L20- Adaptive Immunity Pt 2
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
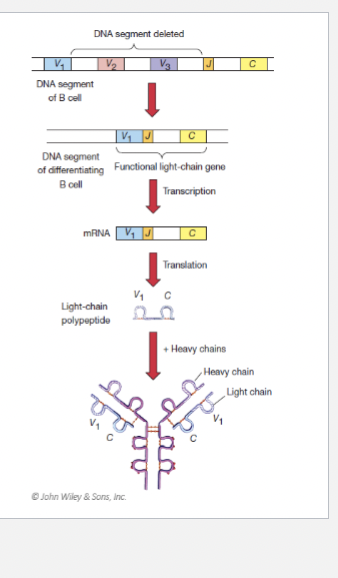
B cell overview
B cell are produced from stem cells in the bone marrow.
B cell maturation also occurs in the bone marrow.
A selection process removes all B cells that recognize self antigens.
Once out of the bone marrow, B cells make their way to the secondary lymphatic tissue until they encounter an antigen presenting cell.
Activated B cells cells result in antibody production.
Antibody producing B cells are known as plasma cells.
Once out of the bone marrow…
B cells make their way to the secondary lymphatic tissue until they encounter an antigen presenting cell.
Activated B cells cells result in antibody production.
Antibody producing B cells are known as plasma cells.

Antibody variability
Humans can make antibodies to as many as 10^13 different antigens.
This allows the host to respond to as many antigens as needed throughout their life.
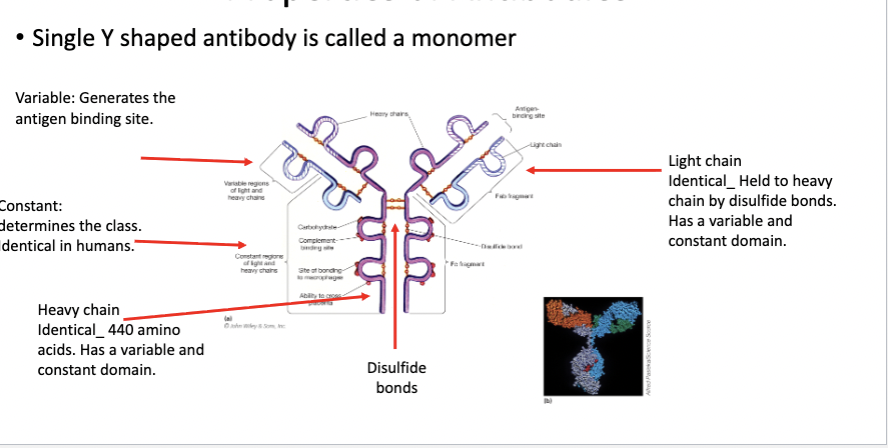
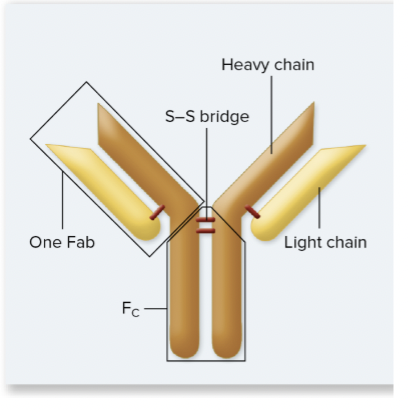
Properties of Antibodies
Single Y shaped antibody is called a monomer
Variable
Constant
Heavy Chain
Light Chain
Disulfide bridge
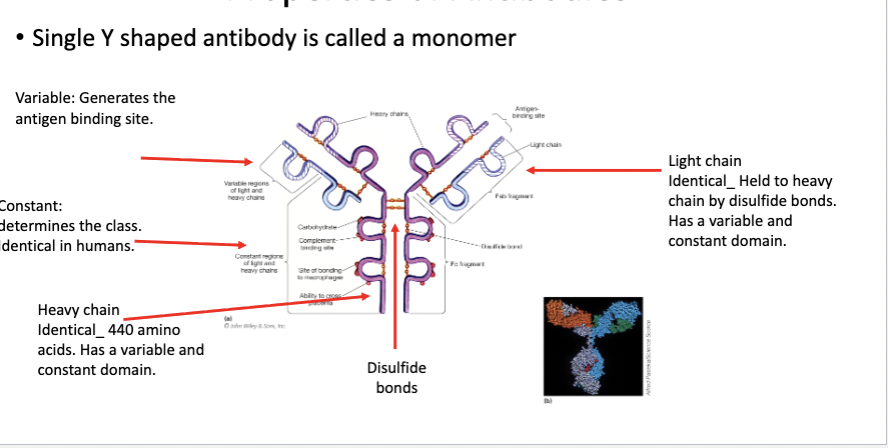
Variable:
Generates the antigen binding site.
