gastric secretions II
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
what is the structure of the pancreas?
bile duct
duodenum
blood vessel
pancreatic duct
endocrine - islets of langerhans cells secrete hormones into blood vessels
exocrine - acinar cells secrete digestive enzymes into the pancreatic duct
what is the functional unit of the exocrine pancreas?
duct cells secrete aqueous NaHCO3- rich secretions (~75%)
granules accumulate during fasting
acinar cells secrete enzymes and NaCl rich secretions (~25%)
what is pancreatic exocrine secretion compose of?
1-1.5 L per day
isotonic or slightly hypertonic and alkaline (pH ~8.0)
functions:
digestion - lipase, amylase and proteolytic enzymes important for nutrient digestion
pH buffering - high levels of HCO3- neutralise HCl emptying from stomach
what do proteolytic enzymes require
activation!
zymogens = inactive enzymes, released from the acinar cells by exocytosis - activated in the upper cell intestine
what is the aqueous component of pancreatic secretion?
generated from columnar epithelial cells that line the ducts
resting - spontaneous secretion
stimulated by secretin (interlobular duct)
what does the aqueous component of pancreatic secretion look like in the unstimulated state?
occurs in the lobules, plasma like in nature
low levels of aqueous secretion
don’t get modification in the interlobular duct
what does the aqueous component of pancreatic secretion look like in the stimulated state?
occurs in the interlobular duct, stimulated by secretin
high levels of aqueous secretion that are high in HCO3- and low in Cl-
CFTR could drive HCO3- and Cl- exchange
CFTR has conductance to both Cl- and HCO3-
predominant pathway for HCO3- in the stimulated state
unclear whether less Cl- secreted and or what is in 1ry secretion is diluted
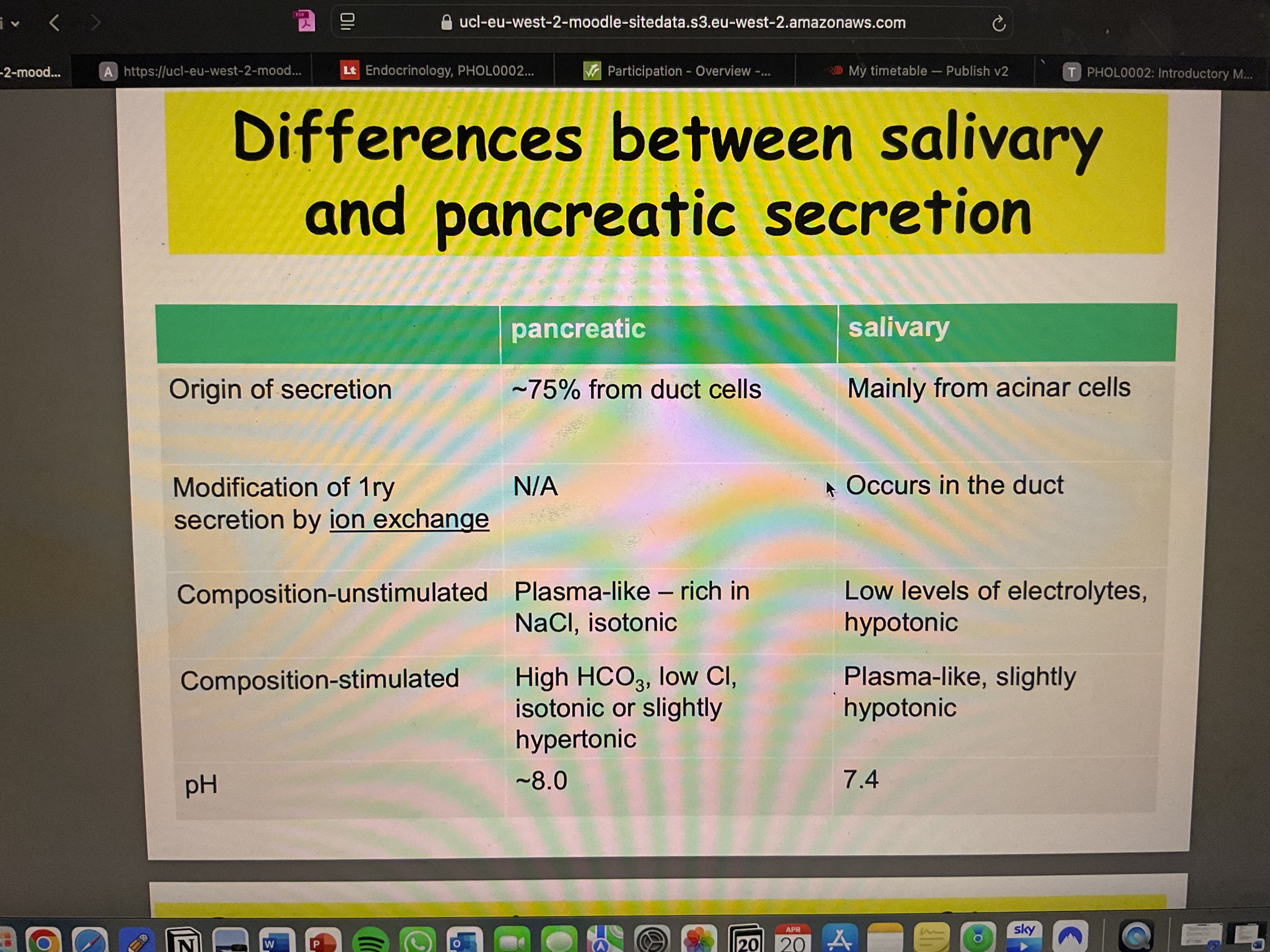
what are the differences between salivary and pancreatic secretion?
