Lecture 8: Acid Base Balance
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
53 Terms
Kidneys are a __ response to acid base balance, whereas respiration is an __ response.
long-term; immediate
There is a gain of hydrogen ions when there is a loss of __ in the __.
bicarbonate; urine
There is a loss of hydrogen ions in the __
urine
Alkalosis occurs when loss of __ exceeds gains in the __ , and the pH is [greater/less than] 7.4
H+; ECF; greater
Acidosis occurs when __ of H+ exceeds __ in the ECF and the pH is [greater/less] than 7.4.
gain; loss; less
The kidneys are responsible for balancing H+ ion __ and __.
loss; gains
When HCO3- is lost from the body, it is the same as if the body has:
gained a H+ ion
When CO2 is lost from the body, it is the same as if the body has:
lost a H+ ion
H+ ion is lost in the formation of carbonic acid
Alkalosis occurs when there is __ of HCO3- to __.
addition; ECF
Acidosis occurs when there is __ of HCO3- in __.
excretion; urine
What is the respiratory response to decreased ECF pH?
inc respiration
(there’s inc arterial [H+] which stimulates chemoreceptor firing → contractions → inc ventilation → dec CO2)
How do kidneys balance pH?
alter plasma HCO3-
When H+ ion decreases in the ECF, the kidney __ HCO3-
expels
alkalosis
Excretion of HCO3- in urine = __ H+ to __
adding H+ to plasma
When H+ ion increases in ECF, the kidney __ HCO3-
retains
acidosis
Addition of HCO3- to plasma = __ H+ from __
removing; plasma
Most of bicarbonate handling occurs in the __
proximal tubule
some in thick ascending limb
What transporters aid in the reabsorption of HCO3-?
AE2: HCO3- in, Cl out
NBCe1: 3HCO3- out with 1 Na+ out
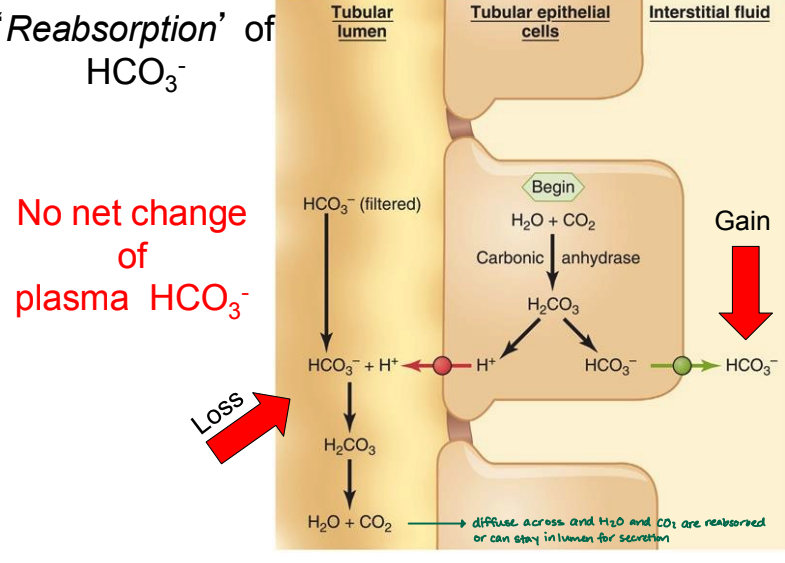
In the tubular lumen, there is a __ of bicarbonate.
loss
(HCO3- that is filtered interacts with H+ → H2CO3 → H2O + CO2)
Why does reabsorption of HCO3- result in no change in plasma HCO3-?
H2O + CO2 in tubular epithelial cells → H2CO3 → H+ & HCO3-
H+ diffuses to tubular lumen and interacts with a filtered HCO3- → H2CO3 = LOSS of HCO3-
HCO3- diffuses into interstitial fluid = GAIN / reabsorbed
the loss and gain cancel each other out
How does a gain in plasma HCO3- affect plasma pH?
increases pH (loses H+)
When does a gain in plasma HCO3- occur?
