Total Joint Arthroplasty
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
most afflicted with arthritis
knee
OA
–Repetitive trauma causes cartilage to breakdown
–Synovial fluid increases
–Result is inflammation and mechanical failure
–Genetic predisposition
inflammatory arthritis
•Rheumatoid Arthritis: autoimmune d/o, symmetrical and polyarticular
•Psoriatic Arthritis
•Systemic Erythematous Lupus
•Ankylosing Spondylitis
inflammatory arthritis results in …
synovitis, joint effusion, warmth and painful erythema
Ankylosing Spondylitis
inflammatory autoimmune d/o effecting primarily the spine and SI jts, but also the limbs.
Can cause eventual fusion of the spine
xray findings of arthritis
–Narrowing of the joint space
–Subchondral sclerosis
–Osteophyte bone spurs
–Bone cysts
–Eburnation of bone
eburnation
ivory like appearance of bone in areas of cartilage erosion
RA lab findings
+ Rfactor and elevated ESR
psoriatic arthritis lab findings
Elevated ESR and HLAB27
AS lab findings
HLA B27
gouty arthritis lab findings
+ uric acid
joint aspirate should appear
clear and yellow
aspirate indic of lymes dz
yellow + PCR
cloudy pus aspirate
septic joint
joint aspirate look at
crystal
uric acid
color
Non-surgical Treatment Options arthritis
•Acetaminophen
•Non-steroidal anti-inflammatories (NSAIDS)
•Corticosteroids → Injections or pills
•Viscosupplements → Synvisc, Euflexa, Orthovisc, Hyalgan…
•Glucosamine/Chondroitin
Total Knee Replacement
•End surface of femur is replaced with metal
•End surface of tibia is replaced with metal
•Plastic liner is inserted between femur and tibia
•Patella is resurfaced with plastic
What is MIS?
•Minimally Invasive Surgery (MIS) is intended to reduce disruption and damage to the muscles and soft tissues.
•MIS techniques facilitate optimal healing and faster, easier rehabilitation in comparison to the standard total joint replacement.
incision in MIS TKR
•Shorter incision → 3-4 inch scar
anesthesia used for MIS TKR
Spinal anesthesia relaxes the muscles more consistently than general, thereby allowing easier exposure and decreased risk of tearing the muscle
benefit of MIS TKR
Quadriceps sparring → small snip in VMO only
how does pt benefit from MIS TKR
•Reduced blood loss
•Faster, easier rehab and return to function
•Faster return of quadriceps strength
•Permanently retains terminal quad strength better than standard TKR
•Better ROM post-op
•Shorter hospital stay
•Same day surgery for healthy pts
Unicompartmental Resurfacing indications
–Medial or lateral compartment disease
–No inflammatory disease
–Intact ACL
knee pain may be a problem of …
lumbar spine or referred pain from hip joint
Causes of Hip Arthritis
AVN
Trauma
Congenital hip dysplasia
Perthes Disease
SCFE
genetics
AVN common in pt with hx of..
corticosteroid, ETOH, trauma
congenital hip dysplasia
Abnormal femoral shaft/head angle, shallow acetabulum (ages 0-5)
Perthes disease
Blood flow to head temporarily stops, causing AVN (ages 5-10)
SCFE
Displaced epiphysis causes collapse of femoral head from AVN (ages 10-15)
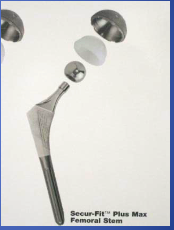
Total Hip Replacement
•Femoral head and neck are removed
•Acetabulum is reamed out and metalic cup is fit into the healthy bone
•Plastic liner is fit into the cup
•Metal stem is fit into the femoral canal
•New ball is placed on the femoral stem
•Joint is reduced: head put into the acetabular cup
Traditional Approaches total hip
posterior or lateral
incision of MIS THR
3-4” incision about 1/3 the size of the standard 8-12” incision
Direct Anterior Approach incision
3-4 inch incision
direct anterior approach hip surgery
•Muscles and tendons not detached from femur or pelvis
•No need for ‘THR Precautions’ or Restrictions of movement
Traditional THR Implant
•Metal cup is press fit into the acetabulum
•Plastic liner is locked into the metal cup
•Stem is press fit into the femoral canal
•Metal head is placed on top of the stem
Metal on Metal THR Implants
Cobalt-chrome surfaces
*Larger head=better mobility & less dislocations
Metallosis: wear leads to damage to bone/tissue & increased metal ions in the blood??
Ceramic on Ceramic Implants
Less debris and wear than metal
* Last longer
* Improved fluid properties
Rare but annoying squeaking
Hip Resurfacing
Head of pts OWN femur is capped with metal ball
*Cap is press fit into acetabulum
*More natural mobility
benefit of hip resurfacing
More natural mobility
Faster recovery
Good for younger patients
mcc of Ankle Arthritis
–OA, RA
–Post-traumatic
disadvantage of fusion for Ankle Arthritis
ALL motion is restricted
3 axis of motion of ankle
inversion/eversion
plantar and dorsiflexion
rotation
Total Ankle Replacement
allows relief of pain while maintaining motion
shoulder arthritis causes
–OA: h/o high intensity overhead activities
–RA
–Post-traumatic
–AVN
–Rotator Cuff Arthropathy
is shoulder arthritis common?
