Pregnancy & Prenatal Care
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
B-hCG is only present after _____________ occurs
implantation
1 multiple choice option
urine & serum pregnancy tests both detect presence of __________________________________________________ which is produced by developing placenta
human chorionic gonadotropin (B-hCG/hCG)
urine pregnancy tests are considered reliable ___________ after the first missed period
a few days
- about 5 wks gestation
serum B-hCG starts to rise _________ after ovulation if pregnancy has occurred
8 days
when will B-hCG peak during pregnancy?
near the end of the second month
- at about 100,000 mIU/mL
- during this time, they double about every 48-60 hrs
after the peak in B-hCG, the levels drop to ____________________ & remain relatively constant
20,000-30,000
what do low or slowly rising B-hCG levels often indicate?
ectopic or probable abortion
___________ can also be used to confirm pregnancy
ultrasound
what will the ultrasound findings be at 5 wks gestational age?
- gestational sac in uterus
- if yolk sac seen, intrauterine pregnancy (IUP) is confirmed
at 5+ wks gestational age, _____ can confirm IUP
TVUS
if empty gestational sac is seen w/ TVUS at 5+ wks, what should you suspect?
ectopic
what will the ultrasound findings be at 6-7 wks gestational age?
fetal heart motion
what should B-hCG levels be at 5 wks GA?
1500-2000 mlU/mL
what should B-hCG levels be at 5+ wks GA?
3500 mlU/mL
what should B-hCG levels be at 6-7 wks GA?
6000-18000 mlU/mL
what are the most common symptoms of pregnancy?
- amenorrhea
- breast tenderness & engorgement
- nausea
- fatigue
- urinary frequency & urgency
what are the most common signs of pregnancy?
- chadwick's sign
- linea nigra
- chloasma/melasma
- palmer erythema
- telangiectasias
- piskacek's sign
- hegar's sign
- leukorrhea
- fetal heart tones
chadwick's sign =
dark bluish or purplish-red color of the vaginal cervical mucosa
linea nigra =
dark line appearing longitudinally from symphysis pubis to umbilicus

