From Skull Drill to Free Will - Test 3 - FACT SHEETS
1/62
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
What is a ‘phobia’?
An intense, irrational fear of something — even if it’s not actually dangerous.
It’s a mental and emotional reaction, often triggered just by seeing or thinking about the feared object or situation.
Common triggers: crowds, being alone, animals, elements (ex: water or fire), etc.
What are the symptoms of a phobia?
Emotional: Panic, feeling overwhelmed
Physical: Rapid heartbeat, sweating, chest tightness, shortness of breath, dry mouth
Behavioural: Avoiding people, places or activities
What are the general treatments for phobia?
Deep breathing
Meditation
Yoga
Therapy or counselling
What are the three main types of phobia?
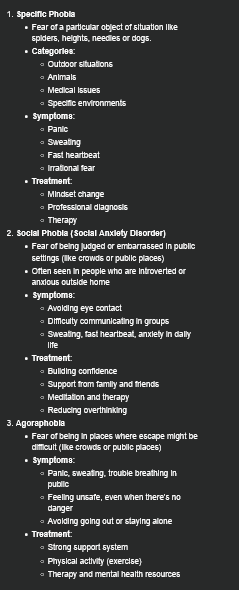
Specific Phobia
Fear of a particular object of situation like spiders, heights, needles or dogs.
Categories:
Outdoor situations
Animals
Medical issues
Specific environments
Symptoms:
Panic
Sweating
Fast heartbeat
Irrational fear
Treatment:
Mindset change
Professional diagnosis
Therapy
Social Phobia (Social Anxiety Disorder)
Fear of being judged or embarrassed in public settings (like crowds or public places)
Often seen in people who are introverted or anxious outside home
Symptoms:
Avoiding eye contact
Difficulty communicating in groups
Sweating, fast heartbeat, anxiety in daily life
Treatment:
Building confidence
Support from family and friends
Meditation and therapy
Reducing overthinking
Agoraphobia
Fear of being in places where escape might be difficult (like crowds or public places)
Symptoms:
Panic, sweating, trouble breathing in public
Feeling unsafe, even when there’s no danger
Avoiding going out or staying alone
Treatment:
Strong support system
Physical activity (exercise)
Therapy and mental health resources
What is ‘Dissociative Identity Disorder (DID)’?
A mental health condition where an individual has two or more distinct identities or personality states.
Affects about 0.1% - 2% of the population.
Often linked to severe childhood trauma (ex: abuse or neglect).
Dissociation serves as a coping mechanism to manage overwhelming experiences.
What are some symptoms of DID?
Identity fragmentation: Two or more distinct identities with unique behaviours and memories.
Memory gaps: Inability to recall personal information or events.
Switching: Sudden shifts between identities, often triggered by stress.
When diagnosing DID, other conditions like substance use or medical disorders must be ruled out.
What are some methods of treatment for DID?
Psychotherapy: Long-term therapy focused on integrating identities and processing trauma.
Medication: Used for co-occurring conditions like depression or anxiety.
Supportive Care: Safety plans and therapeutic alliances are crucial.
True or False: DID is often underdiagnosed due to stigma and lack of awareness.
True.
True or False: Alters can range from 2 - 15 over time.
True.
True or False: DID significantly impacts relationships, work, and self-care due to identity disruptions and memory lapses.
True.
What is ‘anxiety disorder’?
Anxiety is a natural response to stress or danger.
It becomes a disorder when it’s persistent, overwhelming, and interferes with daily life.
According to the DSM-5, anxiety disorders are marked by excessive fear and behavioural changes.
What are some common types of anxiety disorders?
Generalized Anxiety Disorder (GAD)
Ongoing worry about everyday issues.
Panic Disorders
Repeated panic attacks with symptoms like chest pain and dizziness.
Social Anxiety Disorder
Fear of being judged in social settings.
Phobias:
Intense fear of specific things (ex: heights, spiders).
Separation Anxiety
Fear of being away from loved ones.
