Countercurrent Exchange system
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
describe where along the nephron it is permeable and impermeable to urea. Where is most of the urea absorbed?
-most of the urea is passively absorbed at the proximal convoluted tubule
-Urea can be passively absorbed at the descending loop of henle and the ascending loop of Henle
-However, it CANNOT be absorbed once you reach the TAL (thick ascending limb of the loop of Henle)
-it CANNOT be absorbed at the collecting duct that is located in the cortex
-it can be absorbed at the collecting duct that is located in the medullary portion of the kidney
How does urea mainly move?
through peritubular transport via solvent drag
Describe the transport of NaCl in various parts of the nephron
NaCl can be passively absorbed at the descending loop of Henle and the ascending loop of Henle
it will be actively absorbed once it reached the TAL and then actively absorbed all throughout the collecting duct
describe where the nephron is:
isosmotic
hyperosmotic
hypoosmotic
isosmotic:
1. at the proximal tubule and the first part of the descending loop of Henle
hyperosmotic:
1. the loop at the loop of Henle
2. the medullary portion of the ascending loop of Henle
3. the medullary portion of the collecting duct
hypoosmotic:
1. at the TAL
2. the distal tubule (it is even more hypoosmotic)
describe the osmolarity of the TAL and explain why this is the case
AKA the Diluting segment
-the TAL is hypoosmotic
-this is because the water cannot leave the tubular fluid, and there is a lot of NKCC transporters that are shunting solutes out of the tubular fluid
describe the osmolality of the descending loop of Henle and explain why this is the case
-the descending loop of Henle is isotonic
