oral health
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
136 Terms
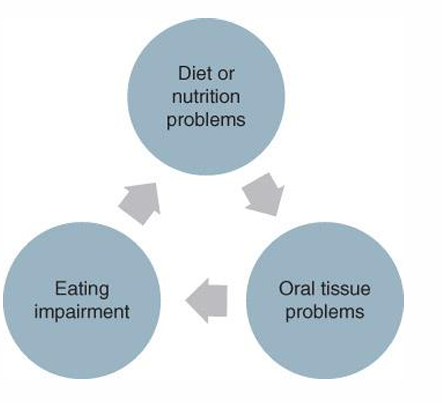
why can problems in the mouth can impact diet and nutrition status
because the oral cavity is the pathway to the rest of the body
nutrition and oral health have what type of relationship
synergistic
how do nutrition and oral health have a synergistic relationship? (3)
Adequate nutrition is essential for all tissues
Oral disease can impact ability to eat
Poor nutrition status can increase risk for oral disease
health issues effected by gingivitis and periodontitis? (5)
CVD
stroke
Endocarditis (inflammation of the heart inner lining)
Pneumonia
Premature birth and low birth weight
interrelationship between nutrition and oral health
development of oral cavity (gestation)
Primary teeth develop around 6 weeks gestation
Mineralization begins around 3-4 months' gestation
development of oral cavity (infancy/childhood)
Tooth eruption varies, usually around 6 months of age
Majority of primary teeth erupt by 2-3 years
development of oral cavity (adolescents)
Most permanent teeth erupt by 16 years of age
what are the parts of the tooth
enamel
dentin
pulp and nerve supply
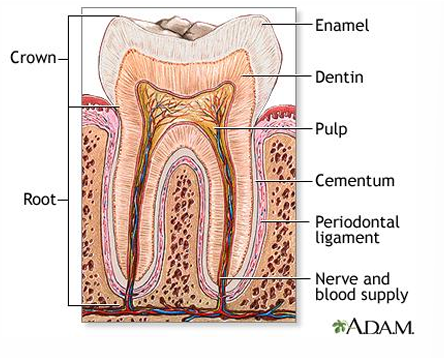
what is enamel
hard mineralized surface of the tooth
what is dentin
boddy tissue forming the bulk of the tooth beneath the enamel
what are dentin and enamel made of?
hydroxyapatite (calcium and phosphorus crystalline structure)
what is more resistant than hydroxyapatite
fluorapatite (forms when fluoride is available)
what deficiencies/conditions are associated with hypomineralization and enamel hypoplasia
vit D, vit A, and malnutrition
what deficiencies/conditions are associated with salivary gland atrophy
vit A deficiency and malnutrition
salivary gland atrophy can impact what
health of teeth
poor oral health can impact what (3)
food choices
nutrition status
overall health
mouth pain can lead to what
decreased intake
mouth pain can lead to decreased intake why? what do most do?(2)
opt for foods that are easier to chew
foods low in nutritional quality
oral tissue turnover (how long)
3-7 days
where to we see the earliest clinical manifestations of nutrition/health issues (where in the body)
in the oral cavity first
which deficiencies are seen more readily in the oral cavity?
water-soluble vitamins, protein, iron
lip, tongue, gum signs and what they indicate? (graph)
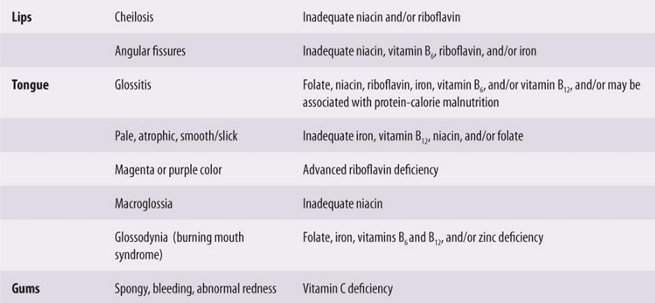
angular fissures are what
cheilosis is what

DENTAL CARIES (CAVITIES)
dental caries is most common what? (2)
one of the most common infectious diseases
most common chronic disease of childhood
dental caries form how? why? (simple)
slow progression and is multifactorial
caries impact life how long?
