Exam 3 Phys - Pulmonology
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
179 Terms
What will happen when we administer a B2 adrenergic agent?
- bronchiolar SM relaxation
- mimicking the effects of the SNS
What will happen when we administer methacholine, a non-selective muscarinic receptor agonist?
- mimics the effects of the PNS action on bronchiolar smooth muscle
- causes bronchial constriction
What will happen as we administer epinephrine?
- vasoconstriction
- bronchiole dilation
What is FEV?
- Forced expiratory volume
- The amount of air someone can force out of their lungs in 1 minute
What are the 3 concepts that lay the foundation for understanding how the respiratory system works?
1. respiratory system is lined by a mucous membrane
2. covered by serous membrane
3. there are constant forces acting on the lung and chest wall
Gas exchange in the lungs is related to what principle?
Diffusion
(high --> low pressure)
Where should we expect to find mucous membranes?
lining all body cavities that are open to the exterior
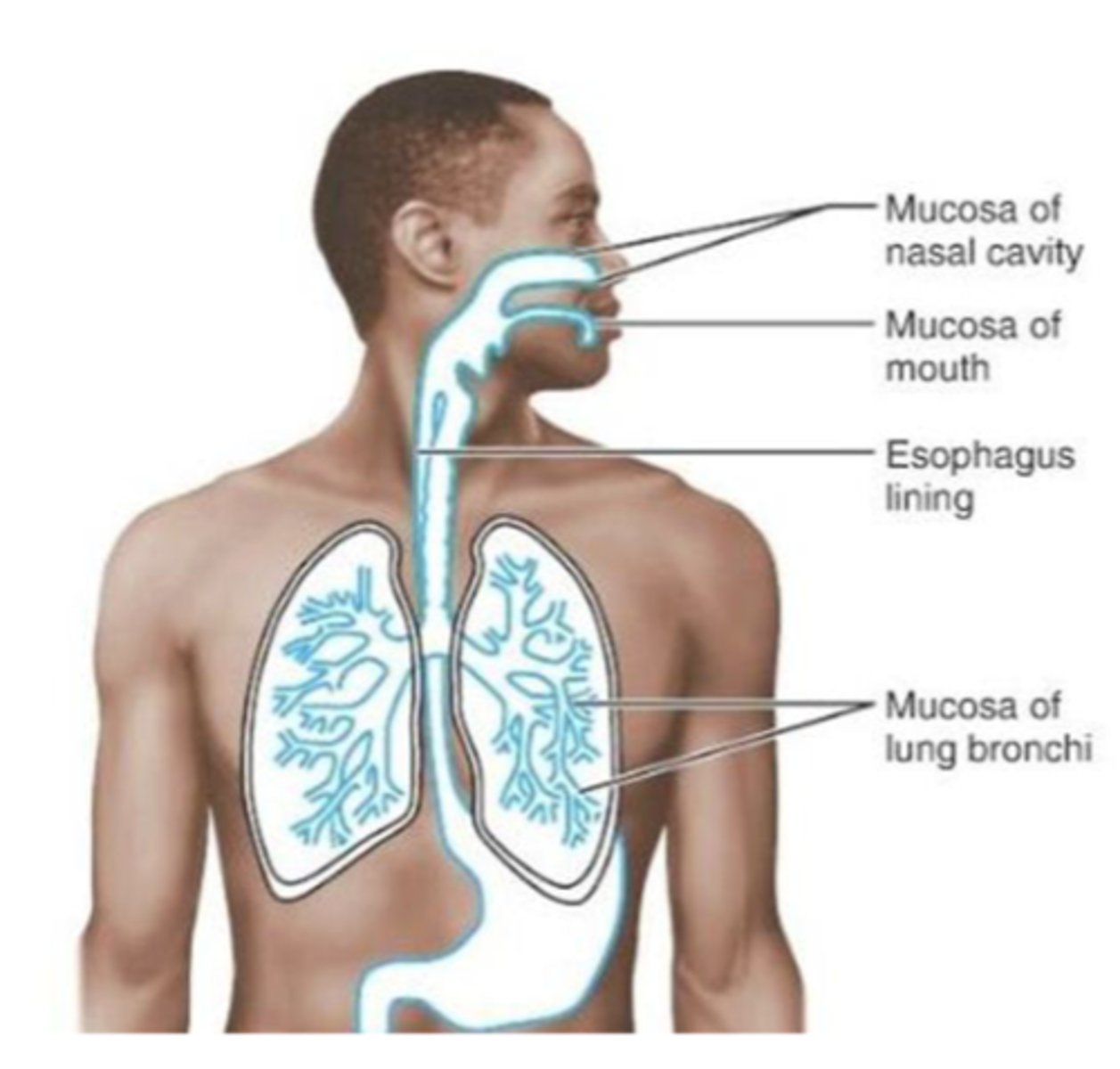
What are mucous membranes composed of?
- epithelial tissue + basement membrane
- underlying connective tissue
- flat cells for gas exchange
- B cells, T cells, and macrophages are found here for quick responses to outside factors
What type of cell is responsible for secreting mucous?
Goblet cells
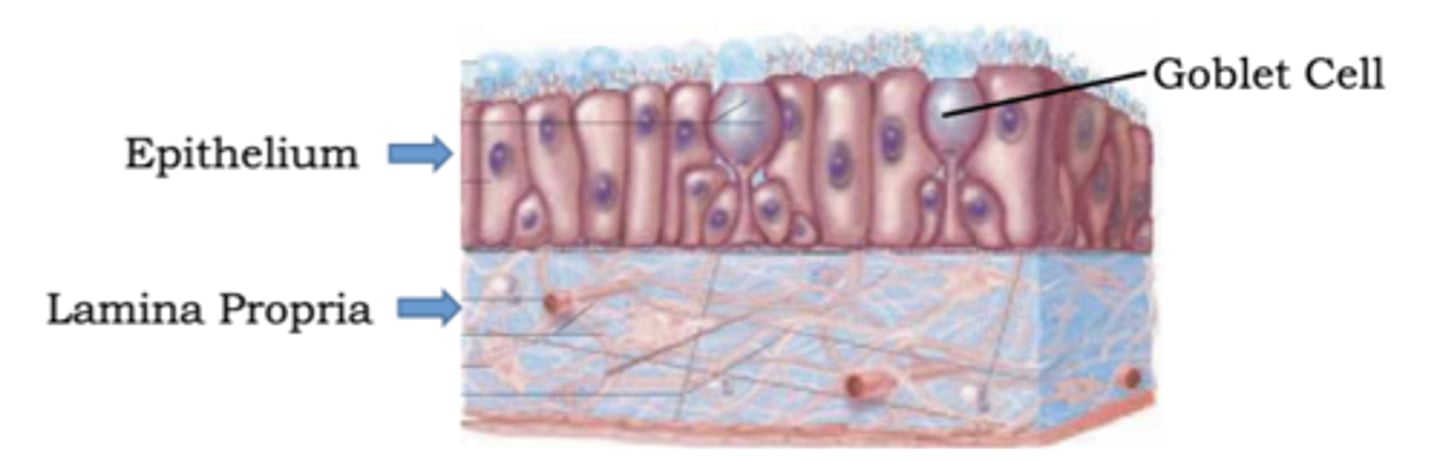
Identify the characteristics of the underlying connective tissue we see in respiratory mucous membranes:
- lamina propria (loose tissue)
- vascularized
- contains lymphatic tissue (MALT)
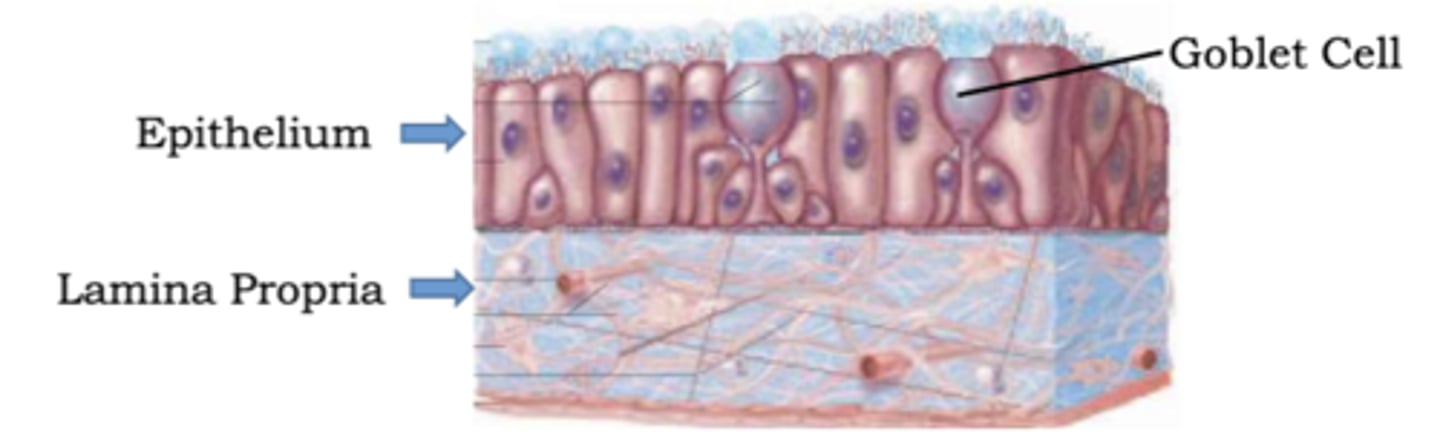
What does mucous do in the respiratory tract?
- moistens and keeps airway humidified
- functions as part of innate immune system
What is the serous membrane in the respiratory system? (covering)
Epithelial tissue + basement membrane that secretes a watery fluid.
What are the 2 layers of the serous membrane?
- parietal pleura
- visceral pleura
Which type of serous membrane adheres to the lung?
Visceral pleura
Where can we expect to find parietal pleura in the thorax?
From the 1st rib (superiorly) to just above the costal margin (inferiorly).
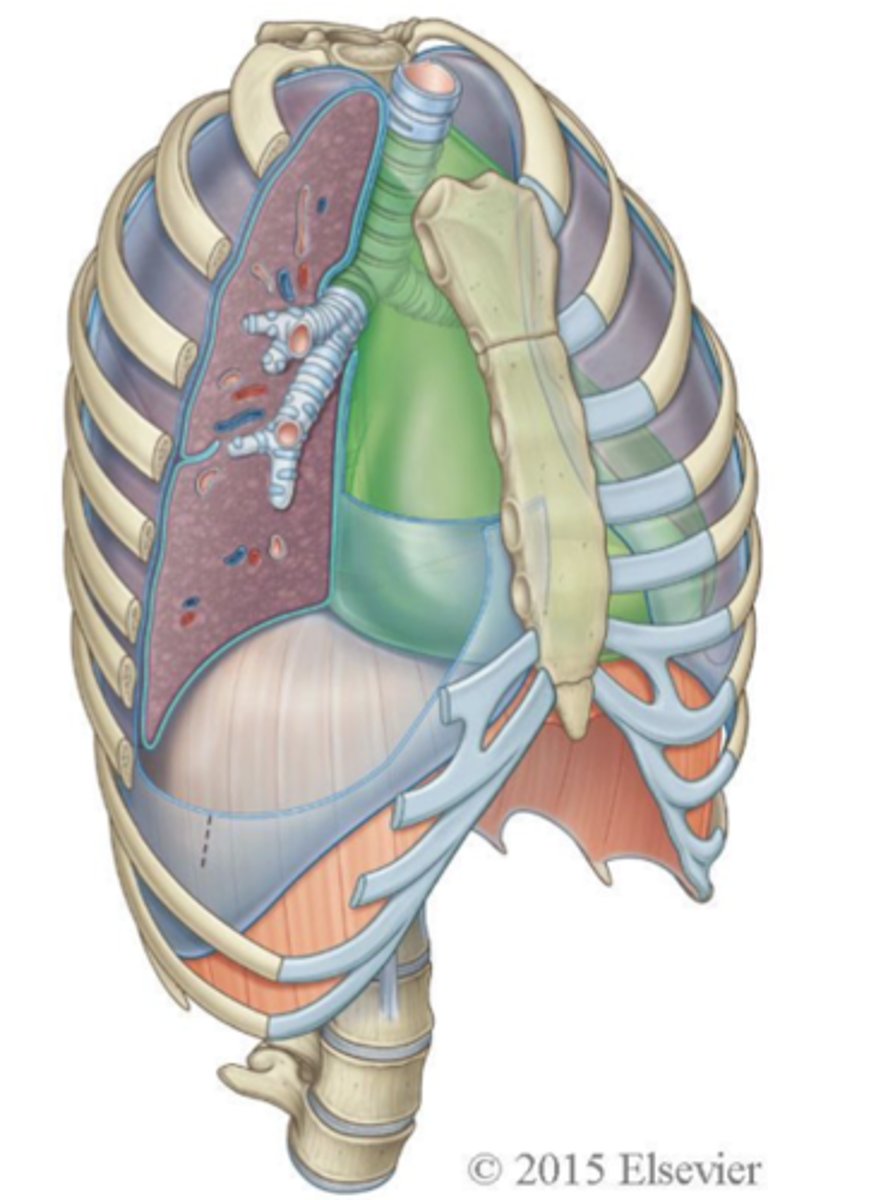
What are the 4 parts of parietal pleura?
