(13) Intro to GI Tract, Stomach Functions, & GI Motility
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
digestive tube that extends from the mouth to the anus (considered external to the body!)
alimentary canal
The alimentary tract provides the body with what three things?
water, electrolytes, nutrients
refers to food being moved through the alimentary tract
motility
refers to food being broken down in the alimentary tract through secretion of juices
digestion
refers to digested food products being transferred into and carried away by blood circulation
absorption
What are the 4 layers of the gut starting with closest to the lumen?
mucosa, submucosa, muscularis externa, serosa
What are the two components of the muscularis externa layer of the GI tract?
circular muscle, longitudinal muscle
What is the function of the mucosa layer of the GI tract?
absorption (nutrients move across layer into the blood stream)
What is the function of the submucosa layer of the GI tract?
supplies the surrounding layers with nutrients (since it has vessels)
What is the function of the muscularis externa layer of the GI tract?
motility (muscle contraction to move things along the alimentary canal)
What does the circular muscle layer of the muscularis externa do?
constricts specific region
What does the longitudinal muscle layer of the muscularis externa do?
pushes and propels substances forward
refers to smooth muscle contracting as a single unit, such as in GI smooth muscle
syncitium
Does GI smooth muscle tend to have a higher or lower resting potential than other smooth muscles? Why?
higher, needs to have resting tone
(excited by continual intrinsic electrical activity so that there is a basal level of tone)
Why is it important that GI smooth muscle is excited by continual intrinsic electrical activity so it can have a resting, basal level tone?
so it can mix and move contents of digestive tract
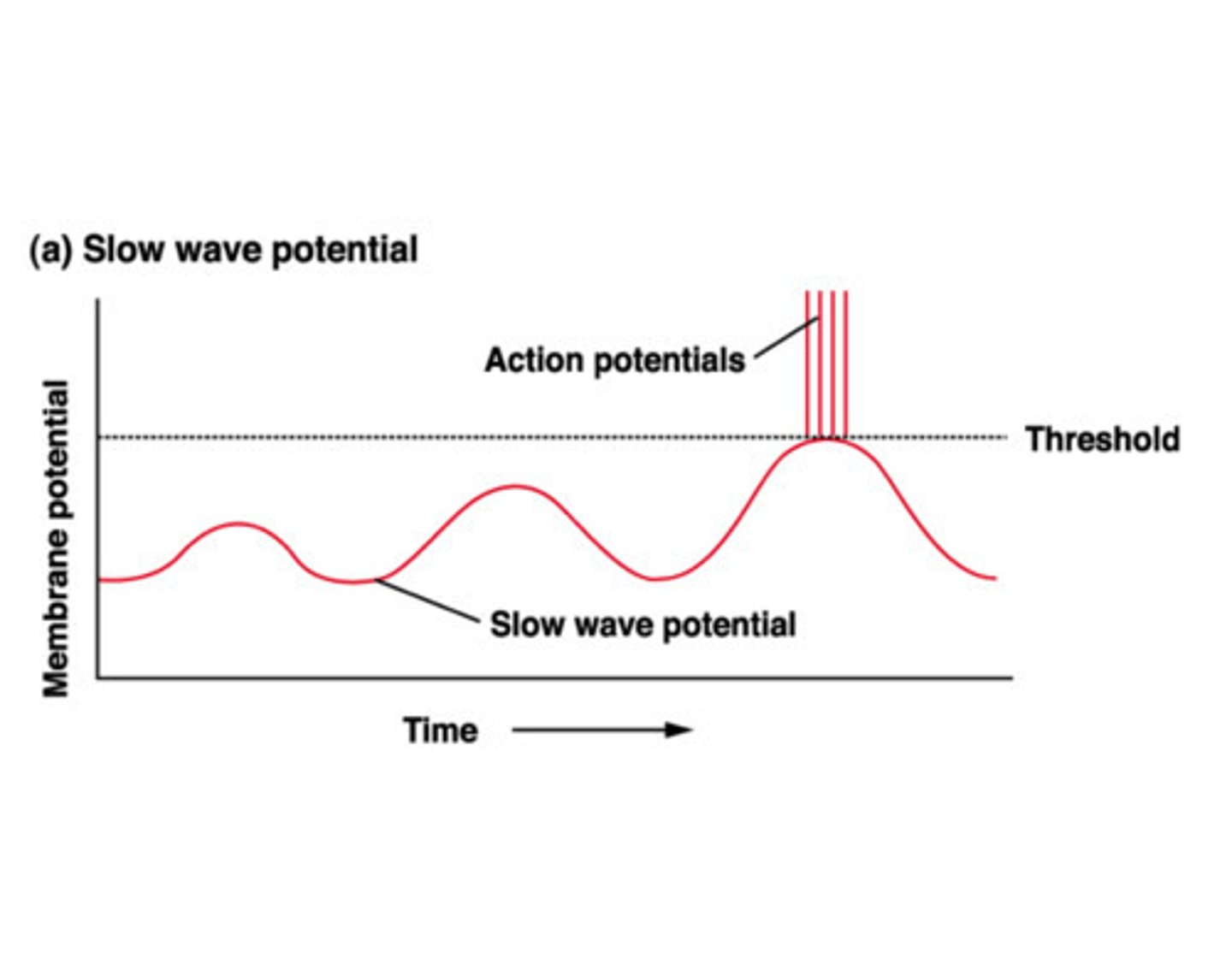
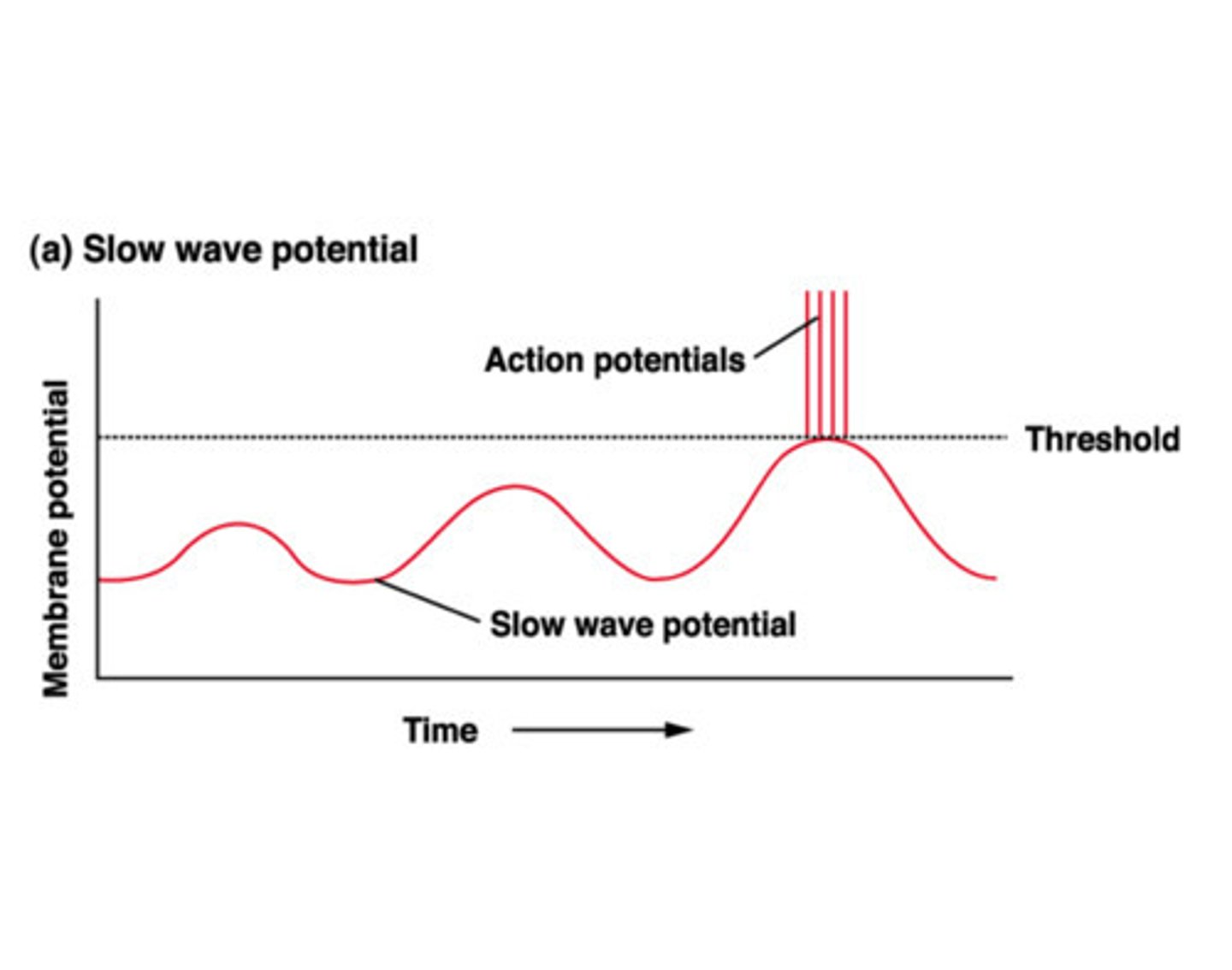
spontaneous depolarizations in GI smooth muscle that set the basal electrical rhythm (BER) of the GI tract; undulating changes in resting membrane potential that are subthreshold
slow waves
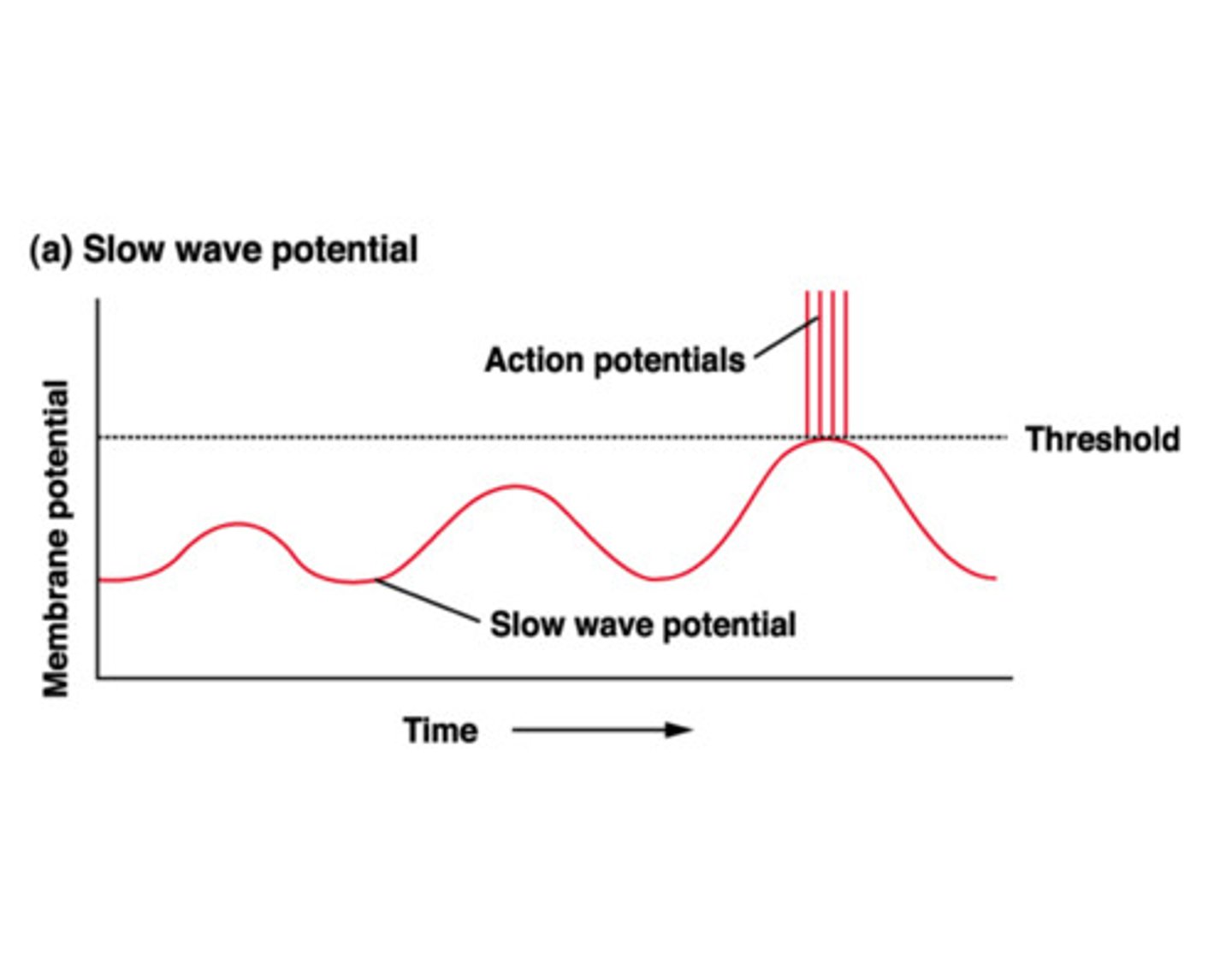
True or false: Slow waves in the GI tract are action potentials.
