Soft Tissue injuries + Chest deformities
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
Bursa
A thin fluid filled sac located throughout the body that acts as a cushion between bones and soft tissues
Olecranon bursitis
Inflammation of the olecranon bursa
Inflammatory, infectious (septic bursitis)
Types of bursitis
trauma, prolonged pressure, break in the skin, gout, RA
Causes of Olecranon bursitis
CBC, CRP, ESR, Fluid aspiration with cell count, culture, and crystals (if concerned for infection)
A 65 y/o women reports to the clinic for elbow pain. She works as a nun and prays in the church every morning. On physical exam the elbow is red, swollen, hot, and tender. ROM is slightly decreased. What diagnostics do you want?
NSAIDs, RICE, cessation of trauma or using elbow pads, maybe aspiration with a steroid injection
A 65 y/o women reports to the clinic for elbow pain. She works as a nun and prays in the church every morning. On physical exam the elbow is red, swollen, hot, and tender. ROM is slightly decreased. CRP and ESR are elevated but all other labs are normal. What is your treatment plan?
Empiric Abx → f/u on culture, surgical I & D, maybe surgical bursectomy
What is the game plan for infectious olecranon bursitis?
Lateral epicondylitis (tennis elbow)
Overuse injury at the origin of the common extensor tendon that is more common in the dominant arm
Activity modification, RICE, NSAIDs, bracing, PT, steroid injection, surgery (IF failed 6 months of conservative)
18 y/o female presents to the clinic for elbow pain that is worsened with wrist extension. She states that she’s been playing tennis for years and is on her way to the state tournament. On physical exam you note tenderness over the extensor carpi radialis brevis muscle, decreased grip strength, and pain with passive wrist flexion. What is your treatment plan?
Medial epicondylitis (golfer’s elbow)
An overuse injury at the site of the flexor-pronator mass and effects ALL common flexor tendons except for the palmaris longis
Elbow xrays (may show osteophytes or degenerative changes but are usually normal)
18 y/o male patient presents to the clinic for elbow pain that is exacerbated by gripping. He notes that he’s just started golfing. On physical exam you note tenderness just distal to the medial epicondyle with gripping or resisted wrist flexion and pronation. What diagnostics do you want?
Cubital tunnel syndrome
Compressive neuropathy of the ulnar nerve within the medial elbow (2nd most common compression neuropathy) that can be caused by elbow dislocation, trauma, surgery, burn, or scar tissue
between the heads of the FCU and aponeurosis
Most common site of compression for cubital tunnel syndrome
EMG, NCV, MUST R/O C8 RADICULOPATHY
Patient presents to the clinic for numbness and tingling of the pinky and ring finger. She states that it is worse at night and with full elbow flexion. You note interosseous atrophy, clawing of the ring and small finger, weakness of pinch and grip, a positive tinel over the cubital tunnel. What diagnostics do you want?
NSAIDs, activity modification, night time splinting at 45 degrees
Patient presents to the clinic for numbness and tingling of the pinky and ring finger. She states that it is worse at night and with full elbow flexion. You note interosseous atrophy, clawing of the ring and small finger, a positive tinel over the cubital tunnel. What is your first line treatment?
ulnar decompression (op)
Patient presents to the clinic for numbness and tingling of the pinky and ring finger. She states that it is worse at night and with full elbow flexion. You note interosseous atrophy, clawing of the ring and small finger, weakness of pinch and grip, a positive tinel over the cubital tunnel. What is your treatment plan SINCE THERE’S WEAKNESS?
carpal tunnel syndrome
A compressive neuropathy of the median nerve at the level of the wrist that is caused by an idiopathically inflamed synovium
Female, obesity, DM, pregnancy, hypothyroidism, RA, repetitive wrist motion, trauma
Risk factors for Carpal tunnel
EMG, NCV
64 y/o female presents to the clinic for pain and numbness of her thumb, index, and middle finger that worsens at night. On physical exam you note a weakened grip, thenar atrophy, a positive phalen and tinel’s. What diagnostics do you want?
