Intraoral Radiography
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
When is imaging needed/indicated?
When there is
Clinical evidence of an abnormality that cannot be fully assessed by physical exam alone
A high probability of disease that is not clinically evident
Should you take x-rays just to look for jaw disease in someone with no symptoms?
No—there’s not enough evidence to support that. X-rays should only be taken when there's a valid clinical reason
What should you do before exposing a patient to x-rays?
Know your diagnostic goals
Use patient info (age, history, exam findings)
Justify why the x-ray is needed
Radiographs should
Record the complete area(s) of interest on the image
Have the least possible amount of distortion
Have optimal density and contrast to facilitate interpretation
After taking an x-ray, what should you assess?
Whether the image meets your diagnostic goals
What do you do if the x-ray doesn't meet diagnostic objectives?
Determine which additional or retaken images are needed
What do Periapical (PA) projections show?
The entire length of the tooth and surrounding peri-radicular bone
What do Bitewing (BW) projections show?
The crowns of the teeth and the adjacent alveolar crests (bone above the teeth)
What do Occlusal projections show?
A larger area of teeth and bone than periapical projections
How many images are in a Full-Mouth Radiographic Series (FMX)?
18-20 images, including:
4 Bitewings (2 per side)
14-16 Periapicals (8 posterior, 4 per side; 6-8 anterior, 3-4 per side)
What is the role of the x-ray source?
It produces the x-rays for imaging
What is the difference between a wall/ceiling mounted and a hand-held x-ray machine?
Wall/Ceiling Mounted: Operator stays outside the room.
Hand-held: Operator is in the room holding the device.
What is a Position Indicating Device (PID)?
It’s a part of the x-ray machine that directs the x-ray beam and is usually shaped like a cone or aiming cylinder
What does the receptor do in radiography?
It detects and records x-rays. Only one side is active, and it needs to face the x-ray source
What are the two types of digital receptors?
Direct (solid-state sensor that captures the image immediately)
Indirect (Photostimulable Phosphor Plates, PSP, that are scanned for the image).
What are the sizes of receptors and their uses?
0: Pediatric
1: small mouth, narrow arch, anterior teeth
2: most commonly used, posterior teeth
4: occlusal (wide view)
What does a periapical projection show?
The entire length of the tooth and surrounding peri-radicular bone, including at least 2mm of bone
What are the two techniques for taking periapical images?
Paralleling (preferred, less distortion)
Bisecting Angle (used when paralleling is difficult)
Why is paralleling the preferred technique for periapical projections?
It results in less distortion, though anatomical constraints may require modifications
What are some other names for the paralleling technique?
Right-angle technique
Long-cone technique
Extension cone technique
What does the paralleling technique show?
It shows teeth and bone in their true anatomic relationship
How do you position the receptor in the paralleling technique?
Position the receptor parallel to the long axis of the teeth, and direct the x-ray perpendicular to both the tooth and the receptor
What tools are used in the paralleling technique?
Receptor holding instrument to keep the receptor in place.
Guide ring to help with cone alignment.
Where do you position the receptor in the maxillary arch when using the paralleling technique?
Place the receptor toward the center or height of the palatal vault
How do you position the receptor in the mandibular arch using the paralleling technique?
Place the receptor deep in the lingual vestibule and push the tongue toward the midline to make space
Why do digital sensors need more space in the paralleling technique?
Digital sensors are rigid and thick, which makes them require more space for proper placement
What anatomical constraints can make parallel receptor placement difficult?
Shallow palate or vestibule
Tori (bony growths in the mouth)
These can prevent parallel placement and cause distortion.
Why is the object-receptor distance increased in the paralleling technique?
The paralleling technique requires more distance between the object (teeth) and the receptor for proper placement
What is the purpose of using a long cone PID in the paralleling technique?
A long cone PID is used to increase the source-object distance and compensate for the increased object-receptor distance
What is the typical distance from the source to the edge of the cone in the paralleling technique?
The distance ranges from 8 to 16 inches, with 12 to 16 inches considered long
How does increasing the source-object distance help in the paralleling technique?