-this is because it is permeable to water; therefore the water is leaving the nephron and entering the interstitial space
describe the osmolality of the thin ascending loop of Henle and explain why this is the case
-the thin ascending loop of Henle is hyperosmotic
-this is because NaCl begins to leave the nephron; but urea enters the nephron through passive diffusion. Overall there is an increase in solutes in the thin ascending limb
-also remember: water cannot leave this segment
describe the osmolality of the collecting duct and explain why this is the case
the collecting duct is hyperosmotic
-under the effects of ADH:
1. more aquaporins will be inserted in the principle cells
2. therefore water will leave the collecting duct and enter the interstitium
3. this will increase the effective concentration of the solutes in the collecting duct--> hyper osmotic
-it also has urea pores that shunt urea into the intersititium. this increases the osmolarity of the intersititium; therefore water is pulled out of the collecting duct and pumped into the intersititium
describe the osmolality of the proximal tubule and explain why this is the case
the proximal tubule is isosmotic
-this is because ions are leaving the nephron; but water is also leaving the nephron
-therefore the solution remains isotonic
describe the osmallity of the distal tubule and explain why this is the case
-the distal tubule will be very hypoosmotic
-this is because a lot of NKCC was already transported out in the TAL; so it is already hypo osmotic when it enters the distal tubule
-the distal tubule can still not get rid of water to offset this hypoosmolarity
-at the distal tubule the hypoosmolarity will become even more profound because the nephron is still shunting out Na+
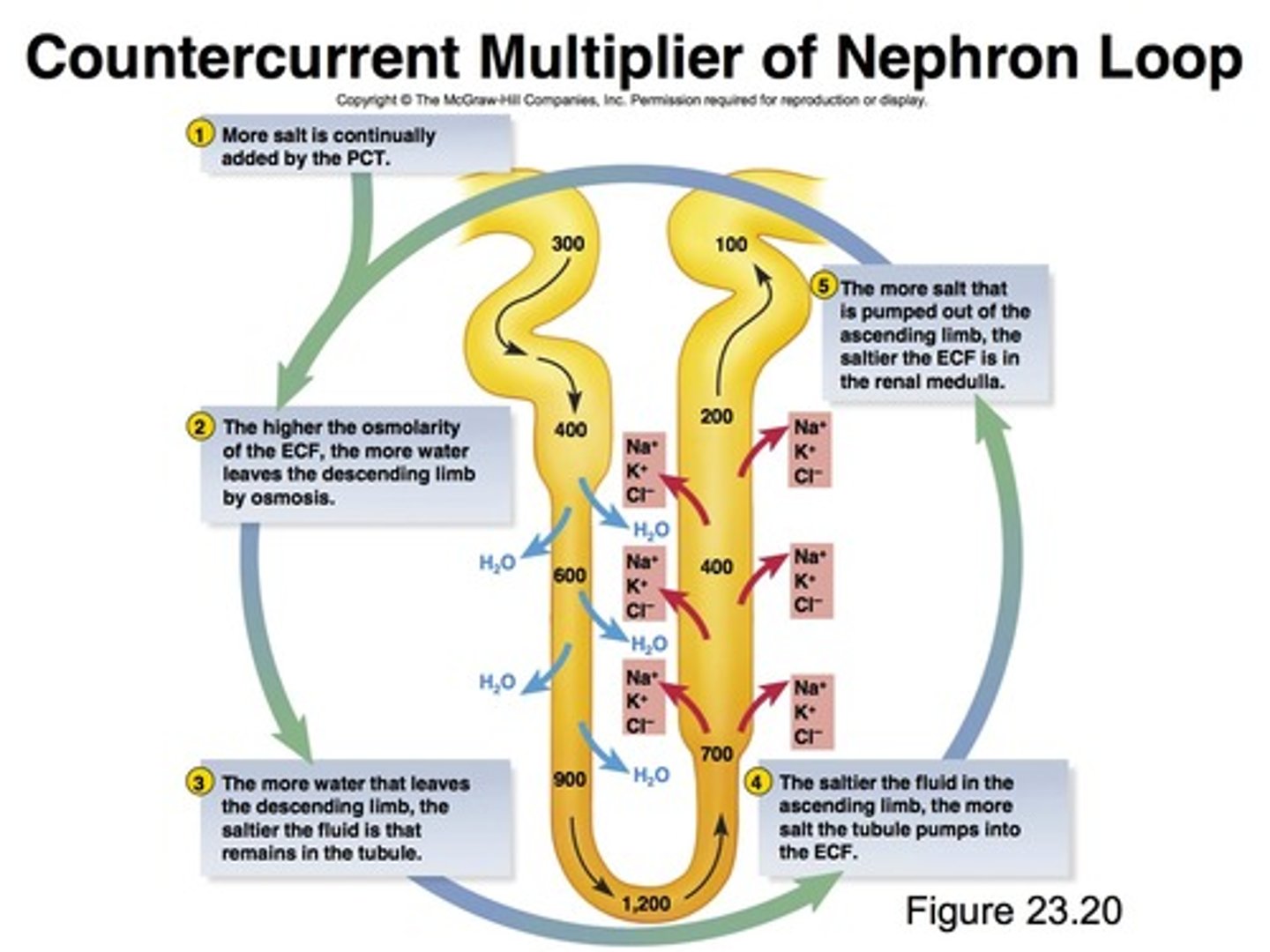
Where does countercurrent multiplication occur
