Final Exam
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
What is an endocrine gland, and what is a hormone?
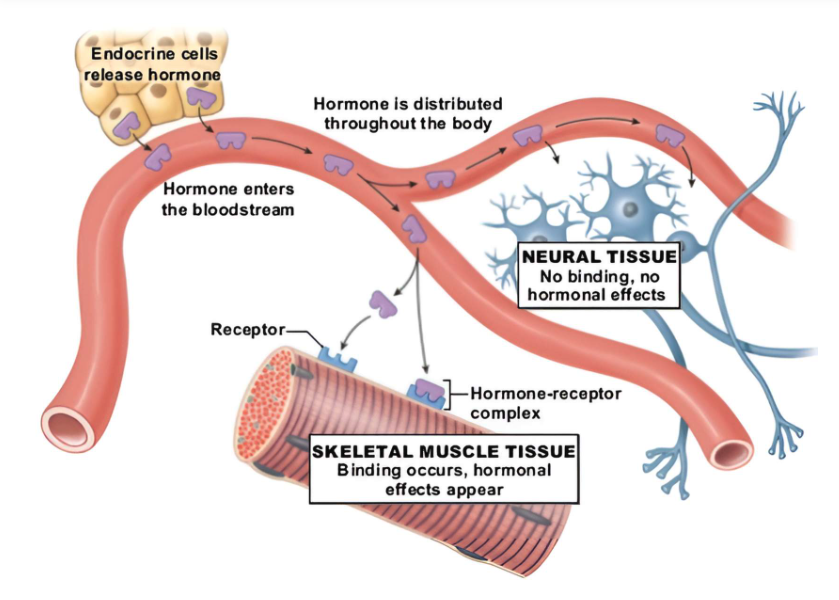
An endocrine gland is a group of specialized cells that synthesize, store, and release a very special chemical into the blood. This chemical is called a hormone. The hormone is released into the bloodstream and circulates throughout the body to specific target cells that have receptors for the hormone. The hormone will then have its effect on the target cell and can either stimulate or inhibit the activity of the cell. We can see this in the image below where endocrine cell release hormones in the blood stream, but they bypass neuronal tissue because the neurons do not have the right receptor to bind the hormones. Alternatively, the skeletal muscle tissue does express the right receptor and the hormone is able to bind to that tissue.
What are the characteristic functions of hormones?
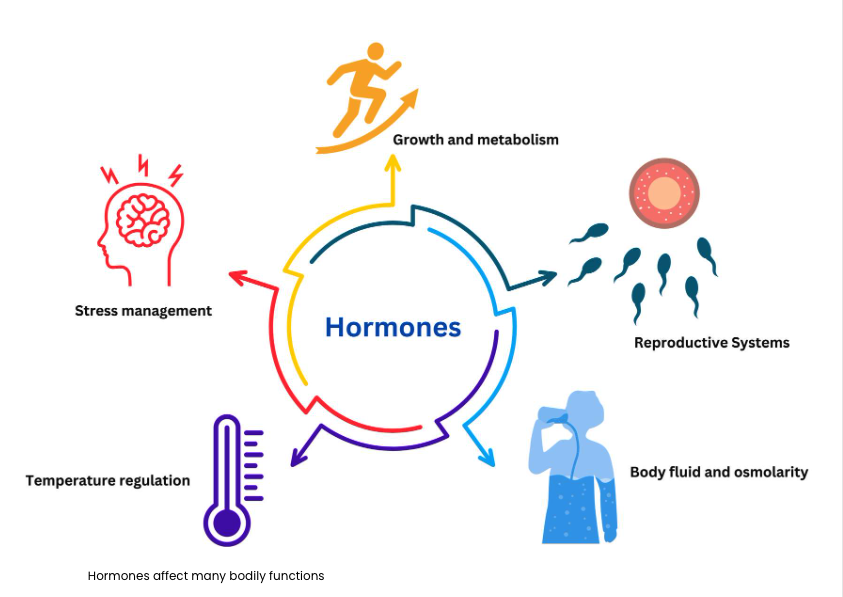
The function of the endocrine system include the maintenance of the internal environment - body temperature, body fluids volume, osmolarity, and adaptations to stress, control of growth and metabolism, and also the control of the reproductive system.
In contrast to the nervous system, the actions of the endocrine system are slower to take effect yet last longer and are generally more widespread throughout the body. While the nervous system has control over the organs with which it is in direct contact, the endocrine system can indirectly affect many organs of the body at a distance by secreting chemicals into the blood.