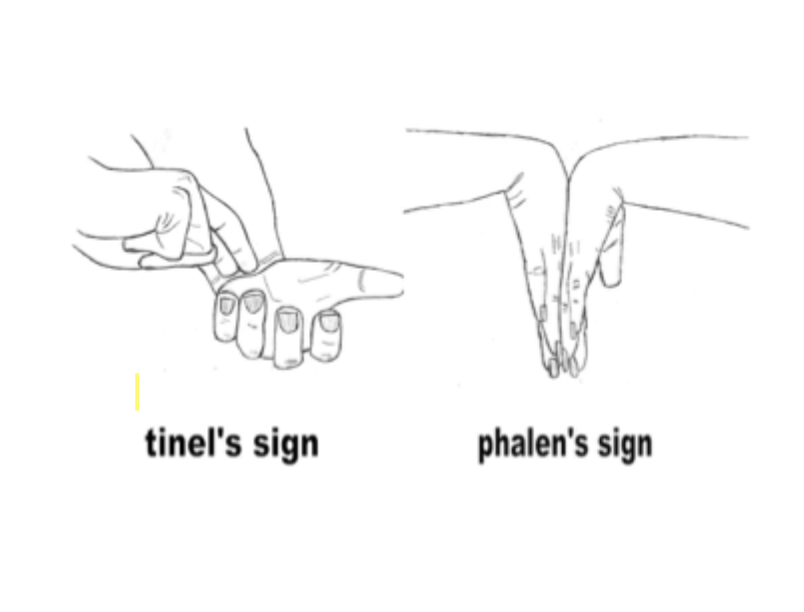
activity modification, NSAIDs, nighttime splinting, maybe steroid injections
64 y/o female presents to the clinic for pain and numbness of her thumb, index, and middle finger that worsens at night. On physical exam you note thenar atrophy, a positive phalen and tinel’s. What is your 1st line treatment plan?
Carpal tunnel release (op)
64 y/o female presents to the clinic for pain and numbness of her thumb, index, and middle finger that worsens at night. She states that she has worked as a secretary for 50 years. On physical exam you note a weakened grip, thenar atrophy, a positive phalen and tinel’s. She has failed non-op treatment. What are you doing?
Ganglion cyst (bible cyst)
A mucin-filled synovial cyst - most commonly in the dorsal carpal of the wrist (70%)
U/s (differentiate from aneurysm, guide aspiration), histopathology (shows a mucin-filled synovial sac)
A 33 y/o female presents to the clinic for a bump on her wrist. She states that she works as a hand model and “can’t go on looking like this.” On physical exam you note a firm and well circumscribed mass that is fixed into deep tissue but does transilluminate. What diagnostics you want?
Bracing and watchful waiting
A 33 y/o female presents to the clinic for a bump on her wrist. She states that she works as a hand model and “can’t go on looking like this.” On physical exam you note a firm and well circumscribed mass that is fixed into deep tissue but does transilluminate. What is your 1st line treatment?
Aspiration (avoid on volar aspect due to radial artery) 50% recurrence
A 33 y/o female presents to the clinic for a bump on her wrist. She states that she works as a hand model and “can’t go on looking like this.” On physical exam you note a firm and well circumscribed mass that is fixed into deep tissue but does transilluminate. What is your 2nd line treatment?
Severe symptoms, neurovascular manifestations
A 33 y/o female presents to the clinic for a bump on her wrist. She states that she works as a hand model and “can’t go on looking like this.” On physical exam you note a firm and well circumscribed mass that is fixed into deep tissue but does transilluminate. When would you do a surgical resection?
Trigger finger
A mechanical impingement of a flexor tendon of the hand (usually middle or ring fingers) at the A1 pulley
NSAIDs, splinting, activity modification, steroid injection at nodule
56 y/o female presents to the clinic for a “clicking ring finger.” PMHx is positive for DM. She states that her finger will get stuck in the flexed position and it POPS open when she tries to extend it. On physical exam she is tender at the A1 pulley level, and you palpate a nodule over the flexor tendon. What is your non-op treatment?
surgical release of A1 pulley (90+% success rate - often recur at other fingers)
56 y/o female presents to the clinic for a “clicking ring finger.” PMHx is positive for DM. She states that her finger will get stuck in the flexed position and it POPS open when she tries to extend it. On physical exam she is tender at the A1 pulley level, and you palpate a nodule over the flexor tendon. What is your op treatment?
