Protozoan Quiz
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
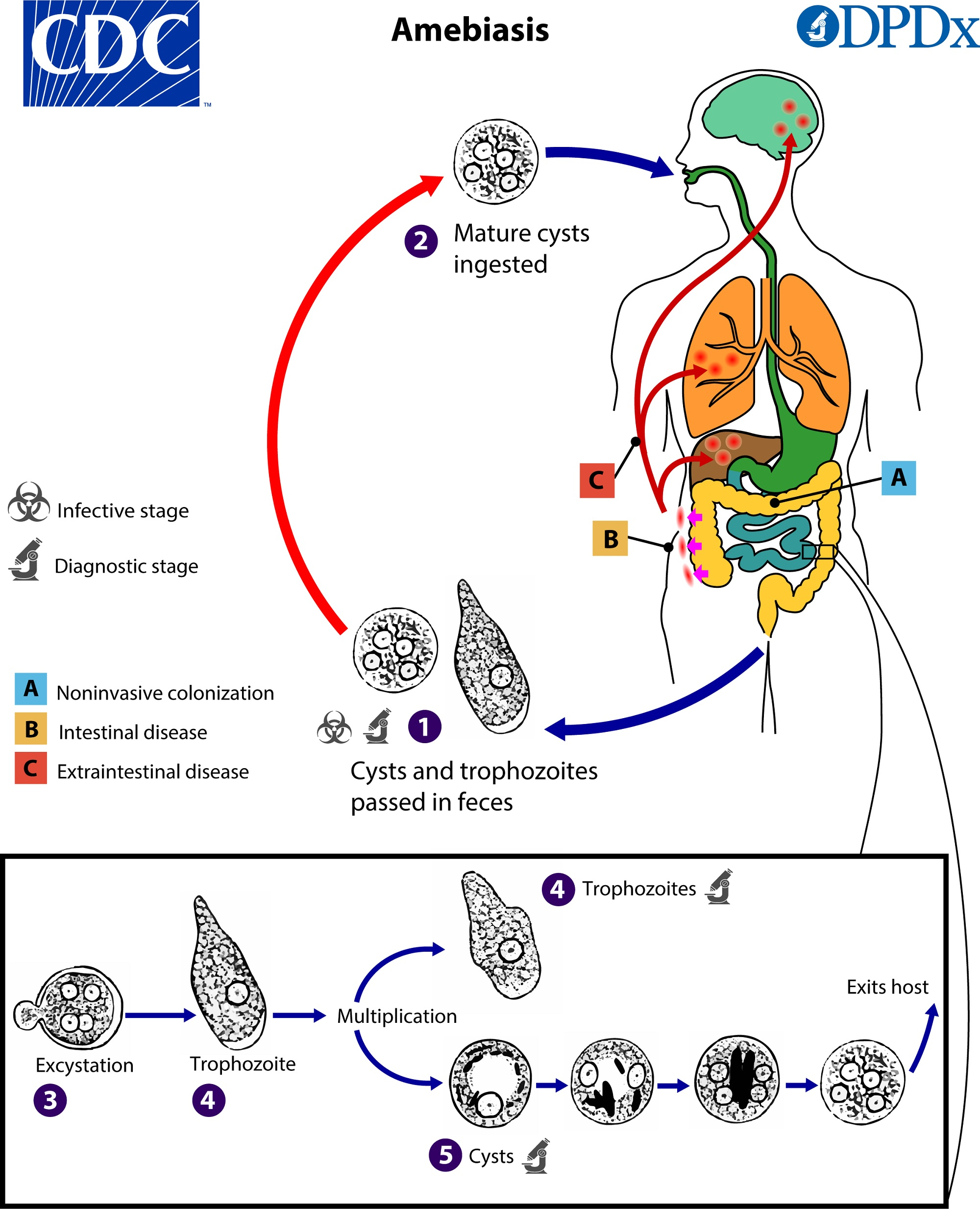
Ameobas
Unicellular
Eukaryotic (more complex than bacteria)
Transmission: Ingestion of cysts from food and water contaminated with fecal material

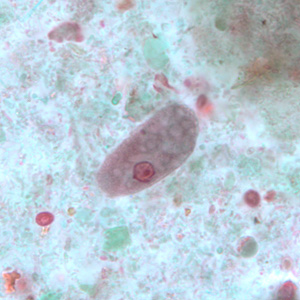
Whats the troph parasite? (20 um)
Entamoeba histolytica (20 u)— Pathogenic
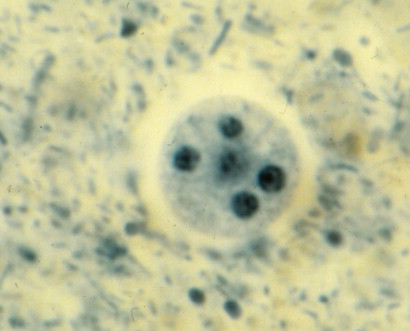
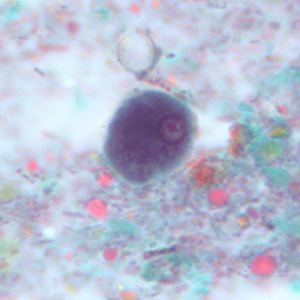
Whats the cyst? (10-20 um)
Entamoeba histolytica (20 u)— Pathogenic
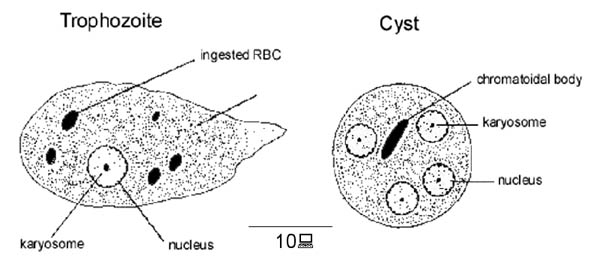
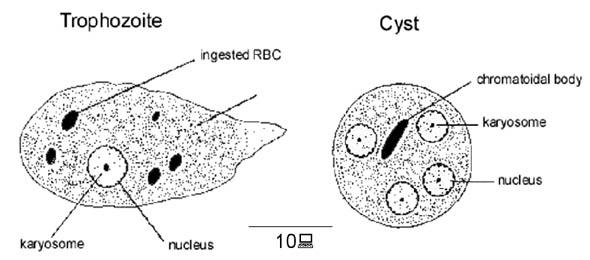
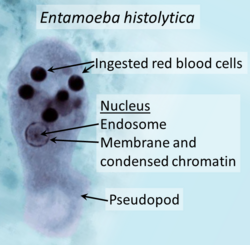
Entamoeba histolytica
Cyst= 10-20 um
Troph= 15-20 um
Type: Amoeba
ID (lab clues): Troph — thin, delicate chromatin ring; central compact karyosome; ingested RBCs (key). Cyst — up to 4 nuclei, smooth-ended chromatoid bars. ~20 μm troph.
