GI E1- Stomach & Duodenum
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
What are the 4 layers of the GI wall?
mucosa, submucosa, muscularis (outer longitudinal & inner circular, oblique in stomach), serosa
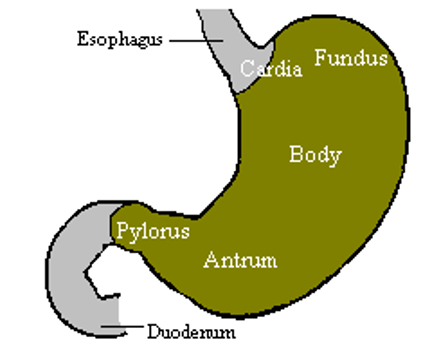
What are the 4 main zones of the stomach?
cardia, fundus (above GEJ), body (corpus), antrum
Combined secretions of mucous cells, parietal cells (HCl + intrinsic factor), and chief cells (pepsinogen I&II) are known as _______
gastric juices
_________ is secreted by G cells in response to food entry to increase stomach motility, mediate gastric acid secretion, and promote constriction of LES.
Gastrin
________ is secreted by I cells of the jejunum in response to fatty substances to increase gallbladder contractility for bile, stimulate pancreatic secretion, regulate gastric emptying & bowel motility, and induce satiety.
cholecystokinin
________ is produced by duodenal mucosa w/ entry of gastric juice from the stomach to stimulate pancreatic fluid/bicarb secretion & neutralize the acidity of stomach contents.
secretin
_____ is a peptide that increases appetite, stimulated GH secretion, and produces weight gain.
ghrelin
What is epithelial damage in the mucosa without accompanying inflammation?
gastropathy
What do hemorrhagic and erosive lesions develop from?
exposure of gastric mucosa to injurious substances OR lack of blood flow to mucosa (ischemic)
ex: meds, alc, medical/surgical stress, portal HTN
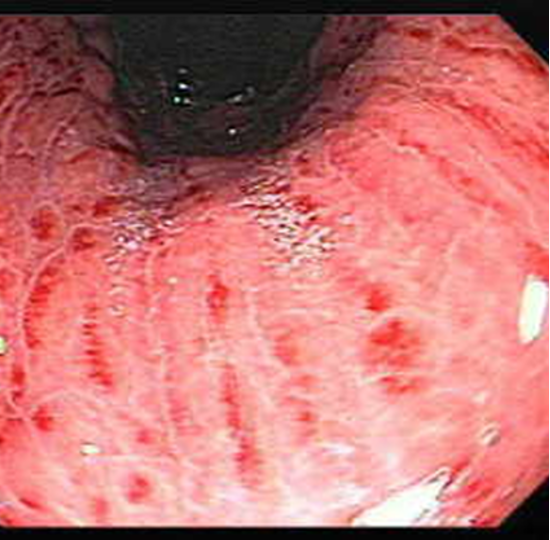
What condition?
upper endo findings: sub epithelial hemorrhages, petechiae, erosions
sx: anorexia, epigastric pain, N, V
UGI bleeding- hematemesis: “coffee ground” emesis, bloody aspirate w/ NG suction, usually insignificant amounts, possibly melena
erosive & hemorrhagic lesions
What condition?
mucosal erosions & subepithelial hemorrhages that develop w/in 72 hours in majority of critically ill pts
bleeding assoc w/ high mortality, but is rarely cause of death
begin prophylaxis upon admission to ICU
rx: IV H2RA, IV PPI, sucralfate susp, omeprazole + sodium bicarbonate (zegerid) rapid release susp
stress gastropathy
What factors significantly increase bleeding in stress gastropathy?
coagulopathy: plt < 50,000/MCL; INR > 1.5
mechanical vent > 48 hrs
other: sepsis, vasopressor, steroids, burns, TBI, PUD, GI bleed
NSAIDs selective for which enzyme are associated with a decrease in ulcers/injury, but a twofold increase in CV complications?