false
(they are subthreshold and do not usually cause muscle contraction)
non-contractile cells that initiate and maintain slow waves in the GI tract; they are pacemaker cells and experiences cyclic variations in Ca++
**these control the appearance of action potentials
interstitial cells of Cajal
What are the pacemaker cells of the GI tract?
interstitial cells of Cajal
How do action potentials (spikes) occur in the GI tract?
slow waves eventually reach threshold (which generates a series of action potentials)
refers to continuous contraction not associated with slow waves; seen in some smooth muscle sphincters of the GI tract
tonic contraction
Where are the regions where there is tonic contraction in the GI tract? (Hint: Their function is to prevent movement from one section of the GI tract to the other.)
sphincters
What causes tonic contraction in some smooth muscle sphincters of the GI tract? (3 things)
continuous entry of calcium, hormones, repeating spike potentials
What are the 4 main depolarizing factors for GI smooth muscle? (EXCITATORY)
stretching, acetylcholine, parasympathetic nerves, GI hormones
What does stretching in smooth muscle trigger?
action potentials and contraction
What neurotransmitter do intrinsic nerves secrete to get GI smooth muscle to contract?
**parasympathetic extrinsic nerves secrete this too!
acetylcholine
What are the 2 main hyperpolarizing factors for GI smooth muscle? (INHIBITORY)
norepinephrine/epinephrine, sympathetic nerves
What neurotransmitter do intrinsic nerves secrete to get GI smooth muscle to NOT contract?
**sympathetic extrinsic nerves secrete this too!
norepinephrine
What does the adrenal medulla secrete to get GI smooth muscle to NOT contract?
epinephrine
Does the parasympathetic nervous system stimulate or inhibit GI motility?
stimulate
(rest and digest)
Does the sympathetic nervous system stimulate or inhibit GI motility?
inhibit
intrinsic nervous system found within the wall of the gut along the entire length of the GI tract
enteric nervous system
True or false: The enteric nervous system can function all by itself without any other input.
true
(but it often does function in conjunction with the sympathetic and parasympathetic systems)
Is the enteric nervous system inhibitory or excitatory?
both
The enteric nervous system gets sensory input from sensory nerves with endings where?
GI epithelium
also called Auerbach's, this is the nerve network located between the longitudinal and circular muscle layers in the GI tract that controls GI contractions & movements
myenteric plexus
(myenteric = movement)
Does the myenteric plexus of the enteric nervous system stimulate or inhibit tonic contraction of the gut wall?
both
What two factors of rhythmical contractions of the GI system can the myenteric plexus modify?
intensity, rate
also called Meissner's, this is the nerve network that controls GI secretion, absorption, & blood flow
submucosal plexus
(submucosal = secretion)
GI reflexes may be triggered by what 3 receptors?
chemoreceptors, mechanoreceptors, osmoreceptors
refers to GI reflexes that are integrated entirely within the enteric nervous system
**controls secretion, peristalsis, and mixing contractions
short reflexes
refers to GI reflexes that go to the sympathetic ganglia (or CNS) and then back to the GI tract
**controls long distance signals, secretory & motor activity
long reflexes
(think about it: they're long enough that they can actually stretch back)
hormone secreted by cells in the mucosa of the duodenum and jejunum in response to fats and breakdown products of fats
**increases contractility of the gall bladder and inhibits stomach mobility
cholecystokinin (CCK)
What cells secrete CCK?
mucosal cells of duodenum and jejunum
CCK is secreted in response to what?
fatty acids in the duodenum
What are the two functions of CCK?
increase contractility of gallbladder, inhibit gastric motility
Does CCK increase or decrease contractility of gallbladder?
increase
(results in bile secretion)
Does CCK stimulate or inhibit gastric (stomach) motility?
inhibit
(once we get some food product in the small intestine, we want to inhibit stomach motility to have time to process what's in the intestine before more starts coming in)
hormone secreted by cells in the mucosa of the duodenum in response to acidic gastric juice emptying into the small intestine
**inhibits gastric mobility
secretin
What cells secrete secretin?
mucosal cells of duodenum
Secretin is secreted in response to what?
acidic chyme entering duodenum (from gastric acid release from stomach)
What is the main function of secretin?
inhibit gastric motility
(also helps stimulate the release of bicarbonate from the pancreas to help neutralize acid chyme)
Does secretin stimulate or inhibit stomach motility?
