Urine + Septicemia & Blood Cultures
1/31
Earn XP
Description and Tags
URINE: - List of acceptable and unacceptable urine samples for culture. - Calculating cfu/ml of urine. - Evaluation of urine cultures for UTI. SEPTICEMIA and BLOOD CULTURES: - Features and constituents of blood culture bottles. - Types and classification of septicemia. - Evaluation of blood cultures for septicemia.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
Acceptable Urine Sample
First morning sample
Clean-catch, midstream urine
Straight catheterized urines
Suprapubic aspirate (SPA - anaerobic)
Indwelling catheter
Unacceptable Urine Samples
Pooled 24 hour urine sample
Unrefrigerated or unpreserved urine past 2 hour of collection (Boric acid/ Sodium borate)
Foley’s catheter
For anaerobic culture (except SPA)
How to calculate cFu/mL of Urine (0.01/100 mL)
a. Count the colonies individually or divide the plate in half and multiply by 2.
b. Multiply the count by 100 to get the number of CFU/ml.
Example: 50 colonies x 100 = 50,000 CFU or 5x10^4 CFU/ml.
c. If the number of bacteria is too numerous to count, report the count ≥ 1x10^5 CFU/ml.
Culturing a Urine
If a 10µL loop is used, each colony represents 100 colonies.
If a 1 µL loop is used, each colony represents 1000 colonies.
Evaluation of the Culture: (Organism workup and AST done)
• >10^5 colony forming units (CFUs)/ml of 1 or 2 org. indicates a true infection for most patients
• Quantities < 10^5 CFUs are significant from surgically collected urines, e.g. suprapubic aspirates
• Acute urethral syndrome (acute cystitis): Use 10^2, instead of 10^5, as long as pyuria is present, especially in pregnant or symptomatic women
Distinction between an infection and contamination?
≥ 3 different organisms of any quantity is usually considered contamination while an infection typically shows a predominant organism in significant quantity.
Evaluation of the Culture: Growth on Media
Growth on MAC = non-fastidious, Gram negative rods are present
Growth on the CNA = Gram positive organisms are present
Gram stain each colony type to identify their morphology and guide further testing.
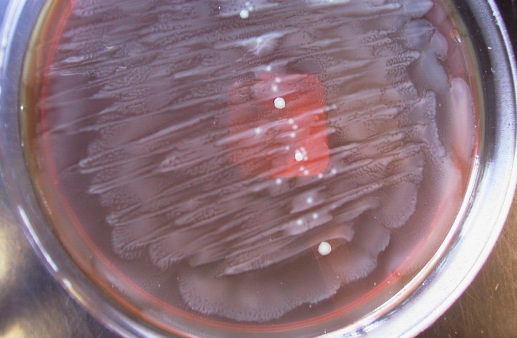
E. coli UTI Sample
1 uL loop, Each colony represents 1000 colonies/ml of urine
Day 1: >100,000/mL lactose fermenting GNR, resembling E. coli.
Day 2: >100,000/mL E. coli, susceptibilities pending
[oxidase negative, indole positive, and beta hemolysis on BAP]
![<ul><li><p>1 uL loop, Each colony represents 1000 colonies/ml of urine</p></li><li><p>Day 1: >100,000/mL lactose fermenting GNR, resembling E. coli.</p></li><li><p>Day 2: >100,000/mL E. coli, susceptibilities pending</p><ul><li><p>[oxidase negative, indole positive, and beta hemolysis on BAP]</p></li></ul></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/6edc005d-d2e8-4e43-b88b-7a30b7d4b71a.png)
GPC UTI sample
1 uL loop, Each colony represents 1000 colonies/ml of urine
Day 1:
> 100,000/mL Gram positive cocci in chains
> 30,000/mL Gram positive cocci in clusters
Day 2: >100,000/mL Enterococci spp.
[with susceptibility results e.g. VRE]
![<ul><li><p>1 uL loop, Each colony represents 1000 colonies/ml of urine</p></li><li><p>Day 1:</p><ul><li><p>> 100,000/mL Gram positive cocci in chains</p></li><li><p>> 30,000/mL Gram positive cocci in clusters</p></li></ul></li><li><p>Day 2: >100,000/mL Enterococci spp.</p><p>[with susceptibility results e.g. VRE]</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/d56636e6-ab1e-43a2-b7cf-383066cc66e6.png)
GNR UTI sample
Proteus = swarming growth, no distinguishable colony due to motility (unable to count)
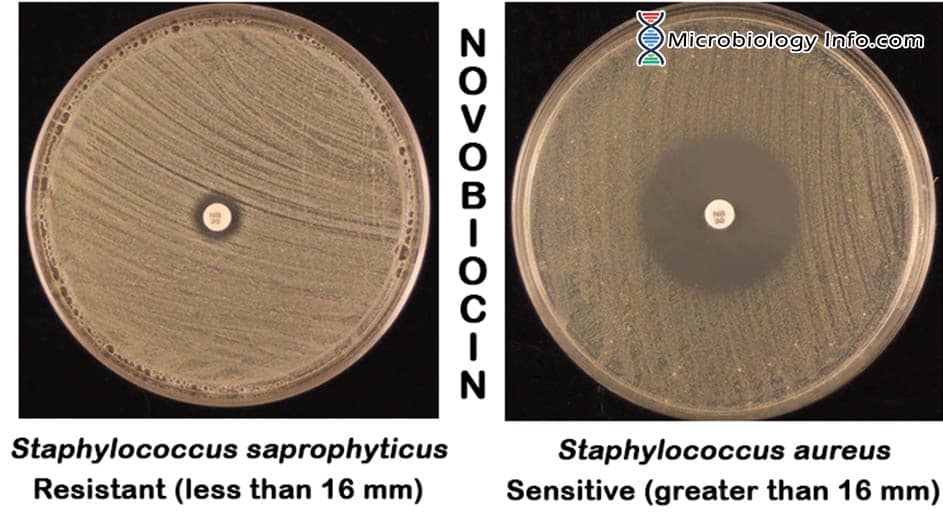
GPC UTI sample
most common in urine include Staphylococcus saprophyticus and Enterococcus faecalis.