chloasma/melasma =
brown pigmentation of forehead, cheeks & nose

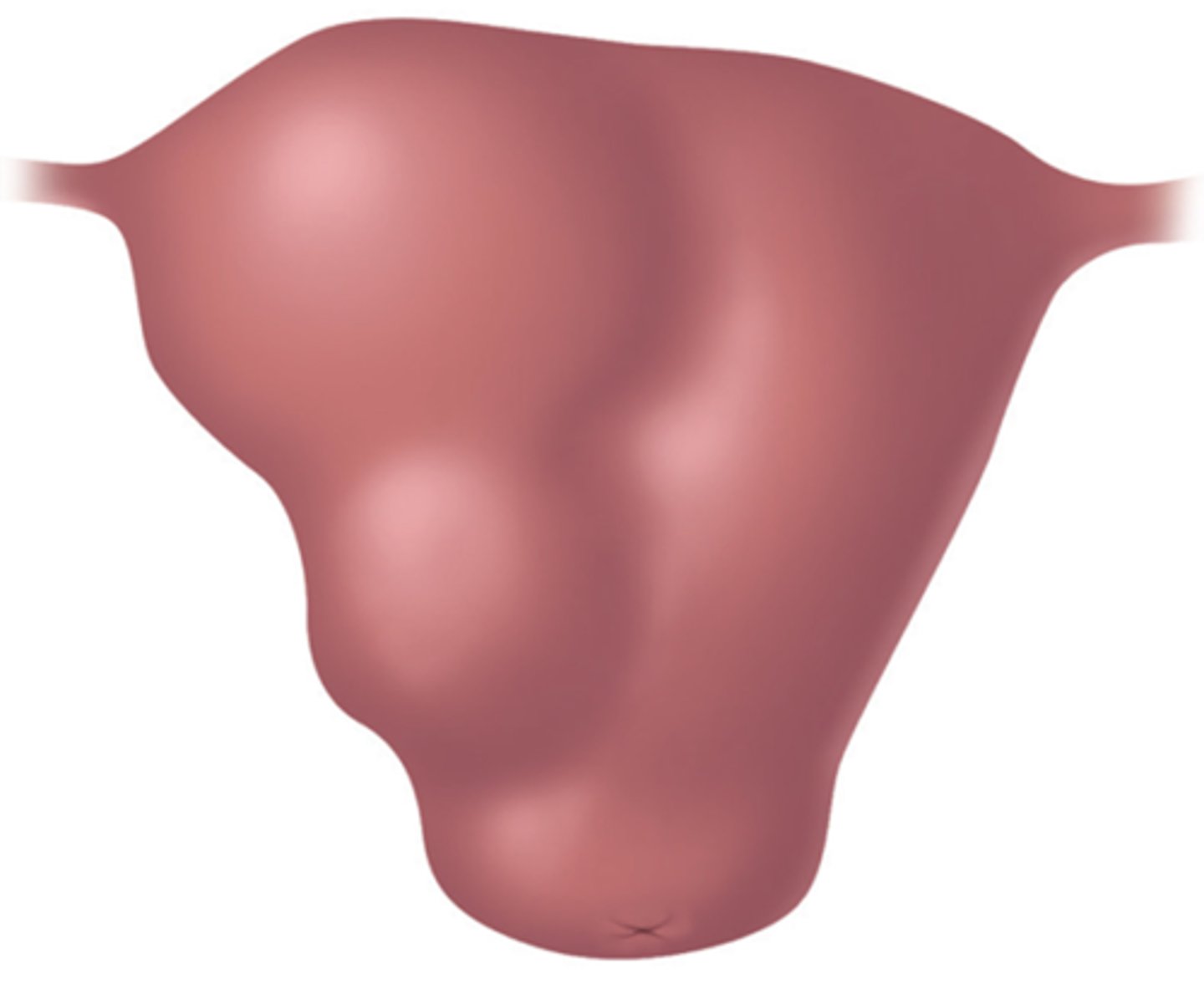
piskacek's sign =
asymmetrical enlargement of the uterus
hegar's (or Goodell or Ladin) sign =
softening of the cervix in early pregnancy
leukorrhea =
increase in vaginal discharge
when may fetal heart tones be detected by hand held doppler?
by approx. 10-12 wks
what is EDD (or EDC)?
estimated date of delivery or estimated date of confinement
- determined by the first day of the last menstrual period (LMP)
what is Nagele's Rule?
subtract 3 months then add 7 days to the date of the 1st day of the last menstrual cycle
* (LMP - 3 months) + 7 days
what is used to determine EDD if LMP is unknown?
ultrasound
(old) general rule of thumb:
- US in 1st trimester = accuracy w/i 1 wk of true EDD
- US in 2nd trimester = accuracy w/i 2 wks of true EDD
- US in 3rd trimester = accuracy w/i 3 wks of true EDD
accuracy of US dating ____________ as the pregnancy progresses
decreases
if an US is obtained in the 1st trimester, is the EDD obtained from the US or calculated from LMP more accurate?
US
1 multiple choice option
will subsequent ultrasounds change the EDD from the first US, despite discrepancies?
no
1 multiple choice option
10-12 wks: can hear fetal heart tones w/ ________ doppler
handheld
16-20 wks: first fetal movements are..
felt by mother
why is dating important?
- assess fetal development
- patient education for upcoming appts
- know when they're likely to deliver (due date)
what is prenatal (antenatal) care?
preventative in nature
- aims to prevent poor outcome
- emphasized risk assessment & health promotion
prenatal care involves an initial _____________ patient evaluation, followed by multiple routine _______ evals throughout the pregnancy
comprehensive ; focused
when should the initial, comprehensive visit take place?
first trimester
when do the follow-up, focused visits take place?
second & third trimesters
what does the initial patient evaluation include?