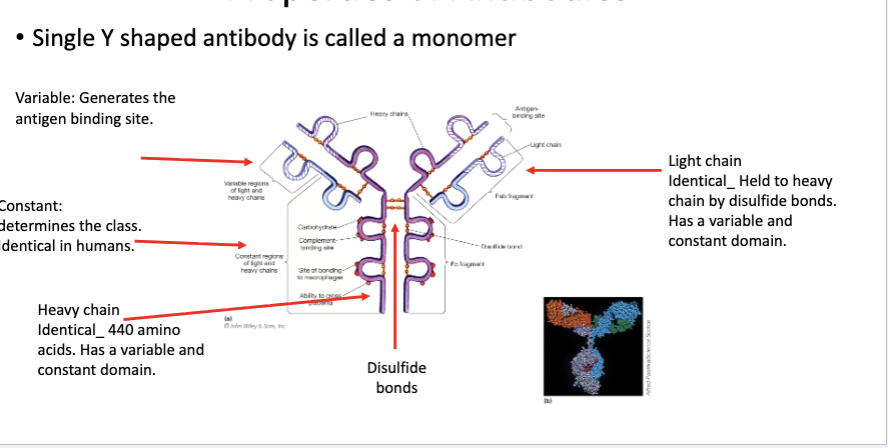
Constant:
determines the class.
Identical in humans.
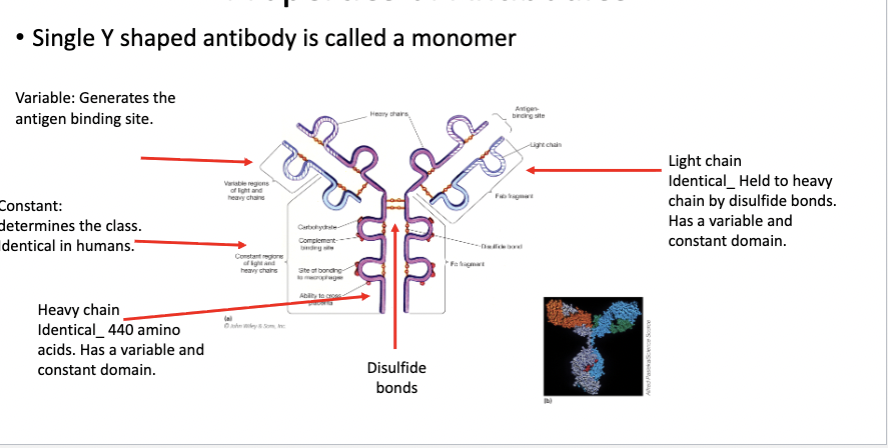
Heavy chain
Identical 440 amino acids.
Has a variable and constant domain
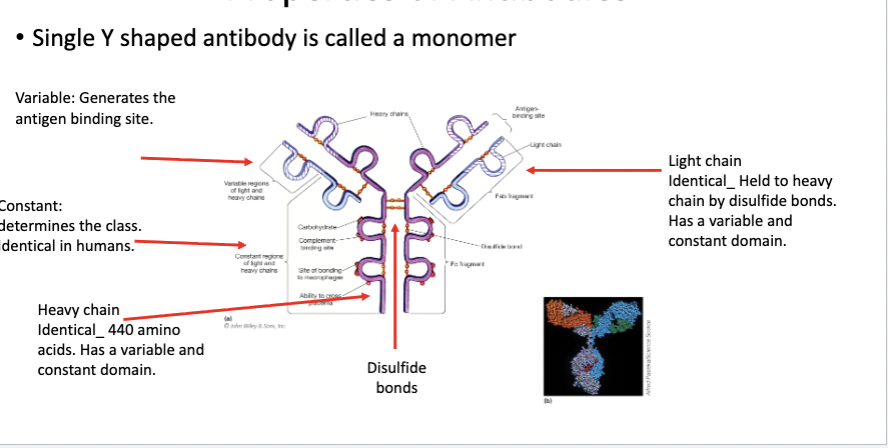
Light Chain
Identical
Held to heavy chain by disulfide bonds.