Host/site/lifecycle: Humans; colon; fecal-oral cyst ingestion; asexual division; invasive potential (portal spread to liver).
Symptoms / disease links:
Non-dysenteric GI illness (abdominal pain, nausea, flatulence, irregularity, fatigue).
Amoebic dysentery — bloody/mucous stools, flask-shaped ulcers, perforation risk, typically no fever.
Amoebic liver abscess (sterile core; amoebae at margins), lungs as secondary; amoeboma can mimic colon cancer.
Co-infections: Bacterial GI pathogens can co-infect.
Bloody stool? Yes.
Entamoeba dispar
Cyst= 10-20 um
Troph= 15-20 um
Commensal Amoeba
ID: Morphologically identical to E. histolytica; no RBC ingestion.
Pathogenic? No.
How to differentiate: Rapid EIA specific for E. histolytica (or molecular).
Bloody stool? No.

Entamoeba hartmanni
Troph=8-10 um
Cyst= 6-8 um
Commensal
Type: Amoeba
ID: “Small E. histolytica.” Troph ~8–10 μm, cyst ~6–8 μm.
Bloody stool? No.

Entamoeba coli
Troph= 15-50 um
Cyst= 10-35 um
commensal
Type: Amoeba
ID: Largest intestinal amoeba. Troph 15–50 μm with eccentric karyosome, coarse/lumpy chromatin; Cyst 10–35 μm with ≥5 nuclei; splintered chromatoid bars.
Bloody stool? No.
Pitfall: Often mistaken for E. histolytica — count nuclei and check nuclear detail.
Entamoeba polecki
cyst= 9-25 um
troph=10-25 um
commensal
Type: Amoeba (pigs/monkeys; under-diagnosed).
ID: Mixed features between E. histolytica and E. coli; variable chromatoid bodies.
Testing emphasis: You won’t be asked to visually ID on tests.

Endolimax nana
Troph= 6-12 um
Cyst= 5-10 um
commensal
Type: Amoeba
ID: Smallest intestinal amoeba. Troph 5–15 × 6–8 μm with big dense karyosome and thin membrane (“ball-and-socket”); cyst 6–8 μm, nuclei look like “potato with eyes.”
Stains: Iron hematoxylin historically helpful to separate from Iodamoeba.
Bloody stool? No.
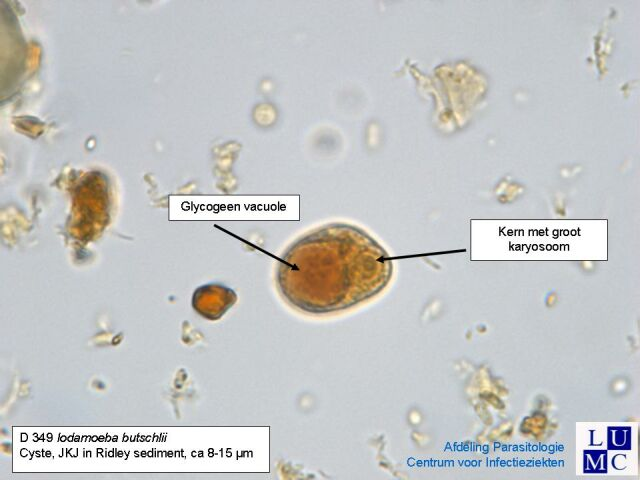
Iodamoeba bütschlii
Troph= 8-20 um
Cyst= 5-20 um (usually 10-12 um)
commensal
Type: Amoeba
ID: Cyst with single nucleus and large karyosome, glycogen vacuole (iodine clears fast, so appears as a large clear vacuole); troph has large dense karyosome and “dirty” cytoplasm.
Bloody stool? No.

Blastocystis (formerly B. hominis)
opportunistic; variable
Type: Stramenopile (grouped here); many subtypes; fecal-oral.
ID: Vacuolated form most common in stool: 5–40 μm with huge central vacuole (90 percent of cell) and 2–4 peripheral nuclei; cyst ~3–10 μm and hard to find.
Symptoms: Often asymptomatic; when ill — nonspecific abdominal pain, bloating, acute/chronic diarrhea, gas; association with IBD noted. No fecal leukocytes.
Co-infections: Very common.
Stains/tests: Concentration + Trichrome
Bloody stool? No.