describe pancreatic disease in cystic fibrosis.
pancreatic acinar cells secrete large quantities of enzymes
Cl- and HCO3- are normally secreted into the ductal lumen via CFTR. this provides a driving force for the fluid movement necessary to maintain solubility of ductal enzymes
in cystic fibrosis:
impaired CFTR function results in low volumes of more acidic fluid, leading to enzyme precipitation
the resultant obstruction of ducts in CF causes:
pancreatic insufficiency
reduced efficiency of nutrient digestion
progressive pancreatic damage
how is pancreatic secretion controlled?
nerves - parasympathetic
hormones:
cholecystokinin (CCK)
secretin
gastrin - from stomach
3 phases of pancreatic secretion:
cephalic - 20%
gastric - 10%
intestinal - 70%
what is the cephalic phase?
sight, smell, taste, chewing → vagal stimulation → secretion of Ach at vagal nerve endings → acinar duct cell secretion → enzymes → HCO-3
what is the gastric phase?
gastric dimension → vago-vagal reflex → secretion of Ach at vagal nerve endings → - acinar & duct cell secretion → enzymes & HCO3- → gastrin release from g cells (via gastric nerves)
peptides in antral lumen → gastrin release from g cells → acinar cell secretion → enzymes & HCO3-
what is responsible for the intestinal phase of pancreatic secretion?
hormones
increase H+ (pH <3.5) - cause secretin release
fat & protein digestion products cause CCK release
what is the pH-stat function of secretin?
secretin controls duodenal pH by:
increase pancreatic HCO3- secretion
decrease gastric emptying
decrease gastric acid secretion
what are the functions of the liver?
carbohydrate metabolism
protein metabolism
lipid metabolism
iron storage
detoxification
synthesis and secretion of bile
what does the liver lobule contain?
central vein
liver cells
bile canaliniculi
portal vein, hepatic duct, bile duct
what are the characteristics of bile?
cholesterol
bile salts & bile acids
water & electrolytes
bile pigments (bilirubin)
0.6-1L per day
isotonic & alkaline
yellow-green in colour
what is the production of bile?