- costal
- diaphragmatic
- mediastinal
- cervical
Which "cavity" in the thorax can be considered a potential space that expands with excess air and fluid?
Pleural cavity
In what direction will skeletal muscles pull on the ribs to expand the lungs?
Outward pull (expansion)
Exhalation is considered what type of process?
Passive process.
How are the lung and chest walls held together?
Through the water pressure between the parietal and visceral layers.
Why is it important to know that the alveoli have elastic fibers in their wall?
Elastic tissue wants to recoil, which endorses an inward pull.
What does it mean to say that the lungs are compliant?
The lungs expand and contract the way they are supposed to.
(scarring, paralysis, etc. make the lungs noncompliant)
What 2 things should a clinician always consider when working on the lungs & chest wall?
- forces at work
- compliance of the lungs and chest wall
What are the components of the upper respiratory tract?
- Nose
- Sinuses
- Pharynx (naso, oro, laryngopharynx)
- Larynx
What is the function of the external nares (nostrils)?
Entrance for air into nasal cavity.
The lateral wall nasal cavity contains 3 pairs of nasal conchae:
- Superior
- Middle
- Inferior
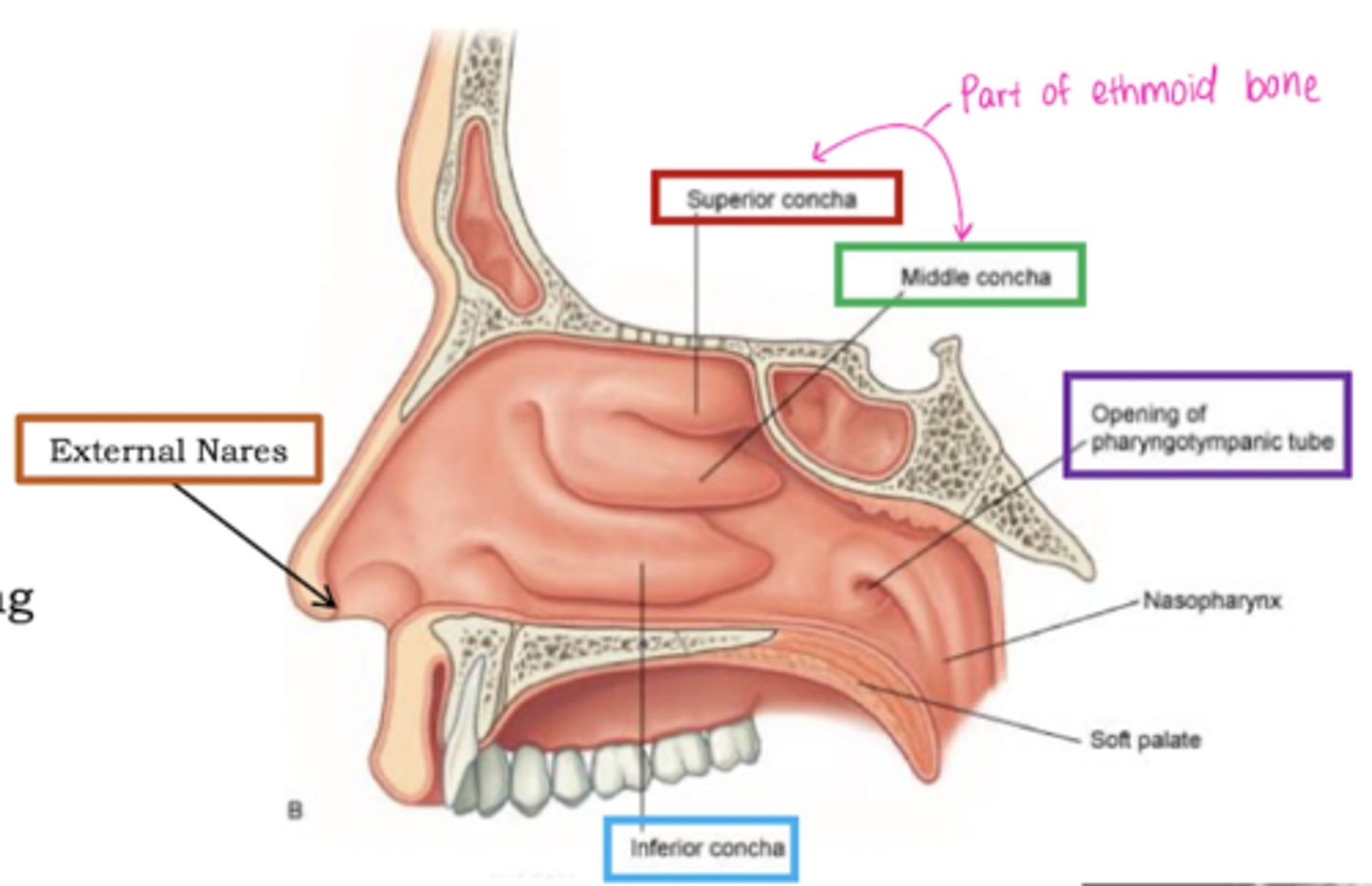
What do nasal conchae do?
- Create turbulence of the air entering the nasal cavity
- Air swirls through the nasal meatuses
- Aids in warming of air
- Removal of particulate material
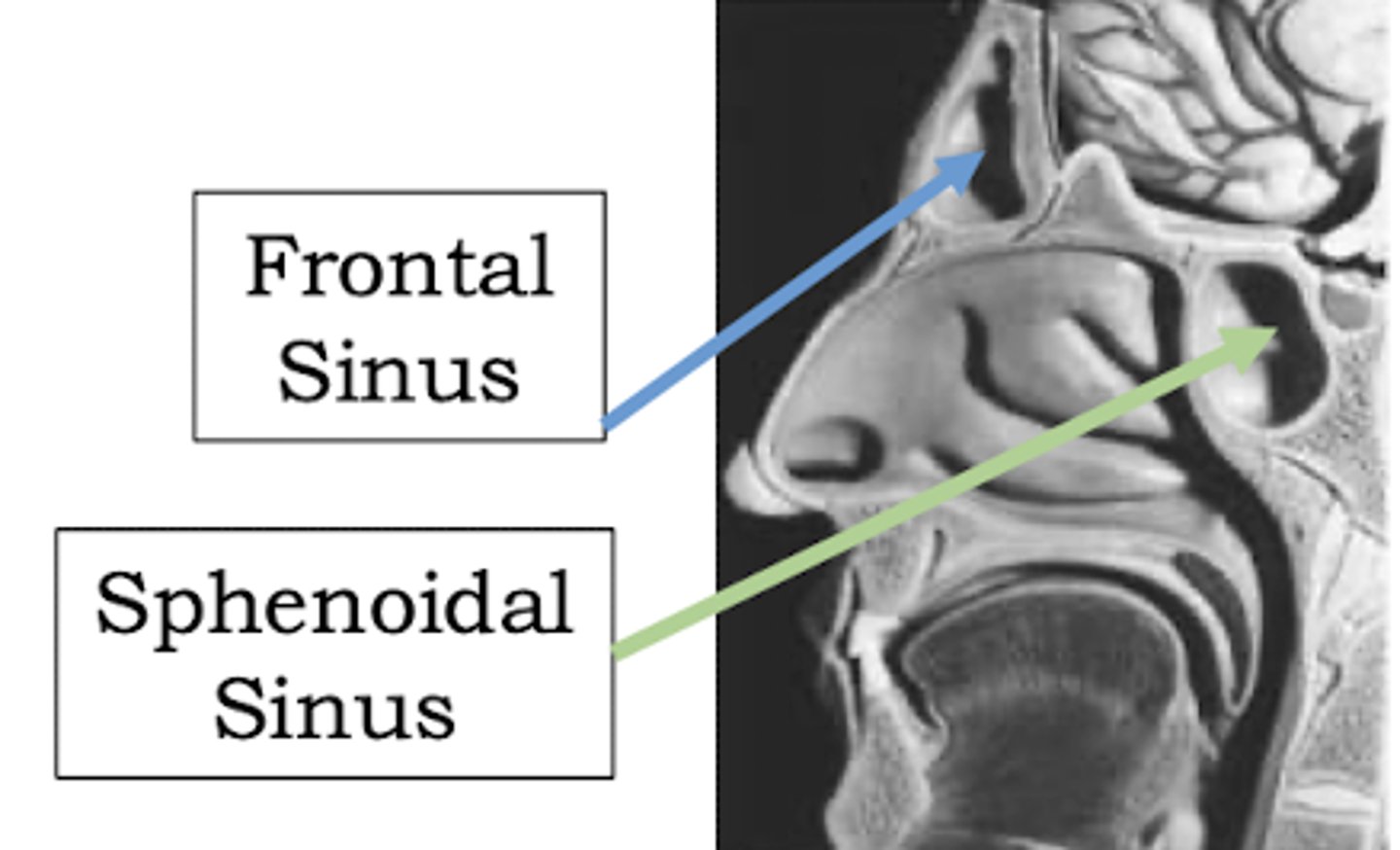
What are the 4 "mucosa lined" sinuses?
- Frontal
- Sphenoidal
- Ethmoidal
- Maxillary
Where does the nasopharynx extend?
From the base of the skull to the soft palate.
The nasopharynx is a passageway for _____ only.
Air.