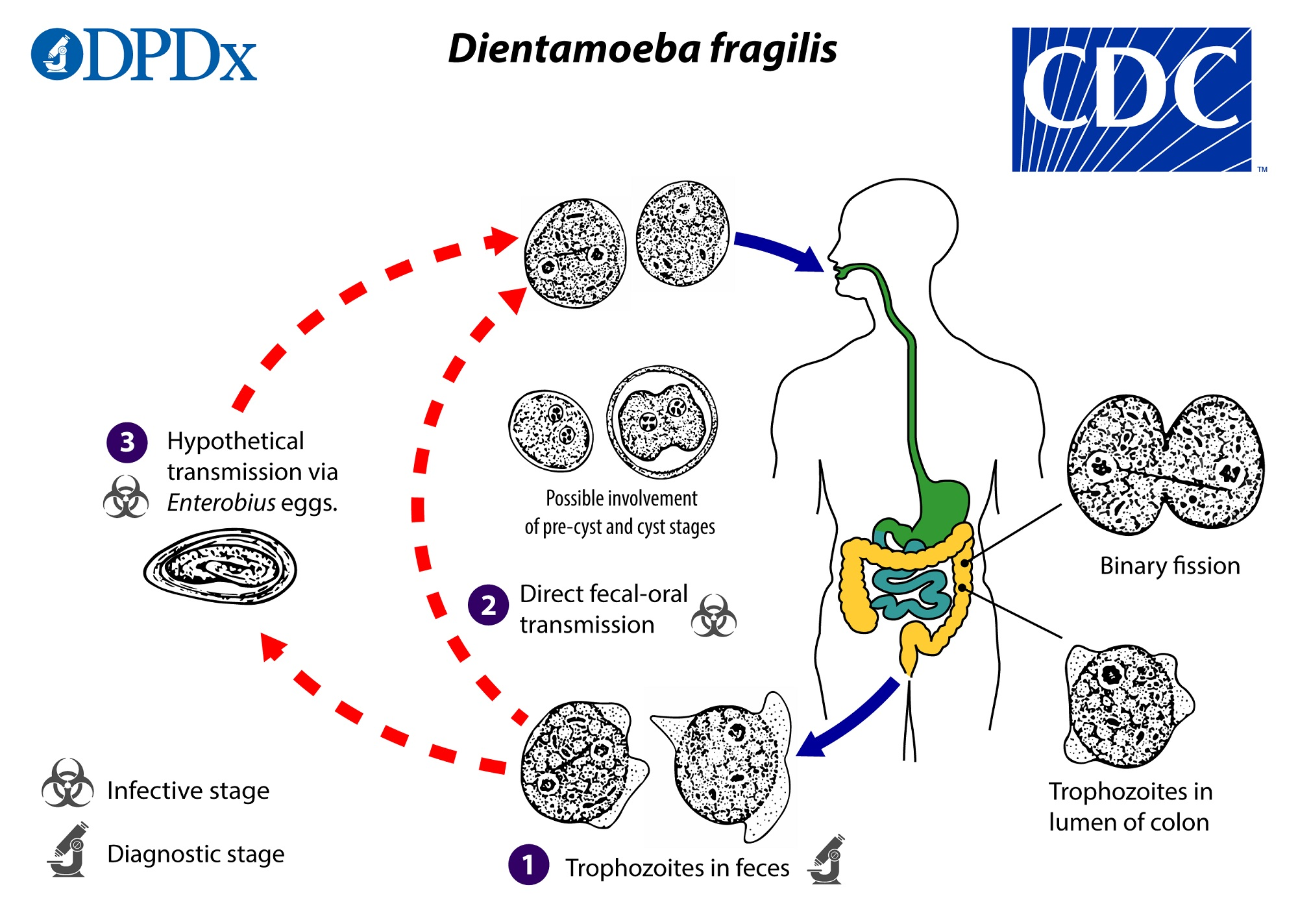
Dientamoeba fragilis
Troph= 5-15 um
Cyst= 4-8 um
occasionally pathogenic
Type: Flagellate (but no external flagella); worldwide.
ID: 4–12(15) μm trophs; 1–2 nuclei (20–40 percent are uninucleate); fragmented karyosome (3–5 granules); no peripheral chromatin; “dirty” cytoplasm. Not seen on wet preps or in concentrates; cyst stage recently described.
Symptoms: Colicky pain, fatigue, weight loss (variable).
Bloody stool? No.
Testing: Permanent stained smears; molecular if available.
