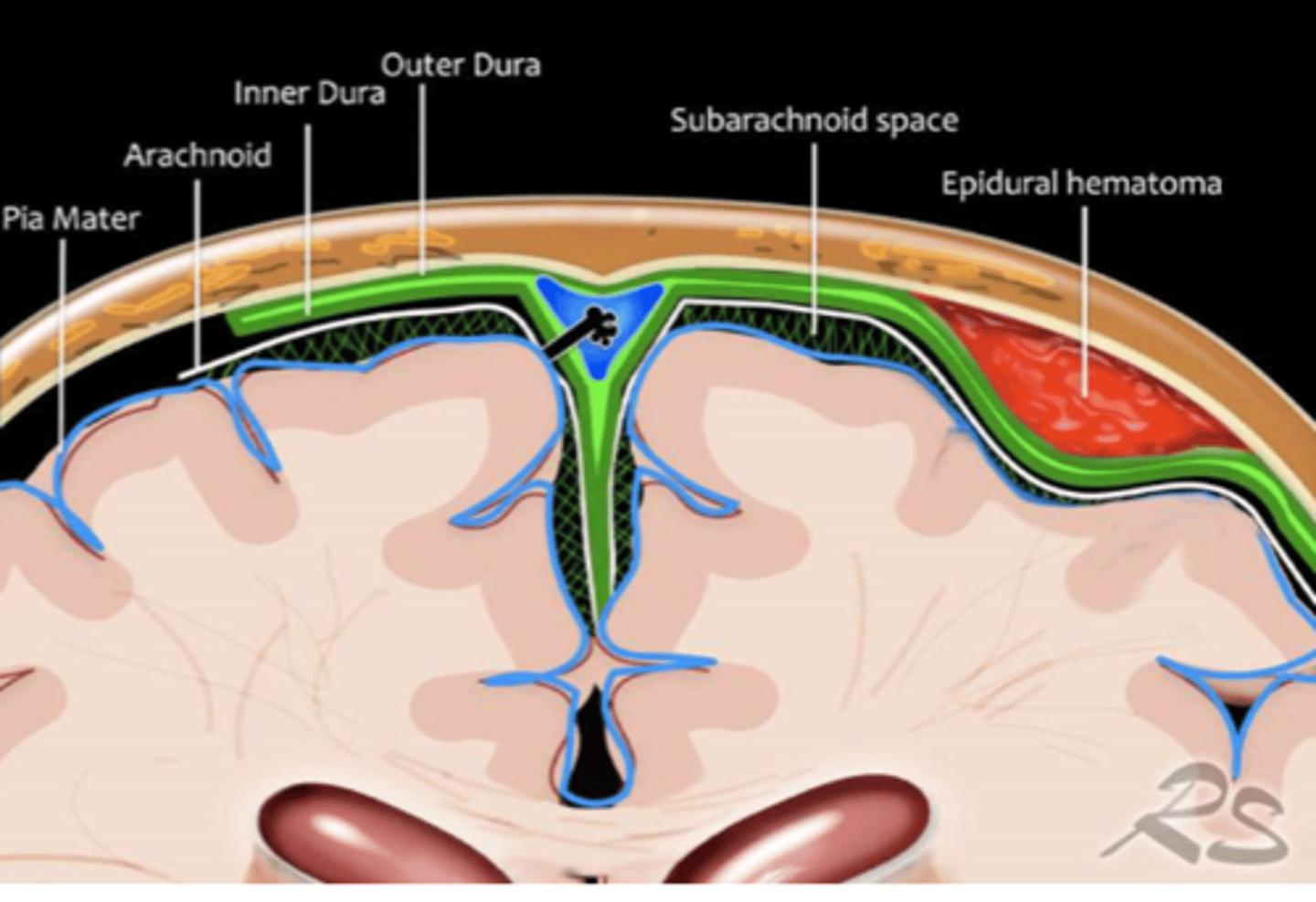
Epidural hematoma
bleeding in potential space between skull and dura matter
-often occurs with fracture of temporal bone with tearing of the middle meningeal artery
-appears convex lens-shaped on head imaging
-Lucid interval - initially symptoms, improves, deterioration
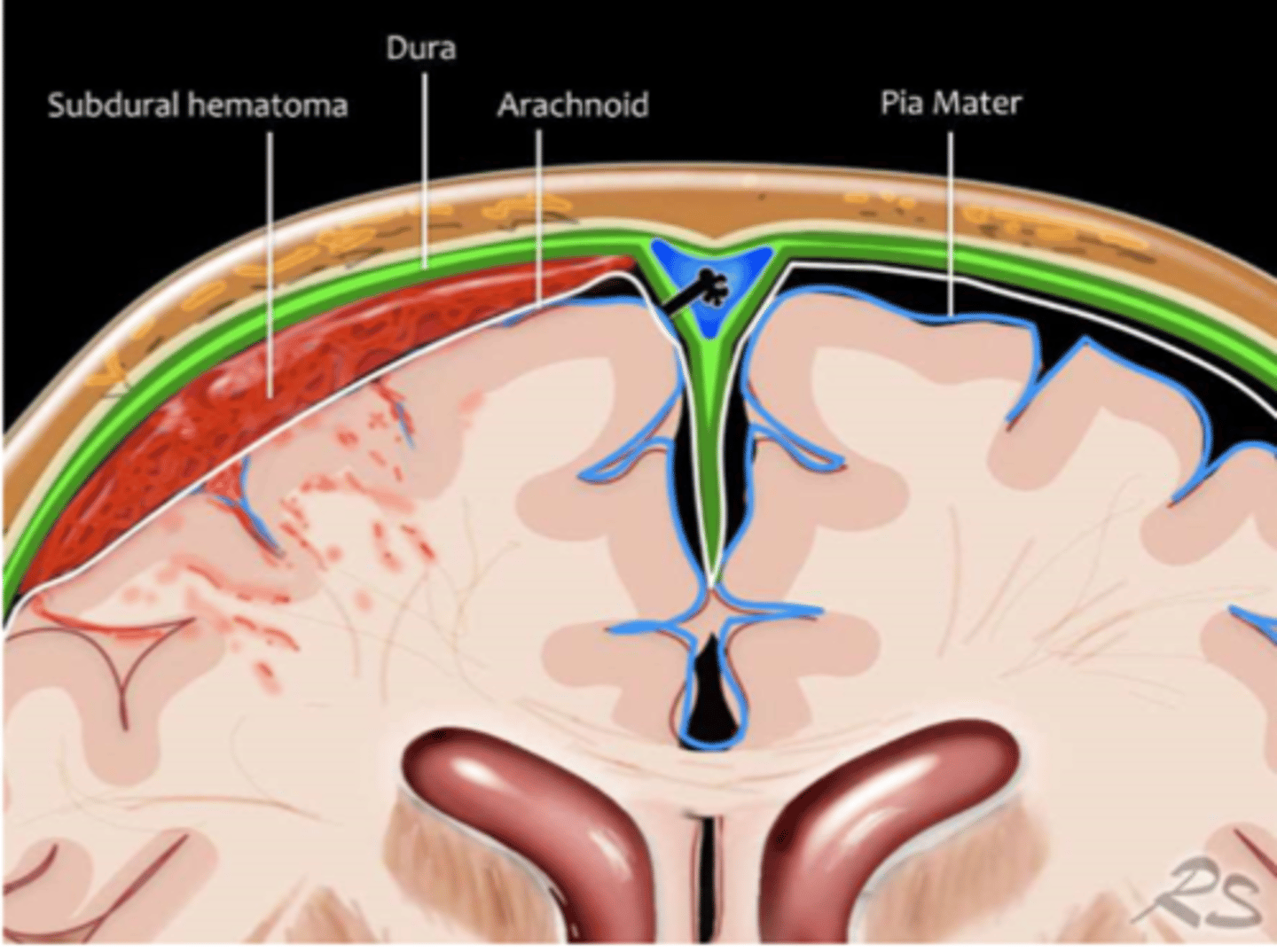
Subdural Hematoma
bleeding between inner layer of dura and arachnoid mater.
-Often occurs rupture of cortical bridging veins
--Head trauma, anticoagulants, elderly, alcoholics with brain atrophy
-Appears concaved, crescent-shaped on head imaging
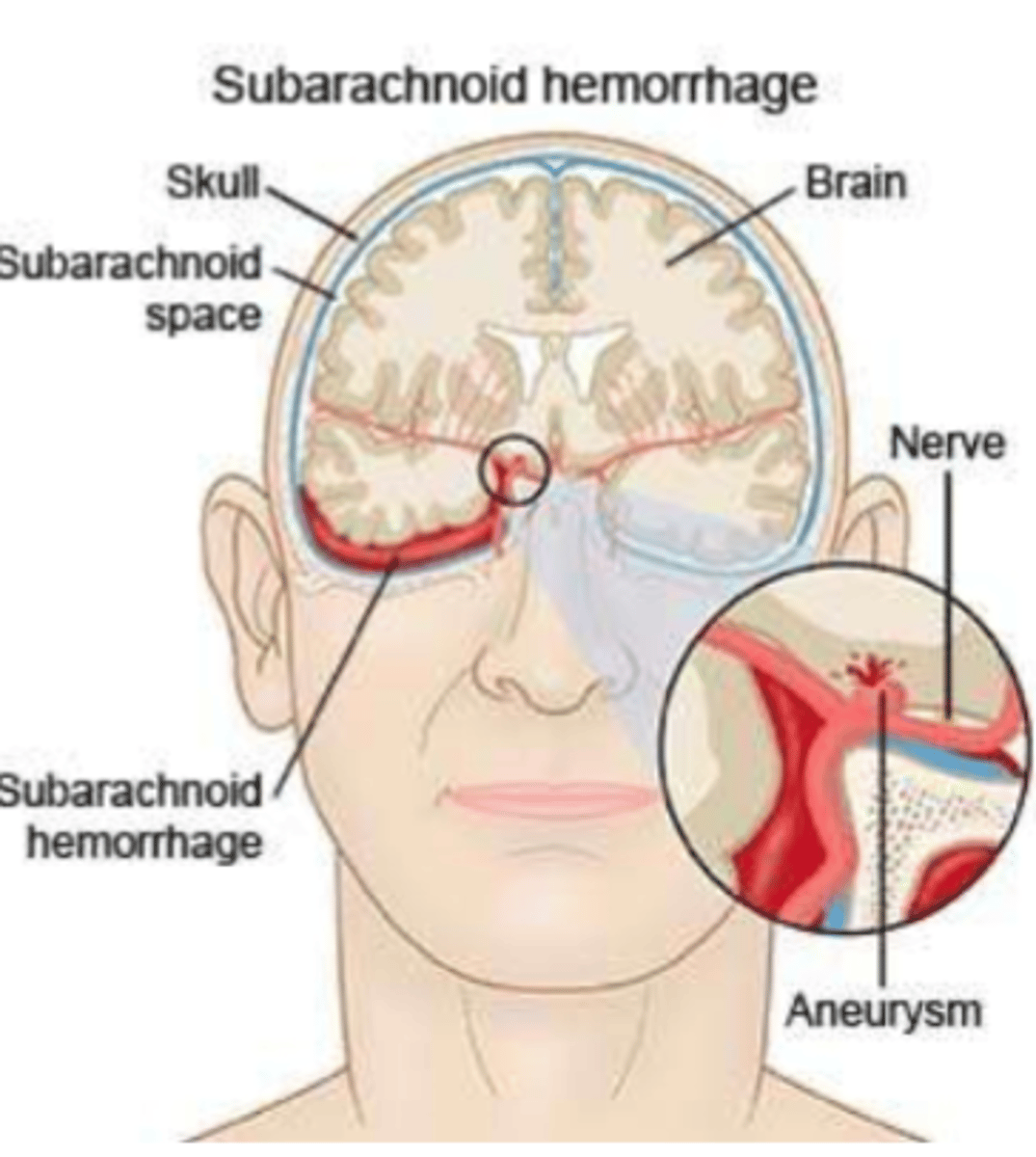
Subarachnoid Hemorrhage
acute bleeding under arachnoid mater. Often occurs rupture of aneurysm or trauma
Horner's Syndrome
disruption along the sympathetic pathway in the autonomic nervous system
-Causes include stroke, tumor, spinal cord injury, etc.
-Idiopathic
-Unknown in 35-40% of cases
-Children are at risk-injury to neck or shoulders during delivery is most common cause