bile acids are derivatives of cholesterol
bile acids are synthesised by hepatocytes or extracted from the blood by an active process
bile acids are conjugated in hepatocytes to form bile salts which are actively secreted into the bile canaliculi
Cl-, HCO3-, Na+, H2O are then added to the hepatic bile as it moves along the bile duct
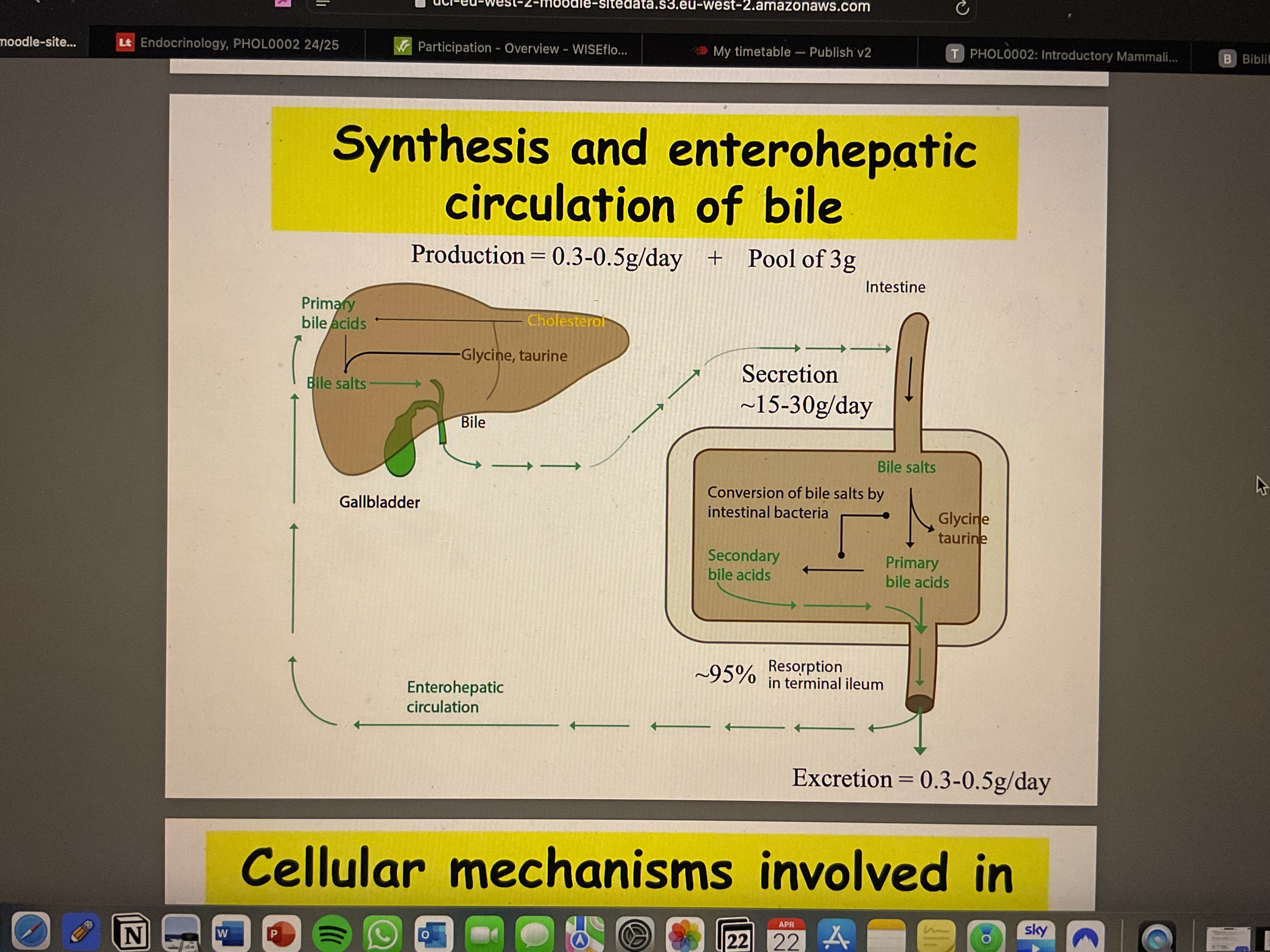
how is bile circulated?
production = 0.3-0.5g/day + pool of 3g
excretion = 0.3 - 0.5g/day
what are the cellular mechanisms involved in bile secretion?
two component:
bile acid-dependent
Na+/BA transporter
95% BA recycled
bile acid-independent
BA conjugated
secreted with Na+ & H2O
in duct Na+, HCO3-, H2O
how is hepatic bile along the bile duct modified?
similar mechanisms to pancreatic secretions
volume is not to the same extent as the pancreas
what is the role of the gallbladder?
stores up to 50% of hepatic bile during the inter digestive phase
concentrates hepatic bile by absorbing Cl-, HCO3-, Na+ and H2O
bile salts in gallbladder are concentrated up to 20-fold
presence of chyme in the duodenum stimulates the release of CCK which causes contraction of the gall bladder
how is bile modified in the gallbladder?
large and long lateral channels creates local high osmotic pressure
concentrated bile → ‘critical micellar concentration’
how is bile secretion regulated?