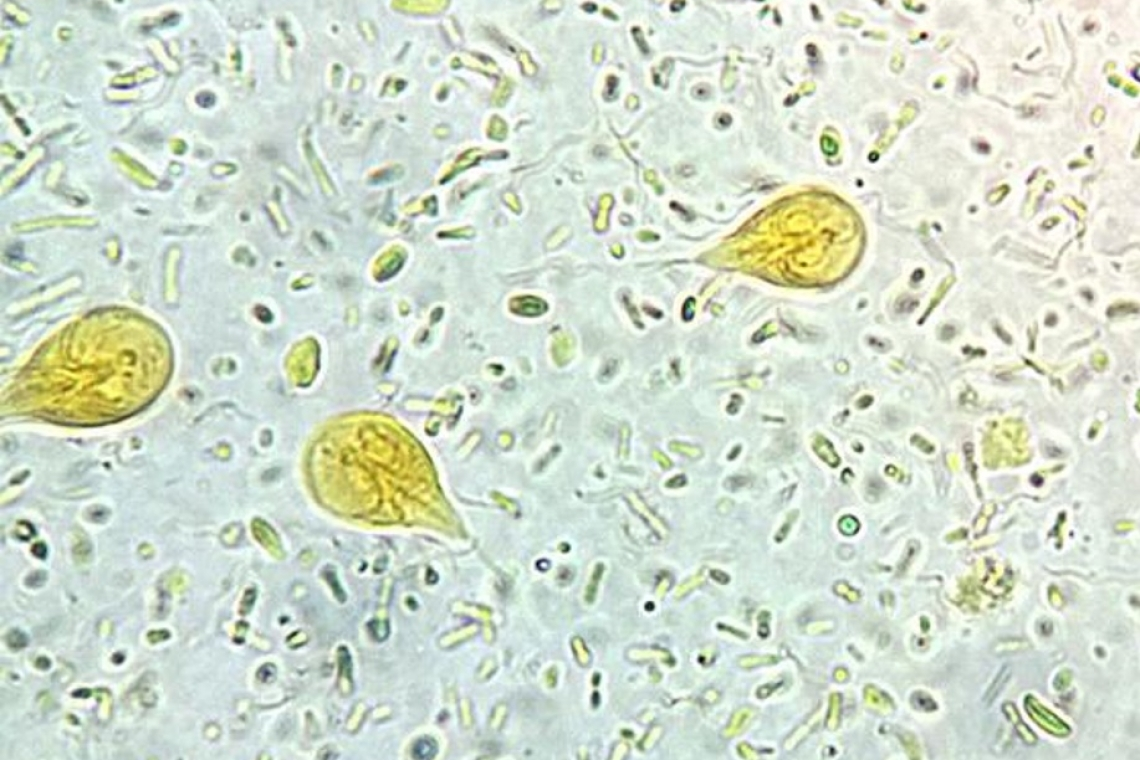
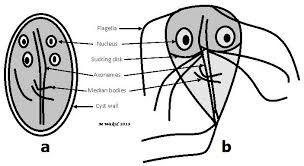
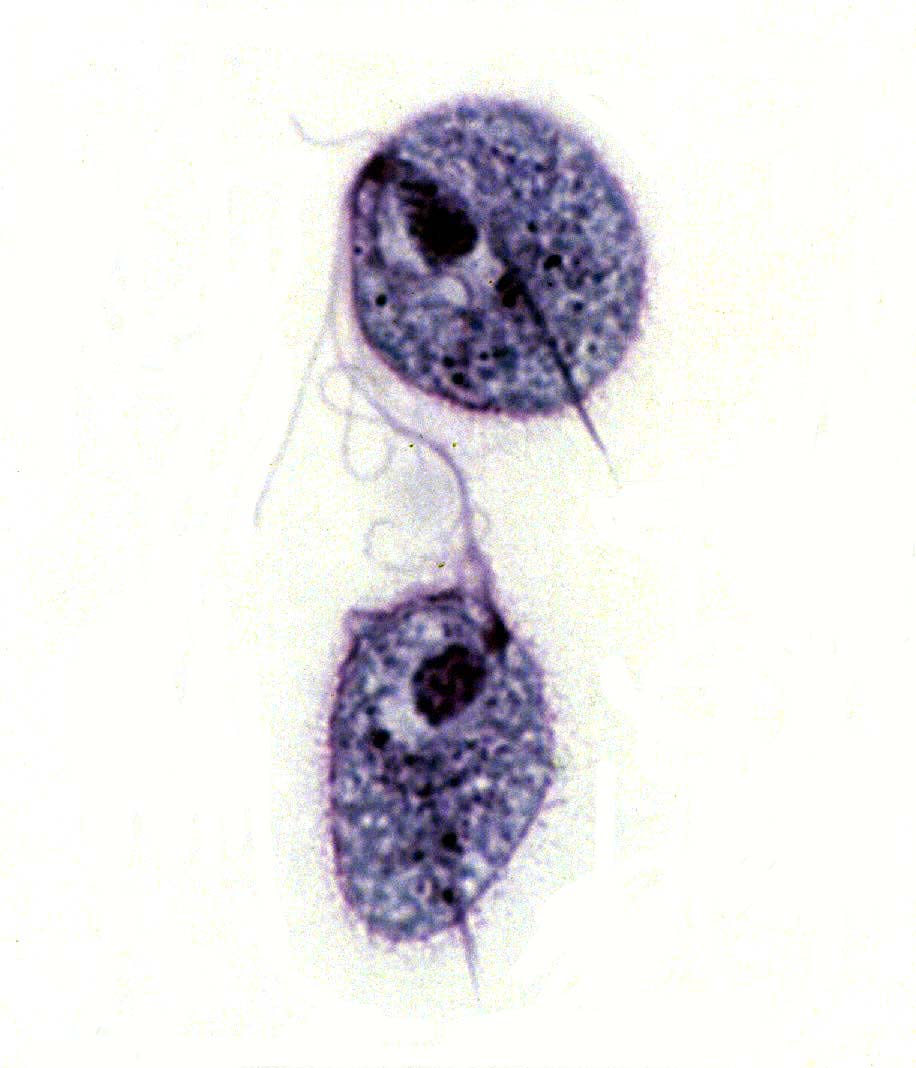
Giardia lamblia / intestinalis / duodenalis
Troph= 10-20 um
Cyst= 11-14 um
pathogenic; common in US
Type: Flagellate
ID: Troph 10–20 μm with 2 nuclei, 2 parabasal bodies, 1 axostyle, 8 flagella; falling-leaf motility; cyst 11–14 μm with up to 4 nuclei (often pale on stains). Attaches to upper small intestine without invasion.
Epi: Daycare, campers/untreated water, beavers/other reservoirs, MSM; incubation 12–20 days.
Symptoms: Steatorrhea — greasy, foul, gray/green, explosive watery diarrhea, flatulence, cramps, distention/belching; chronic relapsing pattern possible.
Bloody stool? No.
