Pain
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
pain definition
a distressing experience associated with actual or potential tissue damage with sensory, cognitive, emotional, behavioral, and social components
because pain is an internal, private experience, what is the gold-standard for its measurement?
self-report
peak-end phenomenon
when asked to report pain over a recent period, pt recall is predominantly influenced by the worst pain experienced over that time (the peak) and most recent pain they experienced (the end)
pain scales
numeric
verbal
visual analog
faces
pain is a ___, not a ___
issue; tissue
nociception
neural process of encoding noxious (painful) stimuli
nociceptor
high-threshold sensory receptor of the peripheral somatosensory NS that is capable of transducing and encoding painful stimuli
noxious stimuli
stimulus that is damaging or threatens damage to normal tissues
afferent
conducting toward something (CNS)
efferent
conducting away from something (CNS)
pain matrix
when peripheral nociceptors are stimulated, the signal travels up the matrix
brain structures that process and regulate nociceptive info
brainstem
amygdala
hypothalamus
thalamus
areas of the cerebral cortex
lateral pain system
discriminative aspect
perceived location and intensity of tissue damage or potential tissue damage
lateral pain system travels
spinothalamic tract (sensory pathway)
lateral pain system processed in the
somatosensory cortex
medial pain system
motivational aspect
emotions and behavior
cognitive evaluative aspect
medial pain system travels
spinolimbic and spinoreticular
medial pain system processed
limbic system (emotional system of brain)
pain matrix generates a
top-down response to regulate afferent signals
pain matrix generation is dependent on
psychological
physiological
social
genetic factors
3 patterns of pain
acute pain
episodic pain
chronic pain
acute pain
starts suddenly, ends when its cause is treated/healed
usually sharp feeling (warning signal)
common causes: strained muscles, broken bones, dental work, surgery, childbirth, infections, and/or burns
episodic pain
time to time, irregular intervals
may be associated with long-term condition (ex. migraines)
can happen out of nowhere or may be caused by known triggers
chronic pain
lasts longer than 3 months, or expected healing time
acute pain might persist and become chronic pain
can happen for no reason
can experience chronic and acute at same time
2 types of chronic pain
chronic primary pain
chronic secondary pain
chronic secondary pain 2 subcategories
neuropathic pain
nociceptive pain
chronic primary pain
neural dysfunction creates pain in the absence of tissue damage
gain of function in the central nociceptive system
chronic secondary pain
pain that is initially experienced as a symptom of another medical condition
continued stimulation of nociceptors from injury
maintained signaling after injury has healed
damage to the somatosensory system
normal nociceptive processing (how it works)
nociceptive stimulus —> nociceptive afferent —> to pain matrix
peripheral sensitization (how it works)
nociceptive stimulus —> nociceptive afferent (increased response of nociceptor to same stimulus) —> to pain matrix
respond more vigorously
increased excitatory transmitter/receptor activity in nociceptive neurons eventually elicits…
long-term functional changes that lead to hyper-excitability, spontaneous activity, and structural changes in connections
respond normally, but more vigorous response of pain matrix
signs of central sensitization: “dysestheasis”
hyperalgesis
allodynia
spontaneous pain
temporal summation
secondary hyperalgesia
hyperalgesis
increased pain response to nociceptive stimulus
ex. pain amplified because already swollen toe after being stepped on later that same day
allodynia
perceiving innocuous (not harmful) stimuli as painful
ex. putting on shirt over sunburn when putting on shirt usually is not painful