when H+ from tubular epithelial cells interacts with (HPO4)2- rather than HCO3-
can occur if not enough HCO3- in filtrate
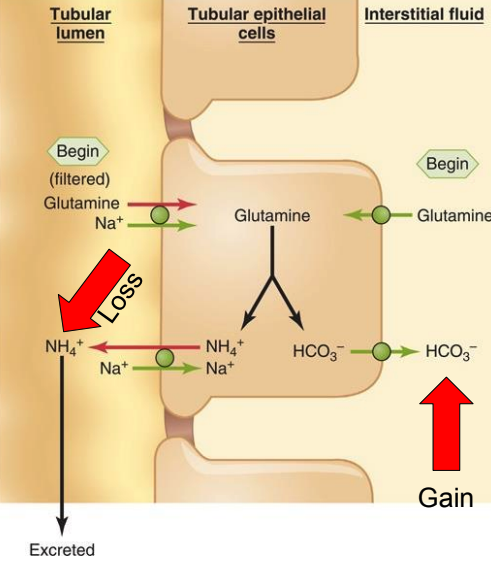
How does glutamine contribute to an increase in HCO3- in the plasma?
filtered glutamine transported into tubular epithelial cell or glutamine from interstitial fluid diffuses into tubular epithelial cell
glutamine → NH4+ + HCO3-
NH4+ transported into tubular lumen → excreted
HCO3- diffuses into interstitial fluid = gain
a-intercalated cells require:
ATP
How do a-intercalated cells contribute to acid balance?
H+ + HCO3-
H+ transported to lumen with ATP
HCO3- out to plasma, Cl- in
What 3 organs does calcium homeostasis occur?
intestinal absorption of Ca2+
kidney: increase Ca2+ reabsorption
bone: increase plasma Ca2+ (via osteoclast stimulation)
Most Ca2+ handling occurs in the __. However, Ca here is __.
bone matrix; unavailable
The Ca in the ICF is mostly __
bound
only 1% here
60% of Ca is __
free
40% of Calcium in the ECF is __
protein bound
Furosemide affects the [region of nephron] by __ Na-2Cl-K channels. This therefore [inc/dec] Ca2+ diffusion through tight junctions.
thick ascending limb; blocking; inc
Thiazide affects the [region of nephron] by __ Na/Cl channels. This therefore [inhibits/enhances] Ca binding protein.
distal tubule; blocking; enhances
__ also increases Ca reabsorption in the distal tubule.
PTH
Vitamin D is processed in the __ and activated in the __ by __.
liver; kidney; PTH
then goes to plasma → GI tract for absorption of Ca
How does PTH affect the bone?
bone resorption → inc release of calcium into plasma
How does PTH affect the kidney?
inc Ca reabsorption → dec urinary excretion of Ca → inc plasma Ca
How does PTH affect vitamin D?
after vitamin D is processed in liver, PTH activates it in the kidney → intestinal epithelium for absorption of calcium → inc plasma Ca
A sufficient plasma Ca concentration will __ PTH
inhibit
20% of blood plasma Mg2+ is __
protein bound
Where is the majority of Mg2+ reabsorbed in the nephron?
thick ascending limb (60%)
30% in proximal tubule
5% in distal tubule
__ is the most abundant intracellular ion and maintains intracellular __.
potassium; osmolarity
Potassium is tightly regulated to excrete the __ amount that is ingested.
same
The control of __ is the major mechanism for regulating body K+
urinary K+ excretion
The majority of K+ is reabsorbed in the __
proximal tubule (67%)
20% in TAL
How do a-intercalated cells regulate K+?
ATP channel that takes K+ in, H+ out → K+ is diffused to plasma

When is K+ reabsorbed in the distal tubule?
in low K+ diet, H+/K+ ATPase channel is activated to help compensate
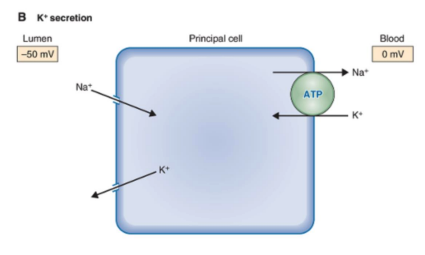
Principal cells cause K+ __
secretion
K+ into lumen, Na/K ATPase filters K+ from blood
Phosphate is mostly found in the __ and is __ there.
bone matrix; unavailable
Phosphate can also be found in the __ (15%) and __ (<0.5%)
ICF; ECF
Phosphate in the ECF is important for __
ICF buffering
Phosphate is inhibited by:
PTH
Most of phosphate is reabsorbed in the __, but this can be __ by PTH.
proximal tubule (70%, 15% in thin descending limb); inhibited
15% of __ is excreted.
1-110% of __ is excreted.
5% of __ is excreted.
phosphate
potassium
magnesium