Testing: FE concentration + Trichrome; collect ≥3 stools on non-consecutive days (intermittent shedding). Rapid EIA, string test

Trichomonas vaginalis
Troph= 7-25 um
pathogenic (urogenital)
Type: Flagellate
ID: Only troph stage, found in urine, vaginal/prostatic secretions; sexual transmission.
Symptoms: Women — itching, burning, dysuria, foamy yellow-green discharge with odor. Men — often asymptomatic; may have prostatitis/urethritis.
Testing: Direct wet prep for motile trophs; (molecular/antigen tests exist, but your deck emphasizes wet prep recognition).

Trichomonas hominis / tenax
Troph=6-20 um
nonpathogenic
Type: Flagellates
ID: T. hominis colon, T. tenax mouth; no cyst stage; look for motile trophs on wet prep; hard to see on permanents.
Chilomastix mesnili
Troph= 10-15 um
Cyst= 6-11 um
commensal
Type: Flagellate
ID: Troph 10–15 μm tear-drop with eccentric nucleus/karyosome and a visible cytostome (“mouth”); rotating/wobbling motility. Cyst lemon-shaped with anterior “nipple”; 6–11 μm.
Bloody stool? No.
Where: Cecum/colon.
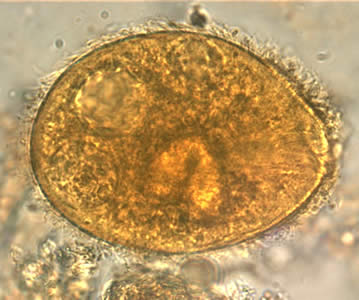
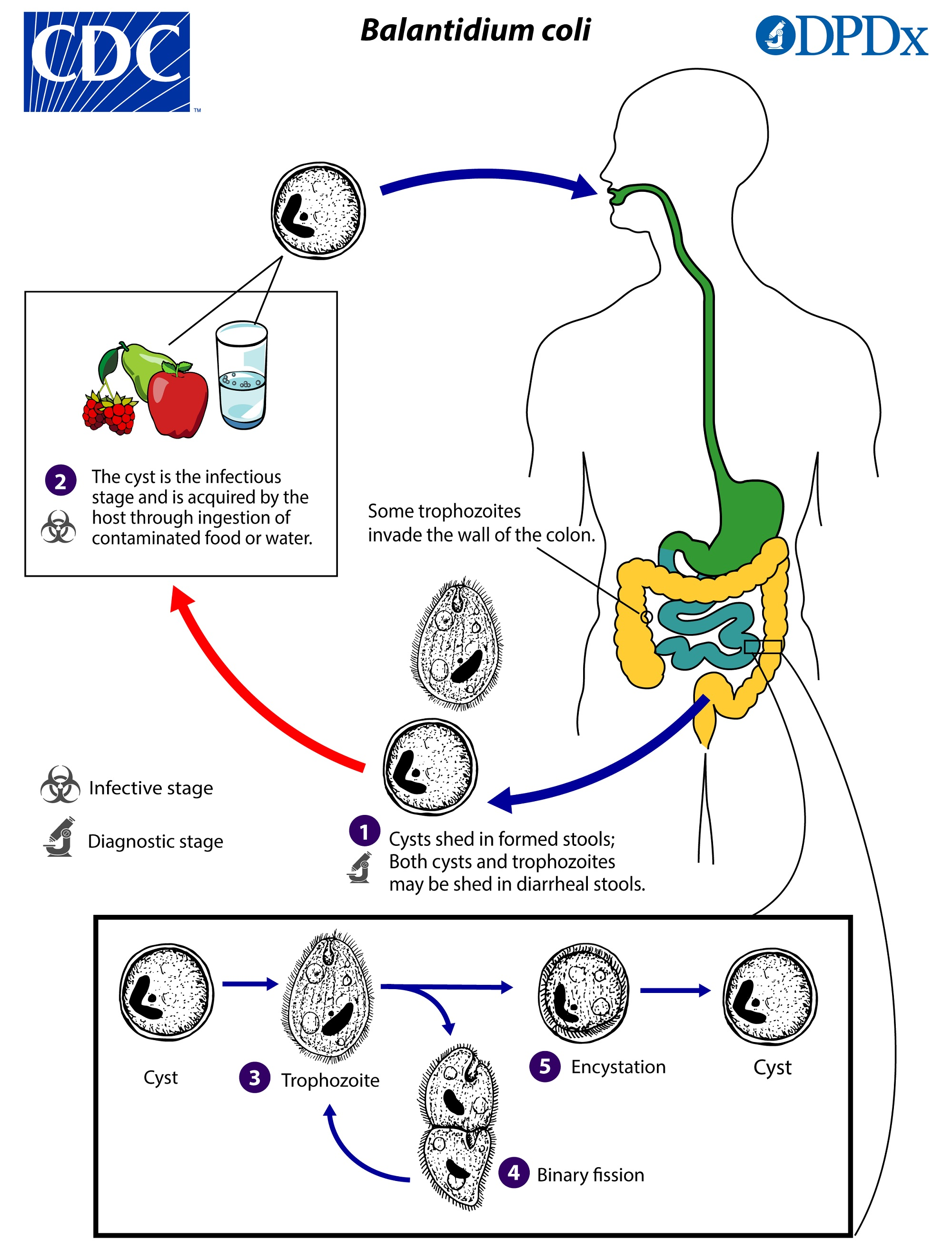
Balantidium coli
Troph= 50-100 um
Cyst= 50-70 um
pathogenic
Type: Ciliate (largest protozoan of humans)
ID: Troph 50–100 μm with cilia, macronucleus (+ micronucleus), cytostome; cyst 50–70 μm with thick wall, macronucleus, +/- cytostome, no cilia.
Host/site/lifecycle: Humans, close association with pigs; colon/cecum; ingest cysts from contaminated food/water.
