Lecture 2: Control of Breathing, Ventilation, Breathing Pattern, and Acid Base
1/70
Earn XP
Description and Tags
Dolinay
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
What is ventilation?
movement of air into and out of the lungs for the purpose of gas exchange
What do inhalation and exhalation depend on?
cyclical ventilatory muscle excitation by motor nerves to diaphragm, intercostal abdominal, and upper airway muscles (ventilation largely driven by muscles)
Hypoxia is a system-wide deficiency in the __ that reach the __.
levels of oxygen; tissues
low O2 sat (lower than 94%)
Hypoxemia is low __.
blood oxygen level
measured invasively in an artery
Where are central chemoreceptors located? What are they sensitive to?
located within medulla
sensitive to pH of environment
Where are peripheral chemoreceptors located? What do they detect and monitor?
located in aortic and carotid bodies
act principally to detect variation of oxygen concentration in arterial blood
monitor arterial carbon dioxide and pH
Central controller (pons, medulla, other parts of brain) → __ → __ → central controller
central controller → effectors (respiratory muscles) → sensors (chemoreceptors, lung, other receptors) → central controller
What are 2 types of ventilatory control? Which ones are under voluntary control?
metabolic: not under voluntary control
behavioral: under voluntary control
The metabolic portion of ventilatory control is geared to the __ requirements of the body in terms of __ consumption and __ production.
metabolic; oxygen; carbon dioxide
The behavioral part of ventilatory control is modulated to facilitate: (3)
phonation, breath holding, express emotion
What contains the inspiratory (drive external intercostals) and expiratory (drive the internal intercostals and abdominal muscles) neurons?
ventral respiratory group
Clusters of specific neurons called __ control breathing.
respiratory centers
The respiratory centers located in the medulla oblongata set the __ and __ of normal breathing.
rate; rhythm
The respiratory centers in the pons regulate the __ and __ of breathing.
rate; depth
The __ is the inspiratory center, and the __ is the expiratory center.
dorsal respiratory group (DRG); ventral respiratory group (VRG)
What are the 5 functions of the dorsal respiratory group?
stimulates inhalations
inspiratory neurons
set by basic rhythm pacemaking
excites inspiratory muscles and sets eupnea (12-15 breaths/min)
cease firing during expiration
What are the 4 functions of the ventral respiratory group?
inspiratory and expiratory neurons
remains inactive during quiet breathing
activity when demand is high
involved in forced inspiration and expiration
How are the DRG and VRG controlled?
via phrenic and intercostal nerves (to diaphragm and external intercostal muscles)
if phrenic nerve is severed, diaphragm goes up and decreases inspiratory capacity
DRG and VRG are both responsible for __ but only __ controls expiration.
inspiration; VRG
In cortical control, there is __ ventilation to a considerable degree.
voluntary
In cortical control, __ is easier than hypoventilation.
hyperventilation
In cortical control, breath holding is limited by both __ and __.
PCO2 and PO2
What can help breath holding? (2)
preliminary hyperventilation: drives PCO2 down
pre-oxygenation: supplemental O2
The __ and __ are involved in fear and rage responses.
limbic system; hypothalamus
The __ is involved in involuntary control of breathing.
medulla
Chemoreceptors in the __ monitor blood O2, CO2, and pH
carotid and aortic bodies
Chemoreceptors in the __ monitor blood CO2 and pH
medulla oblongata
Decreased blood O2, increased CO2, and decreased pH decrease __ stimulation of the heart, which __ the heart rate.
parasympathetic; increases
Decreased blood O2, increased CO2, and decreased pH increase __ stimulation of the heart, which __ heart rate and stroke volume.
sympathetic; increases
Decreased blood O2, increased CO2, and decreased pH increase __ stimulation of blood vessels, which increase __.
sympathetic; vasoconstriction
In the central nervous system, PCO2 in blood → __ in the CSF due to __.
H+; dissociation (which accounts for 70-80% of total drive)
In the peripheral nervous system, __ is 20-30% of the total drive, __ is triggered only when PaO2 <60 (hypoxemia), and __ is from metabolic processes.
PCO2; PO2, H+
Central chemoreceptors are triggered the most in response to what process?
changes in pH
What is the mechanism to activate central chemoreceptors?