Has a variable and constant domain.
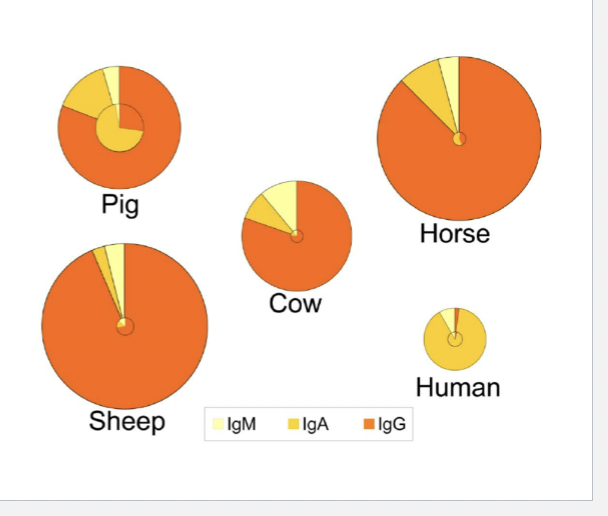
5 classes of heavy chain
There are 5 classes of heavy chain antibodies
IgG
IgA
IgM
IgD
IgE
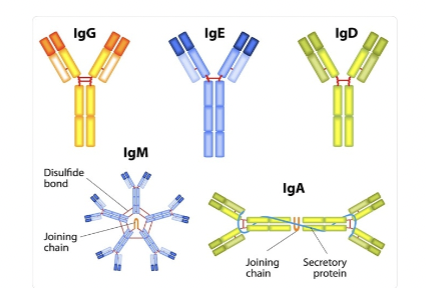
What regions do antibody shape depend?
Depends on the kind of constant region.
IgG components
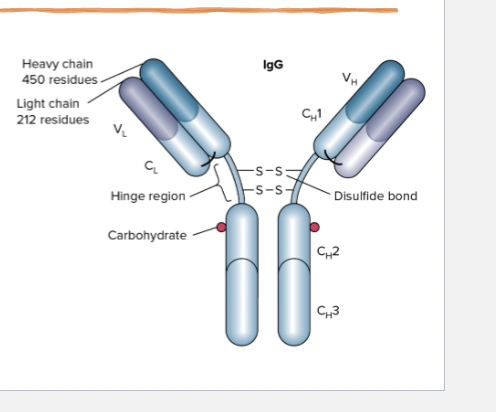
The main class found in the blood (20% of
all plasma protein, 80% of immunoglobulin
pool).Largest quantities are produced in
secondary responseAntigen binding site: Binds antigen, Tissue-
binding sites attach to receptors on
phagocytic cells. Binds microorganism to
engulfing cells. Can opsonize bacteria,
viruses, toxins.Is the only antibody that can cross the
placenta. Also found in milk and colostrum.
IgG Antigen Binding site
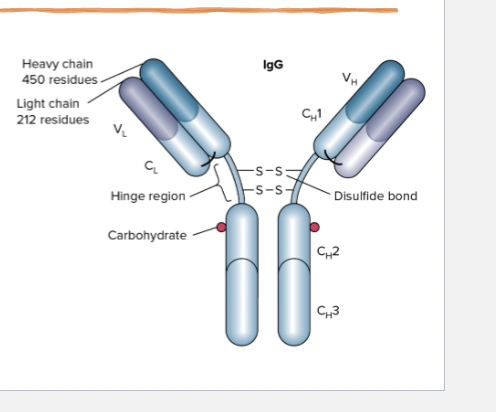
Binds antigen, Tissue- binding sites attach to receptors on phagocytic cells. Binds microorganism to engulfing cells.