Symptoms: Asymptomatic to chronic non-bloody diarrhea; fulminant disease causes mucoid, bloody stools, weight loss, explosive diarrhea; flask-shaped lesions and perforation possible (hyaluronidase implicated).
Bloody stool? Yes (in severe disease).
Risk: Poor sanitation, alcoholism, malnourishment, immunocompromise.

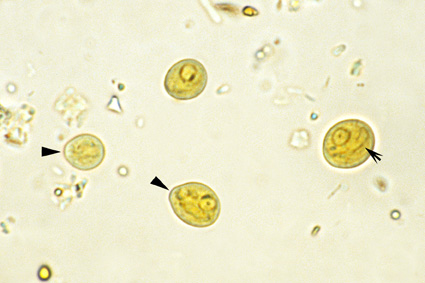
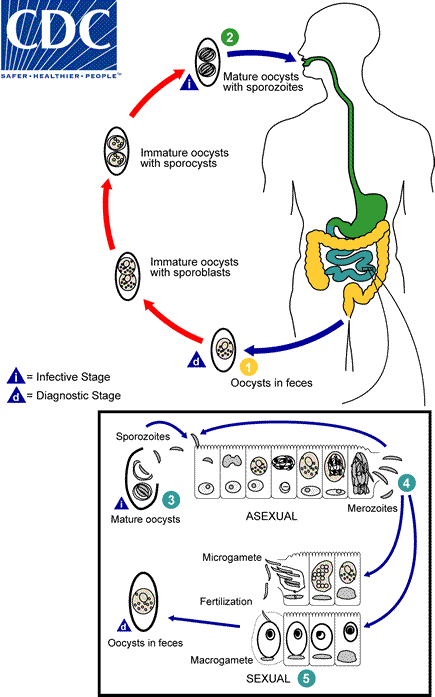
Cystoisospora (Isospora) belli
Troph= 25-33 µm x 10-19 µm
Cyst= 20–33 and 8–19 um
pathogenic
Type: Coccidia; small intestine.
ID: Oocyst: immature with 1 sporoblast; mature with 2 sporocysts, each with 4 sporozoites.
Symptoms: Severe diarrhea, steatorrhea, fever, nausea, weight loss; notorious in HIV-positive patients.
Bloody stool? No.
Stains/tests: Modified acid-fast; stool O&P.

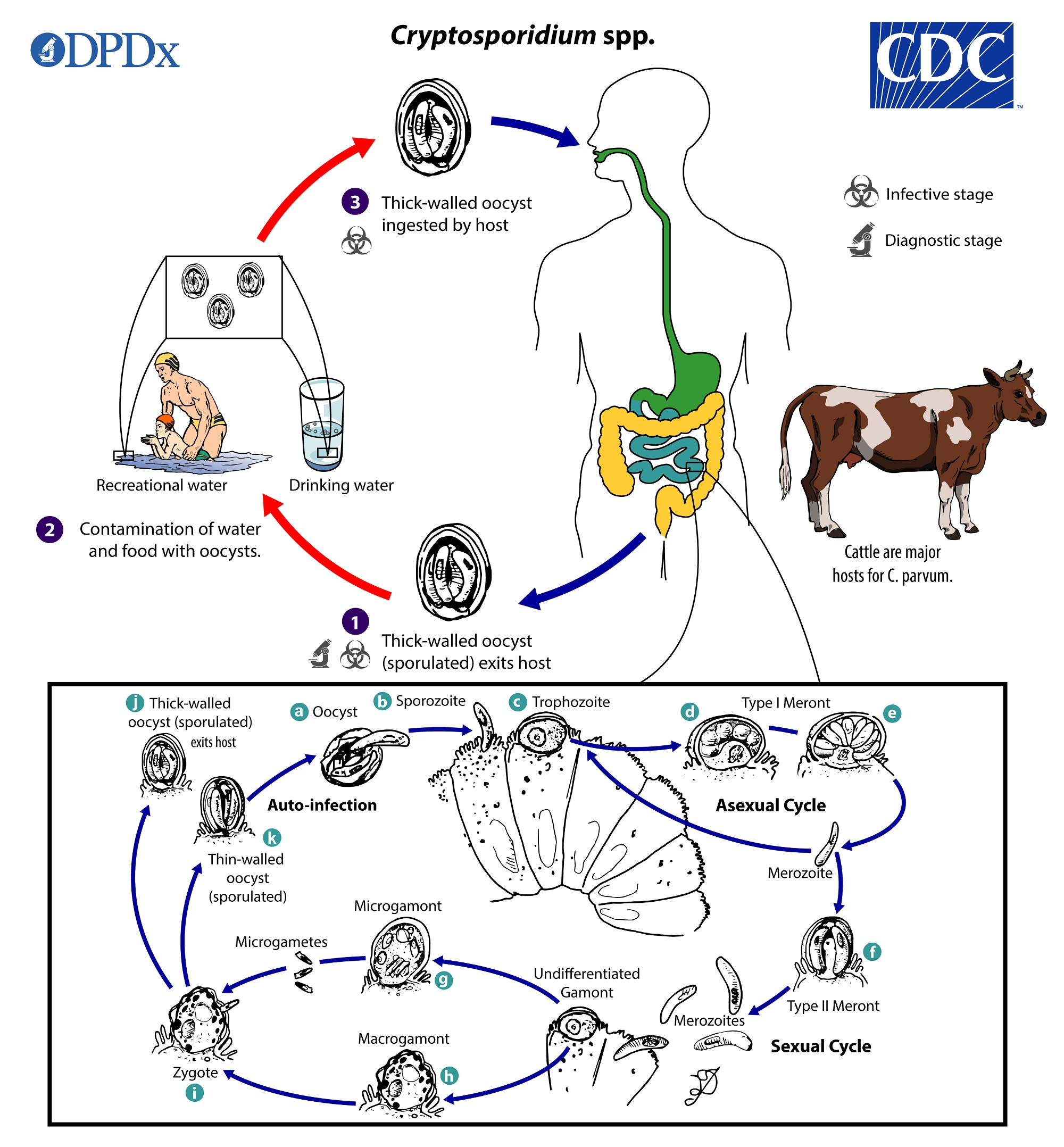
Cryptosporidium parvum
Cyst= 4-6 um
Troph= 2-3 um
Cryptosporidium parvum — pathogenic
Type: Coccidia (infects brush border of small intestinal epithelium).