CO2 passes to medulla and then to CSF → in CSF, it combines with water to form H2CO3, which dissociates into HCO3- + H+ → inc in H+ will activate/trigger central chemoreceptors → sends signal to inspiratory center
blood brain barrier doesn’t let H+ pass through, only CO2
Small changes in the carbon dioxide content of the blood (PaCO2) quickly trigger changes in __.
ventilation rate
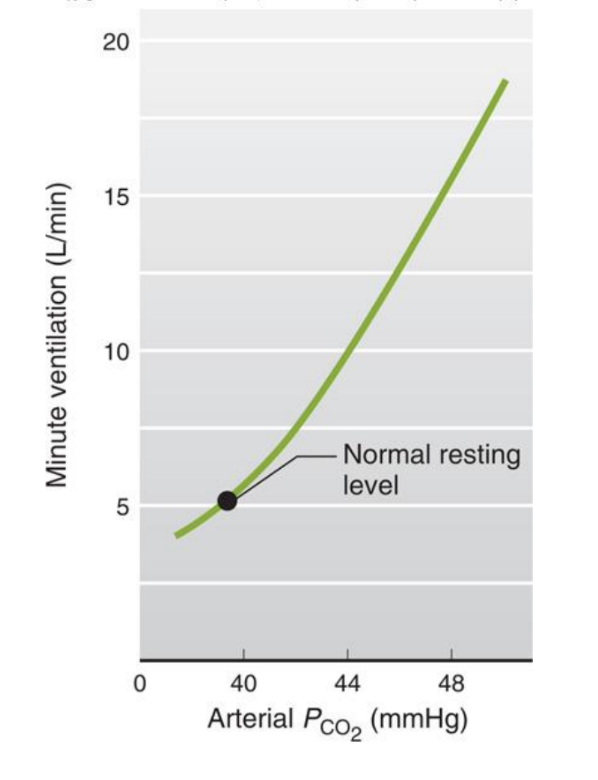
The ventilatory response to CO2 tends to be linear with an increase in ventilation of 1-2 L/min for every __ mm Hg rise in PaCO2.
1 mmHg
When PO2 is <60, __ increases.
respiration rate
