pneumonia pathology
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
Classification of pneumonia
CommunityAcquired Bacterial Pneumonia
CommunityAcquired Viral Pneumonia
Nosocomial Pneumonia
Aspiration Pneumonia
pneumonia in immunocompromised patients
Necrotizing pneumonia and pulmonary abscess
Chronic pneumonia
community acquired bacterial pneumonias usually follow
viral upper respiratory tract infection
what is the most common cause of CAP (lobar pneumonia)
Streptococcus pneumoniae
other common causes of CAP
Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, Legionella pneumophilla, Mycoplasma pneumoniae, and Pseudomonas aeruginosa.
Haemophilus influenza causes which type of pneumonia
Encapsulated and unencapsulated forms of H. influenzae are important causes of community-acquired pneumonia.
encapsulated H.influenza in children
cause a particularly life threatening form of pneumonia in children, often after a respiratory viral infection.
which adults are at risk of H.influenza pneumonia
those with chronic pulmonary diseases such as chronic bronchitis, cystic fibrosis, and bronchiectasis.
H. influenzae is the most common bacterial cause of
acute exacerbations of COPD
Staphylococcus aureus causes
secondary bacterial pneumonia in children and healthy adults after viral respiratory illnesses (e.g., measles and influenza in children and adults).
Staphylococcus aureus complications
lung abscess and empyema.
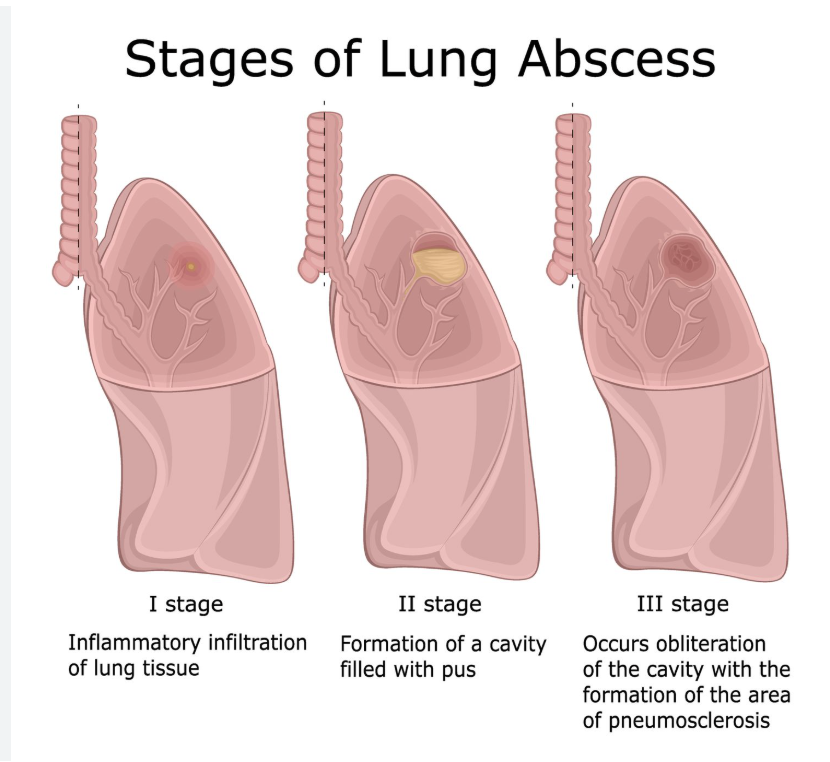
Lung abscess is defined as necrosis of the pulmonary tissue and formation of cavities containing necrotic debris or fluid caused by microbial infection
empyema
collection of pus in pleural cavity
who is at more risk of staphylococcus aureus pneumonia
right-sided staphylococcal endocarditis is a serious complication of intravenous drug abuse.
M. catarrhalis causes pneumonia in
older adults
M. catarrhalis causes
-acute exacerbation of COPD in adults (second most common cause of it).
-otitis media (infection of the middle ear) in children.
other organisms causing otitis media infections
S. pneumoniae and H. influenzae, M. catarrhalis
Klebsiella pneumoniae is the most frequent cause of
gram-negative bacterial pneumonia.
klebsiella related pneumonia affects
debilitated (weak) and malnourished individuals, particularly chronic alcoholics.
klebsiella characteristic feature
Thick and gelatinous sputum is characteristic because the organism produces an abundant viscid capsular polysaccharide, which the patient may have difficulty coughing up.