It reduces beam divergence, reduces magnification, and ensures that the complete anatomy is captured
When is the bisecting angle technique useful?
When paralleling can't be applied due to anatomical constraints or rigid digital sensors
What is Cieszynski’s rule of isometry?
two triangles are equal if they share one complete side and have two equal angles
How is the receptor positioned in the bisecting angle technique?
As close as possible to the lingual surfaces of the teeth
How do you bisect the angle in the bisecting angle technique?
Mentally bisect the angle between the long axis of the teeth and the long axis of the receptor
What happens to the tooth length in the bisecting angle technique?
The actual length of the tooth is equal to the length of the tooth on the image, except for multirooted teeth
What causes distortion in the alveolar ridge in the bisecting angle technique?
The alveolar ridge often projects coronally (toward the crown) to its true position, leading to distortion in the apparent alveolar bone height around the teeth
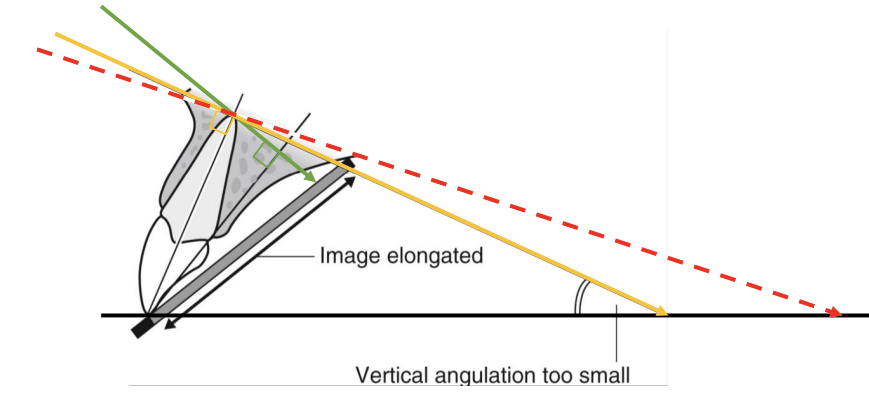
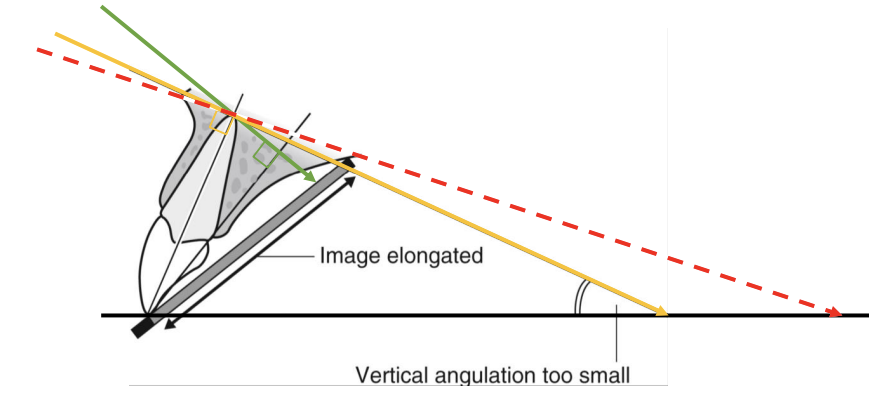
What is vertical angulation?
The angle between the x-ray beam and a line parallel to the floor or occlusal plane
What is positive angulation?
Positive angulation occurs when the cone points downward
What is negative angulation?
Negative angulation occurs when the cone points upward
How does vertical angulation affect radiographic images?
Vertical angulation significantly influences dimensional accuracy and can cause shape distortion
What happens with under-angulation (vertical angle too small)?
Elongation occurs, causing the teeth to appear longer than their true size
What happens with over-angulation (vertical angle too large)?
Foreshortening occurs, causing the teeth to appear shorter than their true size
What are the advantages of the paralleling technique?
Geometrically accurate images with little magnification (with long cone).
Reproducible results.
Periodontal bone levels well represented.
Positioning devices guide horizontal and vertical angulation.
What are the disadvantages of the paralleling technique?