COX-2
All NSAIDS except which ones should be used with caution in those w/ CV risks factors?
ASA and naproxen
What is the pathogenesis of NSAID induced gastric injury and bleeding?
inhibition of prostaglandin synthesis, which is needed for mucosal protection and healing; 3 pathways
inhibit COX-1 activity
inhibit COX-2 activity
direct cytotoxic effects on epithelium
Dyspeptic symptoms from NSAID induced injury do not correlate w/ disease severity. When would a diagnostic upper endoscopy be indicated?
alarm sx
What is the treatment for NSAID related injury/dyspepsia?
PPIs > H2RAs; empiric 2-4 wk trial w/ PPIs
refer for EGD if sx persist
misoprostol (cytotec) for prevention of ulcers (avoid in women of childbearing years due to termination of pregnancy)
What is the treatment of alcohol induced gastropathy?
H2RAs, PPIs, or sucralfate initiated empirically for 2-4 wks
What condition?
portal HTN → gastric mucosal/submucosa capillary/venule congestion
often asx, possible chronic GI bleeding or hematemesis
rx: propranolol or naldolol to decrease portal HTN
portal hypertensive gastropathy
Inflammation of the gastric mucosa w/ histologic evidence of inflammation via endoscopic or radiologic evaluation +/- erosions / hemorrhages is known as _______
Gastritis
what bacteria?
spiral gram negative
secretes urease → converts urea to ammonia → neutralizes stomach acidity
spiral shape allows it to bury into mucous layer → CAGA toxin injected into stomach cells → bacteria attach easily → chronic inflammation
person-person transmission, mode unknown
h. pylori
What is h. pylori associated with?
chronic gastritis / inflammation, PUD, gastric cancer (group 1 carcinogen)
What population is h. pylori increased in?
> 60, non whites, immigrants from developing countries (inversely correlated w/ lower socioeconomic status)
What are the 3 gastritis phenotypes associated with h. pylori?
Mild diffuse w/o disruption of acid secretion & no clinical illness
Inflammation in gastric antrum only, inc risk of duodenal PUD
Inflammation mainly in gastric body, inc risk of gastric ulcers & cancer
When should H. pylori testing be conducted?
pts < 60 w/ uncomplicated dyspepsia,
functional dyspepsia
all immigrants from prevalent regions - Japan, Korea, China
What are noninvasive testing options for H. pylori?
urea breath test & fecal antigen immunoassay
(*** must d/c PPIs 7-14 days prior & abx 28 days prior)
What is the first line treatment for H. pylori?
triple therapy x 10-14 days
Prevpac BID: 1 tab lansoprazole, clarithro, 2 tabs amoxicillin
Helidac QID: 2 tab metro, tetra HCL, 2 tabs bismuth subsalicylate, plus ranitidine (H2RA)
What condition?
autoimmune; destruction of fundic glands
anti-intrinsic factor abs, intestinal metaplasia, severe gland atrophy
loss of acid inhibition of G cells → achlorhydria & hypergastrinemia (> 1000 PG/ml)
increase risk of gastric cancer (carcinoid tumors)
pernicious anemia gastritis
what is indicated with a new diagnosis of pernicious anemia?
EGD
What is the treatment for acute bacterial infection / phlegmonous / necrotizing gastritis?
broad spectrum abx & possible emergent gastric resection
What kind of patients is viral gastritis due to CMV seen in?
AIDs, bone marrow or solid organ transplant recipients
what kind of patients are fungal gastritis infections seen in?
immunocompromised & diabetics
what condition?
eosinophils infiltrate antrum and proximal intestine
+peripheral eosinophilia
rare
sx: anemia, abd pain, early satiety, postprandial vomiting
tx: corticosteroids
eosinophilic gastritis
What condition?
large thickened gastric folds in body of stomach → chronic protein loss
unknown eti
sx: N, epigastric pain, wt loss, diarrhea
tx: cetuximab, gastric resection
menetrier disease / hypertrophic gastropathy
what condition?
loss of gastric or SI epithelium that extends to penetrate muscularis mucosa
erosions- small & superficial; ulcers- 5mm - several cm
caused when normal mucosal defenses are impaired / overwhelmed by acid or pepsin
peptic ulcer disease (PUD)
What plays an important role in maintaining defenses against ulcers?
prostaglandins
what are the most common risk factors for PUD?