*Note; S. saprophyticus is NB (novobiocin) RESISTANT
GPR UTI sample
typically considered contaminants like Listeria monocytogenes or Corynebacterium species.
Features and constituents of blood culture bottles
Sodium polyanethol sulfonate (SPS 0.03%), the most common anticoagulant used.
Maintain a ratio of 1:5 (blood to broth medium)
Resins or charcoal are used to absorb inhibitors.
Blood Culture Bottles
Blue Cap = Aerobic
Purple Cap = Anaerobic

Bacteremia
the presence of bacteria in the blood. Disease may or may not be present.
Septicemia
bacteria, or their toxins, are causing harm to the host. Disease is present.
Some Effects of Sepsis
Life-threatening symptoms such as hypotension, DIC, and organ failure. May indicate undiagnosed cancers linked to Clostridium septicum (leukemia, lymphoma, large bowel cancer) and Streptococcus bovis (GI tract cancer).
Sepsis Causative Agents
Coagulase-negative staphylococci
Staphylococcus aureus
Viridans streptococci and S. pneumoniae
Enterococcus spp.
Beta-hemolytic streptococci
E. coli and other members of the Enterobacteriaceae
Yeast (approximately 50% caused by Candida albicans; rarely by Malassezia
Classification of Bacteremia/Sepsis by Site of Origin
-Primary bacteremia: endovascular source such as infected cardiac valve or intravenous catheter
-Secondary bacteremia: extravascular source such as lungs in pneumonia
Classification of Bacteremia/Sepsis by causative agent
Gram-positive bacteremia caused by S. aureus, S. pneumoniae
Gram-negative bacteremia caused by P. aeruginosa, E. coli
Anaerobic bacteremia caused by Bacteroides fragilis (highly virulent, medical emergency)
Polymicrobial bacteremia caused by mixture of enterococci and Gram-negative organisms
eg. in case of bowel perforation
Classification of Bacteremia/Sepsis by Place of Acquisition
Community-acquired: S. pneumoniae bacteremia
Nosocomial: 72 hrs. after hospital admission, P. aeruginosa and enterococci bacteremia
Classification of Bacteremia/Sepsis by Duration
Transient: dental, colonoscopic, cystoscopic procedures
Intermittent: meningococcemia, gonococcemia,
pneumonia
Continuous: endovascular source like endocarditis and infected catheters
Blood Cultures Collection:
Chlorhexidine is used during surgery for skin antisepsis before collection to reduce contamination risk.
Specimen Collection and Transport
Collect 2-3 specimens per 24 hours
Specimens collection should not be closer than 3 hrs
Blood volume for specimen: Collect 20mL of blood
Specimen should be transported at room temp. within 2 hours
Bugs/milliliter of Blood
Adults: usually <30 microbes/mL
Children: could be up to 10^3/mL or more
Critical Issues in Laboratory Handling of Blood Cultures
In cases of septicemia, most blood cultures become positive by 72 hours.
Multiple bottles would be positive versus only single bottle in case of a contamination.
Isolation of same organism in blood and from a sterile site
simultaneously.
Isolation of members of Enterobacteriaceae, S. aureus, P. aeruginosa, S. Pneumoniae, H. influenzae, C. albicans always indicate an infection.
Most common contaminants are Propionobacterium acnes, diphtheroids and Staphylococcus coagulase-negative species.
For slow-growers, keep the cultures longer (up to 4 weeks)
Alternatives to Culture (Quick Screening Methods)
Urinalysis (Chemical analysis): elevated nitrate reductase and leucocyte esterase
Difference between Community Acquired vs Hospital Acquired Pathogens
Hospital Acquired pathogens also include Pseudomonas aeruginosa & Enterococci
Community Acquired UTI Pathogens
E. coli
Klebsiella pneumoniae
Other Enterobacteriaceae
Staphylococcus saprophyticus
Routes of Infection: Ascending vs Descending
ascending route (99% of infections), where pathogens travel from the lower urinary tract to the kidneys, or through the descending route (in blood), where pathogens spread from systemic circulation to the kidneys.
Common Commensals of the Urinary Tract
Corynebacterium
Lactobacillus
Staphylococcus, coagulase negative, other than Staph. saprophyticus
Streptococcus
mecA gene of Staphylococcus aureus
A gene that confers resistance to penicillin, methicillin and other beta-lactam antibiotics, making Staphylococcus aureus more difficult to treat detected through rapid test such as agglutination and assays