inhibit
hormone secreted by cells in the mucosa of the upper small intestine in response to fatty acids, amino acids, and carbohydrates
**can inhibit gastric mobility but main function is to stimulate insulin release
gastric inhibitory peptide (GIP)
What cells secrete GIP?
mucosal cells in upper small intestine
GIP is secreted in response to what?
food products in small intestine (fatty acids, amino acids, carbs)
What are the two functions of GIP?
inhibit gastric motility, stimulate insulin release
Does GIP stimulate or inhibit stomach motility?
inhibit
Does GIP stimulate or inhibit insulin release?
stimulate
propulsive movements in the GI tract that cause food to move forward at an appropriate rate to accommodate digestion and absorption
usual stimulus is distention of the gut, but also requires an active myenteric plexus
peristalsis
What stimulates peristalsis?
distention of the gut
Peristalsis requires what neural network in the GI tract to be active?
myenteric plexus
(as part of the enteric nervous system)
Aside from peristalsis, what is the other kind of movement in the GI tract? Why is it important?
mixing movement, mixes in enzymes to break down food for absorption
circulatory system in the GI tract that consists of the blood vessels of the GI tract, along with the spleen, pancreas, and liver
blood that supplies that GI tract, spleen, & pancreas then goes through the portal vein to the liver
splanchnic circulation
(liver can further process and filter bad things it before it all gets to systemic circulation)
Increased GI activity [increases/decreases] blood flow to the GI tract. The gut wall now starts using up a lot of oxygen, increasing the metabolic rate of that area. Circulation increases further to that area, and eventually, the oxygen concentration in the blood [increases/decreases] (since it's basically being pulled away) and results in what condition?
increases, decreases, vasodilation
Do the GI mucosa and glands secrete vasodilators or vasoconstrictors during the digestive process? What are some examples?
vasodilators, VIP (vasoactive intestinal peptide) and bradykinin
What is the only voluntary stage of ingestion of food?
deglutination (swallowing)
Ingestion 1: Food in the mouth initiates a relaxation of the jaw muscles, resulting in the jaw dropping. This is so what process (i.e. chewing) can occur?
mastication
Ingestion 2: Once the jaw drops to fit food in the mouth, the drop immediately initiates a strong reflex in the jaw muscles, resulting in what?
rebound contraction
Chewing is important because it nutrients to start to be released from what substance in fruits and vegetables?
cellulose
Chewing is important because it [increases/decreases] the surface area of the food. This makes it easier for digestive enzymes to work.
increases
Ingestion 3: In early stages of ingestion, after getting done chewing, our tongue voluntarily pushes the food back into what region?
pharynx
What is the "point of no return" for ingestion of food?
once it enters the pharynx
(from this point on, swallowing becomes entirely automatic and cannot be stopped)
Ingestion 4: Food passes through the pharynx into the esophagus. This occurs in less than 2 seconds and does what to respiration, if anything?
interrupts it
Ingestion 5a: When food is being ingested, it sends impulses to what part of the brain, which initiates a series of automatic pharyngeal muscle contractions?
brain stem
Ingestion 5b: What is the nearby region that pulls upward after ingestion of food, preventing reflex of food into the nasal cavity?
soft palate
Ingestion 5c: Movement of what two structures prevents food from entering the trachea?
vocal cords, epiglottis
Ingestion 6: As the bolus moves down the pharynx, what structure relaxes in order to allow food to move easily into the esophagus?
**at this point, the entire wall of the pharynx contracts, propelling food into the esophagus
upper esophageal sphincter (pharyngoesophageal)
Ingestion 7a: What do we call the continuation of the initial wave that began in the pharynx to move the food through the esophagus?
primary peristalsis
Ingestion 7b: What do we call the movement that results from the distention of the esophagus caused by retained food?
secondary peristalsis
Ingestion 8: The food moves through the esophagus and reaches what structure at the stomach, which normally remains tonically constricted but undergoes a receptive relaxation that allows the bolus (swallowed food) to move into the stomach?
gastroesophageal sphincter
True or false: The myenteric plexus controls GI movement.
true
(because myenteric = movement)
Which statement is incorrect?
A. The myenteric plexus is located in the submucosa.
B. The intrinsic plexuses innervate smooth muscle and exocrine and endocrine glands.
C. The plexuses are influenced by extrinsic nerves.
D. The plexuses coordinate local digestive tract activity.
E. There are two major networks of nerve fibers forming the plexuses of the gut.
A
(located between the longitudinal and circular muscle layers in the muscularis externa)