The levels of __ (3) in blood and CSF provide information that alters the rate of ventilation.
oxygen, CO2, hydrogen
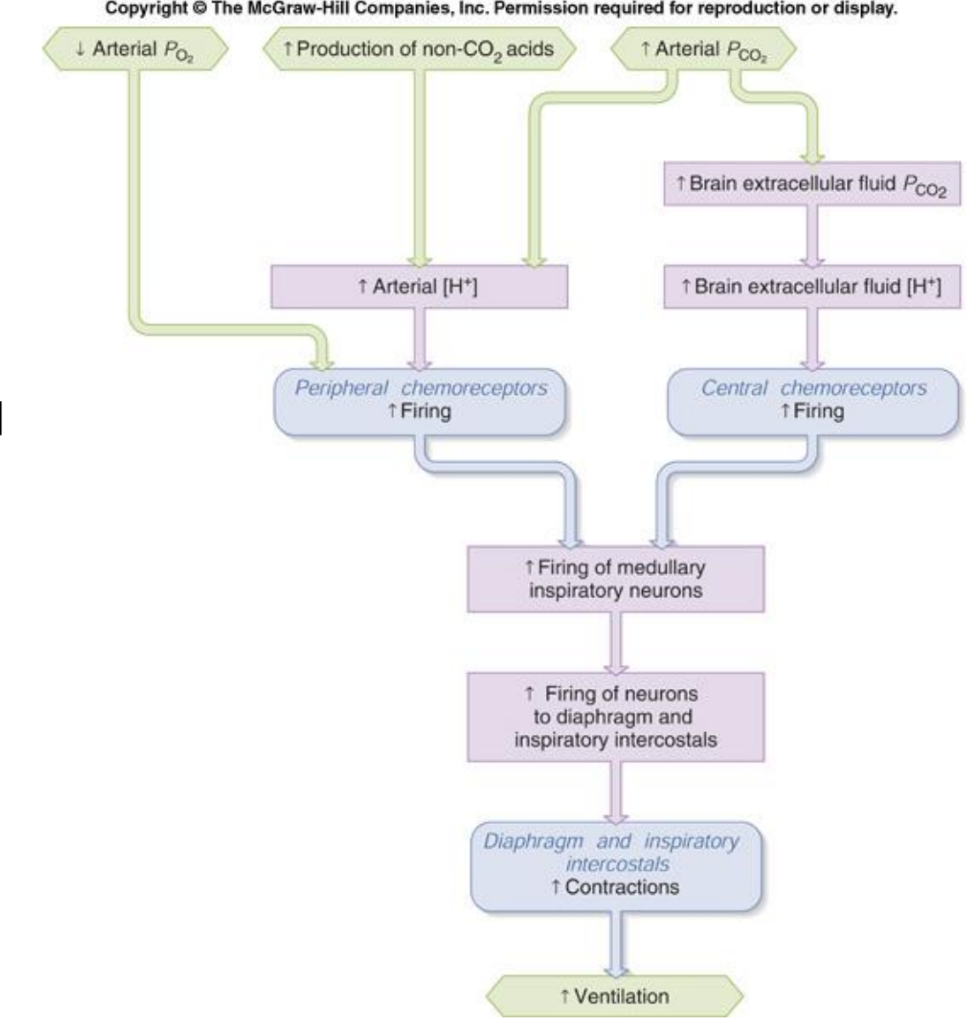
Describe the mechanism that occurs when there is a decrease in arterial PO2.
dec arterial PO2 → inc firing of peripheral chemoreceptors → inc firing of medullary inspiratory neurons → inc firing of neurons to diaphragm and inspiratory intercostals → inc contractions in diaphragm and inspiratory intercostals → inc ventilation
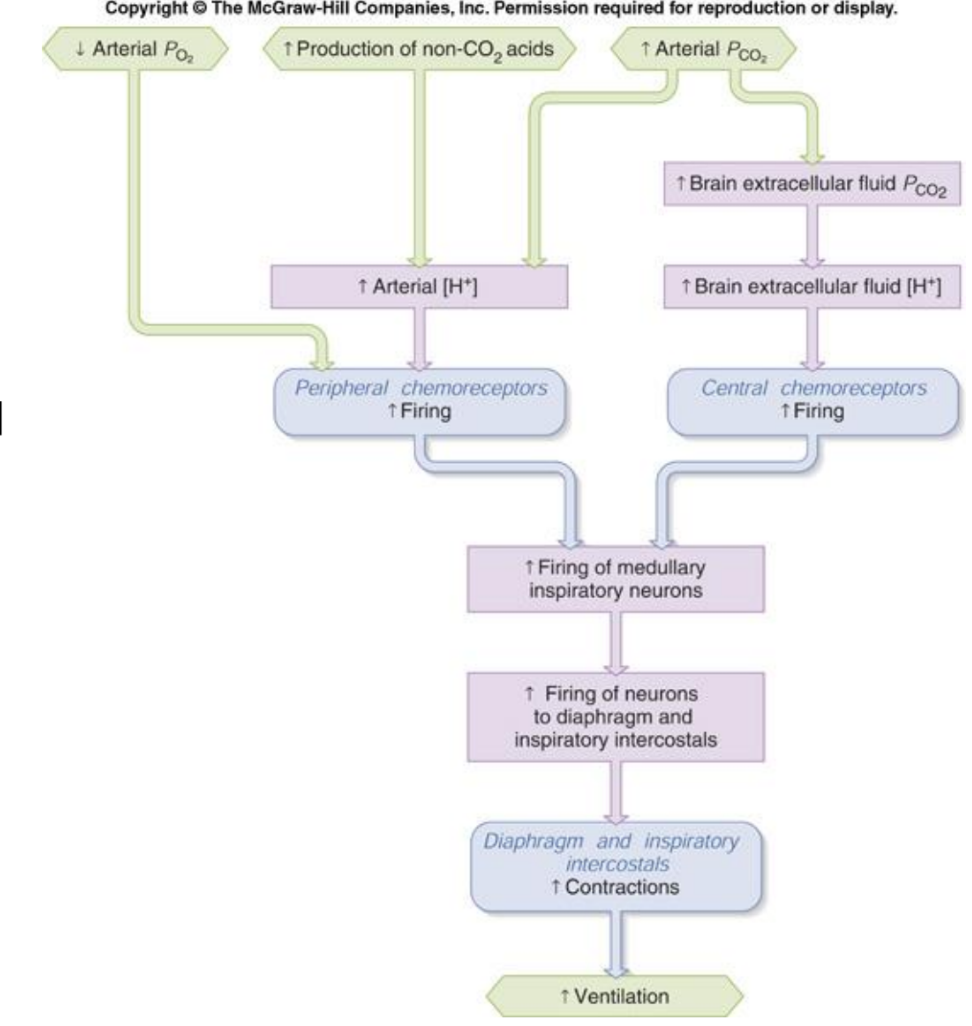
Describe the mechanism that occurs when there is an inc production of non-CO2 acids.