lifetime burden as once a tooth is infected, it requires restoration and maintenance throughout life
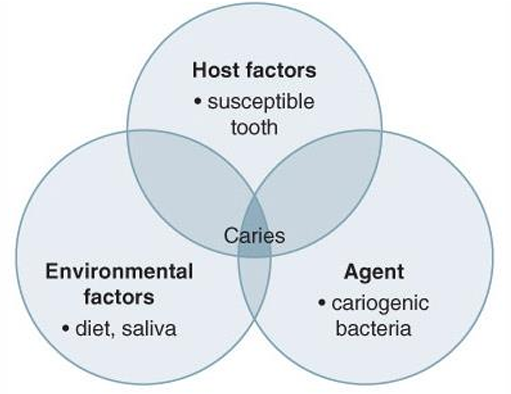
model of etiologies of dental carries (host, environmental, agent)
host is the susceptible tooth
agent is the cariogenic bacteria
environmental factors is diet and saliva
what does cariogenic bacteria cause
plaque
what causes caries generic)
multifactorial
caries form due to interaction between what 3 things
Host (tooth)
Agent (plaque)
Environment (diet and saliva)
what is plaque
colonized bacteria on tooth surfaces
what does plaque do
causes enamel to demineralize (because it is on the enamel surface)
how does plaque impact teeth (what does it cause and how)
the cariogenic bacteria in the plaque metabolized fermentable CHO —> acid is produced—> pH below 5.5—→ demineralization of enamel
what pH is risk for teeth
5.5 or below
pH of 5.5 of below causes what
demineralization of enamel —→ removes minerals from tooth—> can penetrate into bloodstream
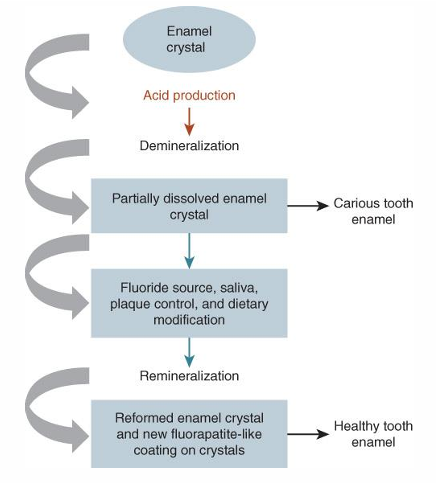
steps in carie formation (2)
demineralization of enamel (reversible)
bacterial invade the tooth (not reversible)
demineralization of enamel, if halted can be
reversed
define remineralization
body’s natural repair process in which calcium and phosphorus from saliva rebuild the enamel
where does the calcium and phosphorus come from?
saliva (which is why it so important)
once bacteria invade tooth, what must occur
tooth restoration is required
demineralization and remineralization process
crystal enamel
acid is produced —> demineralization
partially dissolved enamel crystals —→ tooth caries OR
fluoride source, saliva, plaque control, and diet mods —→ remineralization
reformed enamel crystals and new flourapatite-like coating on crystals
healthy tooth enamel
etiology of dental caries (what is the root causes)- 4
susceptible tooth
microorganisms
substrate- dietary factors
foods
how can foods be etiology to dental caries (what factors does it depend on)
composition of the food (cariogenic foods)
amount
frequency and duration of exposure
form and consistency
food combinations
when we talk about a susceptible tooth, what do we look at (4)
composition of the tooth and enamel
tooth location
pits and fissures in tooth crown
quantity of saliva
microorganisms do what that is at risk for caries
metabolize fermentable CHOw
what 3 bacteria metabolize fermentable CHO
streptococcus mutans
streptococcus sanguis
lactobacillus
when we talk about dietary factors, what is of concern
carcinogenicity
carcinogenicity refers to what?
caries-promoting properties of a diet or food
what does carcinogenicity depend on (4)
composition of food
amount of CHO consumed
frequency and duration of CHO exposure
form and consistency of food consumed
what are cariogenic foods
food with fermentable CHO
what type of foods are low in carcinogenicity
starch foods
when is caries promoting potential increased (based on food) (3)
when finely ground, heat treated, high in sucrose
examples of cariogenic foods
Examples: pretzels, crackers, white bread, chips, and crackers (sticky-can stay in mouth)
Fruit drinks, soda, sweetened teas, sugar-sweetened beverages, and sweetened dairy product
why are some starchy foods or sweet foods cariogenic, and others are less?
