Balance, Coordination, and Proprioception in DPT 652
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
Balance
Dynamic process by which body's position is maintained in equilibrium (at rest or moving); best when Center of Mass (COM) over Base of Support (BOS).
Center of Mass (COM)
The point in a body where the mass is evenly distributed and balanced.
Center of Gravity (COG)
The point where the total weight of a body is concentrated.
Momentum
The quantity of motion an object has, dependent on its mass and velocity.
Base of Support (BOS)
The area beneath an object that includes every point of contact that the object makes with the supporting surface.
Limits of Stability (LOS)
The maximum distance a person can lean in any direction without losing balance.
Ground Reaction Forces (GRF)
The force exerted by the ground on a body in contact with it.
Center of Pressure (COP)
The point of application of the ground reaction force, representing the center of the distribution of vertical forces.
Nervous System
The system responsible for sensory perception of body orientation in space, including visual, vestibular, and somatosensory systems.
Sensorimotor Integration
The process of combining sensory information with motor responses for adaptive and anticipatory postural control.
Motor Strategies
The planning, programming, and execution of movements required for maintaining balance.
Musculoskeletal Contributions
Factors such as postural alignment, flexibility, joint integrity, and muscle performance that affect balance.
Contextual Effects
Environmental factors that influence balance, including the predictability of the environment and the type of support surface.
Support Surface
The type of ground or surface that affects stability, such as firm vs. slippery or stable vs. unstable.
Effects of Gravity
The influence of gravitational forces on body positioning and balance.
Inertial Forces
Forces that affect the body due to its motion or lack of motion.
Sensory Control of Balance
Perception of body in space & movement via peripheral receptors (visual, somatosensory (proprioceptive, joint, cutaneous) and vestibular systems.
Visual system
Info on position of head relative to environment, orientation of head to maintain level gaze, direction & speed of head movements.
Somatosensory system
Info about position & motion of body & body parts relative to each other & support surface (muscle spindles, GTOs, joint receptors, skin mechanoreceptors help).
Vestibular system
Provides info about position & movement of head w/respect to gravity & inertial forces & fast head movements. Receptors in semicircular canals detect angular accel of head; receptors in otoliths detect linear accel & head position w/respect to gravity & slow head movements.
Sensory Organization for Balance Control
Vestibular, visual & somatosensory inputs combined to produce orientation & movement. When 1 system is inaccurate (d/t injury or environment), CNS must suppress inaccurate input and combine appropriate sensory inputs from other 2 systems.
How To Use Info In Intervention - Visual system
Use it when proprioceptive or vestibular inputs are unreliable (d/t damage or on boat or ramp, etc.); by visually fixating on target.
How To Use Info In Intervention - Somatosensory system
When visual or vestibular inputs unreliable.
How To Use Info In Intervention - Vestibular system
When visual & somatosensory inputs unreliable (i.e. pt with DM with certain deficits).
Types of Balance Control
Function requires: static, dynamic, automatic postural reactions.
Feedforward control
For movements that occur too fast to rely on sensory feedback (e.g. reactive responses) or anticipatory aspects of postural control.
Anticipatory control
Activation of postural muscles, in advance of performing skilled movements (e.g. obstacles in environment).
Closed loop control
Used for precision movements that require sensory feedback (e.g. standing on a balance beam).
Motor Strategies for Balance
Need to keep COM over BOS; 3 primary movement strategies.
Balance Muscle Activation Strategies - Ankle Strategy
Quiet stance & small perturbations (slow on large firm surface); activation typically distal to proximal; requires 5-10° of ankle DF; fair to good strength in ankle DF and PF.