inc production of non-CO2 acids → inc arterial H+ conc → inc firing of peripheral chemoreceptors → inc firing of medullary inspiratory neurons → inc firing of neurons to diaphragm and inspiratory intercostals → inc contractions in diaphragm and inspiratory intercostals → inc ventilation
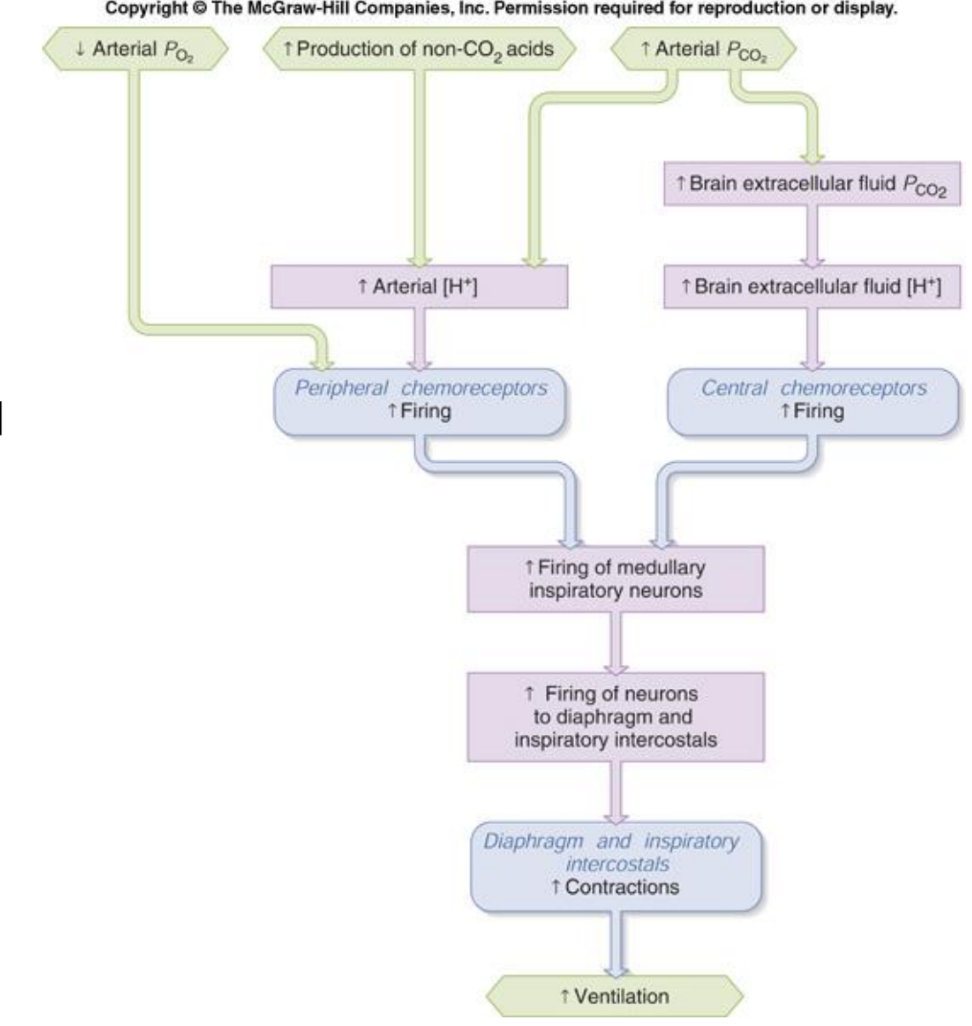
Describe the mechanism that occurs when there is an inc of arterial PCO2.