Dupuytren’s contracture
A benign proliferative disorder where there is hypercellular activity and myofibroblast that develops nodule commonly affecting the palmar fascia (aponeurosis)
Hand therapy (mild), steroid injections or clostridial collagenase injections (done by a hand surgeon)
34 y/o male presents to the clinic for hand pain. On physical exam his ring finger is held in flexion and there is decreased ROM at the MCP joint. You are able to palpate a nodular band along the palm of the hand that is tender. What is your non op treatment plan?

Palmar fasciectomy (might need a skin graft)
34 y/o male presents to the clinic for hand pain. On physical exam his ring finger is held in flexion and there is decreased ROM at the MCP joint. You are able to palpate a nodular band along the palm of the hand that is tender. What is your op treatment plan?

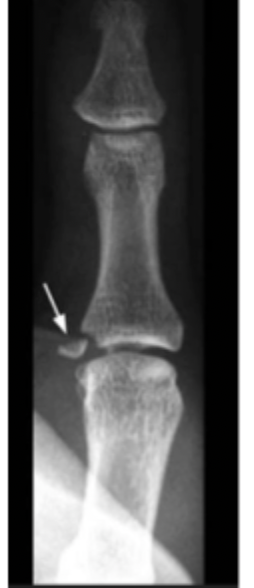
radially directed force causing hyper-adduction of the thumb MCP joint
MOI for a gamekeeper’s thumb (AKA thumb collateral ligament (UCL) injury, skiers thumb)
Thumb Xray with stress views (avulsion/condylar fracture), MRI (see the ligaments)
30 y/o male presents to the ED for a hand pain that is exacerbated by grasping things. He states that he caught himself with his hand after falling. On physical exam you not tenderness of the UCL and during a radial ulnar stress exam. What diagnostics do you want?
Thumb spica splint (4-6 weeks)
30 y/o male presents to the ED for a hand pain that is exacerbated by grasping things. He states that he caught himself with his hand after falling. On physical exam you not tenderness of the UCL and during a radial ulnar stress exam. X-rays reveal an avulsion fracture. What is your non-op treatment (for grade 1-2 partial UCL tears)?
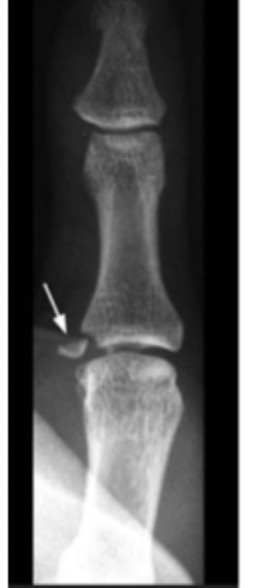
UCL repair
30 y/o male presents to the ED for a hand pain that is exacerbated by grasping things. He states that he caught himself with his hand after falling. On physical exam you not tenderness of the UCL and during a radial ulnar stress exam. X-rays reveal an avulsion fracture. What is your op treatment for grade 3 partial injuries?
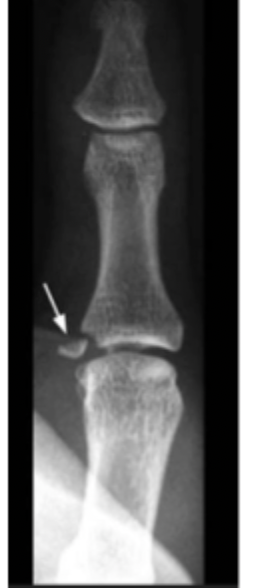
UCL reconstruction with tendon graft
30 y/o male presents to the ED for a hand pain that is exacerbated by grasping things. He states that he caught himself with his hand after falling. On physical exam you not tenderness of the UCL and during a radial ulnar stress exam. X-rays reveal an avulsion fracture. What is your op treatment for a chronic injury?