Agoraphobia
Fear of places where escape may be difficult.
What are some causes and risk factors of anxiety disorders?
Genetics
Family history of anxiety
Brain Chemistry
Imbalances in serotonin, dopamine
Personality Traits
Negativity, perfectionism
Trauma
Abuse or distressing experiences.
What are some symptoms of anxiety disorders?
Emotional: Excessive worry, fear, irritability.
Physical: Fatigue, headaches, chest pains, trouble sleeping.
What are some methods of treatment for anxiety disorders?
Therapies
CBT, exposure therapy, mindfulness.
Medications
Antidepressants, anti-anxiety meds
Lifestyle Changes
Regular exercise, sleep and reduced caffeine.
What is ‘Complex Post-Traumatic Stress Disorder (CPTSD)’?
Complex PTSD results from per longed or repeated exposure to traumatic events often from interpersonal harm (E.g., abuse, neglect) most commonly occurring during childhood.
C-PTSD is deeply rooted in developmental trauma, where a child lacks safety, attunement, or protection during critical brain development.
Trauma is not just an event - it's a lasting wound in the nervous system.
What are the differences between PTSD and Complex PTSD?
PTSD:
Caused by singular traumatic events (ex: assault)
Flashbacks, nightmares, hypervigilance
Often adult onset
CPTSD:
Results from prolongued traumatic events (ex: childhood abuse)
All PTSD symptoms plus emotional dysregulatuion, negative self-concept and relational difficulties
Often begins in childhood
What is ‘Mass Hysteria’?
The spontaneous outbreak of atypical thoughts, feelings, or actions in a group or social aggregate. Manifestations may include psychogenic illness, collective hallucinations, and bizarre actions (American Psychological Association, 2018).
What are the two subtypes of mass hysteria?
Mass Psychogenic Illness: The collective fear of an occurrence, be it natural or supernatural.
Mass Sociogenic Illness: A collective experience of psychosomatic symptoms, such as symptoms of a gas leak with no actual threat or reasonable cause, or inexplicable twitching.
What are the two subtypes of mass hysteria symptoms?
Mass Anxiety Hysteria: Typically includes symptoms like chest pain, headaches dizziness, fainting.
Mass Motor Hysteria: Typically includes symptoms like twitching, unstoppable laughing/crying. partial paralysis, trance-like states and altered speech patterns.
What are some supposed triggers of mass hysteria?
Psychosocial environment
Supernatural/religious beliefs
Mass vaccinations
Air pollution
Food poisoning
What populations are most likely to fall for mass hysteria?
Children and adolescents
What were the Salem Witch Trials?
One of the most well-known outbreaks of mass hysteria
Salem, Massachusetts in 1962.
200 members of the community, mostly women and children, were accused of practicing witchcraft.
19-25 people may have lost their lives due to this hysteria.
True or False: There is no known cure for Mass Hysteria.
True.
It will typically calm down throughout time or when the patients are removed from the source (in cases of gas and ergot poisoning.)
What is ‘Trichotillomania (TTM)’?
A a mental health disorder where people feel strong urges to pull out their hair.
Hair pulling may happen on the scalp, eyebrows, or other body areas.
It is classified as an OCD-related disorder in the DSM-5.
The word comes from Greek:
Tricho/Thrix = hair
Tillo/Tillein = to pull
Mania = excessive behavior; madness or obsession
TTM affects mental well-being, confidence, and daily life.
What is the history of Trichotillomania?
The term 'Trichotillomania' was coined in 1889 by French dermatologist François Henri Hallopeau.
Hallopeau used it for a patient who pulled his hair in tufts.
Earlier, philosopher Epictetus mentioned hair-pulling in 101 AD during emotional stress.
The disorder was officially recognized by the American Psychiatric Association in 1987.
What are some symptoms of Trichotillomania?
Repeated hair pulling that leads to hair loss or bald patches.
Strong urges before pulling, followed by relief.
Pulling may be done knowingly (focused or without awareness (automatic).