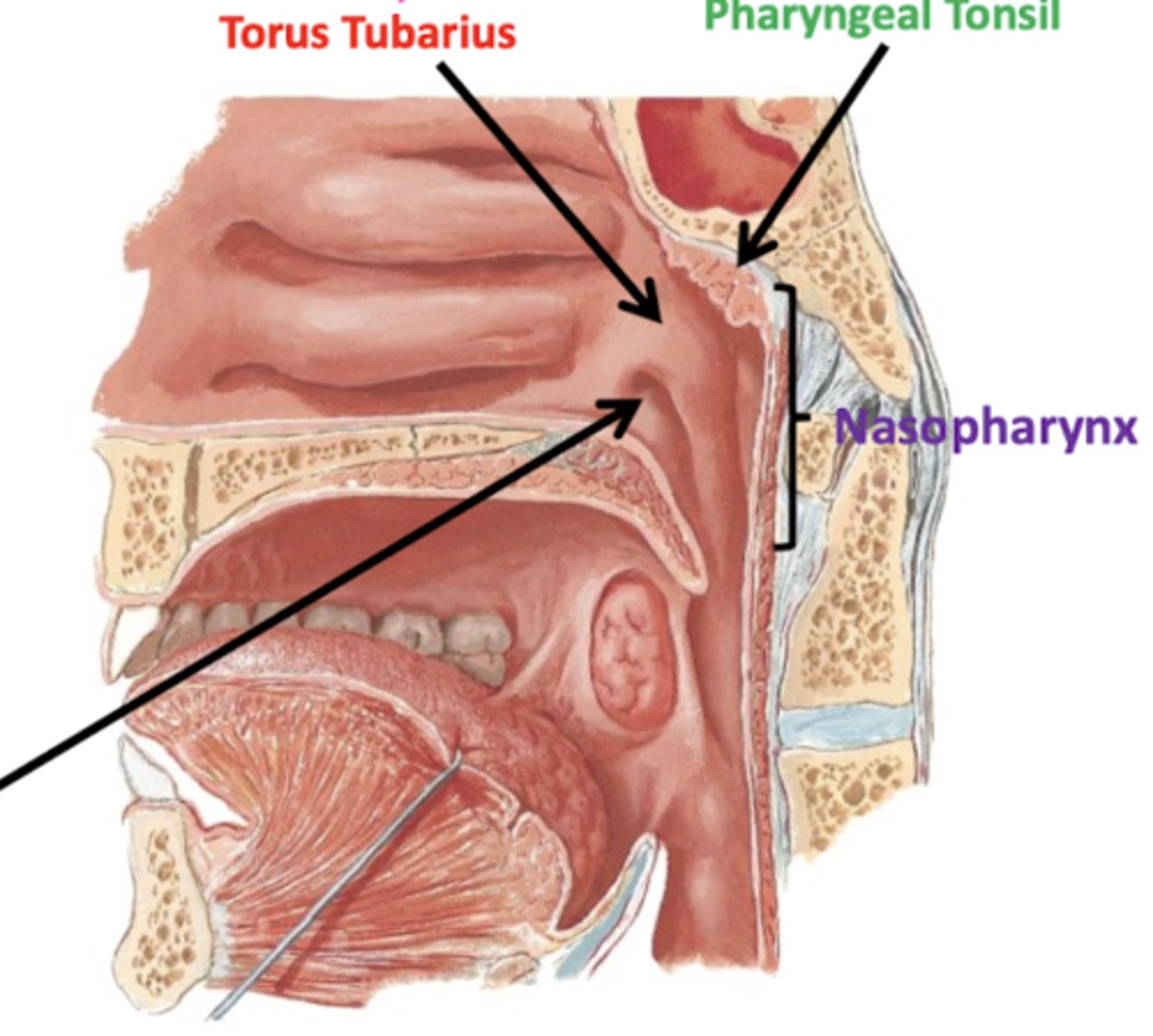
What are the 5 openings of the nasopharynx?
- 2 nostrils
- Mouth
- 2 Eustachian tubes (opening of auditory tube)
Where are the pharyngeal tonsils located?
Posterior wall of the pharynx (called adenoids if enlarged)
What is the torus tubarius?
An elevation formed from the auditory tube.
Where does the oropharynx extend?
- Lies posterior to the oral cavity.
- From the soft palate to the tip of epiglottis.
When might the oropharynx be deemed "clinically important"?
Throat cancer (blocked airway).
The oropharynx serves which functions?
Respiratory and digestive.
Which tonsils are contained in the oropharynx?
- Palatine
- Lingual
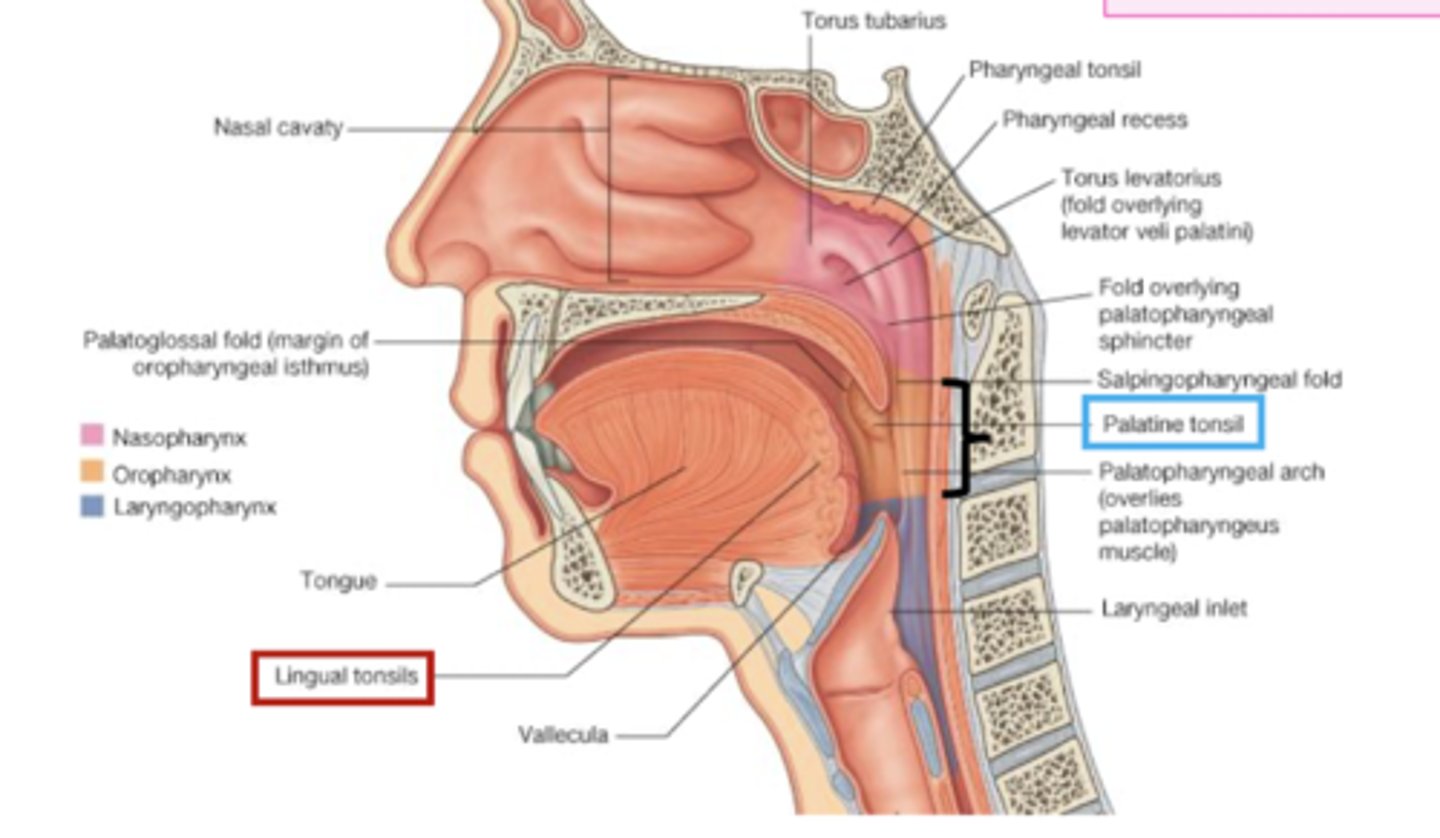
Where does the laryngopharynx extend?
From the tip of epiglottis to superior esophagus (C6 level)/inferior border of cricoid cartilage.
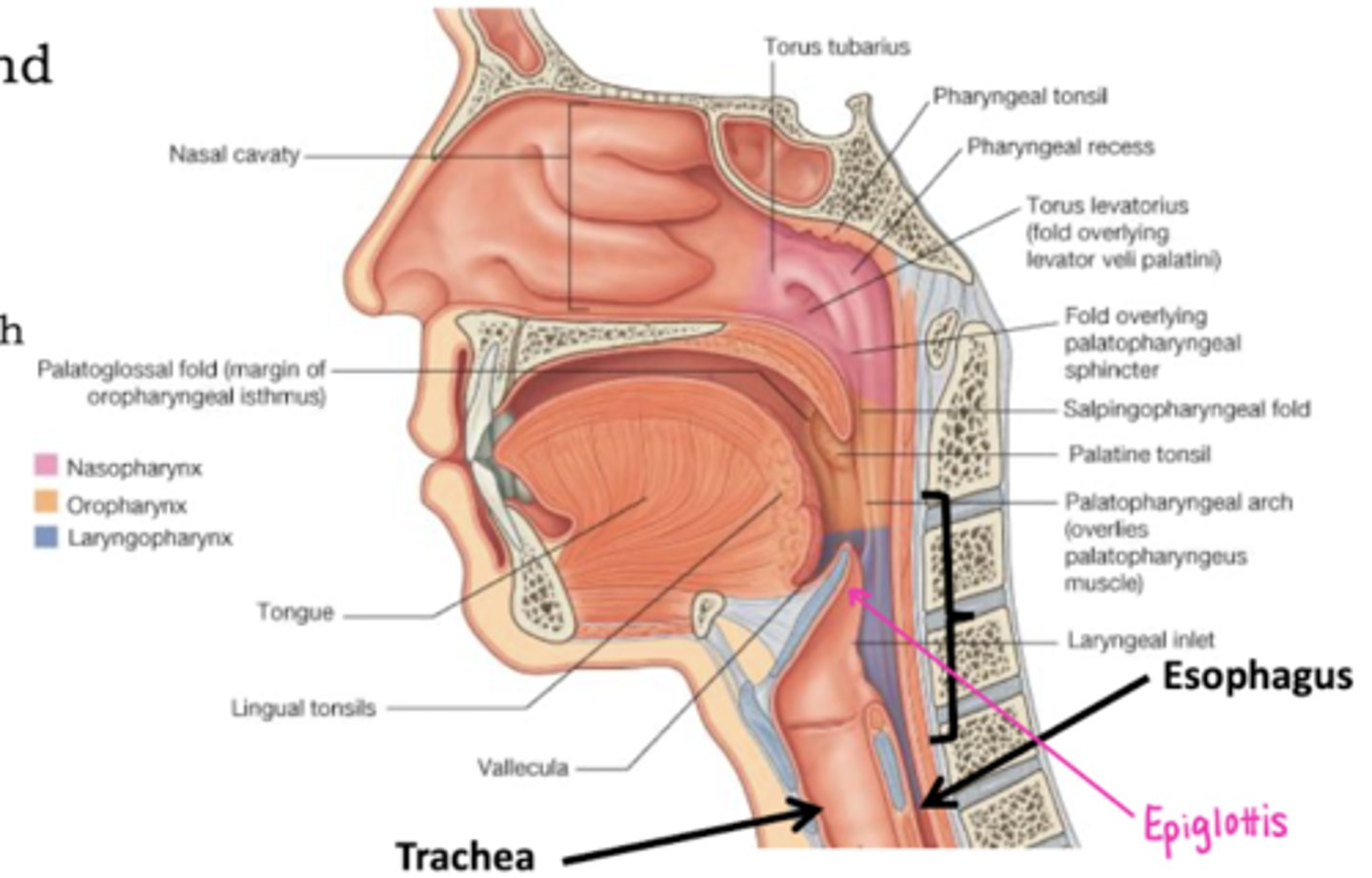
The laryngopharynx is a passageway for:
Air and food.
The laryngopharynx is continuous with:
Both the esophagus and larynx.
What may be an important "clinical connection" with the laryngopharynx?
Endotracheal intubation
(blade of the laryngoscope is advanced through the laryngopharynx).