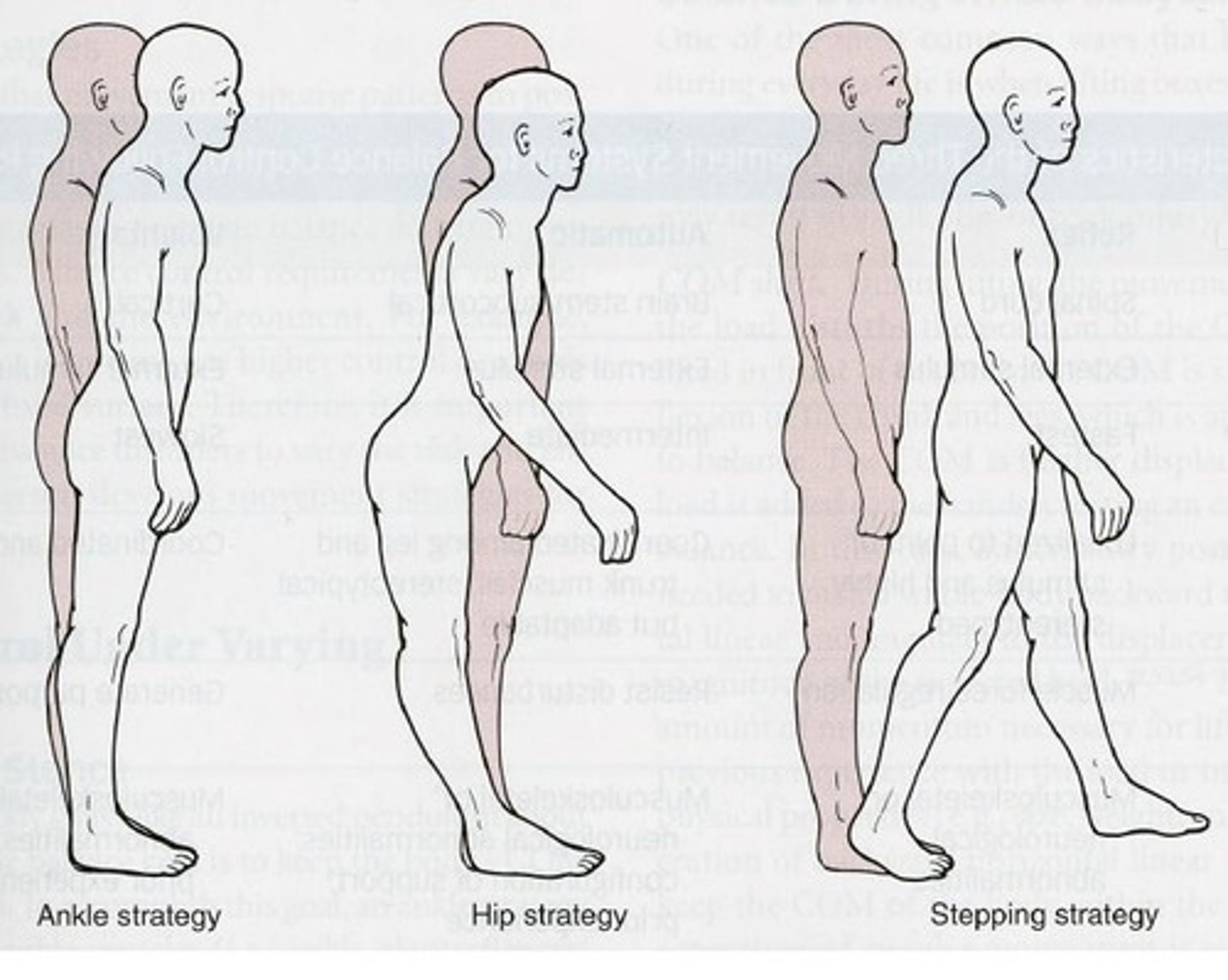
Balance Muscle Activation Strategies - Hip
Narrow surfaces, fast or bigger perturbations; requires 30° hip flexion and 5° ext; fair to good strength in hip flexors and extensors.
Balance Muscle Activation Strategies - Stepping
For larger perturbations that move center of gravity outside base of support.
Weight-shift Strategy
Control M/L perturbations; shift body weight laterally from 1 LE to other; hips key points of control using hip abd and add muscles (some help from ankle invertors & evertors).
Suspension Strategy
Quickly lowers COM by flexion knees, causing associated flexion of ankles & hips.
Combined Strategies
Depends on task & environment.
Balance Control Under Varying Conditions
During stance- ankle muscles/glut med/TFL/iliopsoas, paraspinals/abd; like inverted pendulum.
Perturbed standing
Internal (proactive m. act) or external (reactive m.).
COM shift
The movement of the center of mass during lifting.
Anticipated weight and momentum
Consideration of the load and its movement during lifting.
Loss of balance
A condition requiring a stepping response to regain stability.
Lifting style
The method of lifting, either with knees flexed or extended.
Balance During Gait
The center of mass is always outside the base of support except during double limb support.
Controlled fall
A technique to maintain balance by intentionally falling in a controlled manner.
Impaired Balance
A condition caused by disease or injury affecting information processing stages.
Sensory input
Information received from the environment that affects balance.
Proprioceptive deficits
Loss of sensory input from muscles and joints, often due to age or diabetes.
Visual loss or deficits
Diminished or impaired vision affecting balance.
Damage to vestibular system
Injury to the inner ear structures affecting balance, often due to infection, TBI, or aging.
Damage to BG, CB, SMA
Injury to the basal ganglia, cerebellum, or supplementary motor area affecting balance.
Motor output
The physical response generated by the musculoskeletal or neuromuscular system.