H. pylori infection, NSAID / ASA use
What condition?
classic sx: epigastric pain → dull, gnawing, aching, “empty, “hunger like” sensation
recurs over weeks-months
acute or worsening pain may indicate ulcer penetration/perforation
PUD
What is the workup for PUD?
study of choice: endoscopy (all gastric ulcers need to be bx)
alt: BA UGI
asses for H. pylori
what kind of ulcer?
antrum & lesser curvature
later in life - 55-70
normal or increased acid secretion
pain & N w/ eating, relieved w/ fasting (look for wt loss, anorexia)
gastric
What kind of ulcer?
duodenal bulb or pylorus
younger age - 30-55
inc acid secretion and dec HCO3 may create small area of gastric metaplasia which becomes colonized by h. pylori
pain relieved by foot intake, recurs 2-4 hrs later, may awaken pt at HS
duodenal
What is the treatment for H. pylori associated ulcers?
avoid smoking
antibacterial + antiulcer therapy
PPI + clarithro or metro + amoxi
PPI + clarithro + metro
bismuth salicylate + metro + tetra + PPI
How do PPIs treat ulcers?
covalently bind acid secreting enzyme H+/K+ATPase → proton pump must regenerate (18 hrs) → inhibit 90% of acid secretion
(action is > 24 hrs)
What is the treatment for NSAID associated ulcers?
d/c NSAID or use selective COX 2 inhibitors
PPIs, H2RAs,
high risk → test for h. pylori, PPI, misoprostol
What increases the risk of GI bleeding, especially in combo with ASA use?
chronic antiplatelet therapy
What is important to remember about post GI ulcer bleeds in patients on antiplatet therapy?
ASA should be restarted as soon as risk for CV events outweighs risk for recurrent ulcer complications
(PPIs may diminish effects of clopidogrel, but studies show you can use them together; least interactive w/ pantoprazole)
what is the most common complication of PUD?
GI hemorrhage
What condition?
infrequent complication of PUD → erodes into adjacent organ
severe abd pain, peritonitis (rigid abd w/ rebound tenderness), leukocytosis
peptic ulcer perforation
what should be avoided with peptic ulcer perforations?
endoscopy
How do you diagnose PUD?
xray → free air under diaphragm
if suspect & no free air → order UGI or CT w/ gastrografin (water soluble contrast)
What is the treatment for peptic ulcer perforation?
NG tube to suction, IV fluids & PPI, consult surgeon for laparotomy or laparoscopy
What condition?
comp of PUD, occurs in < 2% of ulcer patients
sx: early satiety, epigastric fullness, vomiting, wt loss, abd distension, vomit previously ingested material
2 types:
edema/inflammation around acute ulcer
chronic permanent scarring/fibrosis w/ outlet narrowing
gastric outlet obstruction
How is gastric outlet obstruction diagnosed?
succussion splash (PE) - audible splash of gastric contents produced by shaking patients torso
barium studies
endoscopy
What is the treatment or gastric outlet obstruction?