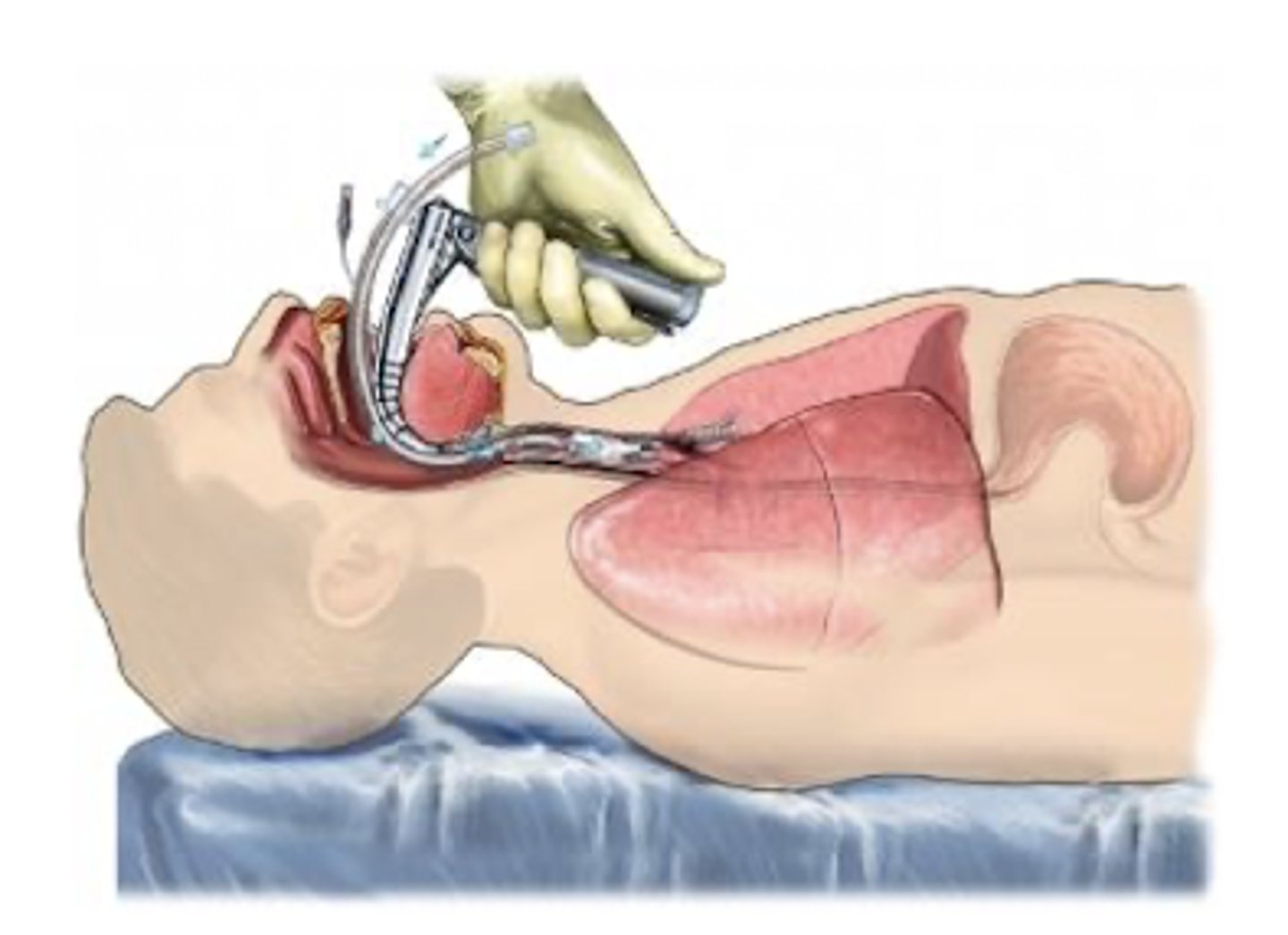
Which respiratory structure represents the interface between the upper respiratory tract and the lower respiratory tract?
Larynx.
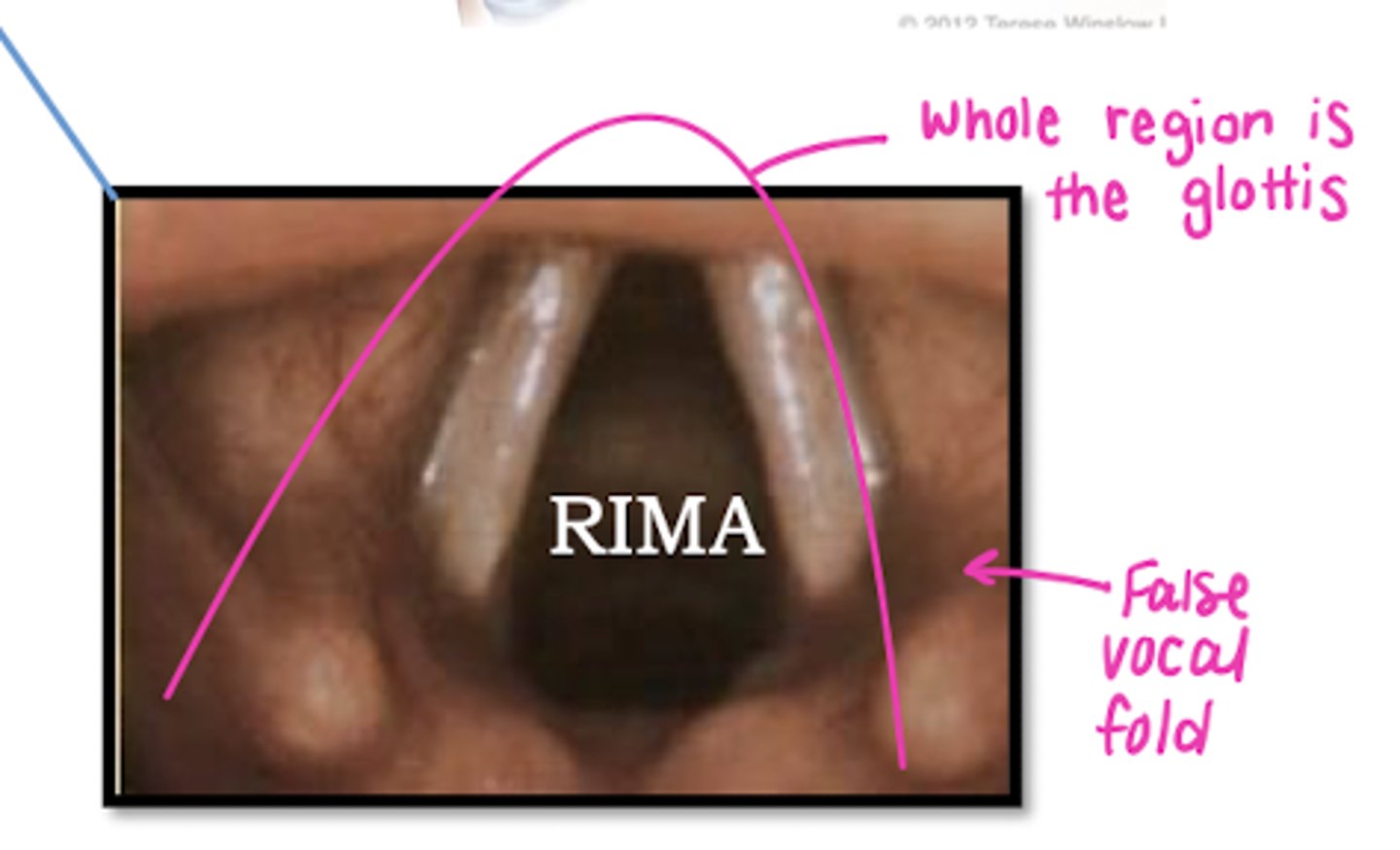
The larynx consists of which structures?
- Epiglottis
-Thyroid cartilage
- Cricoid cartilage
- Glottis (rima glottidis & true/false vocal cords)
Which cartilage is responsible for keeping the airway open?
Thyroid cartilage.
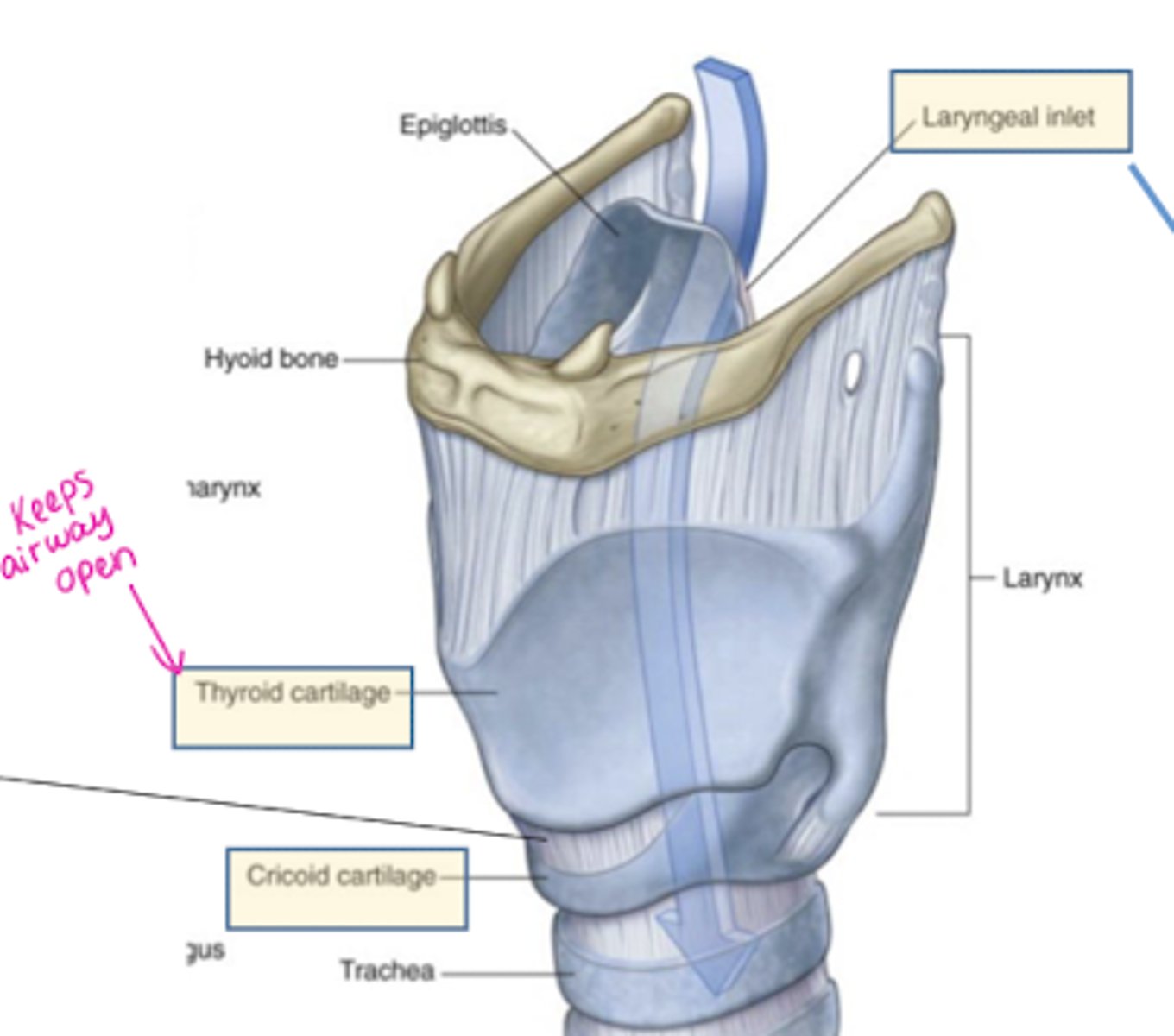
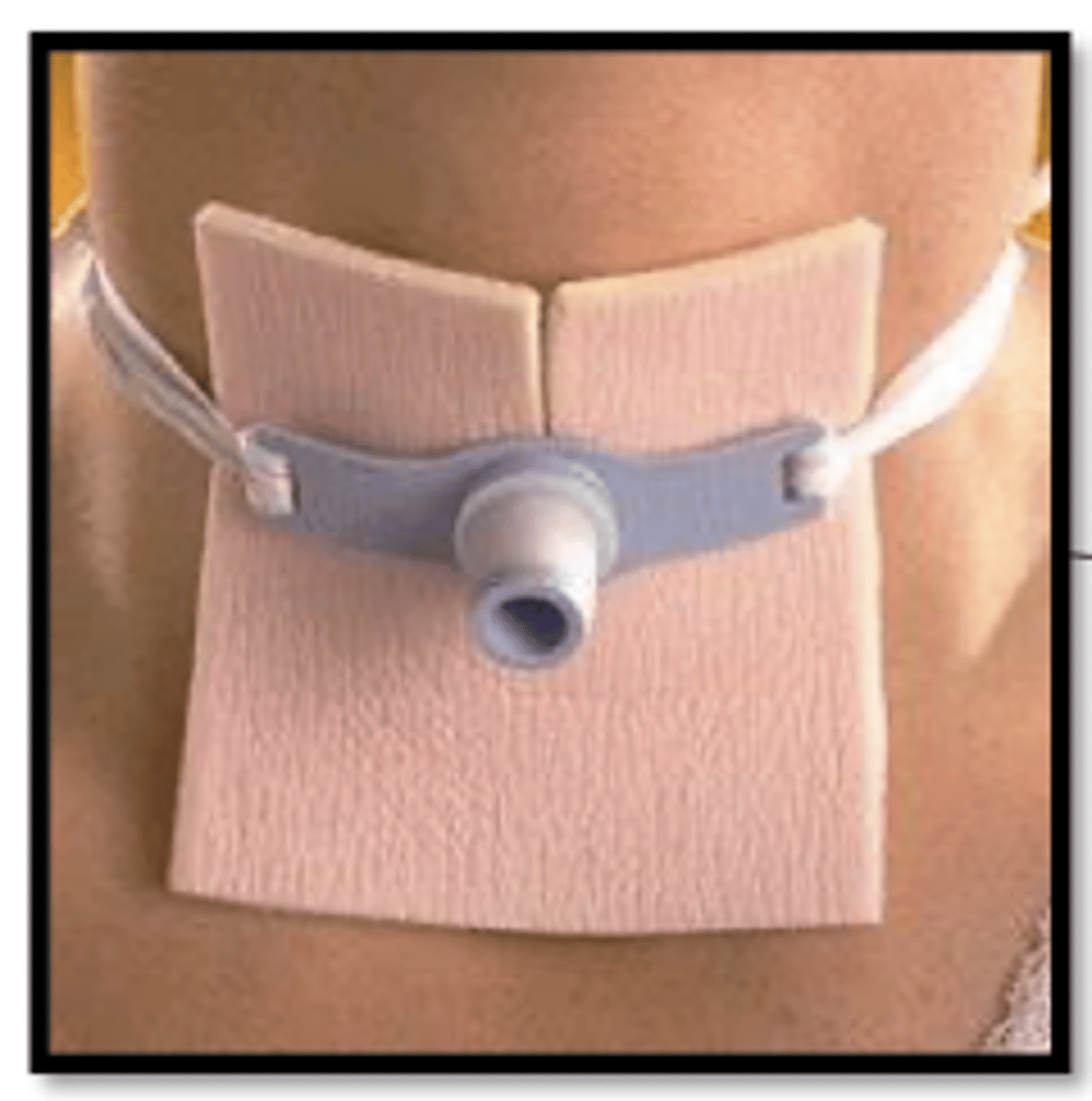
Where would a tracheostomy be placed?
