Osteoporosis, Rheumatoid Arthritis
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Connective tissue includes:
Bone, cartilage, tendons, ligaments, lymphatic tissue, bone marrow
Osteoarthritis
Most common form of arthritis in US
Degeneration of cartilage and the underlying bone.
Symptoms often include pain, stiffness, and swelling in the affected joints.
Areas osteoarthritis affects include:
Osteoarthritis (OA) commonly affects weight-bearing joints, such as:
• Knees
• Hips
• Spine (especially lumbar and cervical areas)
• Feet (especially big toe)
In contrast, Rheumatoid Arthritis (RA) is a systemic autoimmune disease that tends to affect smaller joints first, particularly:
• Fingers (MCP and PIP joints)
• Wrists
• Toes (MTP joints)
High risk patients for developing osteoarthritis include:
African Americans
Women
Older aged
Tip: OA is not considered normal process of aging
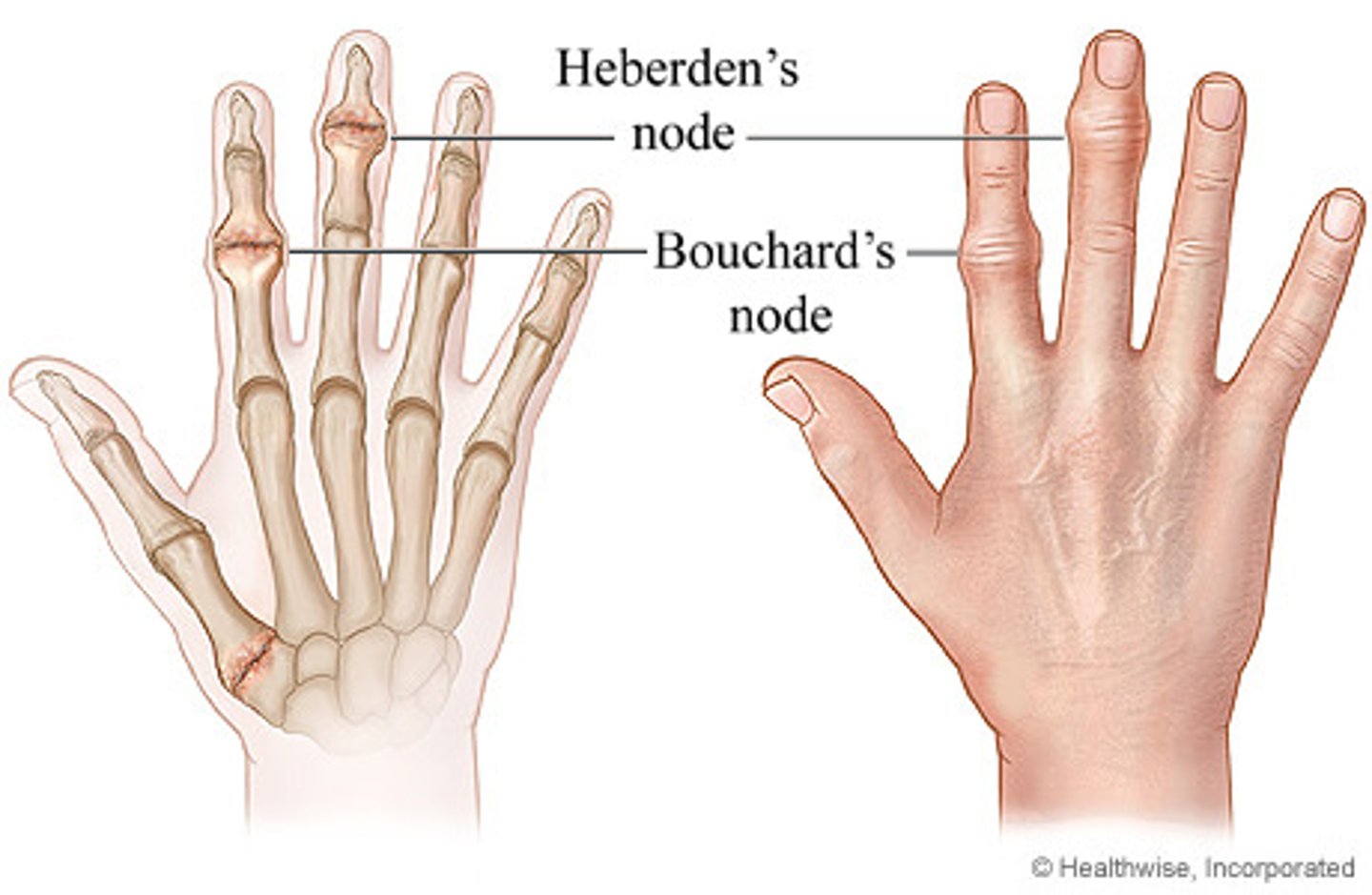
Bouchnard's Nodes
Bony swellings that develop on the proximal interphalangeal joints of the fingers, commonly associated with osteoarthritis.