PNS stimulates blood flow & therefore BA recycling
fatty acid & amino acids in chyme entering the duodenum stimulate secretion of CCK into the blood
acidic chyme entering duodenum stimulates secretion of secretin into the blood
CCK causes contraction of gallbladder
secretin enhances flow of bile rich in HCO3- from liver
what is the role of bile in fat digestion & absorption?
Digestion
emulsification of fat - increases efficiency of lipase action
activation of pancreatic lipase, cholesterol esterase
Absorptive
micelle formation - a micellar solution differs from an emulsion in that:
a far soluble compounds are in solution
much smaller particles (greater stability)
micelles are essential for uptake of fat-soluble compounds, BUT are not absorbed into the epithelial cell at the same time as the fat
how is fat emulsified?
in the stomach, ingested fat form large fat globules
as the fat globules enter the duodenum, they are coated with bile salts
fatty droplets are pulled off the large fat globules and a stable emulsion is created
how are mixed micelles formed?
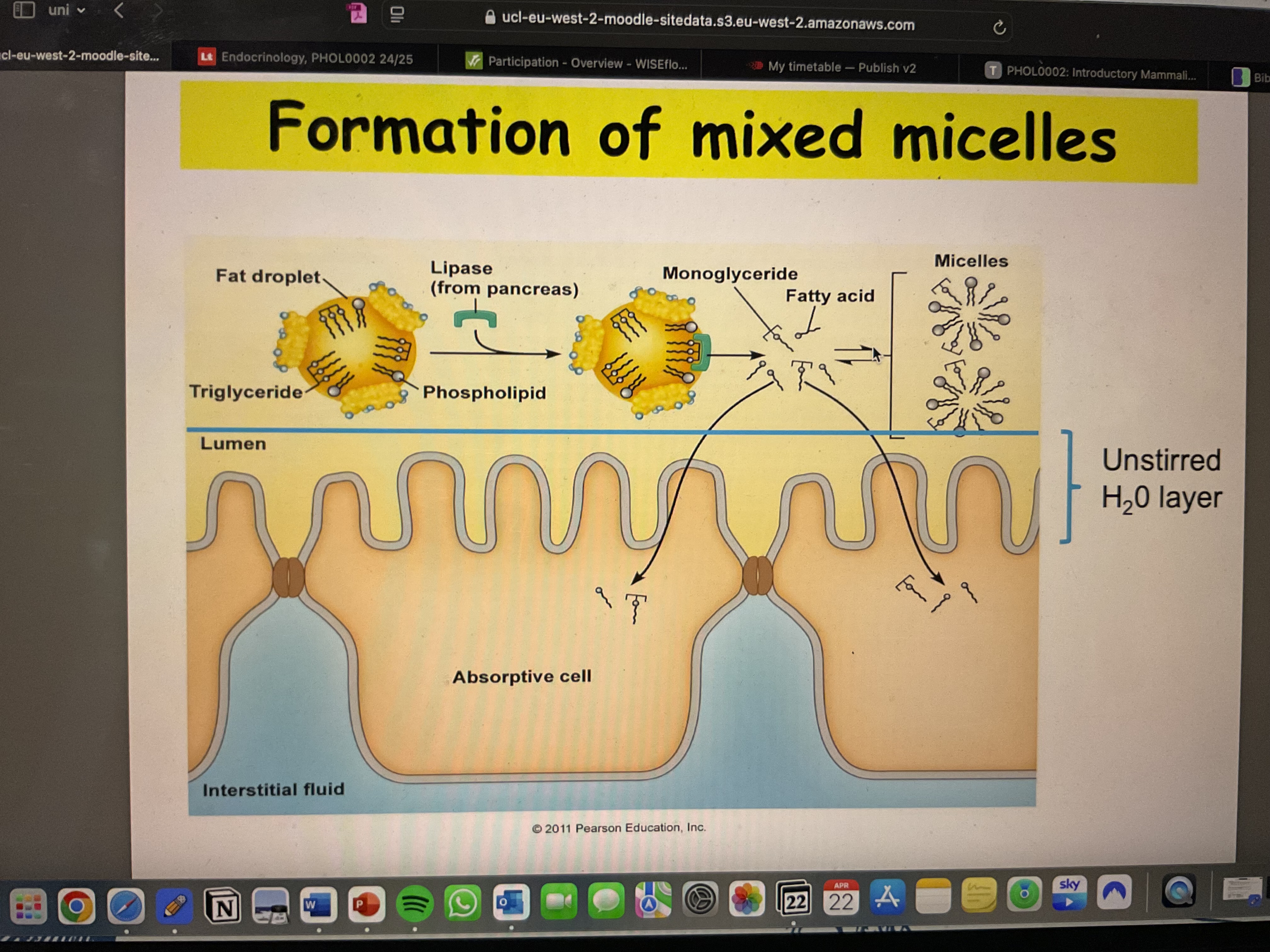
why are micelles important to fat absorption?