In the cricothyroid ligament (between the thyroid & cricoid cartilage).
What is the function of the epiglottis in the larynx?
Covers laryngeal inlet during swallowing.
What are the parts of the lower respiratory tract?
- Trachea
- Bronchi (1, 2, 3)
- Bronchioles (terminal, respiratory)
- Respiratory unit
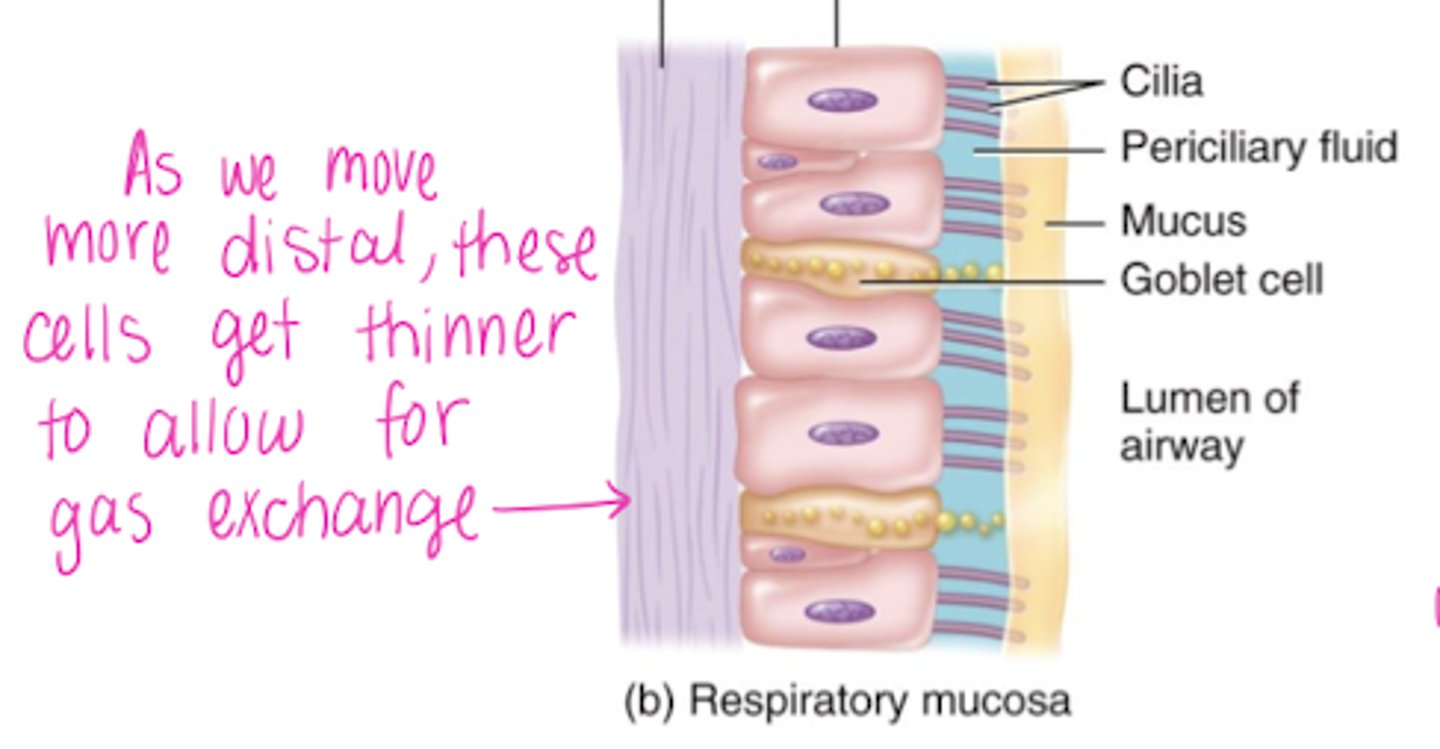
The nasopharynx, laryngopharynx, trachea, primary bronchi and secondary bronchi are all lined with:
Pseudostratified (ciliated) columnar epithelium with goblet cells dispersed throughout the tissue.
What are the "3 important changes" that take place as you move down the bronchial tree?
- Cartilage rings decrease
- Smooth muscle increases
- "Height" of the epithelium decreases
The bifurcation of bronchial tree is called the _______.
Carina.
What effect does chronic smoking have on the respiratory cilia?
It paralyzes them, which prevents normal mucous excretion (by they have a bad cough).
The trachea aligns with which vertebrae?
C7 - T4/5
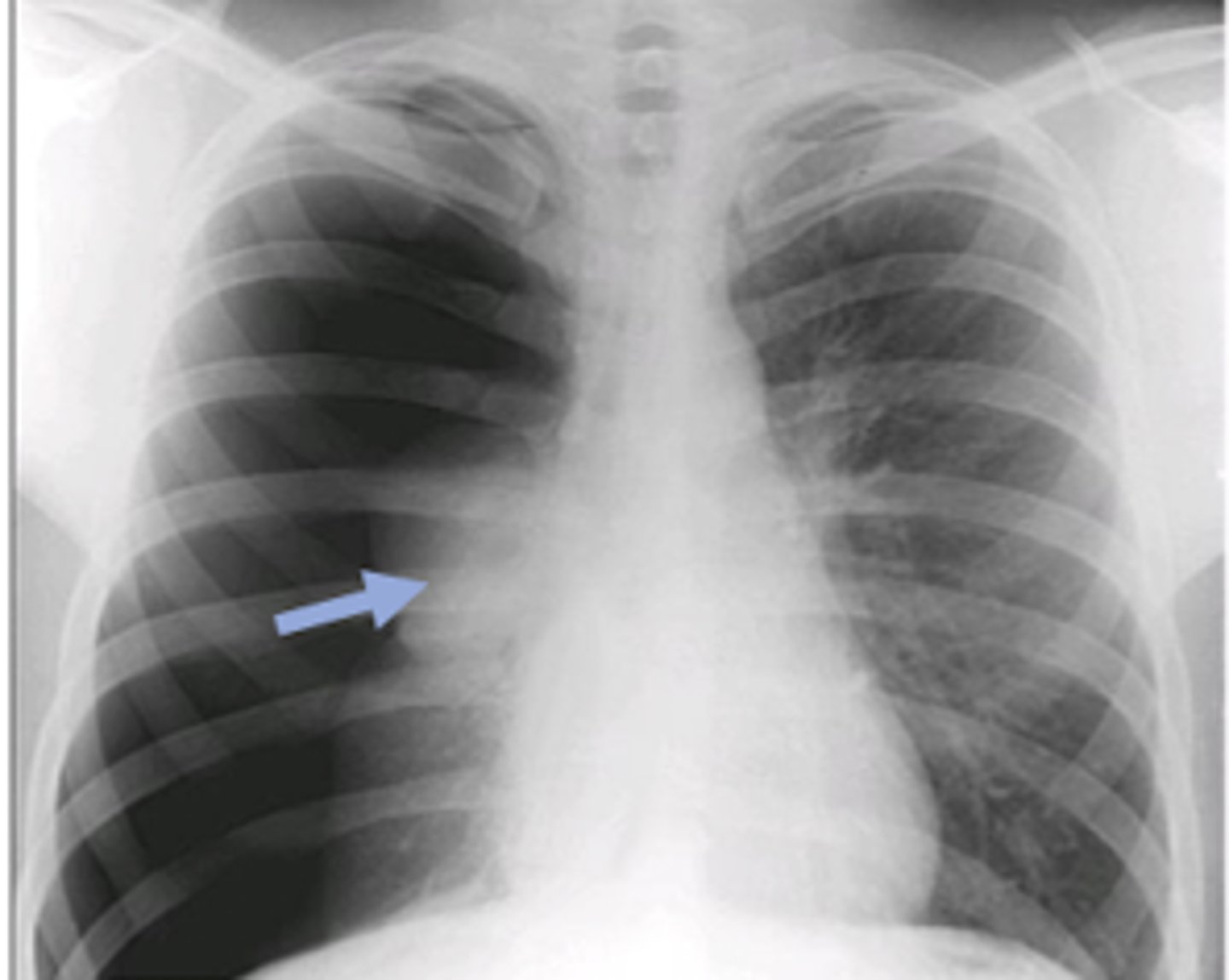
What is the difference between the right and left main bronchi?
- Right is wider and more vertical.
- Foreign bodies tend to lodge on the right side.