Pseudomonas aureginosa present in patients in
Typically a nosocomial pathogen, but can also be seen in association with cystic fibrosis
• Patients with neutropenia (chemotherapy)
• Extensive burns
p.aeroguinosa mortality rate
Pseudomonas bacteremia is a fulminant (severe and sudden) disease, with death often occurring within a matter of days.
P.aeroguinosa histology
Histologic examination reveals organisms invading the walls of necrotic blood vessels (Pseudomonas vasculitis), leading to secondary coagulative necrosis of the pulmonary parenchyma.
P.aeroguinosa invasion
P. aeruginosa has a propensity to invade blood vessels at the site of infection, with consequent extrapulmonary spread.
Legionella pneumophila related disease
Pontiac fever
Pontiac fever
self-limited upper-respiratory tract infection caused by L. pneumophila, without pneumonic symptoms.
Legionella pneumophila flourishes in
artificial aquatic environments, such as water-cooling towers and within the tubing system of domestic (potable) water supplies.
Legionella pneumophila mode of transmission
inhalation of aerosolized organisms or aspiration of contaminated drinking water.
Legionella pneumophila susceptible people
individuals with predisposing conditions such as cardiac, renal, immunologic, or hematologic disease. Organ transplant recipients are particularly susceptible.
Legionella pneumophila prognosis
may be quite severe, frequently requiring hospitalization and producing a fatality rate of 30% to 50% in immunosuppressed individuals.
diagnosis of Legionella
Rapid diagnosis is facilitated by demonstrating Legionella antigens in the urine or by a positive fluorescent antibody test on sputum samples; culture remains the standard diagnostic modality. PCR-based tests can be used on bronchial secretions in atypical cases.
Morphologic changes in pneumonia
- lobular bronchopneumonia and lobar pneumonia distribution
-consolidation= replacement of the air by exudate in the alveoli.
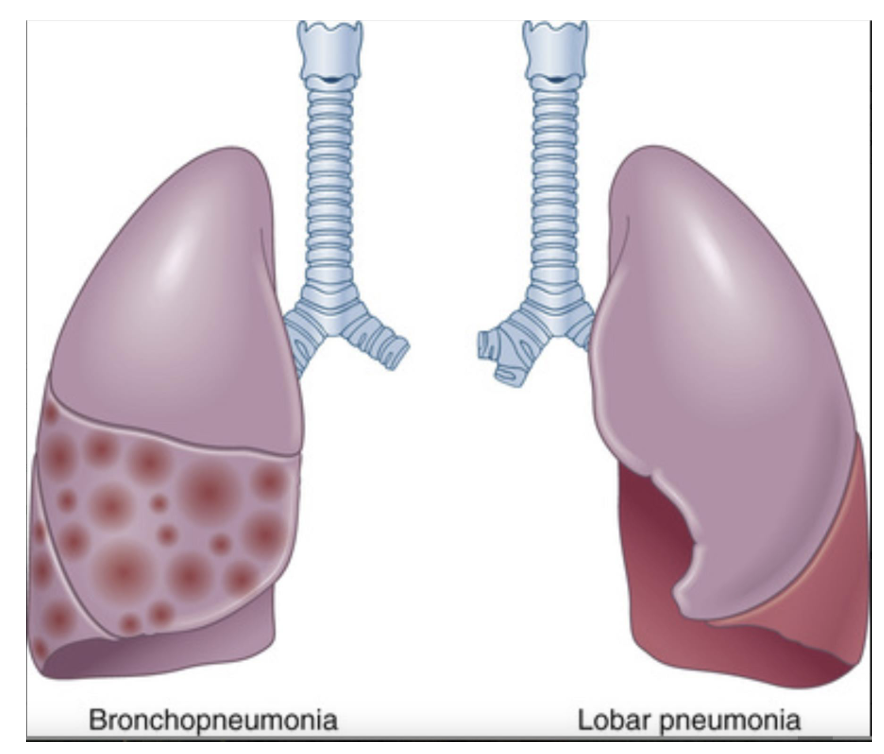
Bacterial pneumonia has two patterns of anatomic distribution:
lobular bronchopneumonia and lobar pneumonia.
lobular bronchopneumonia
Patchy consolidation of the lung is the dominant characteristic of bronchopneumonia
neutrophil-rich exudates that fill the bronchi and bronchioles and spill over into the adjacent alveolar spaces only.
lobar pneumonia.
consolidation of a large portion of a lobe or an entire lobe defines lobar pneumonia.
what is consolidation
refers to “solidification” of the lung due to replacement of the air by exudate in the alveoli.
