L. 29 - Immunity to Infection: Host-Pathogen Interactions and Defense Mechanisms
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
What are the six types of pathogens that cause infectious diseases?
Extracellular bacteria, intracellular bacteria, viruses, parasites, fungi, and prions.
What occurs when an organism successfully avoids innate defense?
Infection, where the organism colonizes a niche in the body.
What is the biological interaction between pathogens and the immune system described as?
A 'horse race' or 'war' where the pathogen tries to replicate while the immune system attempts to eliminate it.

When does a host experience 'disease' from a pathogen?
Only if pathogen replication results in detectable clinical damage.
What can cause disease even in the absence of colonization?
Bacterial toxins.
What is immunopathic damage?
Injury to host tissues caused unintentionally by the immune response.
What determines the best effector mechanisms to counter a pathogen?
The invader's lifestyle and mode of replication.
What are the first obstacles encountered by an invader?
Intact skin and mucosae.
What happens when the immune system is compromised?
Opportunistic pathogens may cause disease.
How do invasive pathogens usually gain access to mucosae?
Via M cells or by binding to host cell surface molecules that initiate receptor-mediated internalization.
What triggers the influx of acute phase proteins and pro-inflammatory cytokines?
A pathogen that penetrates skin or mucosae.
What role do PRRs play in innate defense?
They mediate the general innate defense by recognizing pathogens.
What are some examples of PRRs?
TLRs, NLRs, RLRs, CLRs, scavenger receptors, and cell-bound collectins.
What is the role of leukocytes activated by PRR engagement?
To eliminate the pathogen or infected cells through various mechanisms.
What is the primary defense against blood infections?
Neutrophils and monocytes provide innate defenses.
What triggers the adaptive immune response?
Local dendritic cells presenting pMHCs to naïve T cells after maturation.
Where do T and B cell activation take place?
In inductive sites in MALT/SALT.
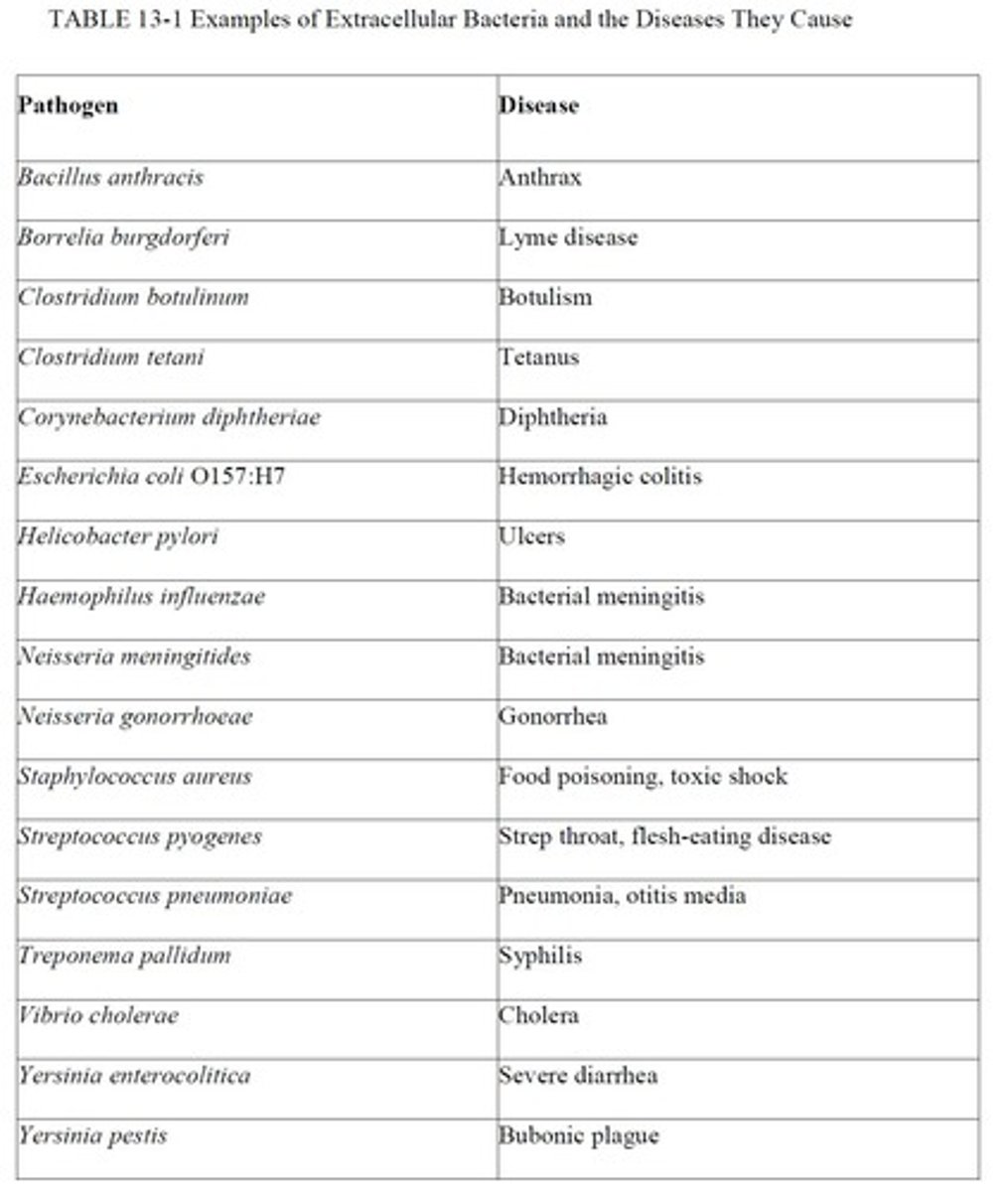
What do extracellular bacteria tend to accumulate in?