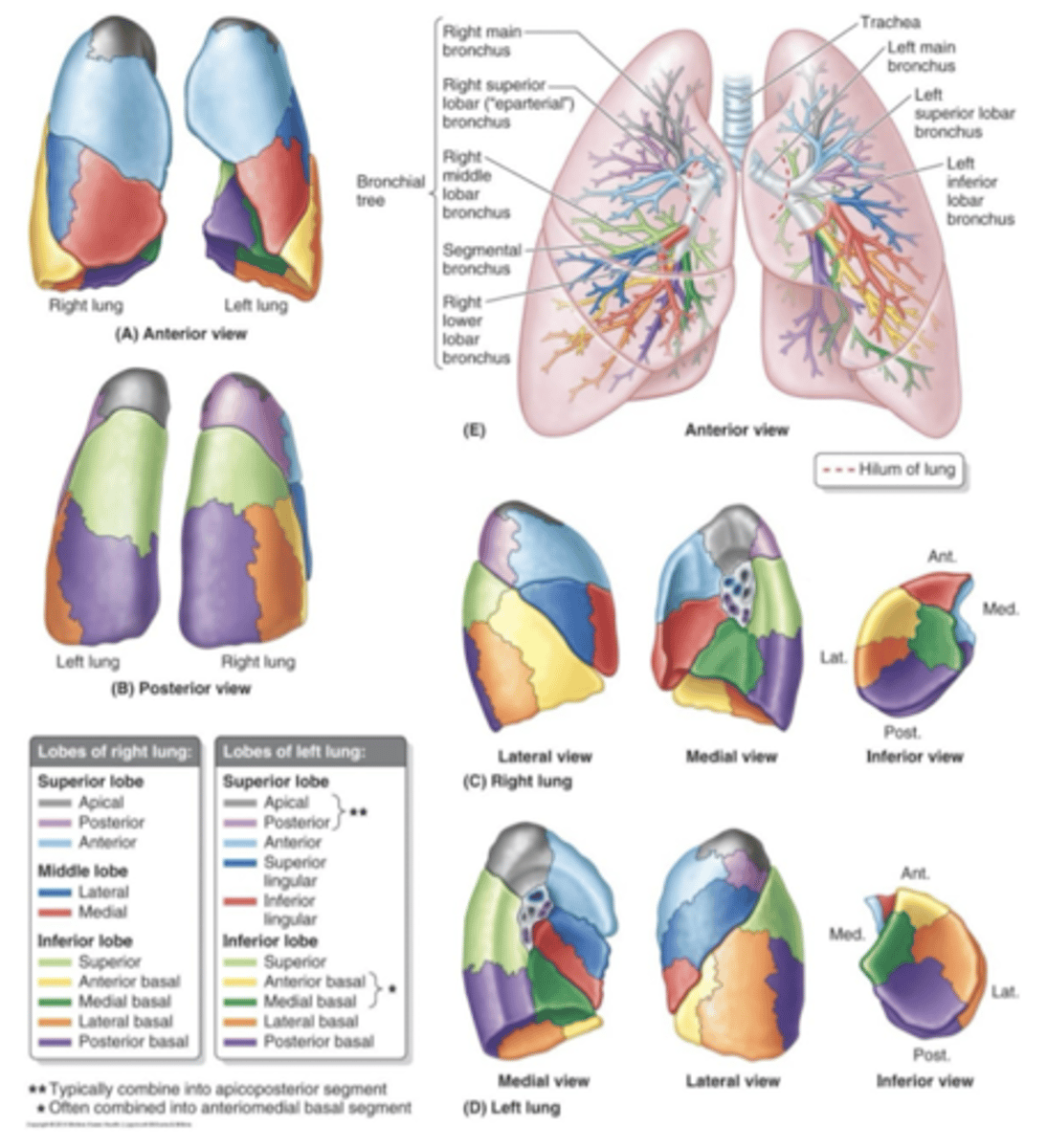
What is the function of the lobar bronchi, and how many are there on each side?
- Supplies a lung lobe.
- 3 right
- 2 left
What is the function of segmental bronchi?
Supplies bronchopulmonary segments.
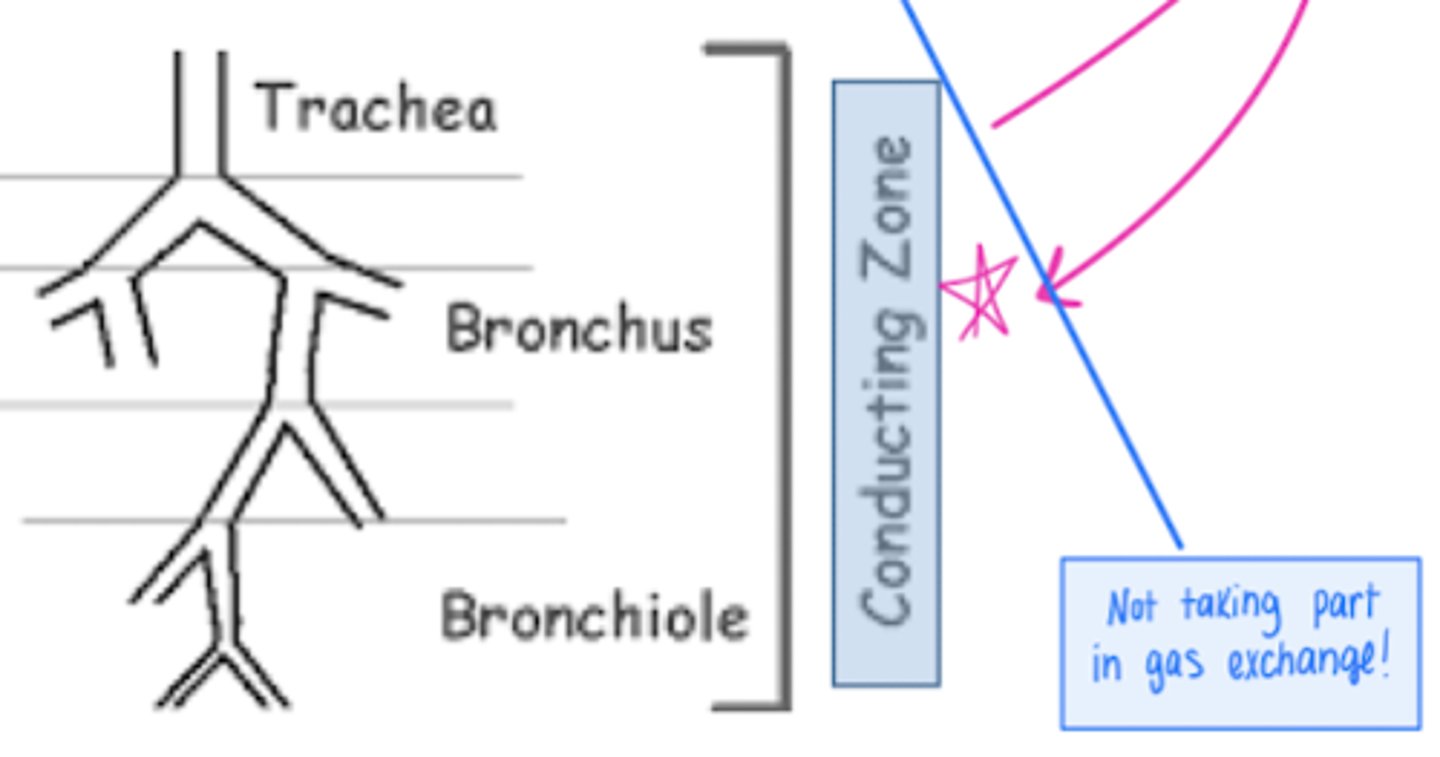
What is the order of structures in the bronchial tree from (from superior to inferior)?
- Trachea
- Right and left main bronchi
- Lobar bronchi
- Segmental bronchi
- Bronchioles
- Terminal bronchioles
Where do you generally see cancerous changes begin in the bronchial tree?
In epithelial cells.
Bronchioles have a lot of smooth muscle. Why is this important?
Allows for lumen diameter.
The trachea, bronchus, and bronchioles are part of the ______ zone.
Conducting! (not taking part in gas exchange)
What is the bronchopulmonary segment?
The area of the lung supplied by segmental bronchus & its accompanying pulmonary artery branch.
What is considered the largest subdivisions of a lung lobe?
Bronchopulmonary segment.
Describe the anatomy & structure of the bronchopulmonary segment?
- Pyramidal shape.
- Apices face the lung root.
- Bases at the pleural surface.
The bronchopulmonary segments are separated from adjacent segments by:
Connective tissue septa.
Why are the bronchopulmonary segments considered "surgically resectable"?
- 8-10 in the left
- 10 in the right
What type of tissue lines the bronchioles?
Pseudostratified columnar epithelium with cilia on their surface (ciliated).
Name the cell in the lamina propria (CT) that is 'sensitized' to the allergen:
Mast cells.
What type of tissue is found in the 'wall' of the bronchioles?
Smooth muscle (with muscarinic/nicotinic/adrenergic receptors)
How do adrenergic's and cholinergic's affect the bronchiole diameter?
- Adrenergic will dilate/relax the airway (ex: albuterol).
- Cholinergic will constrict the airway.
Smooth muscle is extremely thin in the respiratory bronchiole. Why is this important?
Allows for potential gas exchange.
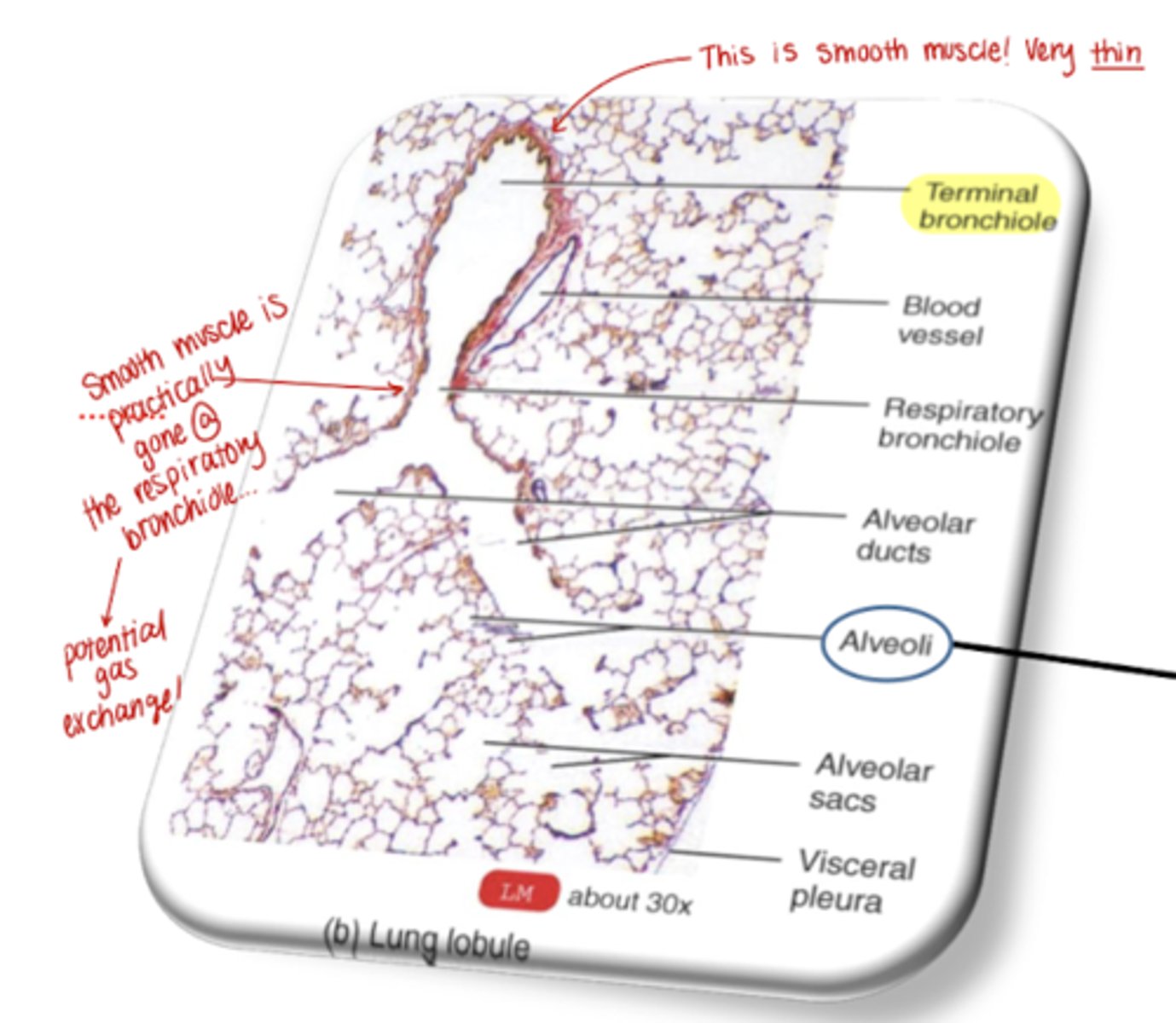
What is a lung lobule?