People often feel shame and may avoid social activities.
Some people may eat pulled hair (Trichophagia), which can block digestion. In serious cases, hair blocks may need surgery to remove.
Emotional effects: Shame, anxiety, depression.
Physical effects: Bald spots, skin damage, scarring.
What are some causes of Trichotillomania?
TTM does not have one clear cause.
It usually comes from a mix of:
Genetics
Brain chemistry (like serotonin or dopamine imbalance)
Stress or trauma (emotional coping)
It may begin during times of emotional pressure or stress.
What are some risk factors of Trichotillomania?
Most cases begin between the ages of 10-13.
More common among females, especially in adulthood.
Risk increases with family history of OCD, anxiety, or depression.
Triggers include stress, boredom, and social isolation.
About 1 in 20 people have a Body-Focused Repetitive Behavior (BFRB).
What are some treatments for Trichotillomania?
Therapies that help:
Habit Reversal Training (HRT)
Cognitive Behavioral Therapy (CBT)
Acceptance & Commitment Therapy (ACT)
Medications that may help:
Clomipramine
N-acetylcysteine (NAC)
Olanzapine
What TEDx Talk was featured during the presentation on Trichotillomania?
'You can't change what you don't know is happening’ by Aneela Idnani.
Aneela Idnani is a mental health speaker and co-founder of HabitAware.
She shared her own experience and emphasized the importance of awareness.
She also developed wearable tools to help people monitor pulling behavior.
What is ‘Alzheimer’s’?
Alzheimer's is a type of dementia, a general term for memory loss and cognitive decline.
It affects memory, thinking, and behavior, and can interfere with daily activities.
Alzheimer's is the most common form of dementia, making up 60-80% of all cases.
What causes Alzheimer’s?
Caused by abnormal protein buildup in the brain (including beta-amyloid and tau).
These proteins kill neurons, leading to permanent brain damage.
Damage starts in specific brain regions and spreads gradually.
Who does Alzheimer’s affect?
Primarily affects older adults, especially 65 years and older.
As you age, your risk of developing Alzheimer's increases.
How does Alzheimer’s progress?
Early stage: Mild memory loss.
Late stage: Loss of ability to converse or respond to surroundings.
Life expectancy after diagnosis: typically, 4-8 years, but can be as long as 20 years.
What are some symptoms of Alzheimer’s?
Early signs:
Difficulty remembering recent events.
Confusion or disorientation.
More severe symptoms:
Suspicion of loved ones.
Difficulty speaking, walking, or swallowing.
May not recognize these issues in yourself due to anosognosia.
What are some treatments for Alzheimer’s?
There is no cure for Alzheimer's.
Medications can help manage symptoms, but they do not stop disease progression.
Common treatments:
Cholinesterase inhibitors
Memantine (Namenda)
What is ‘Huntington's Disease (HD)’?
“Huntington's disease causes nerve cells in the brain to decay over time. The disease affects a person's movements, thinking ability and mental health.” (Mayo Clinic)
A rare, inherited neurodegenerative disorder that progressively impairs movement, cognition, and mood.
Huntington's Disease was first described in 1872 by Dr. George Huntington, who observed its hereditary pattern and progressive nature.
It affects approximately 400,000 people worldwide, with a prevalence of 4 to 5 cases per 100,000 in Western populations.
In the United States, about 30,000 individuals are symptomatic, and an estimated 200,000 are at risk of developing the disease.
What causes Huntington's Disease?
Huntington's Disease is caused by an expansion of CAG repeats in the **HTT** gene.
Normal genes contain 10 to 35 repeats, while individuals with HD have 36 or more repeats.
This mutation leads to the production of a toxic huntingtin protein that damages neurons, particularly in areas of the brain responsible for movement and thought.
The disease follows an autosomal dominant inheritance pattern, meaning there is a 50% chance that an affected parent will pass the mutation to their child.
What are some symptoms of Huntington's Disease?