De Quervain’s tenosynovitis
Inflammation of the 1st dorsal compartment (extensor pollicis brevis and abductor pollicis longus at the base of the thumb) due to overuse of the wrist
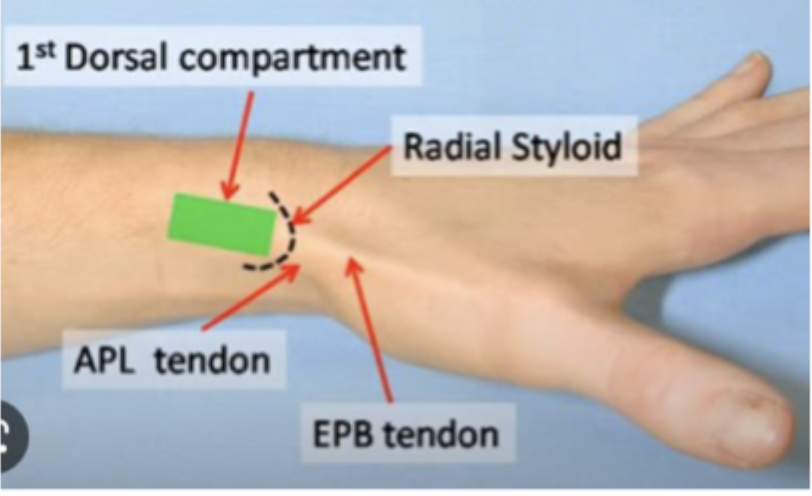
thumb spica splint for bracing, rest, activity modification, NSAIDs, corticosteroid injection
45 male presents to the clinic for wrist pain that worsens when grabbing objects. On physical exam you note tenderness at the level of the radial styloid, pain with resisted deviation, and a positive finkelstein test. X-rays are negative. What is your non-op treatment?

Surgical release of the 1st compartment
45 male presents to the clinic for wrist pain that worsens when grabbing objects. On physical exam you note tenderness at the level of the radial styloid, pain with resisted deviation, and a positive finkelstein test. X-rays are negative. What is your op treatment?

Trochanteric hip bursitis
A common cause of hip pain that is due to a sac between the muscle/bone or muscle/muscle (deep to the IT band) that can be inflamed or irritated by friction or impingment
females, side sleepers
Risk factors for Trochanteric hip bursitis
Ice/heat, anti-inflammatories, activity modifications, PT, steroid injections
45 y/o female presents to the clinic for lateral hip pain that is exacerbated by sleeping and walking. On physical exam you note point tenderness over the greater trochanter. Xrays are normal. What is your treatment plan?
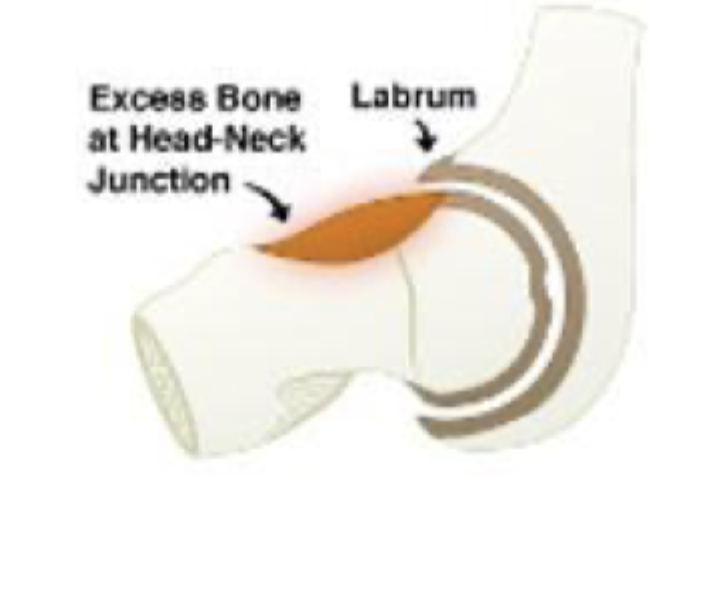
Femoroacetabular impingement syndrome (FAI)
A condition where there is abnormal bony contact between the femoral head and the acetabulum leading to hip pain and dysfunction - STRUCTURAL ABNORMALITY
vigorous hip motion (repetitive abnormal contact leading to intra-articular hip chondral damage and the labrum)
MOI for Femoroacetabular impingement syndrome - common in young active adult hips
Cam impingement, Pincer impingement, mixed
Types of FAI
Cam impingement
What type of FAI is characterized by extra bone growth of femoral head/neck that results in non-rounded shape (too broad) causing shearing at the chrondro-labral junction - young athletic males
Pincer impingement
What type of FAI is characterized by excess bone growth on the acetabulum that leads causing “over coverage” of the acetabulum - active middle aged women

activity related groin pain, reduced hip motion, stiffness, clicking or popping
FAI is often asymptomatic until there is increased hip motion (especially flexion) → what are the symptoms?