Four stages of lobar pneumonia
-Congestion
-Red hepatization
-Grey hepatization
-Resolution
Congestion
heavy lung; vascular dilatation, intra-alveolar fluid with few neutrophils, and often the presence of numerous bacteria
Pathology: Alveolar capillaries dilate, leading to increased blood flow and fluid exudation into alveoli.
Microscopy: Alveoli contain serous fluid, bacteria, and few neutrophils.
Red hepatization
massive confluent exudation, as neutrophils, red cells, and fibrin fill the alveolar spaces
Pathology: Exudation of fibrin, red blood cells (RBCs), and neutrophils into alveoli. The lung appears red and firm, resembling the liver.
Microscopy: Numerous RBCs, neutrophils, and fibrin in alveolar spaces.
Grey hepatization
progressive disintegration of red cells and the persistence of a fibrinosuppurative exudate
Pathology: RBCs break down, leaving a gray, firm lung. Neutrophils persist, and fibrin deposition increases.
Microscopy: Fewer RBCs, more neutrophils and macrophages, heavy fibrin deposits.
Resolution
exudate within the alveolar spaces is broken down by enzymatic digestion to produce granular, semifluid debris that is resorbed, ingested by macrophages, expectorated, or organized by fibroblasts growing into it
Pathology: Macrophages clear fibrin and debris, restoring normal lung function.
Microscopy: Predominantly macrophages, minimal fibrin.
pores of kohn
openings allowing communincation between alveoli
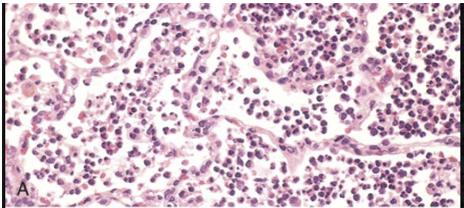
The congested septal capillaries and extensive neutrophil exudation into alveoli correspond to early red hepatization. Fibrin nets have not yet formed.
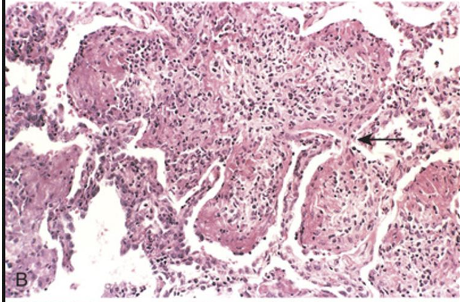
Early organization of intraalveolar exudates, seen in areas to be streaming through the pores of Kohn (arrow).
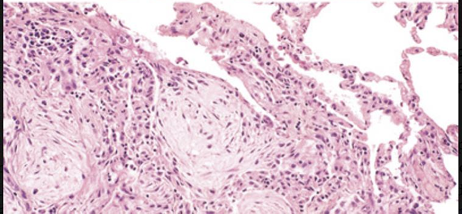
Advanced organizing pneumonia, featuring transformation of exudates to fibromyxoid masses richly infiltrated by macrophages and fibroblasts.