inc arterial PCO2 →
inc arterial H+ conc → inc firing of peripheral chemoreceptors
inc brain extracellular fluid PCO2 → inc brain extracellular fluid H+ conc → inc firing of central chemoreceptors
→ inc firing of medullary inspiratory neurons → inc firing of neurons to diaphragm and inspiratory intercostals → inc contractions in diaphragm and inspiratory intercostals → inc ventilation
The ventilatory response to CO2 tends to be __ with an increase in ventilation of __ L/min for every 1 mmHg rise in PCO2. This response tends to be characterized by noticeable increases in __.
linear; 1-2; tidal volume
The ventilatory response to low PO2 is __ with minimal increase in ventilation until PO2 falls below __. This response tends to be characterized by noticeable __ in breathing frequency and a sense of __.
non-linear; 60 mmHg; increases; dyspnea
The __ chemoreceptors mechanism is responsible for 70-80% of ventilatory responsiveness to CO2.
central
The fastest way to alter pH is to __
change respiratory rate
How does the body respond to acid load?
buffering (after minutes) → respiratory compensation (after minutes) → renal excretion (after days)
What is the acid-base equilibrium equation?
CO2 + H2O ←→ H2CO3 ←→ H+ + HCO3-
What is the importance of arterial blood gas sampling? (3)
determines pH and partial pressures of respiratory gases
determines other serum blood levels
assesses response to therapeutic interventions (left atrium has most oxygenated blood and should have 100% O2 Sat)
What is the normal range for arterial blood CO2 tension (PaCO2) when doing an arterial blood gas?
35-45 mmHg (higher or lower = not good)
What is the normal range for arterial bicarbonate (HCO3-) when doing an arterial blood gas?
22-26 mmol/L
The pH of arterial blood gas should be between:
7.35-7.45 (7.4 ideal)
The pCO2 of arterial blood gas should be between:
35-45 (40 ideal)
The bicarbonate of arterial blood gas should be between:
22-26 (24 ideal)
Acidosis occurs at a pH of __, and the danger zone is __.
<= 7.35; danger zone <7.1
Alkalosis occurs at a pH of __, and the danger zone is __.
>= 7.45; danger zone >7.5
What are the two types of acidosis and what compensation mechanisms occurs as a result?
[HCO3-] < 24 mEq/L → metabolic acidosis → PCO2 < 40 mmHg → respiratory compensation (breathing more: exhaling more CO2)
(low bicarbonate/ high H+, can’t buffer anymore)
PCO2 > 40mmHg → respiratory acidosis → [HCO3-] > 24 mEq/L → renal compensation
What are the two types of alkalosis and what occurs as a result to compensate?
[HCO3-] > 24 mEq/L → metabolic alkalosis → PCO2 > 40 mmHg → respiratory compensation (breathing less)
PCO2 < 40mmHg → respiratory alkalosis → [HCO3-] < 24 mEq/L → renal compensation
If compensation is not appropriate, suspect __.
mixed acid-base disorder
Hyperventilation → [inc/dec] CO2 → [inc/dec] pH
dec; inc
Hypoventilation → [inc/dec] CO2 → [inc/dec] pH
inc; dec
The __ is the measurement of the difference/gap bw negatively charged and positively charged electrolytes.
anion gap
If the anion gap is too high or too low, it may be a sign of: (3)
pulmonary, renal, or other organ dysfunction
What is the formula for anion gap, and what is the normal anion gap?
anion gap = Na+ - (Cl- + HCO3-) - 12 ± 2
normal = 12
The peripheral chemoreceptors are primarily responsive to __ and __ in systemic arterial blood.
hypoxia; unbuffered H+
__ chemoreceptors account for 20-30% of the ventilatory responsiveness to CO2.
peripheral
Metabolic __ augments the ventilatory response to __, whereas metabolic __ attenuates (reduces) it.
acidosis; CO2; alkalosis
The __ is the respiratory center that sets our basis pacemaking for breathing.
DRG
The __ is involved in forced inspiration and expiration.
VRG
__ are most sensitive to pH changes.
central chemoreceptors
The __ are most sensitive to hypoxemia with PaO2 < 60 mmHg.
peripheral chemoreceptors
When the body senses that the pH has strayed from pH 7.5, the immediate changes to normalize come from __, and the delayed changes come from __.
respiratory system; renal system