Can opsonize (to coat a pathogen like bacteria or a virus) with special molecules called opsonins (such as antibodies or complement proteins to mark it for destruction), viruses, toxins
IgM components
Makes up 5% of the immunoglobulin pool.
Found as a monomer on the surface of B cells (BCR) and is secreted as a pentamer by plasma cells.
Monomers are arranged in a pinwheel held together by a disulfide bond and a joining(J) chain.
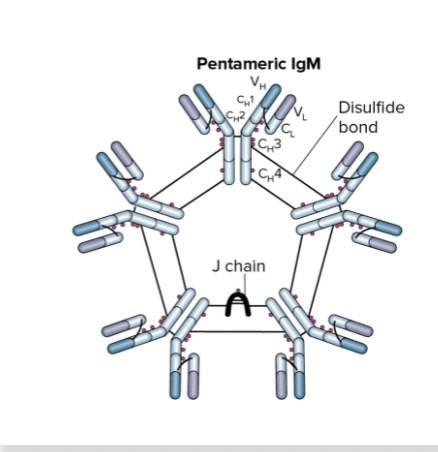
Where is IgM found?
Found as a monomer on the surface of B cells (BCR) and is secreted as a pentamer by plasma cells.
IgM important info
Soluble, pentameric antibody is the 1st antibody secreted in primary response after antigen stimulation.
Only antibody produced following T- cell independent B-cell activation.
1st antibody made by fetus.
Too large to cross the placenta.
Stays in the blood.
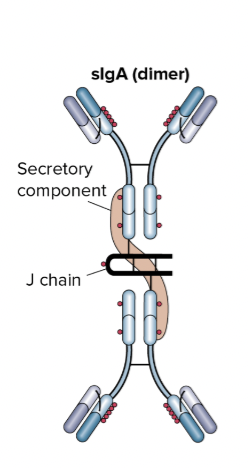
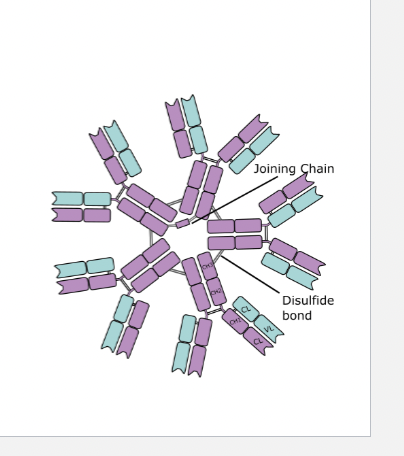
IgA components
Makes up about 12% of immunoglobulin.
Small amount in blood (Monomeric) but very abundant in mucus membrane secretions.
Secretion IgA consists of 2 monomers held together by a J chain (join chain) which has a secretory component (protects against proteolytic cleave).
Guards entrance into the body by binding to antigens on microorganisms before they enter the blood.
Immune barrier.
Where are igA usually found?
Small amount in blood (Monomeric) but very abundant in mucus membrane secretions.
High concentration in colostrum where it provides mucosal immunity.
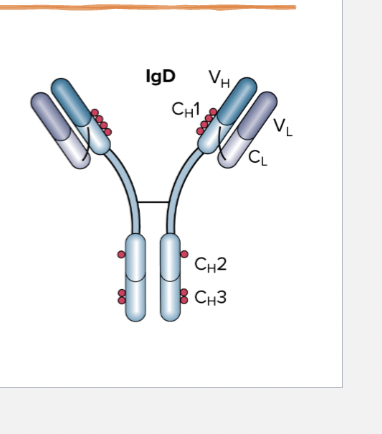
IgD components
Found on B-cell membranes (BCR) like IgM.
Is rarely secreted.
It may help initiate immune responses and some allergic reactions.
In addition, IgD levels rise in some autoimmune conditions.
Where is IgD usually found?
on B-cell membranes (BCR) like IgM.