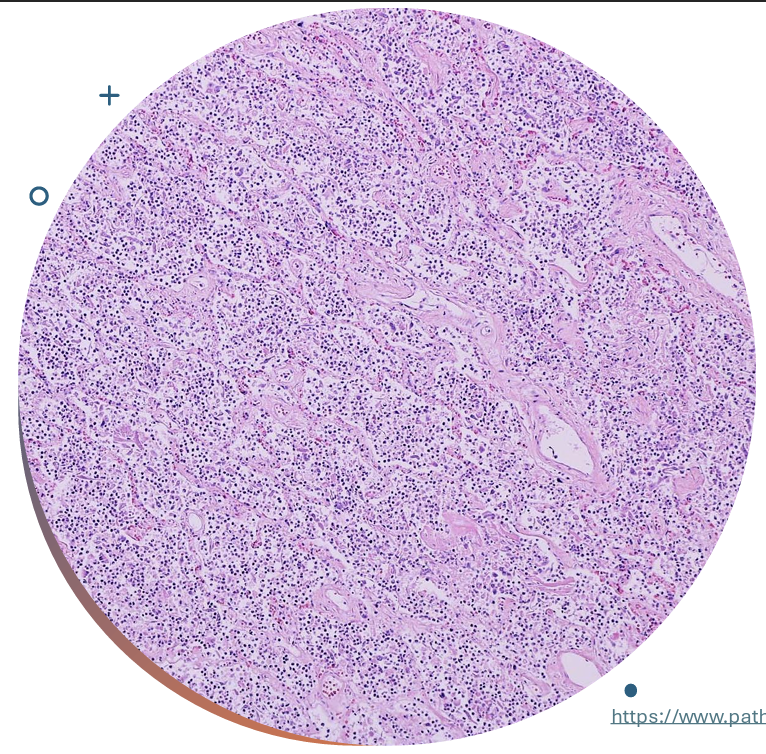
intra-alveolar neutrophilic infiltrate (in virus no exudate in alveolar space)
Microscopic findings in bacterial pneumonia
The alveolar exudate of neutrophils is seen mainly.
The surrounding alveolar walls have capillaries that are dilated and filled with RBCs.
Such an exudative process is typical for bacterial infection. This exudate gives rise to the productive cough of purulent yellow sputum seen with bacterial pneumonias.

The pattern of patchy distribution of bronchopneumonia is seen.
The consolidated areas here very closely match the pattern of lung lobules (hence the term "lobular" pneumonia).
microbes that cause Community-Acquired Viral Pneumonias
influenza types A and B, the respiratory syncytial viruses (RSV), human metapneumovirus, adenovirus, rhinoviruses, rubeola virus, and varicella virus.
they cause which type of infection
upper respiratory tract infections (“common cold”).
characteristics of viral pneumonias
-inflammation within interstitial space (not in alveolar space)
- damage leading to necrosis of the respiratory epithelium inhibits mucociliary clearance and predisposes to secondary bacterial infections.
can viral and bacterial pneumonia be distinguished by radiology
When the process extends to alveoli, there is usually interstitial inflammation, but some outpouring of fluid into alveolar spaces may also occur, so that on chest X-ray, the changes may mimic those of bacterial pneumonia. As a result, it is not possible to distinguish bacterial and viral pneumonia based on radiologic appearance alone.
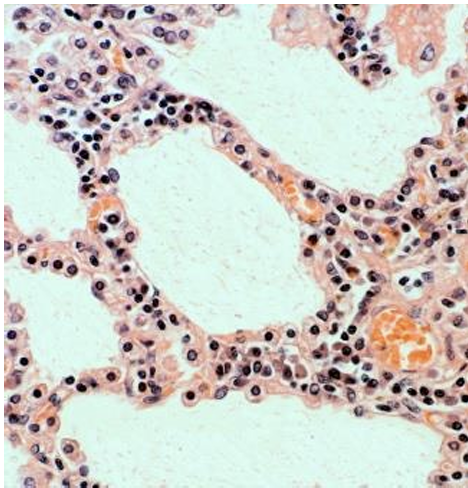
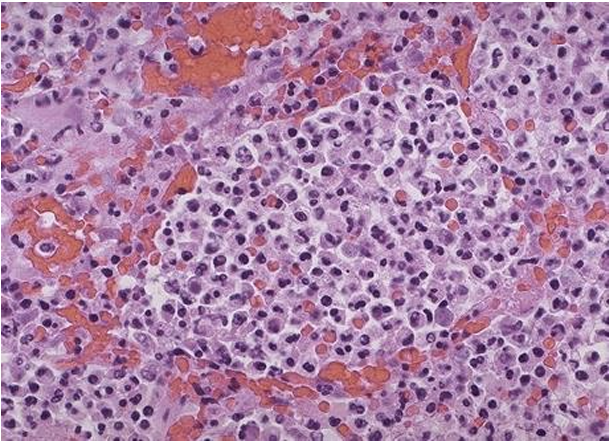
viral pneumonia
The inflammatory reaction is largely confined to the walls of the alveoli.
• The septa are widened and edematous; they usually contain a mononuclear inflammatory infiltrate of lymphocytes, macrophages, and, occasionally, plasma cells.