Symptoms typically begin between ages 30 and 50 and may initially include subtle motor issues, mood changes, and cognitive decline.
As the disease progresses, individuals may experience chorea (involuntary movements), memory loss, and psychiatric symptoms such as depression.
Juvenile Huntington's Disease, which occurs before age 20, is rarer but tends to be more severe.
How is Huntington's Disease diagnosed?
Diagnosis of Huntington's Disease involves a combination of genetic testing (CAG repeat count), neurological examinations, and brain imaging, such as MRI scans that may show striatal atrophy.
Early diagnosis can be challenging due to the overlap of symptoms with other disorders.
How is Huntington's Disease treated?
Currently, there is no cure for Huntington's Disease.
Management typically includes medications like tetrabenazine for chorea and antidepressants for mood stabilization.
Additional therapies, including physical, occupational, and speech therapy, help maintain function.
Experimental treatments, such as AMT-130 (gene therapy) and PTC518 (a protein-lowering drug), are currently undergoing trials.
The lifetime care costs for a Huntington's Disease patient average about $20 million. Families often face emotional strain, caregiving challenges, and ethical dilemmas related to genetic testing and end-of-life care.
Research efforts are focusing on gene-editing techniques (such as CRISPR), RNA interference, and stem cell therapies. The partnership between Novartis and PTC518 aims to advance the development of treatments to reduce the buildup of toxic proteins.
What is ‘Obsessive Compulsive Personality Disorder (OCPD)’?
A personality disorder that “involves an extensive preoccupation with perfectionism, organization and control. People with OCPD have rigid beliefs and need to have control of themselves, others and situations.” (Cleveland Clinic)
Is ego-syntonic:
“Compatible with the ego or conscious self-concept. Thoughts, wishes, impulses, and behavior are said to be ego-syntonic when they form no threat to the ego and can be acted upon without interference from the superego.”
(APA Dictionary of Psychology)
Can impede daily functioning
Develops in late adolescence and early adulthood
Can lead to social isolation
Control is used as a coping mechanism in order to feel safe
“High achievers” can have their perfectionism get in the way
Less likely to ask for help since they don’t see a problem in their behaviour
Overly conscientious of ethics, values and morality
What are some causes of OCPD?
Childhood experience
Genetics
Environmental factors
What are some treatments of OCPD?
Medication
Cognitive Behavioural Therapy (CBT)
Relaxation training
True or False: Indigenous people are less likely to receive professional help for mental health (and to some extent mental illness) than non- Indigenous people.
True.
True or False: Young Indigenous women are more likely to have a problem with chronic health conditions and have adverse, mental health and mental illness then Indigenous men.
True.
True or False: There have been mental health disparities among Indigenous people being reported, from contemporary factors like facing barriers to accessible services to mental health services and temporary factors such as assimilationist and colonial policies
True.
True or False: Indigenous people are more likely to experience very serious psychological distress 2.5 more than non- Indigenous people
True.
True or False: Nearly 45% or roughly half of the Indigenous population (mainly Indigenous adults) have reported receiving a mental health diagnosis
True.
What is ‘Pica’?
A compulsive eating disorder in which people eat non-food items.
What populations are affected by Pica?
Affects both children and adults.
Is more common in children.
Pica in pregnant women ranges anywhere from 0%% to 68% based on various studies.
Pica is present in up to 50% of children ages 18 - 36 months.
True or False: The term ‘pica’ comes from a bird species.
True.
‘Pica Pica’ is the Latin name for the Eurasian Magpie, which has a reputation for eating weird things.
What are some symptoms of Pica?
Anemia
Constipation
Electrolyte imbalance
Lead poisoning
Small and large intestine obstruction
Pica can be extremely dangerous based on the non-food ingested.
What are some causes of Pica?
Culture
Stress and anxiety
Nutritional deficiencies
Medical conditions
Typically a manifestation of an underlying medical condition, like iron deficiency anemia in adults.
Is commonly an isolated disorder, but can be comorbid with schizophrenia, OCD and trichotillomania.