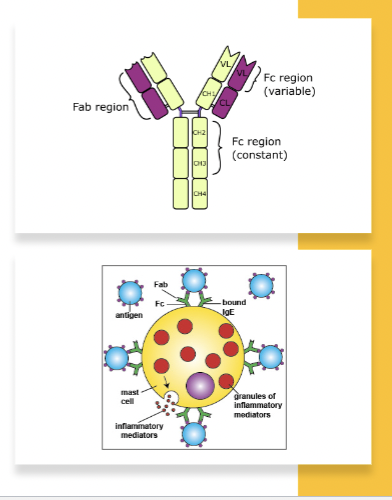
IgE components
High Affinity for receptors on the plasma membranes of
basophils in the blood or mast cells in the tissues (via
tissue binding site).The antigen-binding sites is free to bind antigens to
which humans can develop allergies, such as drugs,
pollens, and certain foods.When IgE is triggered by an antigen, the associated
basophils or mast cells secrete various inflammatory
mediators, such as histamine, which produces allergy
symptoms.High levels in body fluids and skin/tissue.
Rare in the blood.
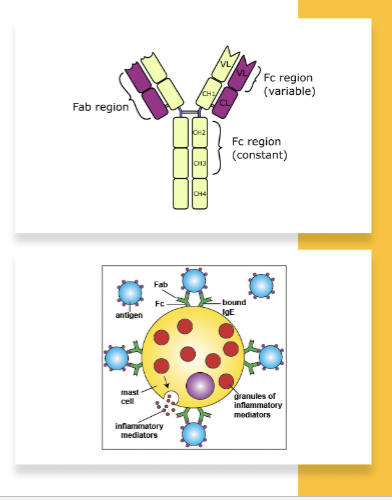
Where us IgE usually found?
on the plasma membranes of basophils in the blood or mast cells in the tissues
High levels in body fluids and skin/tissue.
Rare in the blood.
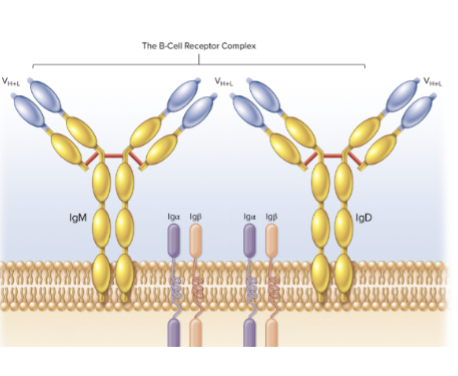
B cell receptors components
Composed of IgM or IgD antibodies.
They do not span the full
membrane.They work by signal transduction
using the accessory proteins (Ig-
a/Ig-b to transmit the signal
2 B cell activation components
T-cell dependent B-cell activation
Vs.T-cell independent B-cell activation
T-cell dependent B-cell
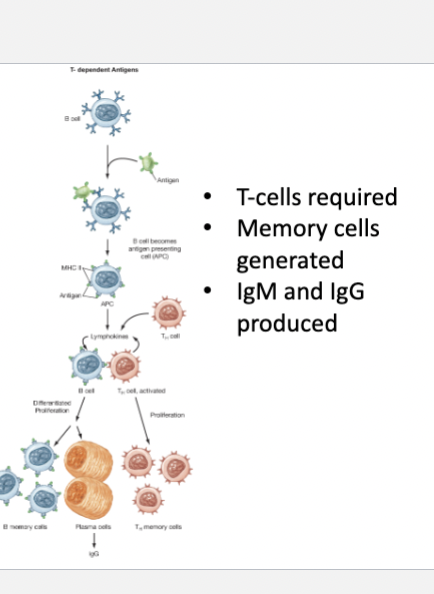
activation
T-cells required
Memory cells generated
IgM and IgG produced
T-cell independent B-cell activation

No T-cells required
No memory cells generated
Only IgM produced

T-cell dependent B- cell activation components
B cell receptor binds antigen --> internalized via endocytosis.
The internalized antigen is broken down and presented on B-cell MHC class II and move to the B-cell surface.
The presented antigen is recognized by CD4 helper T cells.
The activated TH2 cells release cytokines that stimulate proliferation of B cells.a
T-cell dependent B- cell activation components CONTINUED
After several round of replication, the activated TH2 cells stimulate production of memory B cells. Subsequent exposures.