- determination of EDD (through LMP; if unknown, order US)
- comprehensive reproductive history (# of pregnancies, outcomes/complications)
- family history (genetic factors)
- social history (smoking, alcohol/drugs, domestic violence, sexual hx, seatbelt use)
- medical history (meds, diseases, surgical hx)
- nutritional assessment (BMI eval & folic acid supplementation)
- physical exam
- labs
what is the leading cause of trauma in pregnancy?
MVA
during medical history, what should you specifically ask about?
*varicella hx
- if no disease or vaccination, baby is at high risk if disease is contracted
*previous c-section
if pt had vertical incision w/ previous c-section:
do not attempt vaginal delivery of this pregnancy
if pt had low, transverse incision w/ previous c-section:
vaginal delivery can be attempted w/ this pregnancy
what does the physical exam include?
- pelvic exam w/ gonn/chalm screen
- PAP smear (if needed according to guidelines schedule)
- uterine size
- comprehensive, overall PE (including: periodontal, thyroid, heart)
fetal heart tones should be heard by doppler if the patient is ____________ gestation
10-12 wks
what labs should be ordered at initial visit (1st trimester)?
- PAP smear (according to screening schedule)
- NAAT (for gonn/chlam)
- RPR/VDRL (for syphilis)
- CBC (Hgb/Hct & MCV)
- blood type & antibody screen
- rubella antibody titer
- hep b surface antigen (HBsAg)
- UA & culture (protein & asymptomatic bacteriuria)
- HIV
- VZV (if no hx of dz or vaccine)
- aneuploidy screening
what can treating IDA (iron deficiency anemia) reduce risk of?
- preterm labor
- growth restriction
- maternal depression
what should be monitored at every routine visit (during 2nd & 3rd trimesters)?
- BP
- weight
- UA (dipstick; for protein & glucose)
- fetal HR, growth, & movement
- eval of any other complaints
- perinatal depression
- eval of normal physiological changes in pregnancy
when is maternal serum alpha-fetoprotein (MSAFP) offered?
15-18 wks
when are (level I) ultrasounds offered?
18-22 wks
when is the glucose load/challenge test (GLT/GCT) done?
24-28 wks
- one or two step method
when is antibody screen (indirect Coombs test) repeated if Rh -?
28 wks
- anti-D immune globulin (RhoGAM) is also given
when should you reassess Hgb/Hct?
28+ wks to assess for anemia
if indicated (high-risk), when should you rescreen for STDs?
28-36 wks
+ rescreen for chlamydia if
you should assess fetal presentation (breech, vertex, transverse, unknown) from ________ onward
36 wks
when should a group B strep culture be obtained?
36 wks
where is the group B strep culture obtained from?
distal vagina & anorectum
what should be done if group B strep culture is positive?
abx prophylaxis should be given to the mother at the time of delivery
- to help prevent possible sepsis, pneumonia or meningitis in the neonate
order a ___ in first trimester if hx of thyroid disease
TSH
order an _______ in first trimester if any risk factors
Hgb A1C
- this can detect undiagnosed T2DM
order a _____________________ in first trimester if hx of drug abuse
urine drug screen
order a ___ in first trimester if high risk of TB
PPD
what should you order for patients w/ SLE (lupus) in first trimester?
antirho & antila antibodies
- positive results can potentially lead to complete heart block in fetus
order ___________________ in first trimester if at high risk
Hep C antibodies
is Hep C treatment done during pregnancy?
no, & both vaginal delivery & breast feeding are okay
what is non-invasive prenatal testing (NIPT)?
eval of fetal cell-free DNA (cfDNA) from maternal blood
- can be done as early as 10 wks gestation (usually 11-14 wks)
NIPT is a __________ test that looks for specific chromosome aneuploidies
screening
1 multiple choice option
what can the NIPT detect?