• In the classic case, alveolar spaces in viral pneumonia are free of cellular exudate.
• In severe cases, however, full-blown diffuse alveolar damage with hyaline membranes may develop (=diffuse alveolar damage/ARDS).
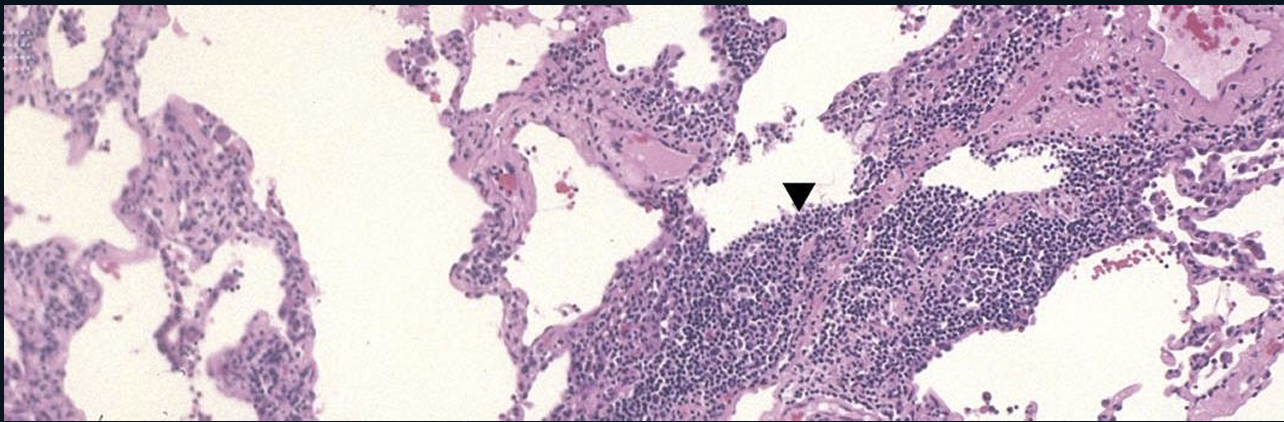
Viral pulmonary infection is characterized by interstitial lymphocytic infiltrates (▼) of small dark blue cells without a significant alveolar exudate and a productive cough.
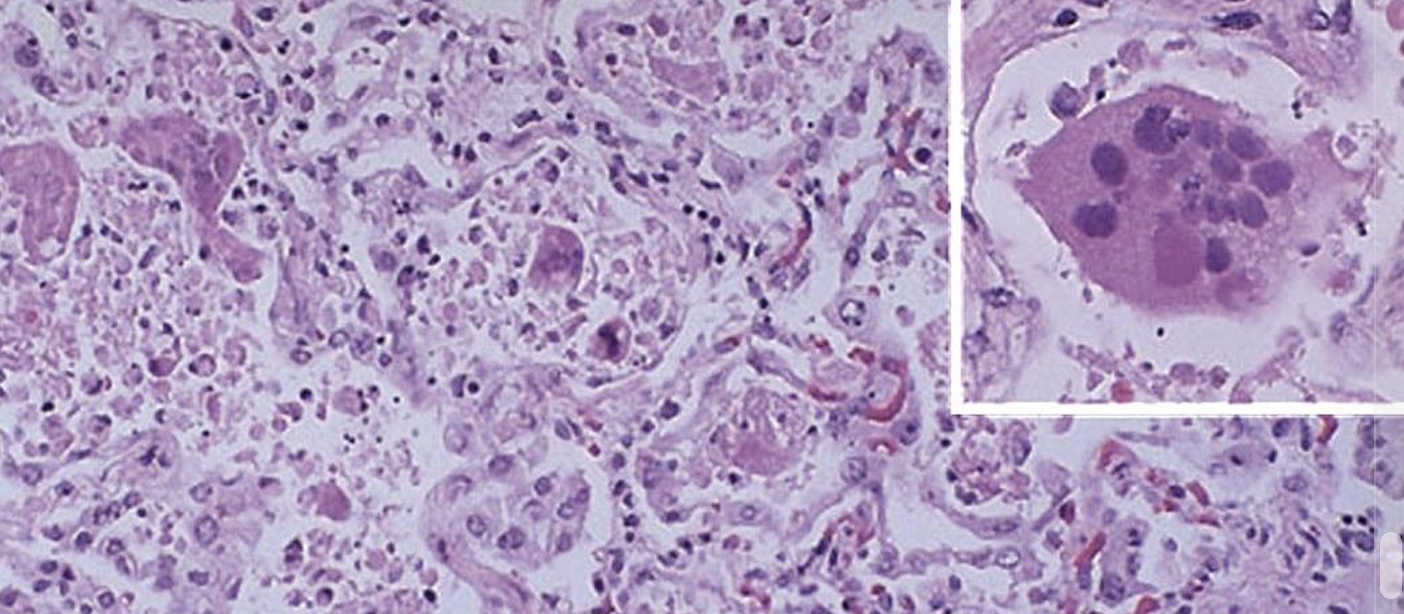
exudate with giant cells in severe case of Respiratory syncytial virus pneumonia
Hospital-Acquired Pneumonias ppl in risk
patients with severe underlying disease, those who are immunosuppressed, or those on prolonged antibiotic regimens.