Receptor positioning can be uncomfortable (gagging risk).
Positioning holders can be difficult for inexperienced operators, especially with digital sensors.
Anatomy (shallow palate) may make it difficult or impossible to use.
What are the advantages of the bisecting angle technique?
Receptor positioning is fairly comfortable.
Relatively simple and quick.
Adequate for most diagnostic purposes if angles are assessed correctly.
What are the disadvantages of the bisecting angle technique?
Geometrically inaccurate images (foreshortening or elongation).
Requires considerable skill.
Not reproducible.
Poor representation of periodontal bone levels.
Zygomatic process may overlap upper molar roots.
What do bitewing radiographs show?
Only the crowns of teeth and adjacent alveolar crests.
Roughly equal distribution of maxillary and mandibular crowns/bone
What are the diagnostic objectives of bitewing radiographs?
Detect early interproximal caries before it becomes clinically apparent.
Detect secondary caries beneath restorations.
Assess loss of interdental and furcation bone
Why are bitewing projections preferred for periodontal bone level evaluation?
Bitewing projections produce more reliable images for evaluating periodontal bone levels than periapical (PA) images
How is the receptor placed during radiographic examination?
The receptor is placed parallel to the lingual/buccal surfaces of the teeth being examined.
It may be oriented horizontally or vertically
What is the vertical beam angle used for radiographic examinations?
The vertical beam angle is parallel to the occlusal plane and perpendicular to the receptor.
0 to 10° vertical angulation compensates for the Curve of Wilson
What is the purpose of the horizontal beam angle in radiographic imaging?
The horizontal beam angle is directed through the interproximal spaces to open contacts between teeth, allowing better visualization of the spaces between them
What is the purpose of the horizontal beam angle in radiographic imaging?
The horizontal beam angle is directed through the interproximal spaces to open contacts between teeth, allowing better visualization of the spaces between them
When are vertical bitewings indicated?
Vertical bitewings are indicated when the patient has moderate to severe alveolar bone loss
What is the benefit of using vertical receptor orientation in bitewing radiographs?
Vertical receptor orientation increases the likelihood of capturing alveolar crests, which is helpful for assessing bone loss
What does a Full-Mouth Radiographic Series (FMX) aim to display?
Crowns and roots of all teeth, periapical areas, interproximal areas, and alveolar bone, including edentulous areas
How many images typically make up a Full-Mouth Radiographic Series (FMX)?
Typically 18-20 images:
4 bitewings (2 per side)
14-16 periapical (PA) images (8 posterior, 6-8 anterior)
If a size 1 sensor is used in a Full-Mouth Radiographic Series, what may need to happen?
More images may be required to capture all the teeth, especially for anterior PAs or vertical bitewings
What are the three general requirements for all radiographic projections?
Record complete area(s) of interest
Have the least possible amount of distortion
Show optimal density and contrast
What is the primary objective of a periapical (PA) projection?
To capture the full length of the tooth root and 2–3 mm of periapical bone
What additional details should a periapical projection capture besides the root and periapical bone?
The entire crown of the tooth
Open interproximal contacts, especially in anterior teet
What are the two main goals of bitewing projections?
Open all interproximal contacts
Capture interproximal bone levels in both maxilla and mandible
What do occlusal projections show that periapical images do not?
A larger area of teeth and surrounding bone
Why are occlusal projections sometimes replaced by CBCT?
CBCT provides 3D scans with more detailed imaging
When might occlusal radiographs still be used instead of CBCT?
When CBCT is not accessible
When lower cost or reduced radiation dose is desired
What size is the occlusal receptor, and in what forms is it available?
3 × 2.3 inches; available as film or PSP, but not direct digital
Where is the occlusal receptor placed in the mouth?
Between the occlusal surfaces of upper and lower teeth, in the occlusal plane
Which side of the occlusal receptor should face the jaw being examined?
The active (tube) side
How is the x-ray beam directed in occlusal radiography?
Through the jaw to the receptor, at a steep vertical angulation
Name the types of standardized occlusal projections for both jaws
Maxillary: Anterior, Topographic, Lateral
Mandibular: Anterior, Topographic, Lateral