spontaneous pain
temporally distinct from external stimulus, unprovoked
described as burning, shooting, electrical
ex. feeling like you hit your funny bone without hitting it
temporal summation
perception of increased pain as response to increased stimulus or continuous presence of stimulus
secondary hyperalgesia
spread of pain adjacent to uninjured areas
ex. paper cut localized to small portion, feel around whole pad of finger
structural reorganization in the cortex (rewiring)
nociceptive message —> cortical neuron —> formation of synapses with new neurons
how we feel more pain than we should
reduced descending inhibition
on the way back down, we can have different tracts in the same limbic systems that can dull our pain a little bit
cellular changes (neuroplasticity) that reflect central sensitization
increased spontaneous activity
increased responsiveness to afferent inputs
prolonged after-discharge in response to repeated stimuli
expansion of receptive fields
some evidence suggests as we move from acute to chronic
pain processing moves from the sensory areas of the brain to the emotional/interventional part
nociceptive pain
pain caused by tissue damage
sensation can be sharp, pricking, dull/aching
ex. pain, infection, broken bone, osteoarthritis
neuropathic pain
pain caused by nerve damage due to injury or disease
sensations are burning, tingling, shooting, electric
ex. diabetic neuropathy, shingles, sciatica
nociplastic pain
caused by changes in how the NS processes pain
not linked with clear injury, tissue damage, inflammation, or disease
sensations vary widely
ex. fibromyalgia, IBS, tension headaches
nociceptive chronic pain
due to continuing stimulation of nociceptive receptors
ex. chronic pain that results from a vertebral tumor pressing on nociceptors in the meninges surrounding the SC
primary hyperalgesia
chemical changes in the damaged tissue awaken sleeping peripheral nociceptors
chronic secondary pain can occur from
central sensitization
ectopic (abnormal location) foci
ephaptic (cross-talk, occurs in demyelinated regions) transmission
ectopic foci
a signal coming from a place it shouldn’t
ridiculopathy (nerve pinched in neck, feeling in fingers)
cross-talk
ephaptic transmission
occurs in demyelinated regions
occurs as a result of lack of insulation between neurons
neuropathic pain can arise from abnormal neural activity in the following:
periphery
CNS in response to deafferentation
dorsal horn
complete nerve resection
results in lack of sensation from that nerve’s receptive field
partial damage
can result in allodynia and sensations similar to an electric shock-pain
damaged area =
demyelinated
demyelinated =
chance for ectopic foci and/or ephaptic transmission
most common cause of neuropathic pain
periphery
A-alpha nerve fibers carry info
related to proprioception (muscle sense)
A-beta nerve fibers carry info
related to touch
A-delta fibers carry info
related to pain and temp
C-nerve fibers carry info
related to pain, temp, and itch
gate theory of pain
mechanism in SC
pain signals can be sent up to the brain to be processed to accentuate the possible perceived pain, or attenuate it at the SC itself
counterirritant theory
inhibition of nociceptive signals by stimulation of non-nociceptive receptors occurs in the dorsal horn of the spinal cord
enkephalin binding depresses
release of substance P (neuropeptide)
antinociceptive systems
suppression of nociception in response to stimulation that would normally be painful
serotonin and norepinephrine
inhibitory
endogenous opioids
chemicals produced by the body that activate the antinociceptive system
found throughout CNS
suppressor system made up of
endogenous opioids
serotonin
norepinephrine
does the antinociceptive system wait around and wait to be stimulated?
no, on in background
stress-induced antinociception
how many sites of antinociception?