ID: Oocysts ~4–6 μm.
Symptoms: Profuse watery diarrhea, cramps, nausea, anorexia — self-limited in immunocompetent; chronic/severe and extra-intestinal in immunocompromised.
Bloody stool? No — typically watery.
Stains/tests: Acid-fast; DFA; ImmunoCard STAT lateral-flow EIA; chromogenic immunoassay.
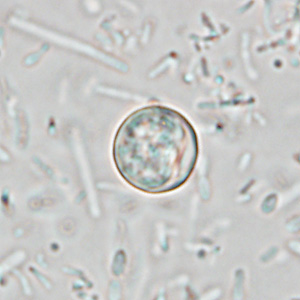
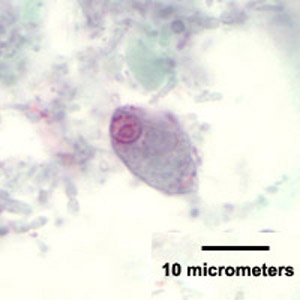
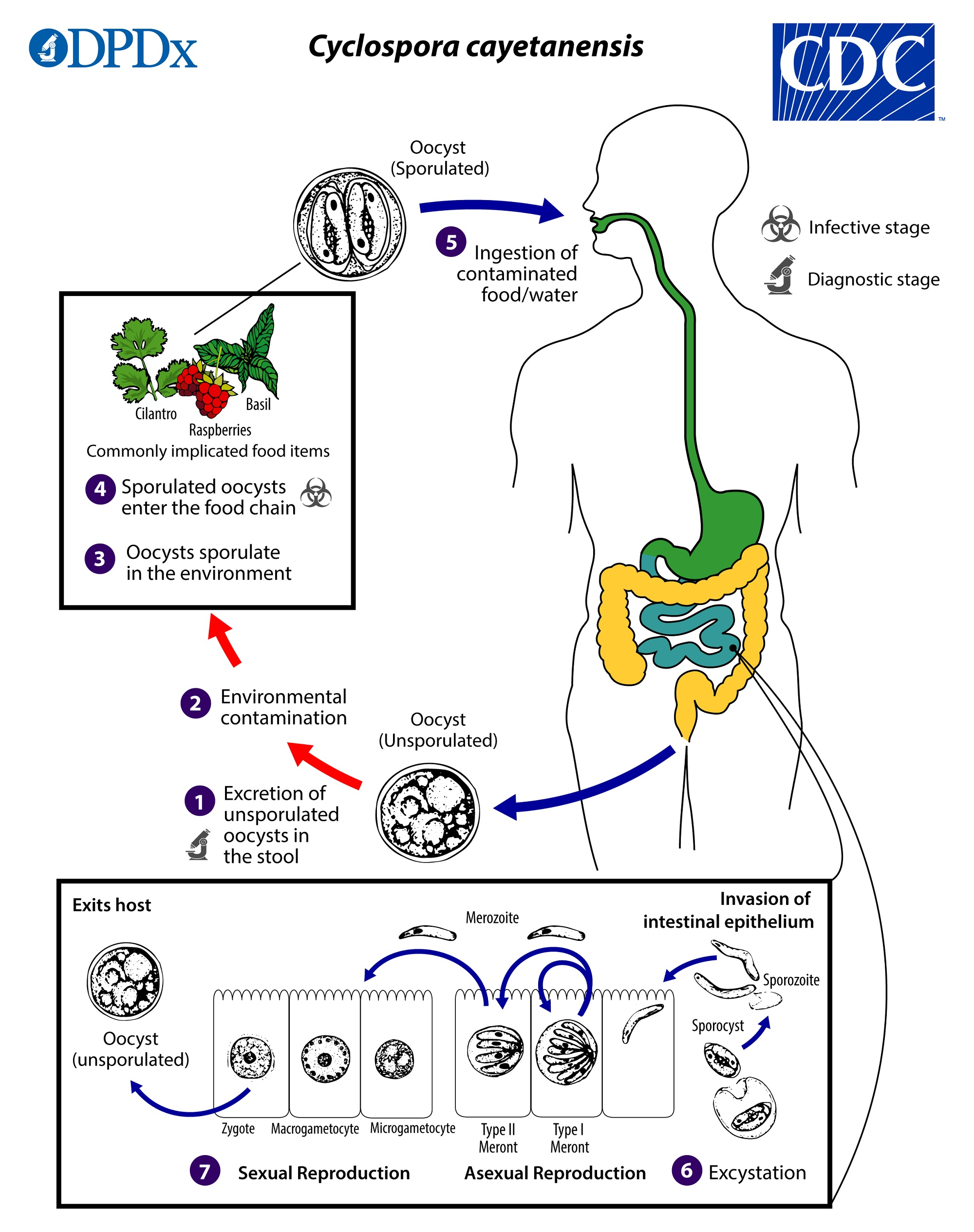
Cyclospora (cayetanensis)
Cyst= 8-10 um
Cyclospora (cayetanensis) — pathogenic
Type: Coccidia; emerging; 8–10 μm.