Musculoskeletal impairments
Issues related to posture, range of motion, and muscle performance.
NM system impairments
Neuromuscular issues affecting coordination and pain.
Balance Deficits with Aging
Challenges in balance due to complex interactions of multiple risk factors.
Matter of Balance program
A published guideline for fall prevention.
Declines in sensory systems
Deterioration of sensory functions and information processing with age.
Compromised APAs
Impaired anticipatory postural adjustments affecting balance.
Fear of falling
Anxiety that can impact balance and mobility.
Balance Deficits from Medications
Increased fall risk in older adults taking more than four medications.
Examination & Evaluation of Balance
A comprehensive assessment including history of falls and sensory input evaluation.
Static Balance Tests
Tests such as Romberg and Single Leg Balance Stance Test to assess static balance.
Dynamic Balance Tests
Tests involving movement on unstable surfaces or transitions between positions.
Anticipatory Postural Control Tests
Tests requiring voluntary movements to counteract predicted disturbances.
Functional Reach Test
A measure of reach distance with less than 10 inches indicating increased fall risk.
Reactive Postural Control Tests
Assessment of responses to external perturbations affecting balance.
Pull Test
A test to assess postural stability by pulling the patient backward.
Push and Release Test
A test to evaluate balance by pushing the patient forward and observing their response.
Clinical Test of Sensory Integration on Balance Test (CTSIB)
A test that evaluates how well a person can maintain balance under various sensory conditions.
Sensory Organization Test (SOT)
The computerized version of the Clinical Test of Sensory Integration on Balance Test.
Tinneti Performance-Oriented Mobility Assessment (POMA)
A test used to assess a person's mobility and balance.
Timed Up and GO Test (TUG)
A test that measures the time it takes for a person to stand up from a seated position, walk three meters, turn around, walk back, and sit down.
Berg Balance Scale
A 14-item test that assesses balance through various functional tasks.
Four Square Step Test
A test that assesses dynamic balance by having a person step in multiple directions.
Dynamic Gait Index (DGI)
An 8-item test that evaluates a person's ability to modify balance while walking.
Functional Gait Assessment
A test designed to assess gait and balance during functional tasks.
HiMAT
High-level Mobility Assessment Tool, used to evaluate high-level balance and mobility.
Four Step Square Test (FSST)
A test that assesses dynamic balance in older adults by moving the center of gravity outside the base of support.
Berg Balance Test
A validated tool that assists in determining the need for assistive devices based on a scoring system.
Activities Specific Balance Confidence Scale (ABC)
A scale that measures a person's confidence in performing various activities without falling.
Falls Efficacy Scale
A scale that assesses a person's fear of falling during various activities.
Balance Training: Static Control
Training that involves maintaining balance in a stationary position.
Balance Training: Dynamic Control
Training that involves maintaining balance while in motion.
Balance Training: Reactive Control
Training that focuses on responding to external forces to maintain balance.
Balance Training: Sensory Organization
Training aimed at decreasing reliance on visual, somatosensory, or vestibular inputs for balance.
Fall Prevention Programs for Elderly
Programs designed to reduce falls among elderly individuals through various interventions.
Fall Prevention for High Risk Elderly
Strategies specifically tailored for elderly individuals at high risk of falling, including home exercises and Tai Chi.
Balance Exercise Progression
A structured approach to gradually increase the difficulty of balance exercises.
Coordination
The ability to use different parts of the body together smoothly and efficiently, which is not synonymous with balance.
Cerebellum
Major section of brain responsible for planning, coordinating and refining movement based on previous experience, sensory feedback before, during and after movement
Coordination Disorders
Ataxia - inability to coordinate timely muscle activations while adjusting for movements at other joints
Causes of Uncoordinated Movement
Injury to cerebellum, nerve, joint
Assessing Coordination
Describe quality of movement: smooth, asynergia, decomposition (robot-like) movement, tremor (intention vs. resting vs. terminal)
Intervention
Base on functional goals with a rehabilitative approach
Proprioception
Unconscious activation of the dynamic restraints surrounding a joint in response to sensory stimuli
Anatomical Structures Involved in Proprioception
Muscle Spindle - Within muscle fibers and kept on slight stretch by gamma motor neuron, stimulated by stretch
Assessment of Proprioception
Stabilize proximal segment, touching lightly, change position in sagittal plane of more distal joint
Proprioception Interventions
Closed chain activities throughout ROM, higher level balance activities
Examples of Interventions
Hands on wobble board 3x30sec has been shown to increase proprioception in shoulders.
Conclusions
Just as with strengthening, be specific to functional outcome and never skip balance/proprioception in treatment