congenital hip issues, repetitive hip flexion (athletes)
Risk factors for RAI
pain in groin with 90 degree flexion, ADDuction, and IR
Describe the FADIR sign
pain in groin with 90 degree flexion, ABDuction, and ER
Describe the FABER sign
Xray (look for lesions, arthritis), MRI (cartilage, labrum damage), CT (look at bones further)
18 y/o male football player presents to the clinic for groin pain that worsens during practice. He notes that his hip becomes stiff and often POPs. On physical exam you not decrease hip ROM (limited flexion and internal rotation), as well as positive FADIR and FABER. What diagnostics you want?
Activity modification, NSAIDs, PT
18 y/o male football player presents to the clinic for groin pain that worsens during practice. He notes that his hip becomes stiff and often POPs. On physical exam you not decrease hip ROM (limited flexion and internal rotation), as well as positive FADIR and FABER. What is your conservative management
steroid injections
18 y/o male football player presents to the clinic for groin pain that worsens during practice. He notes that his hip becomes stiff and often POPs. On physical exam you not decrease hip ROM (limited flexion and internal rotation), as well as positive FADIR and FABER. What is your intervention management?
hip arthroscopy or arthroplasty
18 y/o male football player presents to the clinic for groin pain that worsens during practice. He notes that his hip becomes stiff and often POPs. On physical exam you not decrease hip ROM (limited flexion and internal rotation), as well as positive FADIR and FABER. What is your surgical management
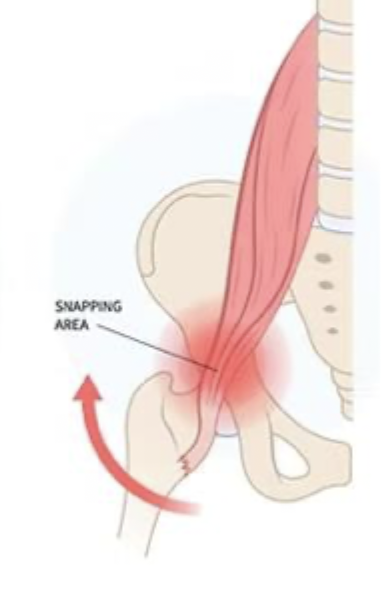
Coxa Saltans (Snapping Hip Syndrome)
An overuse phenomenon that produces a snapping sensation or audible sound in the hip during movement - common in athletes
Exernal (most common), Internal, Intra-articular (most severe)
Types of Coxa Saltans
External
What type of Coxa Saltans is caused by IT band or gluteus maximus tendon snapping over the greater trochanter (runners, dancers)

Internal
What type of Coxa Saltans is caused by iliopsoas tendon snapping over the iliopectineal eminence, femoral head or anterior hip structures (repetitive hip flexion peeps)
intra-articular
What type of Coxa Saltans is caused by labral tears, loose bodies, cartilage damage, or hip impingement and is characterized by pain, clicking, and mechanical symptoms
with the hip in flexion, palpate the greater trochanter and apply pressure → snapping stops
For an external Coxa Saltans what are you going to see on physical exam?
Not visible BUT audible when hip is moved from flexed and ER to a extended and IR position
For an internal Coxa Saltans what are you going to see on physical exam?
Ober’s test, iliopsoas snapping, thomas test, FABER, FABIR
Special tests for Coxa Saltans
no treatment
What is your non-op treatment for NON-PAINFUL Coxa Saltans
PT, maybe steroid injection with U/s guidance
What is your non-op treatment for PAINFUL Coxa Saltans
Prepatellar bursitis
Swelling and inflammation of the anterior knee bursa associated with kneeling (common in nuns and tile layers)
Xrays (r/o foreign body), Aspiration with gram stain and culture (staph a most common)
65 y/o male presents to the clinic for knee pain. He states that he worked as a tile layer for 40 years. On physical exam you note the anterior knee is warm and tender to the touch as well as decreased ROM. What diagnostics do you want?