• Patients on mechanical ventilation
causes of Hospital-Acquired Pneumonias
Gram-negative rods (members of Enterobacteriaceae and Pseudomonas spp.) and S. aureus are the most common isolates; unlike community-acquired pneumonia, S. pneumoniae is not a common pathogen in the hospital setting
Aspiration pneumonia occurs in
debilitated patients or those who aspirate gastric contents while unconscious (e.g., after a stroke) or during repeated vomiting.
aspiration pneumonia characteristics
The resultant pneumonia is partly chemical, due to the extremely irritating effects of the gastric acid, and partly bacterial.
aspiration pneumonia pathogenesis
Aspiration pneumonia is often necrotizing, pursues a fulminant clinical course, and is a frequent cause of death in individuals predisposed to aspiration.
In those who survive, abscess formation is a common complication.
Pneumonia in the Immunocompromised Patients caused by
-fungal infection seen in immune suppression cases
Cytomegalovirus
Pneumocystis jiroveci
Mycobacterium avium complex (MAC)
Invasive aspergillosis
Invasive candidiasis
Lung Abscess causes
Lung abscess is defined as necrosis of the pulmonary tissue and formation of cavities containing necrotic debris or fluid caused by microbial infection
Bronchial obstruction, particularly with lung cancer obstructing a bronchus or bronchiole.
Impaired drainage, distal atelectasis, and aspiration of blood and tumor fragments all contribute to the development of abscesses.
An abscess may also form within an excavated necrotic portion of a tumor.
Aspiration of gastric contents, usually accompanied by infectious organisms originating in the oropharynx.
Mycotic infections and bronchiectasis may also lead to lung abscesses.
It may be a complication of bacterial pneumonias necrotizing , particularly those caused by S. aureus, Streptococcus pyogenes, K. pneumoniae, Pseudomonas spp
causes og lung abcesses
It may be a complication of bacterial pneumonias necrotizing , particularly those caused by S. aureus, Streptococcus pyogenes, K. pneumoniae, Pseudomonas spp., and, rarely, type 3 pneumococci.
Mycotic (fungal) infections and bronchiectasis may also lead to lung abscesses.
not usually present in viral pneumonia only bacterial and fungal
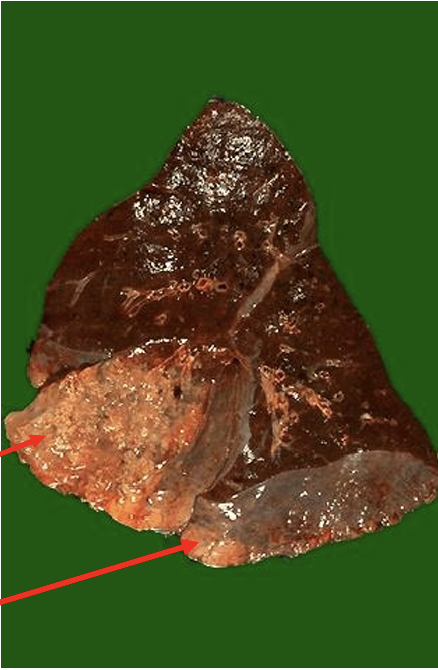
Almost the entire middle lobe of this right lung is involved by a chronic abscess as seen here on section. The area of abscess is yellow tan, and it was very firm.