NGT aspiration 5-7 days→ large, foul smelling liquid
IV fluids & PPI
may require surgery/endoscopic dilation in 1 yr
What can cause gastric outflow obstruction at the pylorus, producing succussion splash?
antral cancer, bezoar, or PUD
What condition?
gastric acid hyper secretion, severe PUD, gastrin secreting tumors
caused by gastronomas
maldigestion & malabsorption due to low pH
sx: unresolved reflux sx, diarrhea, wt loss
zollinger-ellison (ZE) syndrome
Where do most gastronomas arise?
gastronoma triangle - junction of cystic duct & common bile duct, head & neck of pancreas, 2nd & 3rd parts of duodenum
90% of ZE patients will develop _____
PUD
What should be obtained with screening for all ZE patients to exclude men 1?
serum PTH, prolactin, LH-FSH, GH
How is ZE syndrome diagnosed?
fasting serum gastrin: > 1000 PG/ml + gastric pH < 4.0
gastric pH: exclude secondary hypergastrinemia due to achlorhydria
secretin stimulation test: differentiate gastrinomas from other causes of hypergastrinemia
What is the best predictor of survival of ZE syndrome?
presence of hepatic mets; tx w/ PPIs & surgical resection
what is the 2nd most common cancer worldwide?
gastric adenocarcinoma
What is a common cause of gastric adenocarcinoma?
chronic h. pylori infection
What are risk factors for gastric cancer?
older age & male, H. pylori, diets high in salt & preserved foods (nitrates), tobacco, pernicious anemia, hx stomach surgery, FHx
Which histologic variant of gastric cancer?
younger pts
worse prognosis
not related to H. pylori
acquired or inherited mutations
“diffuse” - poorly differentiated
Which histologic variant of gastric cancer?
forms glandular structures
more common
environmental factors
arises from multi step progression from inflammation (H. pylori) to metaplasia to dysplasia (cancer)
intestinal type
The following symptoms are signs of what?
virchow’s node (supraclavicular)
sister Mary Joseph nodule (umbilical)
blumer shelf (rigid rectal shelf)
krukenberg tumor (ovarian mets)
metastatic gastric cancer
Virchow’s node (left supraclavicular area) is indicative of _______
mets of gastric carcinoma
What are indications for an endoscopic evaluation for gastric cancer?
any pt > 60 w/ new onset dyspepsia
persistent dyspepsia or resistant to tx
screening in high areas of occurrence
what is the treatment for gastric cancer?
surgery & TNM staging, chemo & radiation
(< 15% long term survival; >45% survive 5 yrs after “curative” resection)
what is the second most common gastric tumor?
gastric lymphoma
What has the same clinical presentation as adenocarcinoma?
Gastric lymphoma
What type of gastric lymphoma?
most are B cell NHL
many arise from mucosa assoc lymphoid tissue (MALT)
infx w/ h. pylori is risk factor
similar presentation to adenocarcinoma
primary gastric
what type of gastric lymphoma?
usually present at advanced stage
seldom curable
nodal lymphoma
what is the treatment for gastric lymphoma?
surgical resection, chemo, +/- radiotherapy
what kind of tumor?
neuroendocrine
rare; <1% of gastric tumors
sporadic or secondary to chronic gastrinemia
tend to metastasize
carcinoid tumor
what kind of tumor?
arise from mesenchymal stem cells
occur throughout GI tract, but 2/3 are in stomach
types: stromal (MC; GIST); leiomyomas, schwannomas
GI mesenchymal tumor
A symptomatic delay in gastric emptying of solid or liquid meals w/o any obstructing lesion is known as _____
gastroparesis
What are the 3 most common causes of gastroparesis?
idiopathic, diabetic neuropathy, post surgical
What are the sx of gastroparesis?
N/V, early satiety, bloating, wt loss
what is the best test to diagnose gastroparesis?
gastric emptying scintigraphy (uses technetium 99 labeled food, performed 1-4 hrs after food ingestion)
what is the treatment for gastroparesis?
pro kinetics: erythromycin IV or PO, metoclopramide PO (both accelerate gastric emptying & antral contractions)
5HT serotonin agents: granisetron, ondansetron
What drug?
dopamine agonist w/ pro kinetic & antiemetic properties
administer w/ meals & at HS
SE: tremor, dystonic rxns, drowsiness, fatigue tardive dyskinesia (black box warning)
Metoclopramide (Reglan)