RICE, NSAIDs, aspiration, activity modification (get some knee pads girlie), bursal resection (RARE)
65 y/o male presents to the clinic for knee pain. He states that he worked as a tile layer for 40 years. On physical exam you note the anterior knee is warm and tender to the touch as well as decreased ROM. What is your treatment plan?
Popliteal Cyst (Baker’s)
Extruded fluid outside the meniscus typically located between the semimembranosus and medial head of gastrocnemius associated with osteoarthritis, inflammatory joint disease, or joint injury.
X-ray, U/S MRI
45 y/o female presents to the clinic for pain and stiffness behind the knee. On physical exam you note a decreased ROM with flexion. What diagnostics do you want?
Activity modification, RICE, NSAIDs, Steroid injections, Aspiration, Surgery with arthroscopy to treat the underlying
45 y/o female presents to the clinic for a pain and stiffness behind the knee. On physical exam you note a decreased ROM with flexion. What treatments do you want to order?
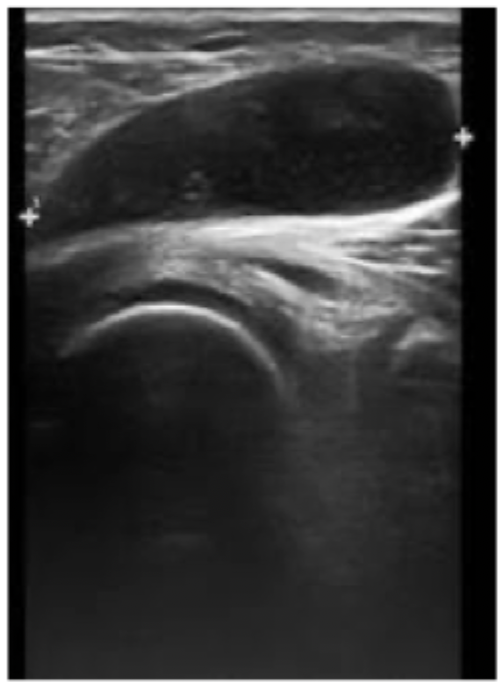
R/o DVT, let it resolve (monitor for compartment syndrome - hella rare)
Our baker cyst lady comes back with SHARP pain and redness in the leg and bruising along the ankle. What do you want to do?
Ankle sprain
One of the most common sports related injuries (usually inversion) that involves the lateral ligaments especially the anterior talofibular ligament - swelling, ecchymosis, TTP
High ankle sprain
A tear of the Anterior tibiofibular ligament (do a squeeze test and external rotation stress test)
3 view ankle (maybe add foot)
Imaging for ankle sprains
RICE, NSAIDs, lace-up brace or walking boot, PT, gradual return
Treatment for ankle sprains
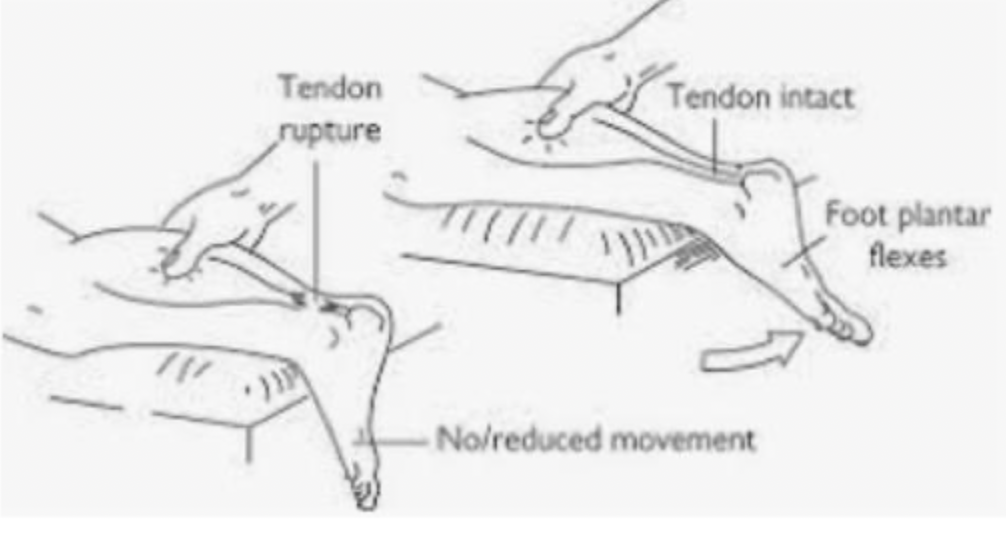
Achilles tendon rupture
An injury common in “weekend warriors” that is the result of sudden forced plantar flexion - commonly misdiagnosed as an ankle sprain
Refer to ortho (operative - acute or chronic ruptures; non-op -sedentary patient, elderly, co-morbidities)
47 y/o male tennis player presents to the ER with ankle pain. He states that he was playing in an ametuer tennis tournament when he felt a pop in his ankle. On physical exam you note a palpable gap over the achilles tendon, a loss of resting foot tone, weakness to plantarflexion, and a positive thompson test. What is your game plan?