Not common bc it is a non-weightbearing joint
xray findings in shoulder arthritis
•Decreased joint space (loss of cartilage)
•Flattening and irregularity of bone
•Bone spurs
•Loose pieces of bone in the joint
Shoulder Hemiarthroplasty
Stemmed Hemiarthroplasty
Copeland Procedure
Total Shoulder Replacement
•Humeral head is removed
•Stem is press-fit or cemented into humeral shaft
•Polyethylene plastic is cemented to the glenoid
•Metal head is put on stem
•Joint is reduced
General Anesthesia
Controlled, reversible state of unconsciousness
4 meds General Anesthesia
amnesia, analgesia, muscle paralysis, and sedation
risk of general anesthesia
N/V, HA, Sore throat, delayed return to normal mental function
malignant hyperthermia
hereditary hypermetabolic d/o of skeletal muscle
hallmark signs malignant hyperthermia
masseter ms spasm, increased temp, rigidity and acidosis
Spinal/Epidural Anesthesia benefit
–Less blood loss
–Better pain control post-op
–Faster OOB & mental recovery
–Avoid risks of GA
Spinal/Epidural Anesthesia risk
–HOTN
–HA, seizure
–LBP, Nerve damage
–Infection
TJR Post-Op Complications
•Deep Vein Thrombosis (DVT)
•Pulmonary Embolus (PE)
•Nerve Injury
•Ileus
•Infection
•Delayed wound healing
•Joint instability
•Peri-prosthetic fracture
•Heterotopic ossification
Deep Vein Thrombosis sx
–Edema, pain, erythema and/or warmth in the limb
–Limb fatigue
–Low grade fever, diaphoresis
–Tachycardia
•May be asymptomatic!
which surgery increased risk of DVT
THR > TKR
test to dx DVT
Doppler US, Venography, MRI
DVT Prophylaxis
•Pneumatic Foot Pumps
•Early mobility
•meds
meds used for DVT prophylaxis - ASA
Inhibit Platelets and COX 1
immediate onset, no monitoring needed
meds used for DVT prophylaxis - warfarin
inhibit vit K
therapeutic 48-72 hours, requires monitoring blood PT/INR
meds used for DVT prophylaxis - Dabigatran (Pradaxa) and LMWH
inhibit thrombin
–Dabigatran (Pradaxa) – oral
–LMW Heparin (Fragmin) (Lovenox) – SQ , immediate onset
meds used for DVT prophylaxis - X inhibitor
Fixed dose, no blood monitoring
–Rivaroxaban (Xarelto) - oral
–Apixaban (Eliquis) - oral
–Edoxaban (Savaysa) - oral
–Fondaparinux (Arixtra) - SQ
PE sx
–Dyspnea, tachypnea, hypoxia
–Pleuritic chest pain
–Tachycardia
–Change of mental status
PE test
–Venthilation/Perfusion (VQ) Scan
–Helical CT
–Pulmonary Angiogram: gives definitive diagnosis
gold standard dx of PE
angiogram
Nerve Injury/Palsy
•Trauma from retractors or saw
•Traction injury from excessive tension or position of limb
Thermal injury from cement
common nerve injury with THR
sciatic nerve
common nerve injury with TKF
peroneal nerve
common nerve injury with TSR
axillary and radial nerve
Ileus sx
–Abdominal distention
–Nausea/vomiting
–Hypoactive/absent bowel sounds
tx ileus
–NPO, NG tube
–Usually self-limiting
mcc of Ileus
•Due to a combination of narcotics, immobility and anesthesia
ileus
functional obstruction of the intestine due to inactivity and/or paralysis of the intestinal muscles
Rf for Infection &Delayed Wound Healing
–DM, RA, immunosuppressed, steroids
–h/o prior sx or h/o prior infection
prevention of infection
pre & post-op Abx
If Infection suspected post surgery…
aspirate and get culture BEFORE Abx are given
synovial fluid anaylsis
–Cell count with diff
–Aerobic/anaerobic cultures
–Gram Stain
–Fungal & AFB
Peri-prosthetic Fractures
•Can occur early, after a fall, or decades late
•Pain with weight bearing activities during the post-op period is NOT normal!
Order an x-ray!
Heterotopic Ossification
formation of lamellar bone inside soft tissue where it shouldn’t exist
•STIFF Post-Op PATIENTS DESPITE THERAPY, MEDS, and WORK!!!
RF for Heterotopic Ossification
co-morbidities such as Ankylosing Spondylolitis, RA, Diffuse idiopathic Sketetal hyperostosis (DISH), Pagets, Quadraplegia or Paraplegia, or TBI.
mc joint affected by Heterotopic Ossification
hip