- trisomy 13, 18, & 21
- gender
higher false positives in detecting:
- turner syndrome (x)
- klinefelter syndrome (xxy)
if the NIPT is negative, then invasive tests (such as, amniocentesis or chrionic villus sampling [CVS]) can be avoided, but if it's positive..
an amniocentesis or CVS is done to obtain fetal tissue
- a diagnostic microarray or FISH will then rule in or out the findings of the NIPT
what is often added if the NIPT is positive, as a further evaluative step?
nuchal translucency
what is nuchal translucency?
an echo-free (dark) area found on US at the back of the fetal neck between 10-14 wks gestation
what has increased nuchal translucency been associated w/?
congenital anomalies
what is the usual schedule for routine check-ups throughout pregnancy?
- q mo up to 28 wks
- q 2 wks from 29-36 wks
- q week after 36 wks
the WHO recommends a minimum of _____ prenatal visits
eight (8)
what is the normal maternal weight gain during pregnancy?
- 3 lbs in 1st trimester
- then, 1/2 to 1 lb/wk
- total of: 30-40 lbs
fetal heart tones can be heard on doppler after ___________
10-12 wks
fetal movement can be felt after ___________
16-20 wks
how is fetal growth evaluated?
by fundal height
what is fundal height?
from the symphysis pubis to the top of the fundus of the mother
- measured in cm
fundal height should match gestational age w/i ____ once the patient has reached 20 wks gestation
3 cm
ask about these things at each appointment to eval for possible complications!!
- HA
- visual changes
- RUQ pain
- edema
- N/V
- urinary sx
- vaginal bleeding
- vaginal leaking of clear fluid
- fetal movement
- cramping/contraction to assess for preterm labor
- mood
what sx require follow-up?
- HA that does not respond to acetaminophen
- persisting visual changes or RUQ pain (longer than a few mins)
- edema involving face
- excessive N/V
- dysuria
- rupture of membranes
- bleeding
- decreased fetal activity
what is one of the most common complications of pregnancy & postpartum?
depression
what does UTD recommend regarding perinatal depression screening?
use formal screening questionnaire once during pregnancy as well as after delivery
what does USPSTF recommend regarding if depression is detected during pregnancy or after delivery?
referral for counseling
which antidepressant has the best safety record in pregnancy & lactation?
sertraline (Zoloft)
which other antidepressant/antianxiety is also safe in pregnancy?
escitalopram (Lexapro)
what are some normal physiological changes in pregnancy?
- nausea
- back pain
- constipation & hemorrhoids
- braxton hicks contractions
- edema of feet & ankles
- GERD
- lower abdominal pain
- varicose veins
- insomia
how is nausea treated in pregnancy?
- OTC: pyridoxine (B6) & doxylamine (antihistamine/Unisom)
- Rx combo: doxylamine/pyridoxine (Diclegis or Bonjesta)
how is back pain treated in pregnancy?
- massage
- Tylenol (acetaminophen)
- heat
- mild stretching
how are constipation/hemorrhoids treated in pregnancy?
- increase water intake
- fiber
- stool softeners
- topical anesthetic & steroids on hemorrhoids
what are braxton hicks contractions?
irregular pattern of contractions
- do not lead to cervical change
how is edema of feet & ankles treated in pregnancy?
elevation
how is GERD treated in pregnancy?
- small meals
- antacids
- H2 blockers or PPIs
how is lower abdominal pain treated in pregnancy?
- stretching of the round ligament
- Tylenol (acetaminophen)
- heat
how are varicose veins treated in pregnancy?
- elevation
- pressure stockings
how is insomnia treated in pregnancy?
diphenhydramine (Benadryl)
what is a maternal serum alpha-fetoprotein (MSAFP) test?
triple or quad screens that detect possible neural tube defect (spinabifida or anencephaly), abdominal wall defects (ompohalocele or gastroschisis) or trisomy disorder
- optional
- ideally performed between 15-18 wks
- false positives are common
if MSAFP results are elevated,
repeating the test is reasonable
two elevated MSAFP results, should be followed w/ a..
level II ultrasound
- to eval for neural tube defect or another anomaly