ID/testing: Requires specific O&P order for Cyclospora; 3 specimens optimal (intermittent shedding).
Symptoms: Flu-like prodrome, explosive diarrhea, weight loss, nausea/vomiting; outbreaks linked to fresh produce.
Bloody stool? No.

Sarcocystis
9–16 μm.
pathogenic (foodborne)
Type: Coccidia; 9–16 μm.
Hosts: Human = definitive host; pig = intermediate (also beef).
Acquisition: Undercooked beef/pork.
Clinical: Foodborne illness; not a common stool O&P target.
Bloody stool? No.
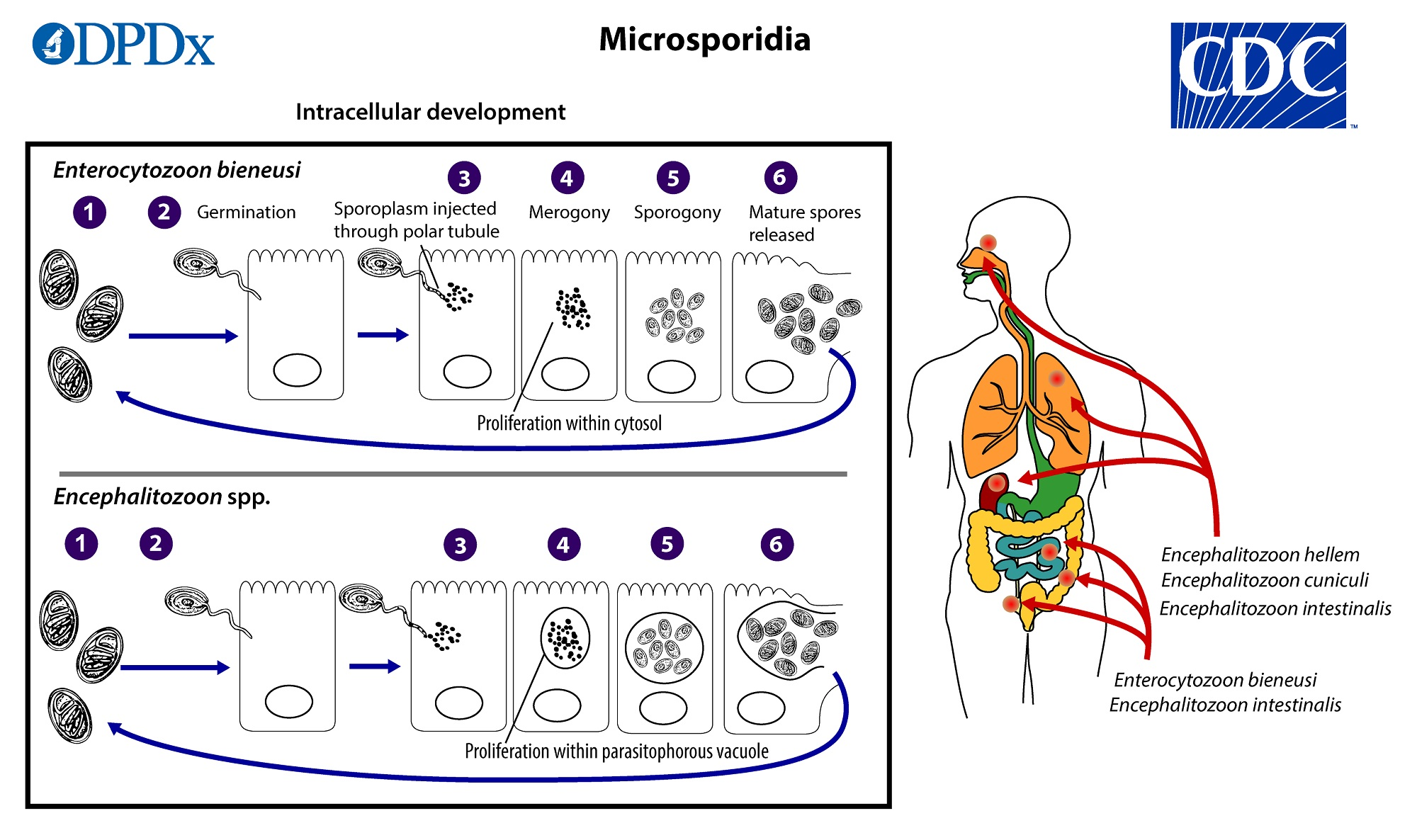
Microsporidia
1.5 - 2 um
pathogenic in immunocompromised
Type: Obligate intracellular; 1.5–2 μm, very small.
Dx: “Impossible to find in feces” on routine O&P; biopsy is the best specimen per deck.
Bloody stool? No.
Which ones cause bloody stool?
Do: E. histolytica (amoebic dysentery), Balantidium coli (fulminant disease)
E. histolytica (pathogenic) vs E. dispar/E. hartmanni/E. coli (non-pathogenic):
RBCs inside troph → points to E. histolytica.
Size (tiny = hartmanni), many cyst nuclei & coarse/eccentric nuclear detail = E. coli.
Antigen EIA specific to E. histolytica or PCR to confirm.
Iron hematoxylin
Classic differentiation aid for small amoebas (Endolimax vs Iodamoeba) in older prep notes
Acid-fast/Modified acid-fast positive?
Cryptosporidium — acid-fast (4–6 μm).
Cystoisospora — modified acid-fast (oocysts with 1 sporoblast → 2 sporocysts with 4 sporozoites each).
(Cyclospora in practice is also acid-fast positive, but your slides focus on ordering specific O&P with three specimens rather than showing the stain panel.)