First class of antibodies generates are IgM. TH2 will stimulate the plasma cells to generate IgG, IgA or IgE in a process called class switching.
Class switching occurs using a process of genetic rearrangement of the gene segments encoding one of the antibody regions.
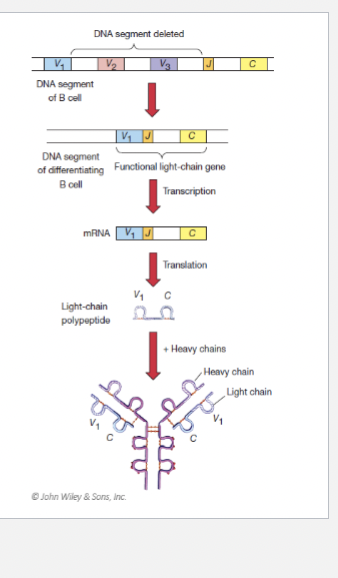
Class switching
occurs using a process of genetic rearrangement of the gene segments encoding one of the antibody regions.
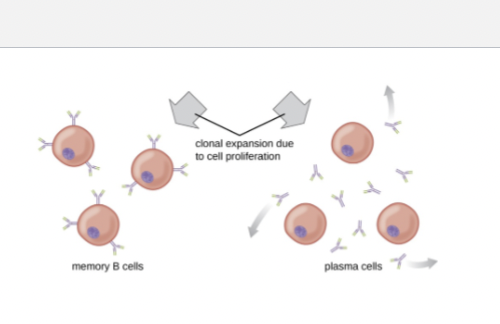
Primary response

Is the first time the antigen encounters the B-cells.
This is a slower response

Secondary response
is when the antibodies are produced by memory cells.
Very rapid and results in clearing the microorganism before you even begin to experience symptoms.
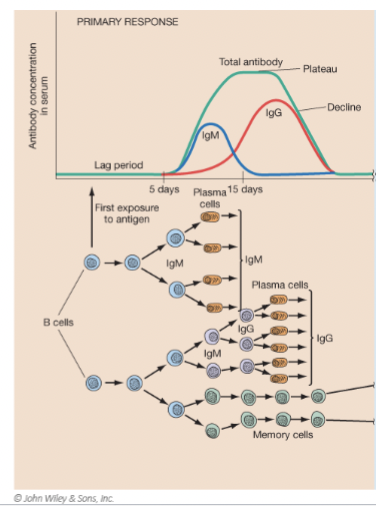
Primary response components
After B-cell encounter, the B-cell divides to make plasma
cells.Within a few days, antibodies are in the blood.
Concentration increase over 10 weeks.1st antibodies are IgM (directly binds foreign molecules).
During T-cell–dependent activation, B cells undergo class switching, usually producing IgG or IgA. These antibodies bind more effectively than IgM.
As the microorganisms are cleared, antibody production drops.
B-cell proliferation results in production of memory B-cells (persist in lymphoid tissue). Can survive for months years without dividing.
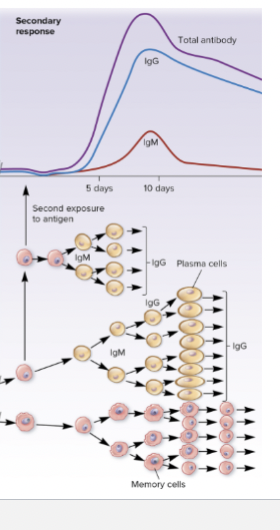
Secondary Response components
Antigen is recognized by memory b-cell.
Because the memory cells are present in high number, they begin making antibodies quicker than 1st response.
They can also begin dividing quicker and making antibodies in greater quantity faster.
IgM is produced before IgG.
IgM is produced in smaller quantities over a shorter period. IgG is produced sooner than primary response + in much larger quantities.
The secondary response is characterized by a rapid increase in antibodies, most of which are IgG.
Heterogeneity: Diversity
The ability of the immune system to generate many kinds of antibodies which react to nearly 10 trillion epitopes.
Humans have only 30,000 genes. How is this possible?