-Unilaterally affects ipsilateral sympathetically innervated structures of the eye and face

manifestations of Horner's Syndrome
-Anisocoria - miosis on affected pupil, especially in dim illumination
-Hyperemia of Conjunctival blood vessels
-Ptosis of Upper Eyelid
-Ipsilateral dilation of facial vasculature (flush)
-Hemifacial Anhidrosis (absence of sweating)
Management of Horner's Syndrome
Acute Onset and Painful:
-Emergency Neurological Consult
Chronic/Congenital:
-management depends on cause
Multiple sclerosis
neurodegenerative disease of the CNS where T lymphocytes recognize myelin as foreign causing inflammation and demyelination of axons in white matter of CNS
-Risk factors include genetic predisposition and environmental factors (after post-viral syndromes) and women aged 15-45
onset of MS symptoms
-Motor or sensory, or visual onset
-75% of patients experience at least one episode of ocular involvement in the course of their disease
-Can affect afferent and efferent pathway of visual system
afferent pathway MS
sensory transmission from retina to the brain
-Optic nerve most commonly involved
efferent pathway MS
motor output to pupillary muscles and extraocular muscles
-Disorders of ocular movement will affect more than 40% of patients with MS
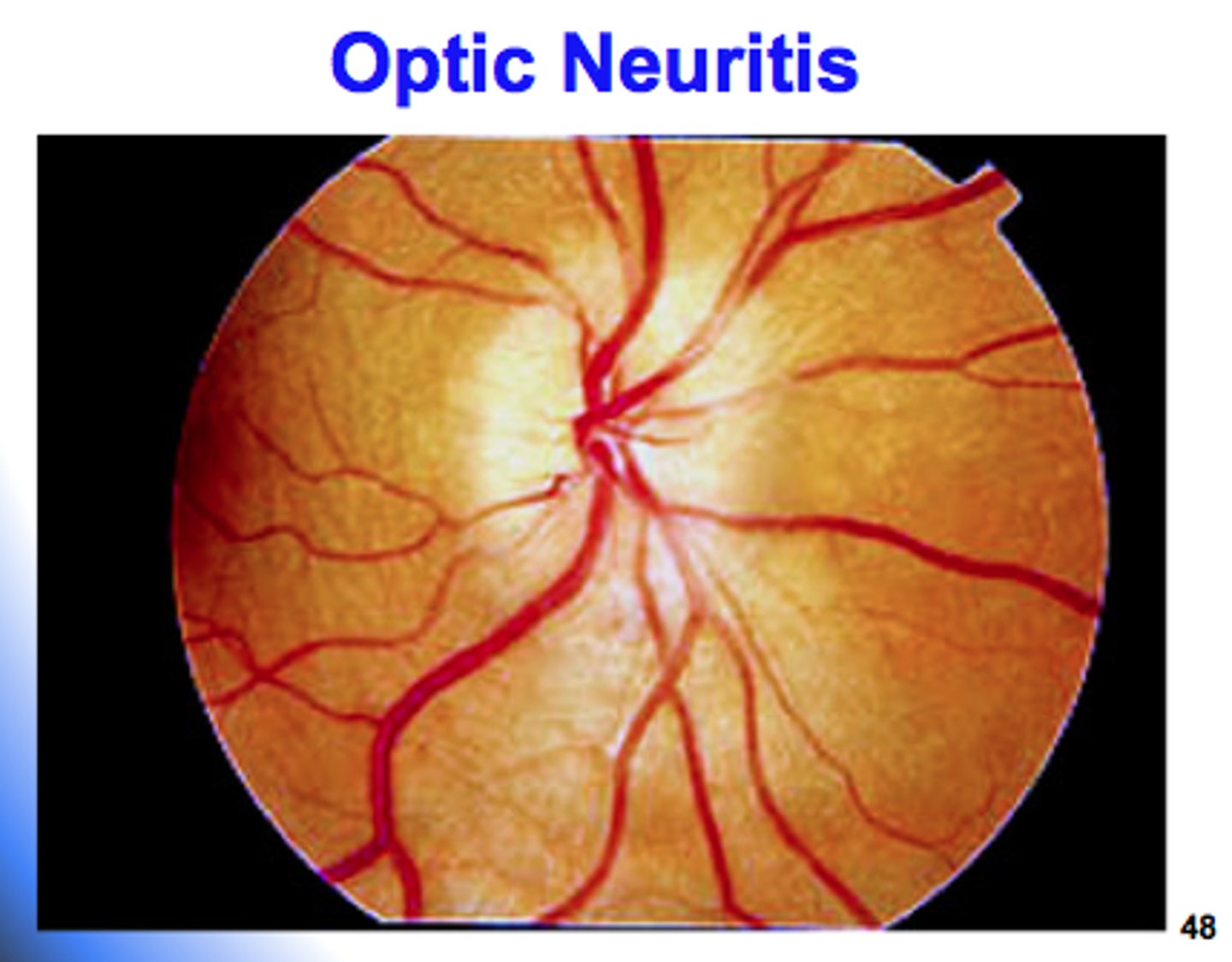
Optic Neuritis
monocular painful vision loss that occurs over hours to days and lasts a few weeks
-Changes in VA can range from mild to severe
-Orbital pain occurs in 92% of patients and usually worse with extraocular movement
-Visible optic disc swelling in 1/3 of patients
-Internuclear ophthalmoplegia occurs in about 30% of patients
related to MS
why is orbital pain from optic neuritis usually worse with extraocular movements?
superior and medial rectus muscles make attachments with the dural sheath that surrounds the optic nerve
-when the muscles contract, they tug on the dura surrounding the inflamed optic nerve and cause pain
MS diagnostics
MRI of the head and spin is performed to evaluate for these demyelinating plaques in the white matter of the brain and spinal cord
-OCT can aid in diagnosis of optic neuritis and MS and monitor progression
-Lumbar punctures can be performed for evaluation of the CSF
management and prognosis of MS
no cure
-30% of patients eventually require assistance for ambulation, and 22% become wheelchair bound
-Majority achieve 20/20 vision one year after and acute episode
-8% retain a VA worse than 20/40
The optic neuritis Treatment Trial (ONTT)
high-dose intravenous corticosteroids improves recovery time for visual function, contrast sensitivity and color vision, but have not been shown to improve final visual outcomes
acute optic neuritis
typically presents as monocular vision loss and eye pain
Uhtoff's Phenomena
temporary worsening of MS symptoms when your body's temperature is raised by fever, exercise, or using a hot tub or sauna
-A decrease in conduction velocity in response to an increase in temperature in MS patients