Pica in people with Autism Spectrum Disorder (ASD) may use it to seek sensory input or alleviate pain and discomfort.
How does Pica get diagnosed?
There are 4 criteria a patient needs to meet in order to obtain a diagnosis:
Time
Mental development
No social or cultural factors
No medical or mental health conditions
Patients must consume non-food items for at least one month in order to qualify for a diagnosis.
There are no tests that can determine Pica, but tests that can determine the harm caused by the non-food ingested (ex: toxicity).
Blood tests
Urine tests
Stool tests
Imaging (x rays, CT scans, MRIs and ultrasounds)
How is Pica treated?
There is no cure- even in less-severe cases- but it can be treated. It cannot, however, be prevented.
People can manage their symptoms by:
Speaking with a doctor or other healthcare providers
Therapy
Mild Aversive Therapy
Behavioural Therapy
Differential Reinforcement
Refraining from keeping Pica items accessivle
Seeking medical help at the first sign of complications.
What is ‘Borderline Personality Disorder’, ‘Borderline’ or ‘BPD’?
“A mental health condition that affects the way people feel about themselves and others, making it hard to function in everyday life. It includes a pattern of unstable, intense relationships, as well as impulsiveness and an unhealthy way of seeing themselves. Impulsiveness involves having extreme emotions and acting or doing things without thinking about them first.” (Mayo Clinic)
Cluster B personality disorders are identified by their inappropriate, volatile emotionality and their unpredictable behaviour.
Identifiable by its extreme fears of abandonment, unhealthy attachment styles and extreme mood swings.
It's chronic but with appropriate treatment it is manageable and can be 'cured’
What is the history of BPD?
1938: Adolf Stern couldn't place patients in one group, but they shared symptoms of psychosis and neurosis.
1967: Otto Kernberg- similar to Stern- suggested that this group of patients be referred to as the 'border line' group since they were in between psychosis and neurosis.
1975: John Gunderson wrote a research paper about BPD; was then given the nickname 'Father of Borderline Personality Disorder'.
1980: Borderline Personality was added to the third edition of the DSM.
1993: Martha Linehan created the first borderline-specific treatment known as Dialectical Behaviour Therapy (DBT).
2008: In the United States, May was officially the month of Borderline Personality Disorder Awareness.
What are some causes of BPD?
Can inherit genes from parents
Certain parts of the brain are smaller or reported inactivity:
Amygdala
Hippocampus
Orbitofrontal cortex
Being a victim of physical, emotional or sexual abuse,
Being exposed to fear or distress for a long period of time,
Being neglected by one or both parents,
Growing up with a serious mental illness in the house such as bipolar or living with heavy drug or alcohol use
What are some symptoms of BPD?
Perceived or real fears of abandonment.
Intense mood swings, or brief periods of severe depression or anxiety,
Impulsivity.
Unstable or changing relationships
Self-injury, suicidal ideation, or suicidal behaviour.
Chronic feelings of emptiness.
Inappropriate, intense anger or rage
Unstable self-image.
Stress-related paranoia or serious dissociative symptoms.
What are the four types of BPD?
Discouraged: Suffer with the symptoms, but more internalized. Very codependent and in need of reassurance.
Impulsive: Very energetic and charismatic, but they do exhibit aggressive, binging, and risky behaviours.
Petulant: Can be very manipulative and controlling; typically have a bunch of unstable relationships due to need for control and power.
Self-Destructive: This focuses on self-hatred and is distinguished by their high energy and lack of sleep.
How do you treat BPD?
Medications
Professionals prescribe:
Antipsychotics.
• Mood stabilizers/anticonvulsants
• Anti-anxiety.
Therapies
Cognitive behavioural therapy
Dialectical behaviour therapy-
The best option; it was specifically designed to treat BPD.
Schema-focused therapy.
Mentalization-based treatment,
Systems training for emotional predictability and problem-solving
Transference-focused psychotherapy.