chapter 3 immunology test 2
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
how long does the immediate innate immune response take
0-4 hours
how long deso the induced innate immunity response take
4 hours to 4 days
how long does the adaptive immune response take
4 hours until the pathogen is destroyed
which 3 cells are involved in the induced immune response and what is their role
macrophages - first to recognize and respond to the pathogen
leukocytes (specifically neutrophils) - called into the site of infection out of the blood
hepatocytes - make acute phase reactants, aid in the clearance of the pathogen, and direct leukocytes to site of inflammation
which 2 cells help recognize self from nonself
macrophages and NK cells
1st effector cells once the pathogen invades
resident macrophages
where are the resident macrophages located
connective tissues in the linings of GI, respiratory tract, lung alveoli, liver
ligand for macrophage CR1
C3b
pathogen C3b surface fragments + degraded by factor I results in
iC3b
iC3b is a ligand for what
macrophages CR3 and CR4
macrophage surface receptors are efficient why?
combination of opsonization by complement and phagocytosis by macrophages
what 5 ligands do CR3 and CR4 recognize
iC3b
LPS (gram - bacteria)
cell-surface structures on yeast
lectins
carbohydrate-binding proteins
examples of lectins
mannose and glucan
scavenger receptors
preference for molecules that are negatively charged
which are scavenger receptors
nucleic acids, gram + and gram - bacteria
what kind of cells are receptors found in
macrophages, monocytes, dendritic cells, granulocytes, and NK cells
how many PRRs are known
100
PRR
pattern recognition receptors
self
normal healthy cell
nonself
microbial cell
altered cell
cancer cell or apoptotic cell
why is there an unequal distribution of receptors
to make sure that at least some of the leukocytes will be able to recognize the pathogen with their innate receptors.
DAMPs
associated with cells that have been damaged
PAMP stands for
pathogen associated molecular patternw
what are PAMPs
components common to many pathogens and/or altered cells and molecules
soluble PRR example
MBL
TLR-4 ligand
LPS
what microorganism does TLR-4 recognize
gram - bacteria
what cells carry TLR-4
macrophages, dendritic cells, mast cells, eosinophils
TLR-7 ligand
single-stranded viral RNAs
cellular location of TLR-4
plasma membrane
TLR-7 recognizes what microorganisms
RNA viruses
what cells does TLR-7 carry
plasmacytoid dendritic cells, NK cells, eosinophils, B cells
where is TLR-7 located
endosomes
TLR-3 ligand
double-stranded viral RNA
TLR-3 recognizes what microorganisms
RNA viruses
TLR-3 is found in what cells
NK cells, dendritic cells, CD8 T cells, various epithelial cells
TLR-5 ligand
flagellin, a protein
microorganisms recognized in TLR-5
bacteria
cells carrying TLR-5
instestinal epithelium
cellular location of TLR-5
plasma membrane
cellular location of TLR-3
endosomes
what leads to TLR-4
LPS → LBP → CD14 → MD2 → TLR4
adaptor protein
MyD88
kinase
phosphorylation
what does IKK stand for
Inhibition of KappaB Kinase
what is the common pathway of intracellular signaling starting with TLR-4
MyD88 binds TLR-4. IKK ends up being activated and it phosphorylates IkB. NFkB is translocated from cytoplasm to the nucleus. directs the transcription of genes for inflammatory cytokines
NFkB stands for
TF nuclear factor kB
what are NOD-like receptors
cytoplasmic receptors for recognition of pathogens
NOD-1
recognizes a degradation product of Gram (-) peptidoglycan
NOD-2
recognizes a degradation product of most bacteria - muramyl dipeptide
what does recognition lead to
NFkB making inflammatory cytokines
pyroptosis
mechanism of death of the macrophage which allows massive release of IL-1. large number of pores are created for release. extreme circumstances
does pryoptosis happen often?
macrophages most likely dont go through this but instead release IL-1 more slowly
netosis
neutrophil specific death
what is the master regulator for inflammation
IL-1
what is IL-1 exactly
inflammatory cytokine made by macrophages that intiates and activates the creation of other inflammatory cytoknes
what two things activate endothelial cells
TNF-alpha and IL-1
CC or CXC means it’s what?
a chemokine
what are the 5 activated cytokines by resident macrophages
TNF-alpha, IL-6, CXCL8, CCL2, IL-12
what does CCXL8 do
recruits neutrophils from the blood and directs them to infected tissue
what does CCL2 do
recruits monocytres from the blood and directs them to infected tissue
IL-12 does what
recruits and activates NK cells to secrete cytokines that strengthen macrophages’ response to infection
what does CCL2 bind to
CCR2
pryogens
raise temperature
what are the 3 pyrogens
IL-1, IL-6, TNF-alpha
sepsis
infection of the blood
what does IL-6 do
acts on local muscle and fat cells to increase temperature and signals to liver cells (hepatocytes) to make acute phase reactants
what are the acute phase reactants
MBL and CRP
CRP stands for
C-reactive protein
3 properties of macrophages
-long lived
-reside in tissues
-work as infection begins (raise alarm to neutrophils)
4 properties of neutrophils
-short-lived
-circulate in blood
-polymorphonucelar leukocytes (PMNs)
-wait for macrophage to sound alarm to enter tissue
are neutrophils present in healthy tissue
no
what attracts neutrophils
release of inflammatory mediators at infection sites
how many neutrophils enter mouth and throat each day
3 × 10^9
after how many rounds of phagocytosis by apoptosis do neutrophils die
1 round
what are the 4 leukocyte adhesion molecules
selectins, vascular addresins, integrins, immunoglobulin superfamily
leukocyte adhesion molecules
four structural classes of adhesion molecules present on white blood cells
what are selectins
carbohydrate-binding lectins. L-selectin
what are vascular addresins
contain carbohydrate groups to which selectins bind
what are the 3 vascular addresins
CD34, GlyCAM-1, MAdCAM-1
what are integrins
typically bind to Ig superfamily proteins. LFA-1
immunoglobulin superfamily
ICAM-1
C3a and C5a
anaphylotoxins- increase inflammation
chemoattractants
nascent
newly formed
4 steps of extravasation
rolling adhesion
tight binding
diapedesis
migration
what receptors are on the surface of a neutrophil
CR1, C3b, CR3 & CR4, CD14, mannose receptors, glycan receptors
primary granular type
azurophilic
secondary granular type
specific
tertiary granular type
gelatinase
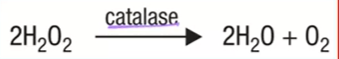
H2O2
hydrogen peroxide. necessary for neutrophils to kill bacteria. it is a toxic oxygen-derived product
lactoferrin
iron binding protein that neutrophils release. has antiinflammatory properties
what’s in primary/azurophilic granules
lysozymes, defensins
what’s in secondary/specific molecules
lactoferrin, lysozyme
enzymatic reaction contributing to neutrophil respiratory burst
neutrophil death process
neutrophil → apoptosis → phagocytosed by macrophage
what does NET stand for
neutrophil extracellular trap
what are NETs
the neutrophil’s nucleus swells and leads to the cell bursting (netosis) leaving behind all of the antimicrobial components of the granules as well as DNA and histones that serve to trap the pathogen
chronic granulomatous disease
if macrophages can’t create NADPH oxidase subunit, they don’t kill efficiently. macrophage gets infected and granulocytes surround it