Tip: think “B” as in closest to the “Body” to differentiate between Bouchnard’s node and Heberden's nodes, which occur at the distal joints.
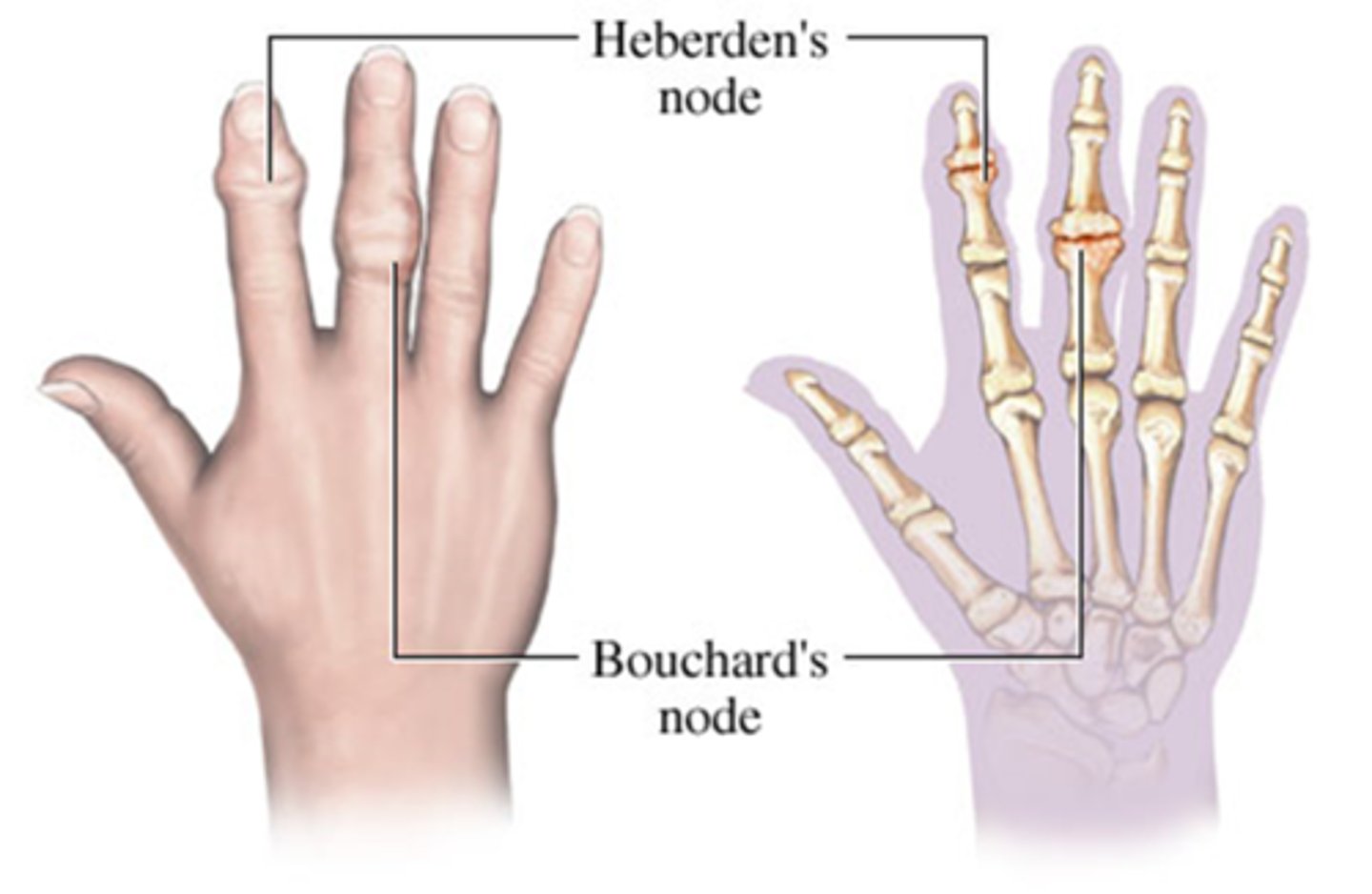
Heberden's Nodes
Osteophytes formation of fingers at the distal interphalangeal joints, commonly associated with osteoarthritis.