cariogenic bacteria metabolize ALL SIMPLE CHO but time retained in the mouth INCREASES CARIOGENICITY of ALL CHO containing foods
when can fruits be of lower carcinogenicity
if part of a mixed meal
if high water content (watermelon < banana)
role of dietary fiber
can stimulate the production of saliva (decreases time in contact with tooth)
role of non-carb components of food
can modulate the cariogenic potential of food
what is cariostatic foods
those that
do not contribute to decay
not metabolized by microorganisms
do not cause pH drop to <5.5 in 30 minutes
examples of cariostatic foods (3 categories)
protein foods
fats and oils
nonnutritive sweeteners
what are anti-cariogenic foods
those that PREVENT plaque from recognizing cariogenic foods
examples of anti-cariogenic foods (3 main categories)
cow’s milk and aged cheese (dairy)
xylitol (inhibit streptococcus mutans)
chewing gum
cows milk and aged cheese role in caries
prevent due to casein, calcium, and phosphorus content
xylitol prevents plaque/caries how
inhibits streptococcus mutans
food amount and caries
strong association between amount of sugar and caries risk
frequency and duration of exposure AND caries
Foods retained in the mouth for longer increase caries risk
Foods that are quickly eliminated from the mouth are less damaging
food combinations role is caries
certain combinations can enhance or prevent caries
remineralization is enhanced when cariogenic foods are eaten with
dairy products
Cariogenic foods and beverages are less cariogenic when consumed with
anticariogenic foods or consumed with a meal
how does sequence of food impact caries risk
eating acidogenic foods between cariostatic or anticariogenic foods can lower risk
so eating protein —> carb/sugar —> protein/fat (example)
what 6 things can increase caries risk (table)
frequent or prolonged meal snacking
frequent of prolonged between meal-sipping (sweetened drinks)
frequent in-between meal use of cariogenic foods (desserts)
chewing sugar sweetened gum
slowly dissolved hard candies (breath mints, cough drops, jolly ranchers)
eating sticky foods like dried fruits or fruit rolls ups
what 6 things can decrease caries risk
limiting snacking to 2-3 times a day
drinking sweetened or acidic beverages instead of sipping (limit carbonated drinks to meal times only)
having sweets with meals rather than between meals
chewing sf gum (xylitol)
consuming fruits, vegetables, dairy products, and nuts as snacks
using water frequently to clean mouth of food debris
we can do what to our diet to reduce caries risk
manage it
how can we manage our diet to reduce caries risk (like what would diet look like)
balanced diet
modify fermentable CHO
snack on cariostatic or anticariogenic foods
chew sf gum
have sweets with meals
how can we control plaque
brush and floss teeth daily
what mineral can be used to aid oral health
flouride
basic oral hygiene is linked to
whole body health
diseases/condition linked to oral health problems
diabetes, osteoporosis, HIV/AIDS, Alzheimer's disease, others
components of good oral hygeine (4)
brush teeth 2x a day for 2 mins —> flouridated toothpaste and soft brush
interdental cleaning (flossing) 2x day
brush tongue
visit dentist regularly
what has been seen to help reduce caries in 5-16 year olds
supervised consumption of chewing gum sweetened with sucrose-free polyol (xylitol only or polyol combinations) for 10-20 minutes after meals
how does fluoride prevent and control dental caries (4)
Inhibit tooth demineralization
Enhances tooth remineralization
Is released from plaque in response to lower mouth pH
Fluoride in dental plaque interferes with acid production by inhibiting essential enzyme activity
what is systemic flouride?
Occurs through supplements or dietary intake of fluoride (absorbed into blood and deposited to bones and teeth)
when is systemic fluoride seen to be beneficial to
from birth until all teeth erupted
benefits children
what is topical fluoride
fluoride added directly onto teeth
when is topical fluoride most effective for
after teeth have erupted
adults and children benefit
fluoride sources
fluoride containing toothpaste, oral fluoride rinses, gels, and foams
Fluoridates drinking water and toothpaste are the most fluoride sources
water and fluoride
Community water fluoridation reduces childhood dental caries by up to 40%
when should one recommend dietary fluoride supplements
ONLY for children at high risk for caries development AND whose primary water source is not fluoridated
done under pediatric dentist supervision
what to consider before recommending fluoride supps
Determination of fluoride level of primary drinking water
Potential sources of dietary fluoride
Caries risk
what is fluorosis
ingestion of excessive fluoride when teeth are still developing which can lead to defective mineralization
why children should not eat toothpaste :)

PERIODONTAL DISEASE
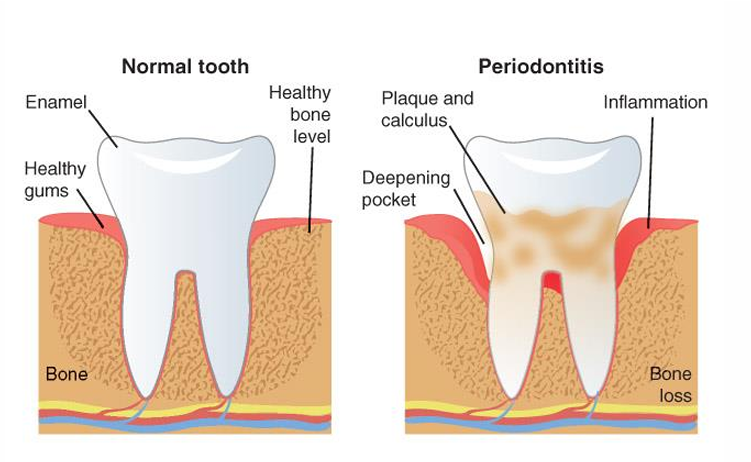
what is periodontal disease
gum disease ; chronic infection of the hard and soft tissue supporting the teeth

periodontal disease is characterized by
gingival recession and bleeding, formation of deep pockets, and loss of bone-supporting teeth (inflammatory process)

what are the 2 types of periodontal disease
gingivitis and periodontitis
what is gingivitis
Common, mild, and reversible from of periodontal disease
Characterized by infected, red, swollen, and bleeding gums
what is periodontitis
Chronic inflammatory disease of supportive tissue of the teeth
Characterized by red, swollen, bleeding gums, teeth with exposed tooth surfaces, and bone loss
what are the factors that cause periodontal disease (3)
microbial
genetic
lifestyle
microbial factors do what (periodontal disease)
Oral bacteria colonize the subgingival pocket and form dental plaque
Progression and severity depend on the virulence of the plaque bacteria and host immune response