Interdigital neuroma (Morton’s)
A compressive neuropathy of the foot that occurs at the transverse intermetatarsal ligament (between 2 metatarsal heads) of the forefoot - usually 3rd or 4th web space
3 view foot x rays, U/S (most helpful), digital nerve block with lidocaine
48 y/o female presents to the clinic for foot pain. She states that it feels like lightning in her feet when she wears high heels to work. On physical exam the space between the metatarsal heads is tender to palpation and when compression is applied their is an audible click (Mulder’s). What diagnostics you want?
Change to a wider shoe box, steroid injection with U/S guidance, Neurectomy (op)
48 y/o female presents to the clinic for foot pain. She states that it feels like lightning in her feet when she wears high heels to work. On physical exam the space between the metatarsal heads is tender to palpation and when compression is applied their is an audible click (Mulder’s). What is your treatment plan?
Plantar fasciitis
Inflammation of the aponeurosis at the calcaneus origin (usually painful at the plantar medial heel that worsens with weight-bearing activities)
Stretching is key, heel cushion cup inserts, supportive shoe wear, night splints, walking boot, steroid injections (last line)
65 y/o male presents to the clinic for foot pain that he states is worse 1st thing in the morning and towards the end of the day. He describes the pain as if he was standing on a sharp rock all day. On physical exam you note tenderness over the medial side of the plantar heel, increased pain with dorsiflexion of the GT, and a tight achilles with dorsiflexion. What is your treatment plan?
heel spur
What is absolutely NOT the source of pain in plantar fasciitis?
Pectus excavatum (cobbler’s chest, sunken chest, funnel chest)
A congenital chest wall deformity where the sternum and anterior ribs grow INWARD - most common chest wall deformity and 3X more common in males
Marfan’s, Rickets, scoliosis
Pectus excavatum is associated with

fatigue, decreased exercise tolerance, recurrent respiratory infections, SOB, chest pain, tachycardia
Pectus excavatum is usually asymptomatic unless it is severe - what are the symptoms
CXR is need (everything else is eh)
What diagnostics do you want for pectus excavatum?
orthotic bracing, PT for posture and chest expansion, Vacuum bell (takes 2-4 years)
Non-op Treatment for pectus excavatum
Nuss (bar pulls out sternum), Ravitch (correction of deformed cartilage)
Op Treatment for pectus excavatum - severe
Pectus carinatum
A congenital disorder in which in chest that flares outward with no known cause
Marfans, Down syndrome, osteogenesis imperfecta, dwarfism, chromosomal disorders
Pectus Carinatum is associated with

Non-op (6 months of bracing)
Treatment of Pectus Carinatum
Rib fractures (usually ribs 4-10)
Most common blunt thoracic injury that occurs due to trauma, rotation, and coughing (rare)
Usually Non-op with incentive spirometry
My 78 y/o great aunt Ann presents to the ED for chest pain after falling at the opera. She states that she smacked her chest on the stairs walking in, but she bought the tickets so she waited until the end of the opera. She reports pain with inspiration and slight SOB. On physical exam you note crepitus over the ribs and tenderness. What is your treatment plan?
pneumo, flail chest (usually 3 consecutive ribs)
Complication of rib fracture
produces a free-floating, unstable segment of a chest wall that paradoxical movement (might require plating)
describe a flail chest