Osteophytes are?
Projections of new cartilage and bone growth in response to mild or severe trauma to joints
What are some of the symptoms of osteoarthritis?
Pain that worsens with activity and improves with rest
Caused by mechanical wear & tear — not inflammation
Decreased ROM, tenderness, bony swelling, tissue swelling, deformity
OA may present more asymmetrical depending on joint usage whereas RA is more symmetrically (same joints on both sides of the body)
Diagnosis of Osteoarthritis
1. lab testing- rule out RA
2. radiographs- confirm joint space narrowing, subchondral sclerosis, and presence of osteophytes
-ACR criteria for diagnosis
Treatment of osteoarthritis
*There is no cure for OA
Use pharmacological and non-pharm therapies
Goals: decrease pain, increase movement, avoid drug toxin side effects
Non-Pharmacologic therapy for OA
weight loss
aerobic exercise
physical therapy/ROM
muscle strengthening
ambulatory assistive devices
appropriate foot wear/insoles
occupational therapy
ADL help
patient education
Pharmacological Therapy for OA
1. acetaminophen (Tylenol) - do not exceed 4g daily
2. NSAIDS - inhibit inflammation and pain as well as GI protection
3. Injections of corticosteroids
**1-3 may be used together, but no more than 1 NSAID
4. Opioid analgesics- use sparingly; habit forming
How do NSAIDS work?
Non-selectively inhibit prostaglandin production
This inhibits inflammation/pain, but also prohibits GI tract protection
How do Opioid Analgesics work for OA treatment?
They bind to opioid receptors in the PNS to decrease pain perception
4 Surgical Options for OA treatment
1. Arthroscopic debridement (remove debris in joint)
2. Arthroscopic synovectomy (remove excess synovial membrane to reduce inflammation)
3. Surgical fusion- fuse together areas of joints to prohibit movement (common in spine)
4. Total Joint replacement
Which joints are affected by RA
involved joints usually distributed symmetrically (ex: bilateral wrists, ankles, or knees)
What inflammation can occur from RA, outside of joints?
lungs (pleuritis, pleural effusion)
heart (pericarditis)
kidneys
blood vessels
salivary glands
bone marrow
CNS
What are some causes of RA?
Unknown antigen triggers immune response
(triggers body to remove substance from body)
Symptoms of RA include:
Joint pain, swelling, erythema, stiffness, fatigue, rheumatoid nodules over bony prominences
*untreated RA leads to complete joint destruction
Extraarticular Manifestations of RA include:
osteopenia (low bone density)