Interstitial regions in connective tissues, lumens of tracts, and blood.
What are exotoxins?
Toxic proteins actively secreted by Gram +ve or Gram -ve bacteria.
What are endotoxins?
Lipid portions of LPS molecules in the walls of Gram -ve bacteria, released when the cell wall is damaged.
How do intracellular bacteria generally enter host cells?
By clathrin-mediated endocytosis.
What is a granuloma?
A structure that walls off an intracellular pathogen, formed around infected macrophages.
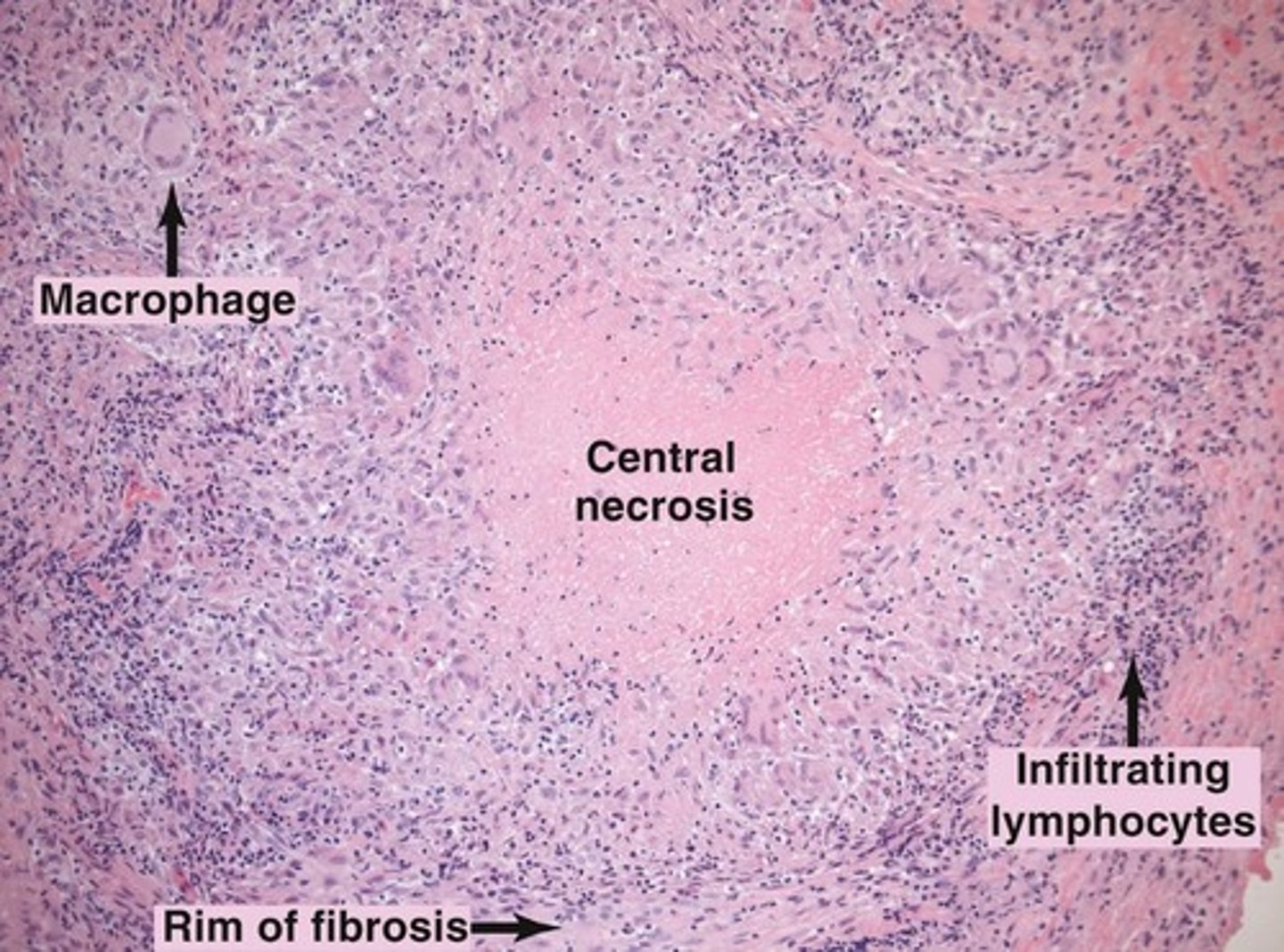
What cytokines play important roles in granuloma formation?
IL-17, IL-12, and IFN-g produced by Th1 cells.
What happens to a granuloma if the trapped pathogens remain viable?
It persists, indicating the disease is becoming chronic.
What can happen if a granuloma breaks down?
Trapped pathogens are released back into the body to resume replication.