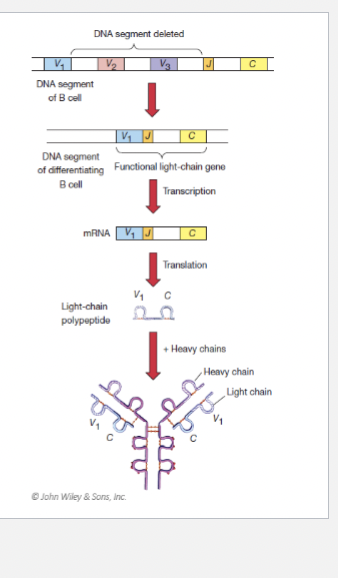
4 types of Antibody Diversity
Combinatorial Joining
Nucleotide Insertion
Splice-site Variability
Mutation
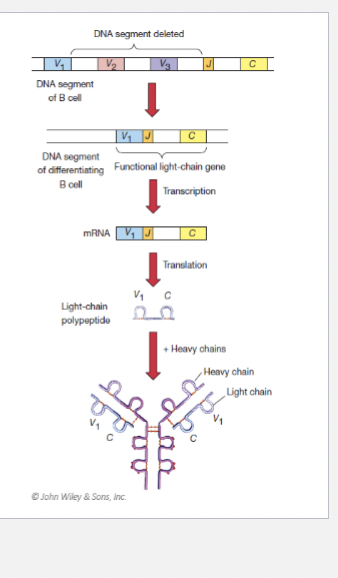
Combinatorial joining:
Segments of DNA are removed during differentiation.
Nucleotide insertion:
During combinatorial joining, nucleotides are
inserted which increases diversity.
Splice-site variability:
CCTCCC + TGGTGG = CCGTGG. Can vary.
Mutation:
Mutations in that occur during T-helper cell stimulation generate variation in antibodies
Clonal Cell Theory
Lymphocytes express receptors to distinct antigen, determined before antibody-antigen interaction.
Binding of antigen to antibody → proliferation of clone daughter cells.
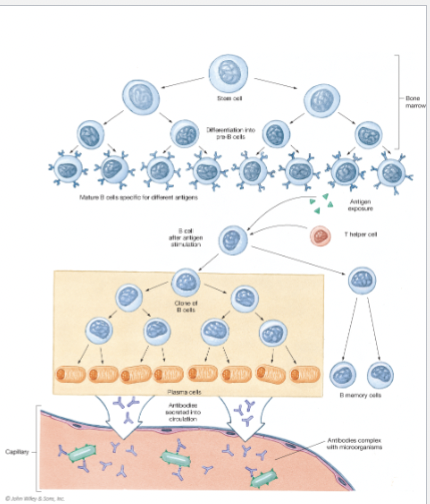
5 Consequence of antibody binding to antigen
Precipitation
Neutralixsation
Complement Fixation
Aggulation
Osponization
Type I Hypersensitivity (Immediate / Allergy)
Mechanism: IgE-mediated
Trigger: Allergens (pollen, peanuts, animal
dander, etc.)Cells involved: Mast cells and basophils
Onset: Seconds to minutes
Pathology: Degranulation → histamine
release → vasodilation, bronchoconstrictionExamples: Anaphylaxis, allergic rhinitis,
asthma, hiv
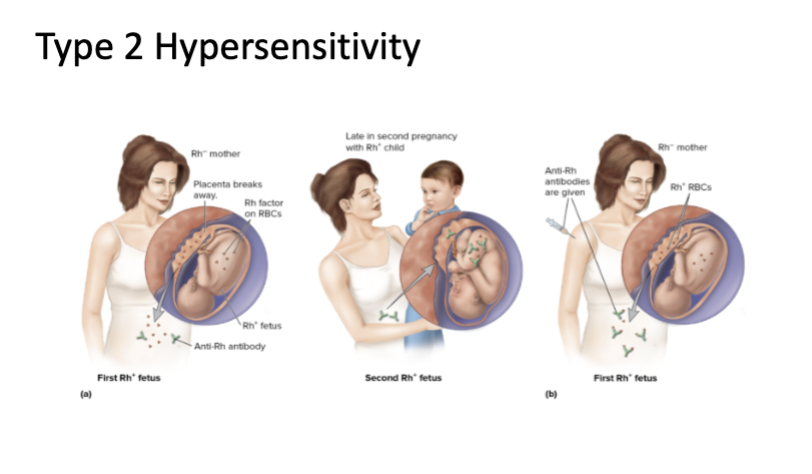
Type II Hypersensitivity (Cytotoxic)
Mechanism: IgG or IgM antibodies against
cell-surface or extracellular matrix antigensTrigger: Self-antigens or foreign cell antigensCells involved: Complement, NK cells,
macrophagesOnset: Minutes to hours
Pathology: Antibody binding leads to cell
destruction (lysis), inflammation, or
dysfunctionExamples: Hemolytic anemia, Rh
incompatibility. Graves disease (antibody-
mediated dysfunction)
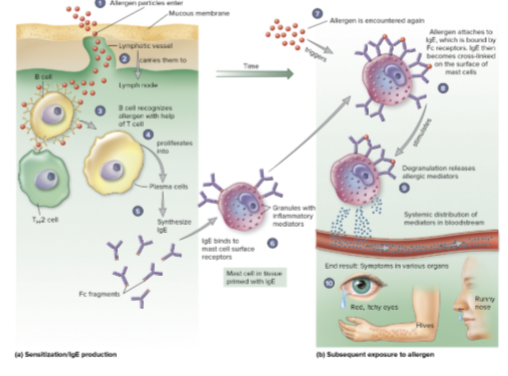
Type 1 Hypersensitivity overview
IgE medicated stimulation of Mast cells.
Mast cells are degranulated and release histamine.

Type 2 Hypersensitivity Overview