muscle weakness
episcleritis (red inflammation of episclera)
scleritis (inflammation of sclera)
pleuritis (inflammed lung lining)
pleural effusion (excess fluid around lungs)
pericarditus (inflammed heart lining)
RA diagnosis
*may take 2 rheumatologists
combine signs, symptoms, lab values, radiographs, ultrasounds
ACR has criteria for diagnosis
Symptoms: symmetrical joint pain, morning stiffness for 30min+, synovitis (check by palpating and ultrasound), 6week long
Why are both Lab testing and symptom checking important for RA diagnosis?
Because 25-30% of those with RA test negative for antibodies!
(and those without RA may test positive)
Risk Factors for RA
female
age 20-50
genetic predisposition
Epstein-Barr virus
stress
older age
environmental factors
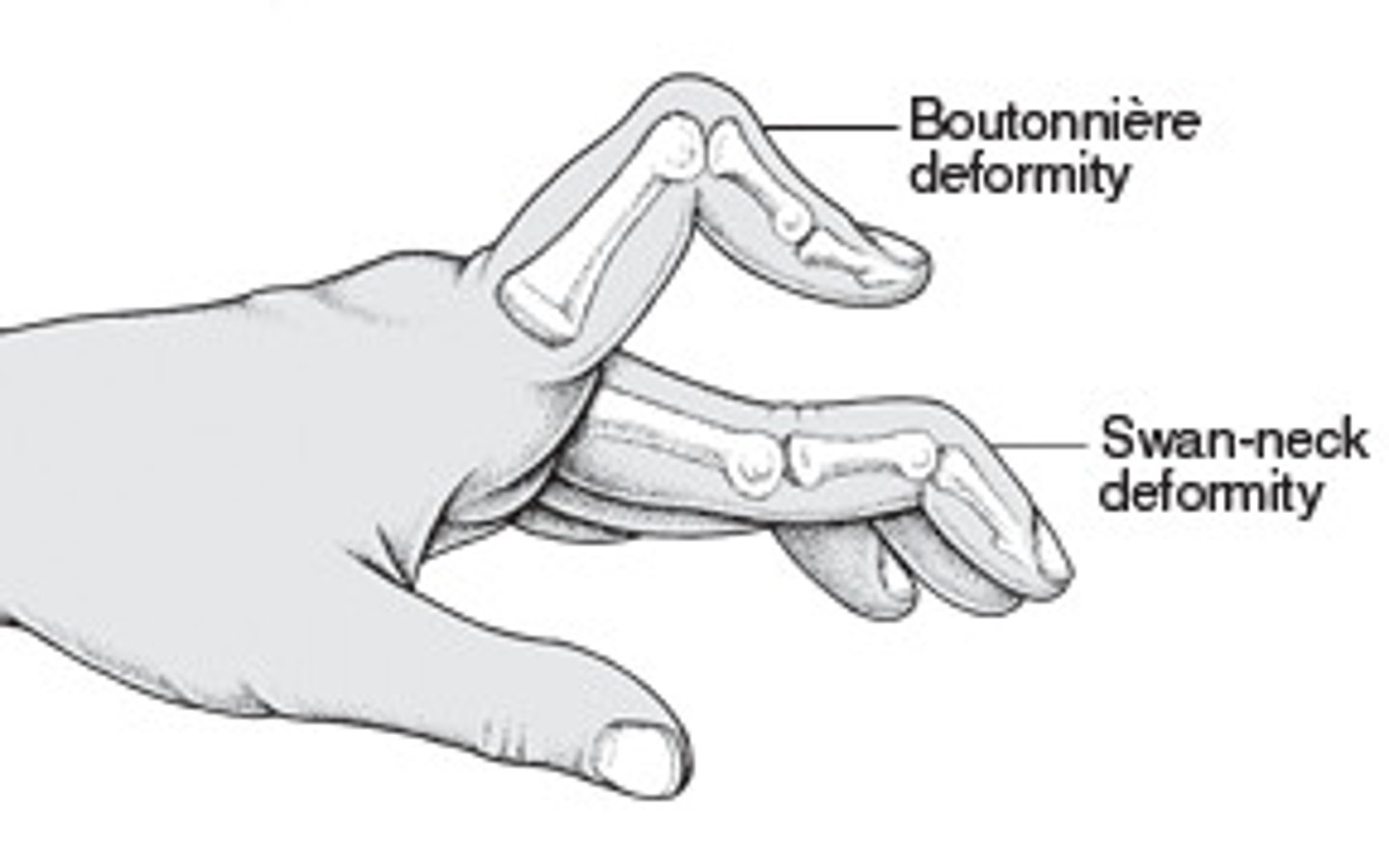
Swan neck deformity of RA
Erythrocyte Sedimentation Rate (ESR)
Speed at which erythrocytes settle out of plasma
Indicating inflammation in the body.
A higher rate can suggest the presence of inflammatory diseases such as rheumatoid arthritis.
C-Reative Protein (CRP)
Diagnostic testing; monitors the response to anti-inflammatory therapy
Antinuclear Antibody (ANA) titer blood test is used for OA or RA?
Used in the differential dx of rheumatic diseases and to detect antinucleoprotein factors and patterns associated with certain autoimmune d/o
Anti-CCP antibodies
Test to detect antibodies.
Result is positive in most people who have RA, even years before symptoms start.
Arthrocentesis is a test used for?
Diagnostic test to determine cause of pain/swelling in a joint
Synovial fluid aspiration by needle
With RA, increased WBCs and RF are present in fluid
Tip: monitor bleeding or fluid leak from needle biopsy site and give Tylenol for pain
Patient-Centered Care for RA include:
1. apply heat or cold to affected areas for
2. encourage daily physical activity
3. monitor for fatigue
4. patient education
5. provide safe environment
6. administer meds and proper positioning as prescribed
7. teach patient signs/symptoms to report (fever, infection, pain upon inspiration, pain in chest)
8. encourage foods high in vitamins, protein, and iron; eat small frequent meals
Pharmacological treatment for RA include:
1. NSAIDS
2. COX-2 Enzyme blockers (less GI distress, higher cardiac disease)
3. Corticosteroids (predinsone..not long term use)
4. DMARDS (biologic / non-biologic)
Corticosteroids and risks associated:
Strong anti-inflammatory meds, not given for long term use.