5
level I
occurs in periphery
level II
occurs in dorsal horn
level III
fast-acting neuronal descending system
level IV
hormonal system
level V
amygdala and cortical level
pain neuroscience education
process to explain to a patient the neurobiology and neuroscience of their pain experience in a manner that is easily understandable and applicable
if a pt truly understands PNE, they will
have less pain
have less disability
move better
perform better with rehab
have better cognitions regarding their pain
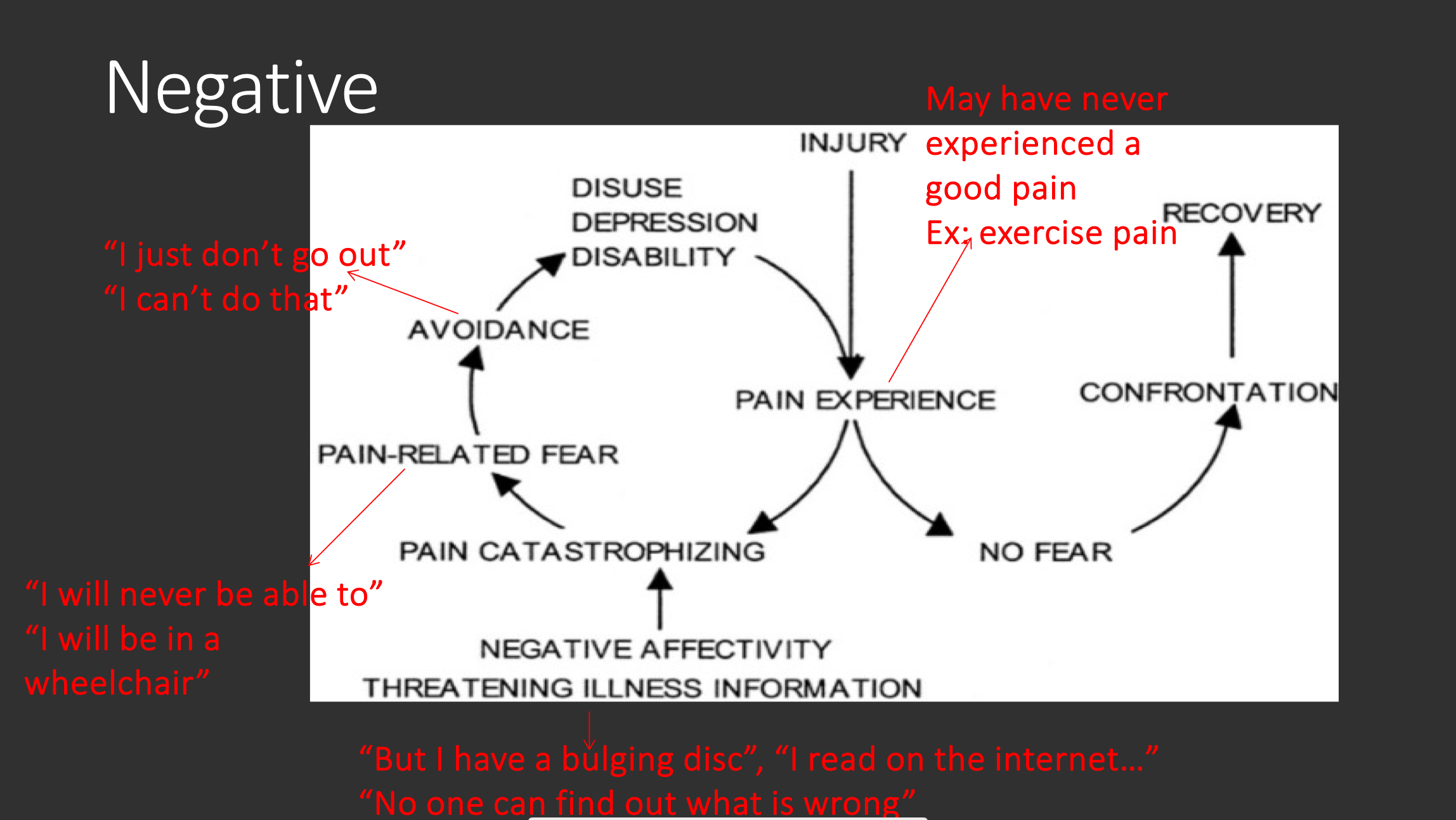
negative pain experience
pain experience —> pain catastophizing —> pain-related fear —> avoidance —> disuse depression disability
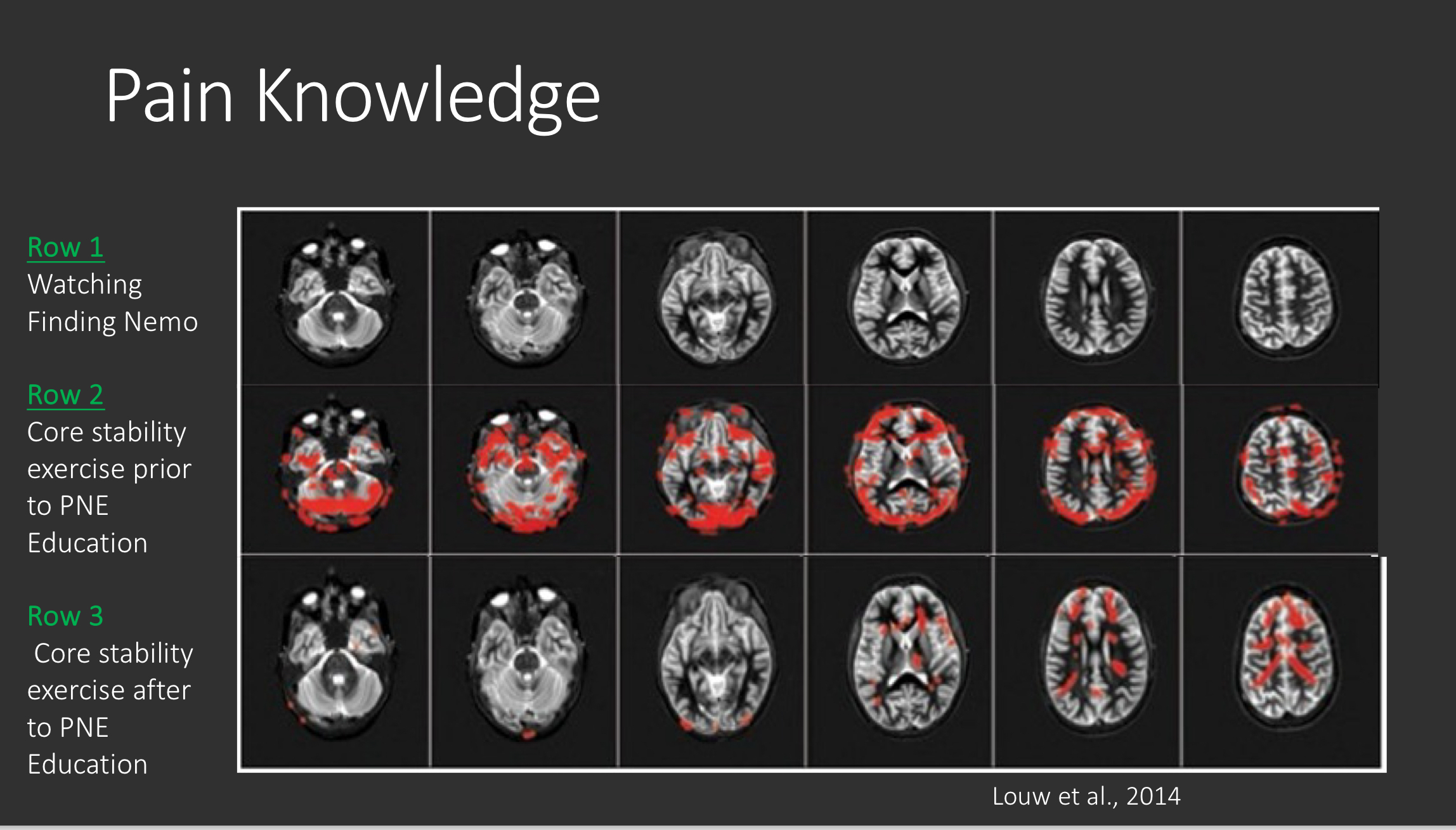
pain knowledge
more activity in brain centers before PNE education
less activity in brain centers after PNE activity (can modulate their own pain)
4 pillars of focus
pain knowledge/education
exercise/aerobics
sleep/stress management
goals setting
pain inhibiting system occurs
throughout the NS
pain is always a
personal experience that is influenced to varying degrees of biological, psychological, and social factors
pain cannot be inferred
solely from activity in sensory neurons
through life experiences, individuals learn
the concept of pain
a person’s report of an experience as pain should be
respected
pain serves an
adaptive role
pain may have adverse effects on
function, social, and psychological well-being
inability to communicate does not
negate the possibility that a human or nonhuman animal experiences pain