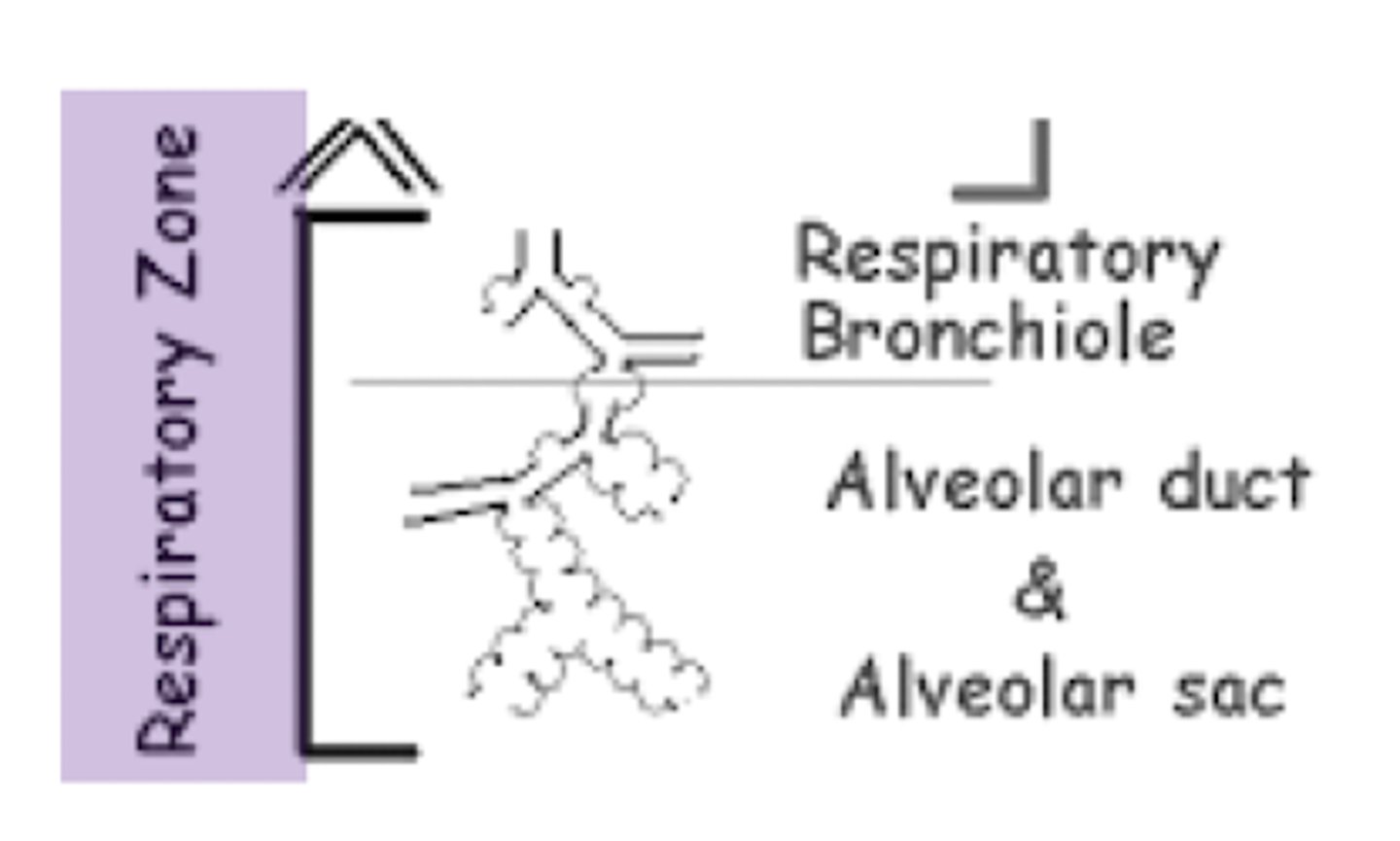
A lung unit distal to respiratory bronchioles.
What does a lung lobule consist of?
- Respiratory bronchioles
- Alveolar ducts
- Alveolar sacs
- Alveoli
What do alveoli form?
The respiratory membrane.
What is the function of respiratory bronchioles?
- They have gas transportation and gas exchange roles due to out pocketings (alveoli).
- They lose smooth muscle, which reduces airway diameter control.
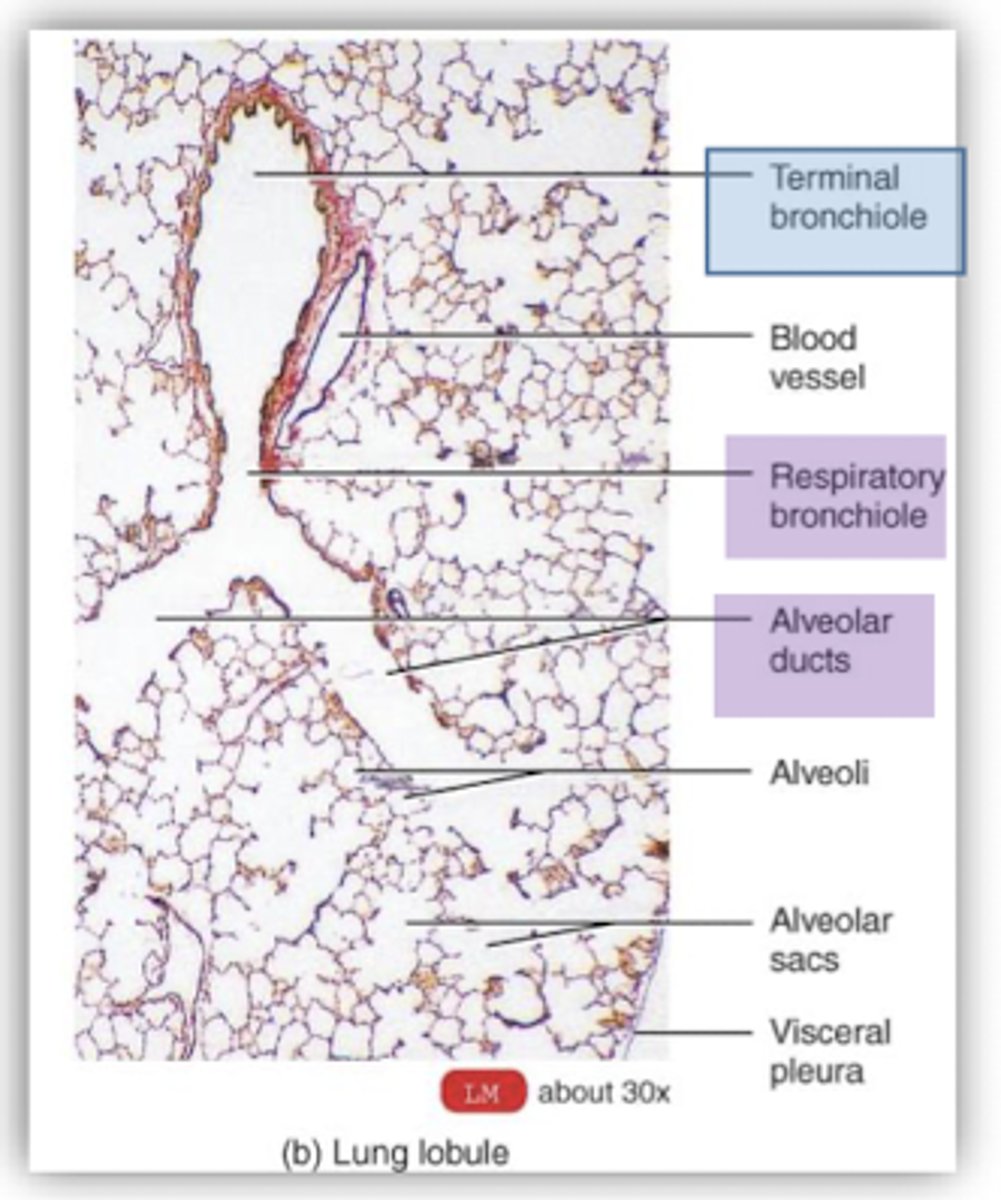
What are alveolar ducts?
- Elongated airways
lined with alveoli.
- They will lead to alveolar sacs.
What are alveolar sacs?
Clusters of alveoli.
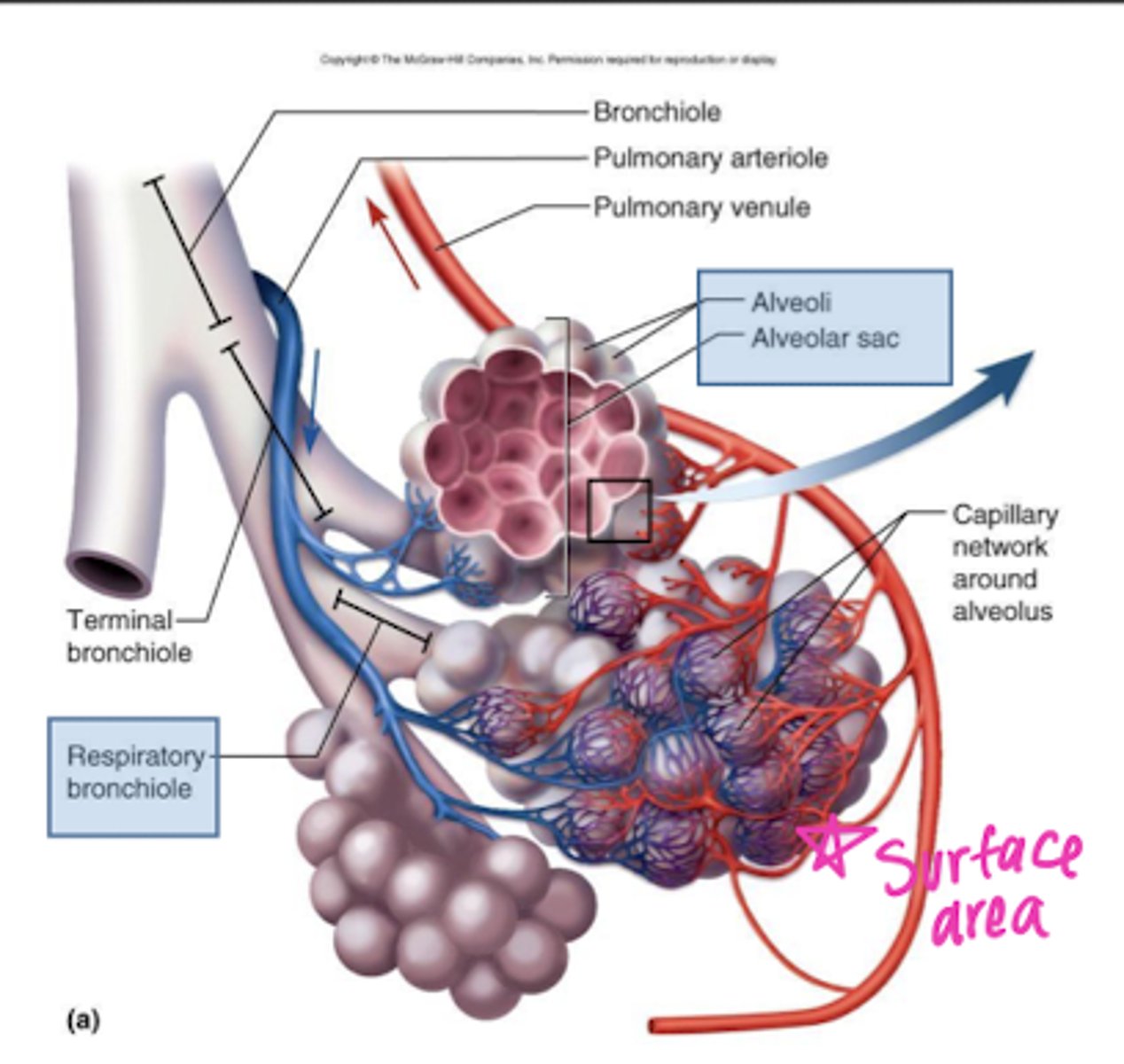
Why do alveoli have such a large surface area?