Tip: observe for Cushingoid changes, monitor weight and BP
Side-effects of too much corticoid hormone or in this case, Prednisone, can cause Cushingoid signs and symptoms to manifest such as:
System/Feature | Cushingoid Sign |
|---|---|
Face | Moon face (round, puffy face) |
Body Fat Distribution | Truncal obesity (fat on abdomen), thin limbs, Buffalo hump (fat pad on upper back/neck) |
Skin | Fragile skin, easy bruising, purple striae, Delayed wound healing |
Muscle/Bone | Muscle weakness, osteoporosis, back pain |
Mood | Irritability, mood swings, possible psychosis |
Immune System | Increased risk of infections |
Metabolic | Hyperglycemia, hypertension |
Reproductive | Irregular periods, decreased libido |
What are some nursing interventions nurses need to watch out for in a patient taking Prednisone long-term ?
🩺 Nursing Responsibilities:
• Monitor physical appearance and behavior
• Check labs: blood glucose, electrolytes (esp. sodium ↑, potassium ↓)
• Assess for infections, skin integrity, bone pain
• Teach patients about gradual tapering of steroids (never abruptly stop)
• Document all changes clearly
Plasmapheresis
Removal of plasma from withdrawn blood by centrifuge
3 Complications of RA
1. Sjogren's Syndrome
2. Secondary osteoporosis
3. Vasculitis (organ ischemia)
What autoimmune disease produces inflammatory joint symptoms throughout the body?
Rheumatoid Arthritis (RA) is a systemic autoimmune disorder that causes inflammation of the synovial lining and affects multiple joints and organs.
What chronic condition generally gets worse with age?
Osteoarthritis (OA) is a degenerative joint disease caused by wear and tear
Gets worse over time, and it's most common in older adults.
Tip: OA is NOT considered a normal part of aging process — but age does influence development.
Cartilage destruction caused by Osteoarthritis can begin between the ages of?
Cartilage destruction between ages of 20 and 30.
Symptoms — NOT cartilage destruction, more common at ages 50 to 60.
What condition presents with symptoms that occur symmetrically and includes generalized stiffness?
Rheumatoid Arthritis (RA) typically presents symmetrically (both sides of the body)
Morning stiffness that lasts over 1 hour.
Which condition can be prevented with proper diet, exercise, and joint protection?
Osteoarthritis (OA) can be delayed or prevented by reducing joint stress,
Maintaining a healthy weight, and using protective equipment.
What symptoms may occur with the onset of RA condition?
RA may cause systemic symptoms such as fever, weight loss, fatigue, and loss of appetite.
Is morning stiffness common in both RA and OA?
Yes, both conditions cause morning stiffness, but in RA it lasts longer (>60 minutes)
OA it's shorter (<30 minutes).
Tip: is asking about stiffness and not pain; there is a difference.
Osteoarthritis morning stiffness and pain differs from RA.
✅ Osteoarthritis (OA)
Morning Stiffness:
- Lasts < 30 minutes
- Improves with movement or "warming up" the joints
• Often comes after inactivity (e.g., after sitting a long time)
Pain:
- Worsens with activity or use (e.g., walking, lifting)
- Improves with rest
• Often described as an "aching" in weight-bearing joints
Which condition affects joint pain and stiffness asymmetrically, especially in weight-bearing areas?
Osteoarthritis (OA) often affects joints asymmetrically, notably in the knees or hips.
This is why you often see patients limping when walking.
Can either RA or OA be completely cured with proper therapy and medication?
Neither RA nor OA is curable.
Treatments manage symptoms and slow progression but do not eliminate the disease.
The cause of narrowing joint space in OA is caused by?
Loss of cartilage due to mechanical wear & tear.
Process: Cartilage → thins → erodes → bone-on-bone contact
Joint space narrowing happens in both OA and RA but how or why?
• OA = mechanical degeneration
• RA = inflammatory destruction
Pain caused by Osteoarthritis typically worsens with joint use, but pain relief may be disturbed depending on the stages of OA. In which stage is pain relief disturbed?
OA: Pain worsens with joint use
Early stages: rest relieves pain
Later stages: pain with rest and sleep is disturbed because of pain and increased joint discomfort
Describe changes of the cartilage caused in Osteoarthritis.
Cartilage becomes:
Dull, yellow, & granular
Soft & less elastic
Less able to resist wear w/ heavy use
How can the application of heat assist with stiffness in joints?
Application of heat can help alleviate joint stiffness in both RA and OA, improving flexibility, especially during morning routines.
What imaging studies are performed to show joint damage in RA and OA?
X-rays and MRIs are used in both RA and OA
Recognize clinical manifestations of OA.
Joint stiffness occurs AFTER periods of rest (makes sense because w/ OA, stiffness improves after warming up a bit)
OVERACTIVITY can cause mild joint effusion which can TEMPORARILY ↑ STIFFNESS