ascending limb of the loop of Henle (main)
distal tubule
can also occur in the collecting duct
definition of countercurrent multiplication
A countercurrent mechanism system is a mechanism that expends energy to create a concentration gradient.
countercurrent exchange
the relationship of the opposite flow of the nephron and the vasa recta
What is the role of the vasa recta
-the descending vasa recta will provide blood and nutrients to the nephron
-the ascending vasa recta will collect waste from the nephron
Describe the flow of the nephron and the vasa recta
-they flow in OPPOSITE directions
-the nephron has the descending limb on the left and the ascending limb on the right
-the vasa recta will have its ascending limb on the left and its descending limb on the right
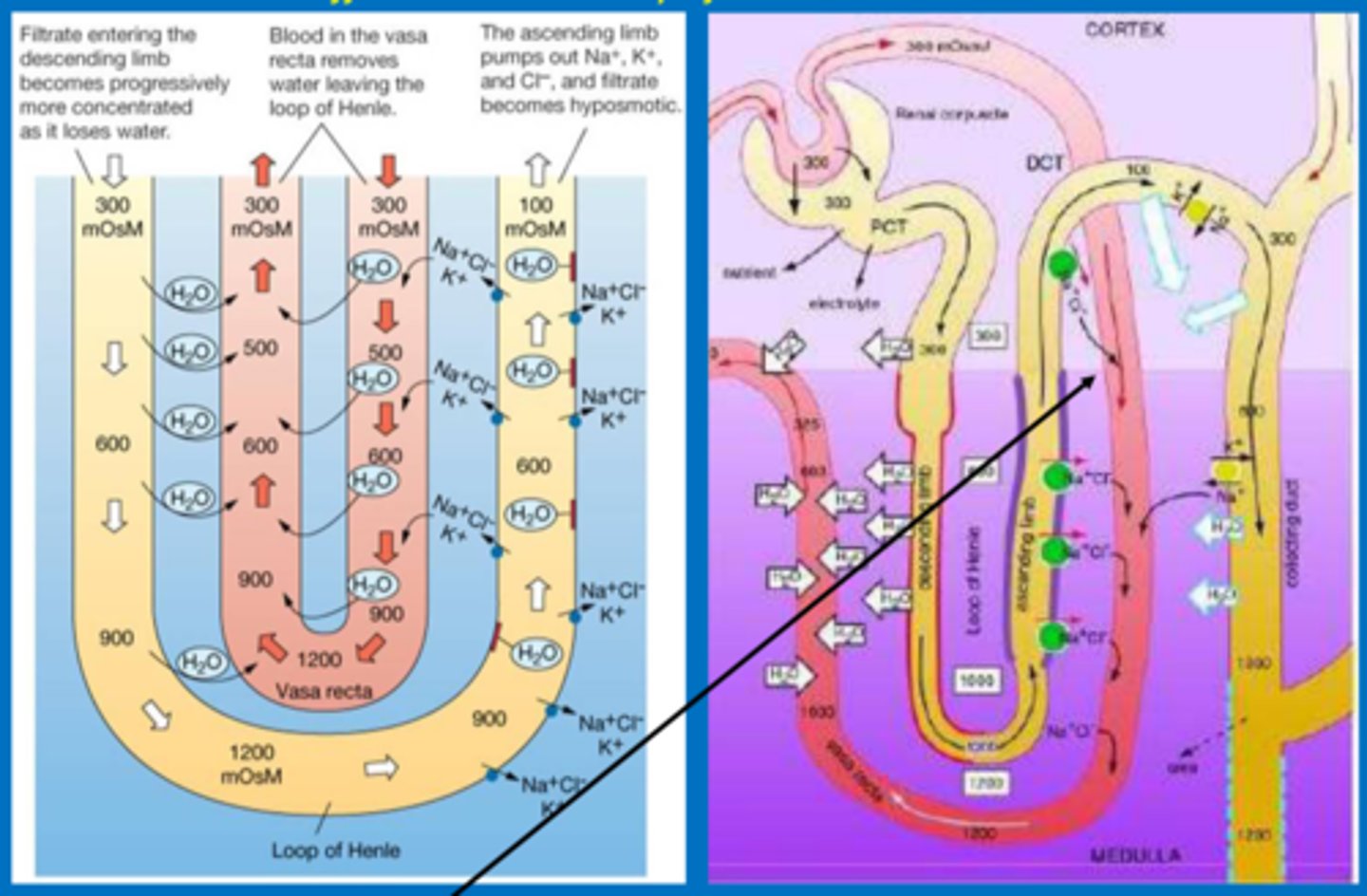
describe the ascending portion of the vasa recta
-the ascending portion will collect waste from the nephron
-it will collect water and get rid of NaCl
describe the descending portion of the vasa recta
-the descending portion of the vasa recta will supply nutrients to the nephron
-it will take up NaCl and get rid of water
Where is the equilibrium of the vasa recta located? what is the effect of this?
-equilibrium is located on the 1st 1/3 of the vasa recta as it moves up
-because the equilibrium is not at the hairpin turn, it will take away some water and NaCl but it mainly takes away the metabolic waste products that were made by the loop of Henle
What does the vasa recta arise from?
the efferent arteriole
describe functions that occur at the proximal tubule
-all glucose and amino acids are reabsorbed
-67% of water, NaCl, K+, etc are reabsorbed
-main function: reabsorption of Na+ and water
what is the key transporter of the PCT and where is it located?