It maximizes points for gas exchange.
The respiratory bronchiole, alveolar duct, and alveolar sac are all part of the ______ zone.
Respiratory (gas exchange occurs).
What types of cells make up alveoli?
- Type I pneumocytes (simple squamous epithelial)
- Type II pneumocytes/septal cell
- Macrophages / "dust cells"
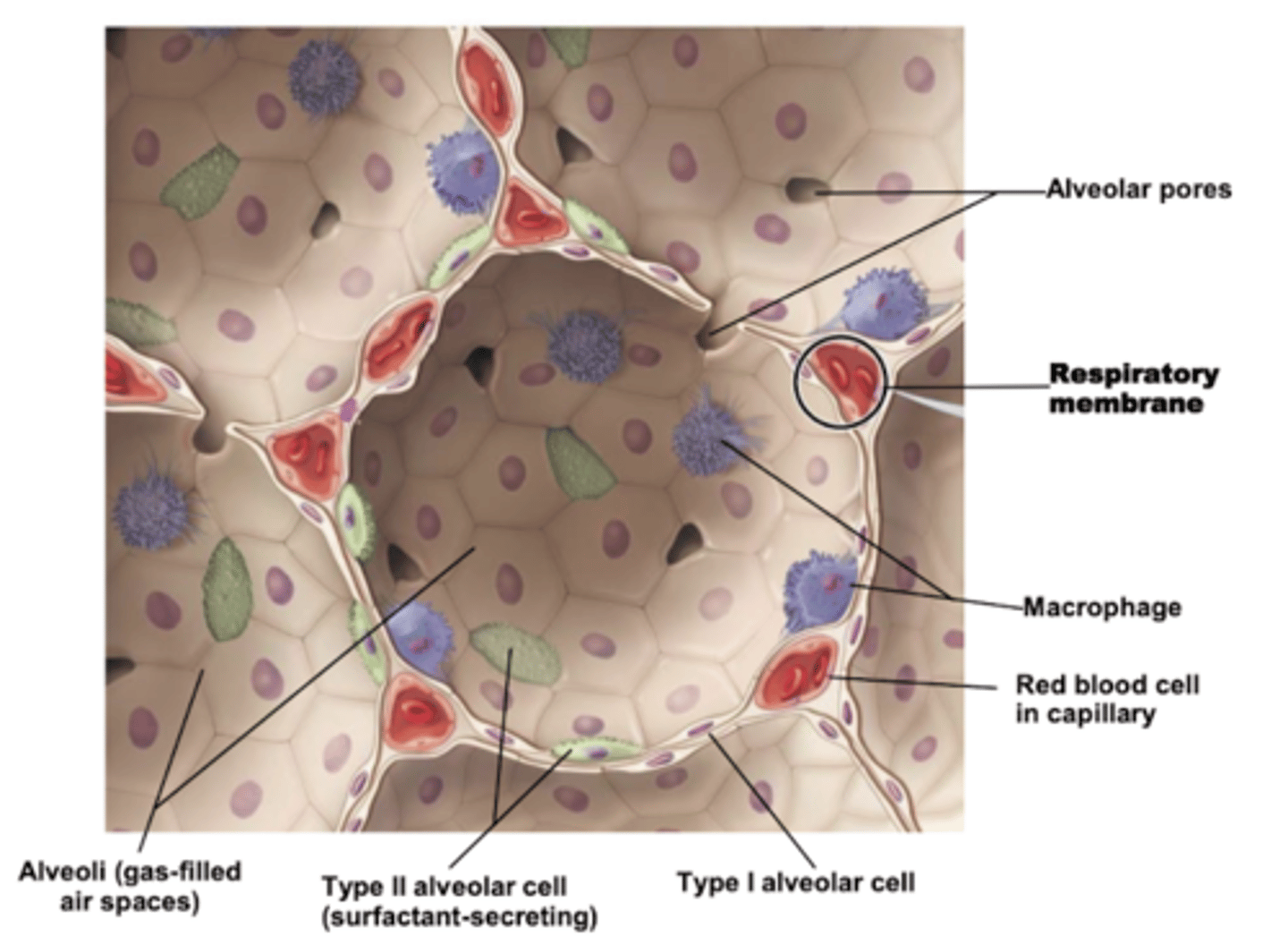
What do type II pneumocytes secrete?
Surfactant (which acts as a detergent that breaks up water surface tension).
What type of cells make up the capillary endothelium?
Simple squamous epithelial.
What is the function of connective tissue in alveoli?
Shared basement membrane between type I pneumocyte and simple squamous epithelial cell of alveoli.
The presence of elastic fibers in the alveolar connective tissue gives alveoli:
Their ability to recoil after they are stretched.
What are the pores of kohn?
- Discrete holes in walls of adjacent alveoli.
- Function as a means of collateral ventilation.
If the lung is partially deflated, ventilation can occur to some extent through the ______.
Pores of kohn.
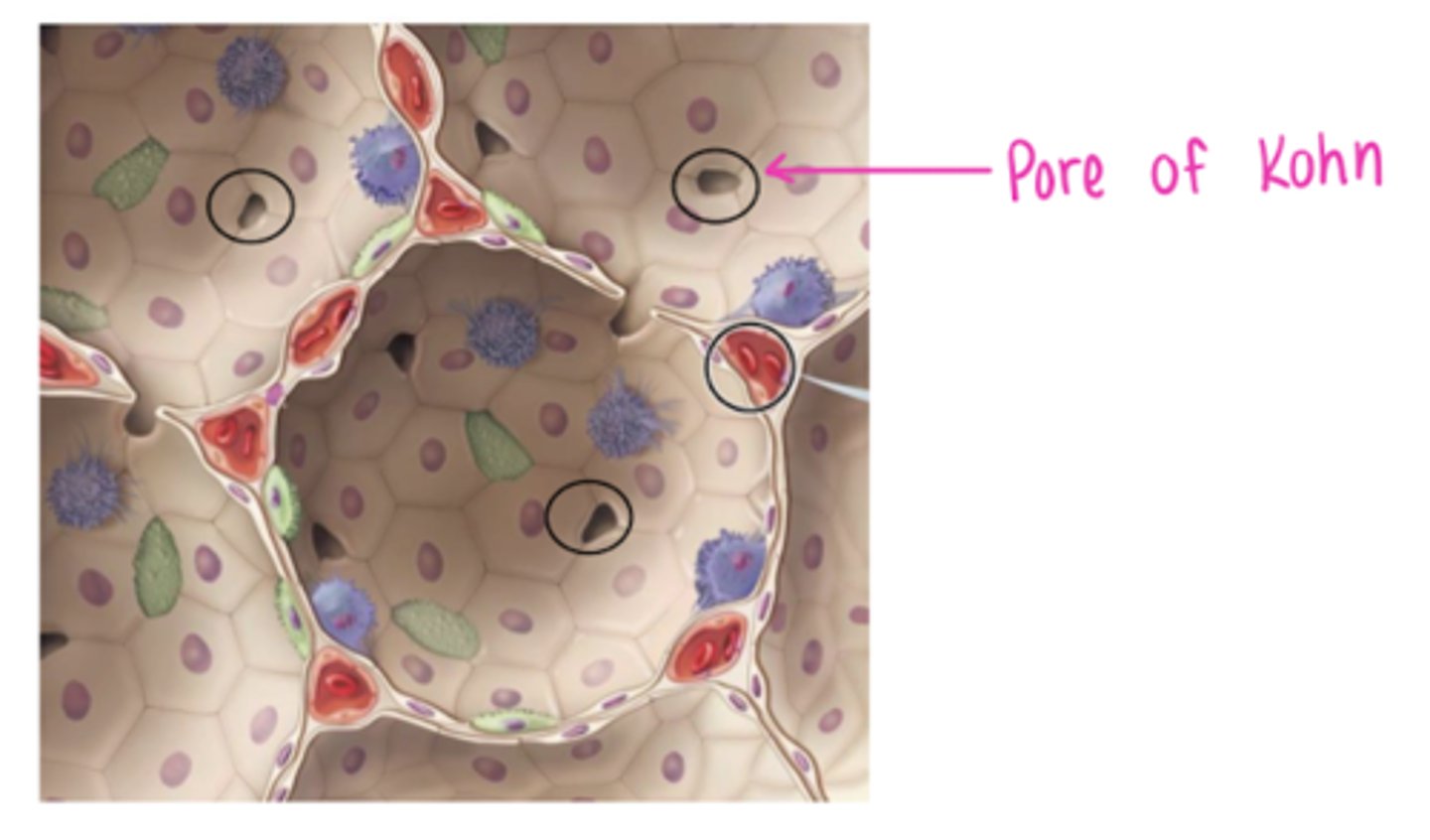
How may the pores of Kohn effect pressure?
They equalize pressure in adjacent alveoli and thus play an important role in the prevention of lung collapse.
What is a potential disadvantage of the Pores of Kohn?
The pores also allow the passage of other materials such as fluid and bacteria, which is an important mechanism of spread of infection in lobar pneumonia.
Pores of kohn can lead to which disease?
Lobar pneumonia.
What are type I alveolar cells (type I pneumocyte) and how do they work?
- Thin-walled cells that are uniquely designed to facilitate the rapid diffusion of gas.
- Because the diffusion distance is small, gas exchanges happen quickly.
What are type II alveolar cells (type II pneumocyte) and how do they work?
- Produce surfactant to coat inside of alveoli.
- Decreases surface tension in alveoli.
What is surfactant?
A lipoprotein that coats the inner surface of the alveolus.
What are 4 functions of type II alveolar cells?
- Aid in compliance (facilitates expansion during inspiration)
- Lowers alveolar surface tension at end-expiration (preventing lung collapse; atelectasis)
- Decreasing the release of proinflammatory mediators (helps control lung inflammation)
- Function as opsonins in antigen presentation to alveolar macrophages
How many layers of tissue must CO2 & O2 cross through in the respiratory membrane?
4 layers of tissue.
Gases move by diffusion, according to the difference in:
Pressure.
What 2 things can have an impact on the rate of diffusion through the respiratory membrane?
- Change in partial pressure of a gas.
- Change in the 'thickness' of the membrane.
What are the 4 layers of the respiratory membrane that a gas crosses?
- Alveolar epithelial wall (type I pneumocyte)
- Alveolar epithelial basement membrane
- Capillary basement membrane
- Endothelial cells of capillary
What is perfusion (Q)?
The distribution of blood flow in the lung (to alveoli).
Vasoconstriction & vasodilation of blood vessels in the lungs affects:
Perfusion (Q)
(the lungs are not perfectly perfused and ventilated).
Overall, what are the functions of pulmonary circulation?
- Facilitate gas exchange.
- Deliver nutrients to lung tissues.
- Act as a blood reservoir for the left ventricle.
- Serve as a filtering system (removes clots, air, etc.)
How are the vessels of pulmonary circulation arranged?
- Arteries/arterioles & veins/venules are arranged in series.
- Capillary beds are arranged in parallel.
What are the typical pressures seen in the pulmonary artery and aorta?
- Mean pulmonary artery pressure is low, ~18mmHg.
- Mean aortic pressure which is high, ~90mmHg.