made in liver
are formed of around 20-40 bile salt molecules and lechitin
they absorb fat-soluble vitamins, cholesterol, fatty acids and monglycerides
hydrophilic shell allows the micelle to cross the unstirred water layer to the epithelial surface
explain intestinal absorption of fat absorption.
unstirred H2O layer
~80g/day absorbed by jejunal enterocytes
resynthesised to triglycerides
packaged into chylomicrons
bile acids (from micelles) are actively absorbed in terminal ileum
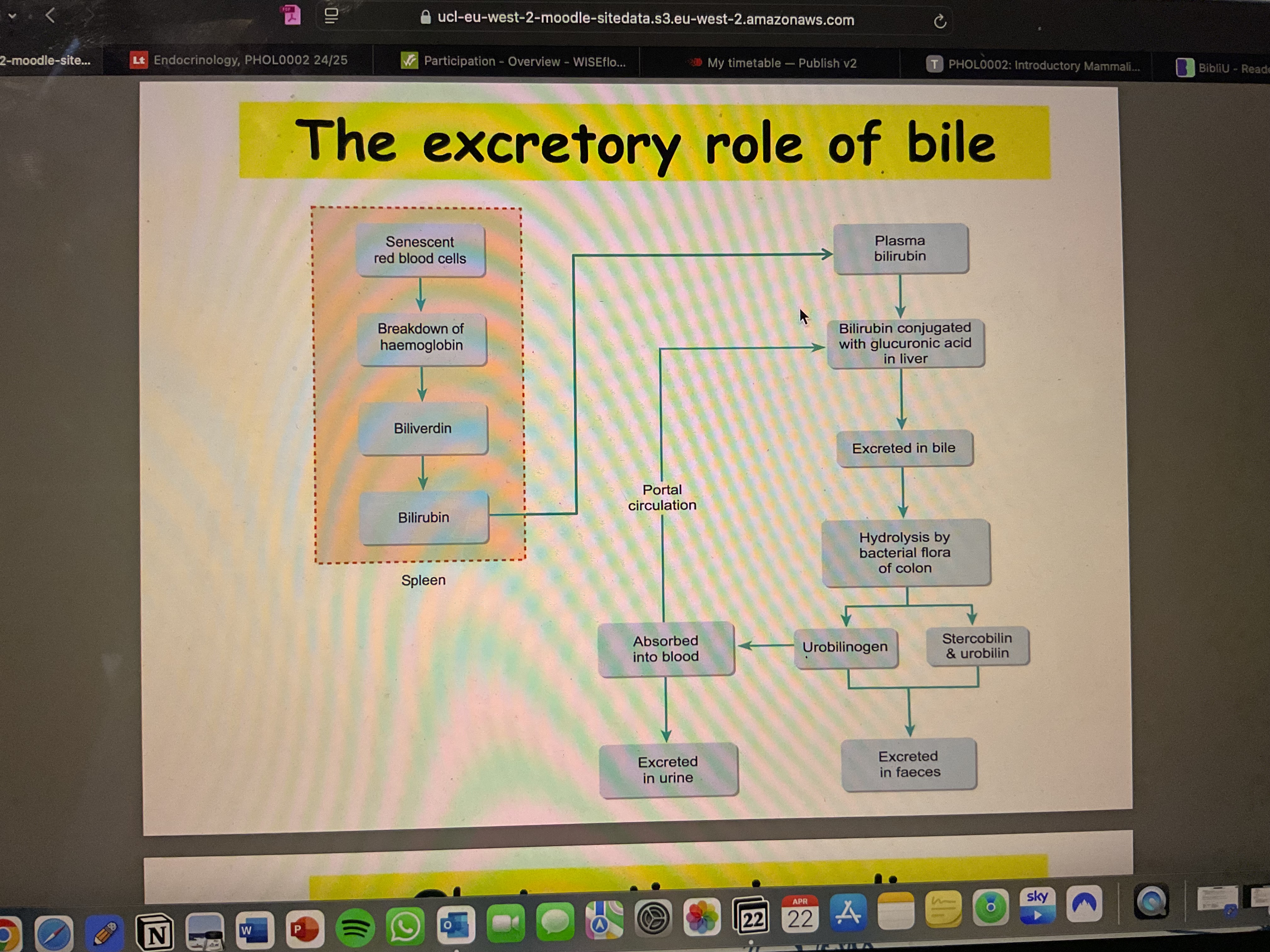
what is the excretory role of bile?