Cytotoxic reaction that results in
the destruction of host cells.IgG and IgM trigger cells within the
host.This is seen during blood
transfusion if wrong blood type
is used.
Transplant and Tissue rejection
Transplant from a genetically different person within the same species = allografts.
Transplant from a different species = xenografts (heart valve).
Typically, reactions do not occur in locations where there is little blood circulating like the eyes or heart valve.
Unless all MHC proteins are the same between donor and recipient, the transplanted organ can be rejected. For example, like twins.
• Organ rejection can occur in 1 or 2 ways:
• Host versus graft disease
• Graft versus host disease
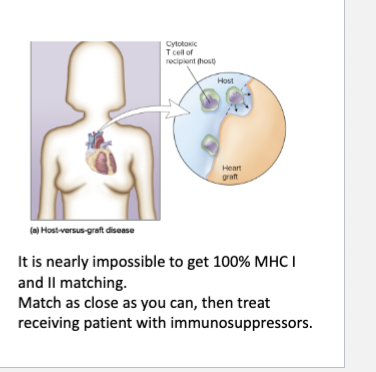
Host versus graft disease: Self vs. non-self
This can occur by two different mechanisms involving T
cells.First: This mechanism relies on the fact that MHC molecules on the surface of transplanted organs are different from those of the host.
Donor MHC class 1 are recognized as non-self by cytotoxic T-cells. CTL will destroy the donated tissue.
Second: Here, the T-helper cells recognize foreign MHC molecules and are triggered to release cytokines.
Cytokines will stimulate the recruitment
of macrophages.Macrophages will enter the graft and stimulate destruction of the organ.
It is nearly impossible to get 100% MHC I and II matching.
Match as close as you can, then treat
receiving patient with immunosuppressors.
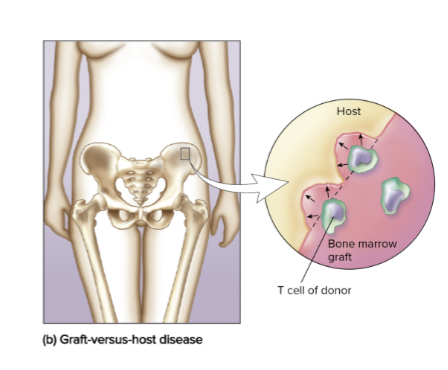
Graft versus host disease
Here, the host cells are attached by the transplanted organ.
Typically seen in bone marrow transplants.
The foreign marrow recognizes the host as being foreign and mounts an immune response against their cells.
Because bone marrow transplant include the introduction of stem cells, more matching criteria needs to be met.
Still followed up with immunosuppressor drug