Na/K+ ATPase that is bound in the basolateral membrane
describe what is reabsorbed at the descending thin limb of the loop of Henle
-water is reabsorbed (through aquaporin 1 channels)
-little NaCl is reabsorbed
describe what is reabsorbed at the thin ascending limb of the loop of Henle
-it is impermeable to water; therefore no water can be reabsorbed into the blood
-it will resorb NaCl passively
describe what is reabsorbed at the thick ascending limb of the loop of Henle
-it is impermeable to water; therefore no water can be reabsorbed into the blood
-it has a lot of NKCC transporters so NA+, K+, and Cl- can be reabsorbed
-it also has a Na+/H+ anti porter
-resorbs NaCl passively
which segment is often called the "diluting segment" of the nephron
thick ascending limb of the loop of Henle (TAL)
describe what is reabsorbed at the distal tubule
-the early segment of the distal tubule is impermeable to water
-it will reabsorb 7% of filtered
-it has a Na+/Cl- symporter that pumps NaCl out of the tubule and into the blood to be reabsorbed
Where is most of the calcium reabsorbed
at the proximal tubule
role of PTH and how it achieves its role
main goal: wants to increase serum calcium and decrease serum phosphate. it does this by:
1. increasing the amount of calcium reabsorbed at the TAL and distal tubule
2. increasing the amount of phosphate excreted by the kidney (by decreasing the amount of phosphate reabsorbed at the proximal tubule)
3. activating vitamin D3 in order to increase the amount of calcium absorbed from the GI tract
4. bone resorption: breaks down bone
how is vitamin D3 activated by PTH?
PTH actually activates 1-alpha-hydroxylase
1. the 1-alpha hydroxylase is used to add an OH to the 1 position of 25OH- vit D
2. this now forms 1,25 OH -vit D (the active form od vitamin D)
-this occurs in the kidney
role of 1,25 OH Vit D
this is the active form of vitamin D
1. will synthesis calbindin D
2. this allows the distal tubules of the kidney to reabsorb calcium
3. it also allows the GI tract to absorb more calcium
What stimulates the release of PTH?
low serum calcium
why do you not want to reabsorb PO4 when you activate PTH?
if you reabsorbed Ca and PO4 they would complex together to form hydroxyappetite and would get payed down as bone--> you still would not increase serum calcium
calcitonin
(role, when it is released, what releases it)
-is released when serum calcium levels are too high
-it will cause more calcium to be excreted in the urine and for bone formation
-it is released by the thyroid
how is filtered calcium reabsorbed?
90% of filtered calcium is reabsorbed by being coupled to Na+ reabsorption
describe the reabsorption of phosphate under normal circumstances
85% is reabsorbed at the proximal tubule (couple to Na+)
15% is excreted in the urine
note: distal sections of the nephron DO NOT reabsorb phosphate
phosphatauria
-increased phosphate in the urine
-due to elevated PTH
describe your body's response to dehydration
1. water deprivation
2. increased plasma osmolarity
3. this stimulates osmoreceptors in the anterior hypothalamus
4. ADH secretion from the posterior pit increases
5. increased permeability to water at the distal tubule and collecting duct
6. increased water reabsorption at the collecting duct and distal tubule
7. this will cause an increase in urine osmolarity and a decrease in urine volume
8. your plasma osmolarity will decrease back to normal
-you will also have increased thirst and increased water drinking that will restore plasma osmolarity back to normal
describe your body's response to water excess
1. water excess
2. decreased plasma osmolarity
3. this stimulates osmoreceptors in the anterior hypothalamus
4. ADH secretion from the posterior pit decreases
5. decreased permeability to water at the distal tubule and collecting duct
6. decreased water reabsorption at the collecting duct and distal tubule
7. this will cause an decrease in urine osmolarity and a increase in urine volume
8. your plasma osmolarity will increase back to normal
-you will also have decreased thirst and decreased water drinking that will restore plasma osmolarity back to normal
general definition of a diuretic
it is an agent that will cause increased urine flow
4 main groups of diuretics
1. things that increase GFR are MILD diuretics
2. substances that inhibit ADH
3. excess osmotically active particles
4. renal transport inhibiting substances
what is the role of alcohol and urination
alcohol will inhibit your ADH (therefore you pee more)
4 main types of diuretics
1. carbonic anhydrase inhibitors
-example: acetazolamide
2. loop diuretics
-example: furosemide
3. thiazide diuretic
-example: chlorothiazide
4. K+ sparing diuretics
-example: amiloride
furosemide
-loop diuretic
-inhibits the NKCC transporter in the TAL
chlorothiazide
-thiazide diuretic
-it inhibits the Na/Cl cotransporter in the distal tubule
amiloride
-K+ sparing diuretic
-inhibits Na+ channel and inhibits K+ secretion