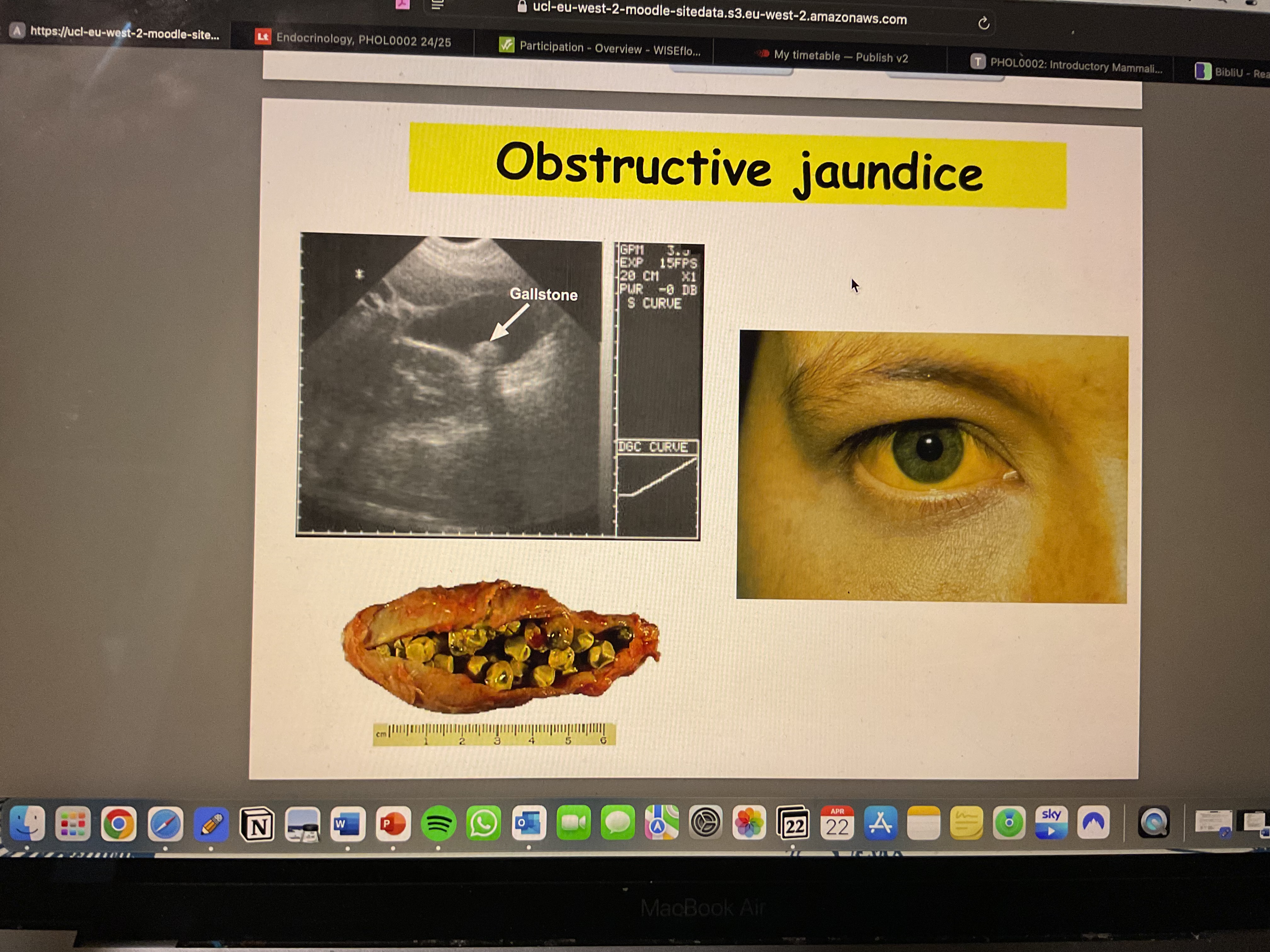
what is obstructive jaundice?