How are hormones secreted, how do they exert their effects, and how are they inactivated?
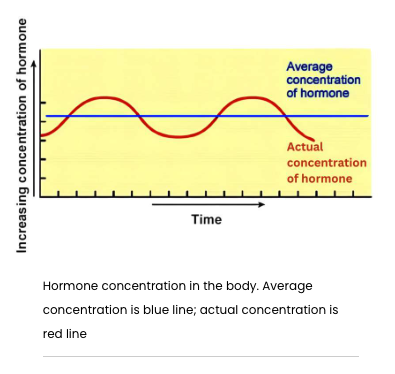
Hormones are secreted into the blood in 'pulses' by a very specific stimulus (neural or blood-borne) and in amounts that vary with the strength of the stimulus. Once secreted by the gland, hormones are present in very small concentration in the blood. They exert their specific effect by binding to receptors on or in target cells and generally act by regulating preexisting reactions. The image to the left shows how hormone concentrations gently rise and fall, but stay within a average range, which is required for their effectiveness. As hormones are used, they eventually are eliminated from the body, mainly by being metabolized in the liver or kidney and excreted through feces or urine.
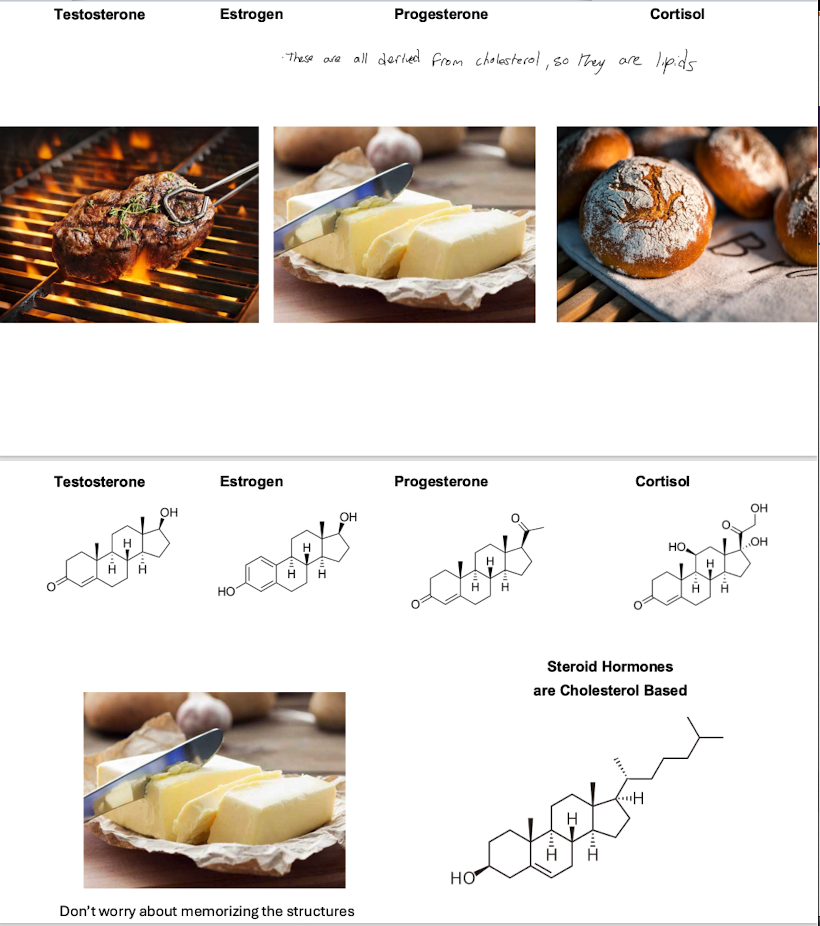
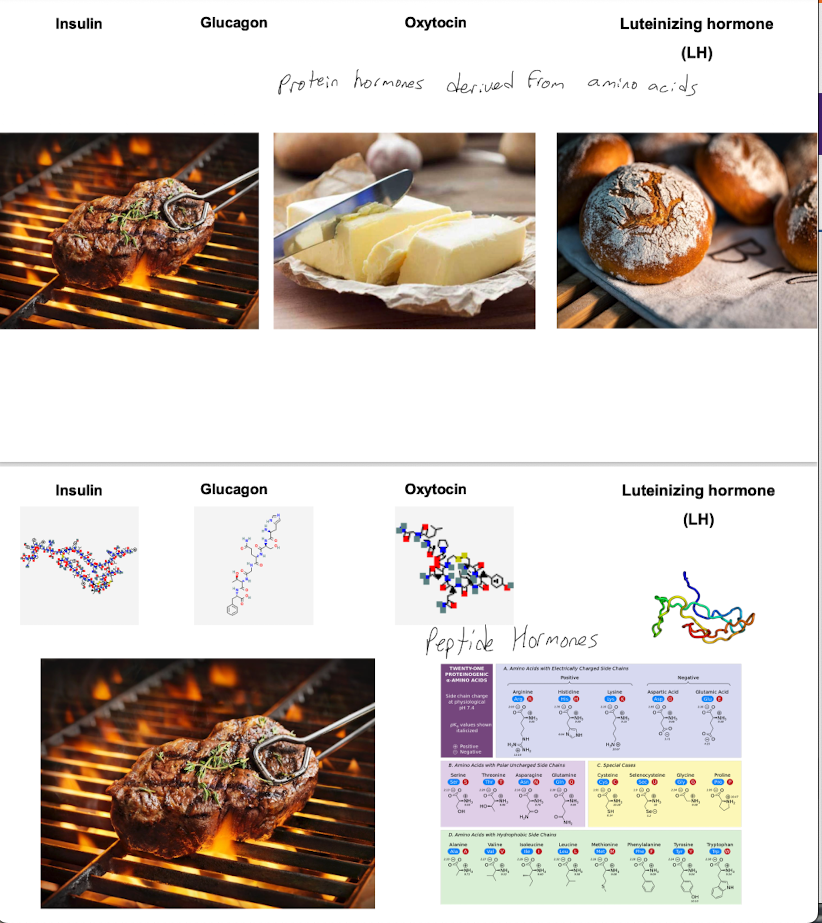
What are the steroid hormones
What are the peptide hormones
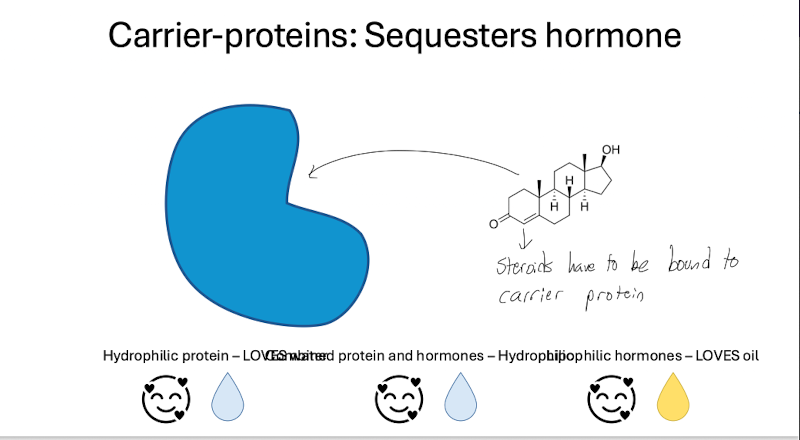
What are carrier proteins and what are the ways hormones work on the cell
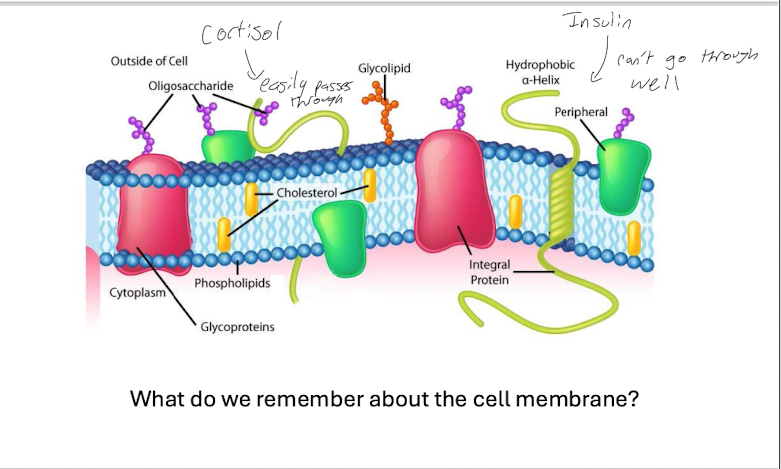
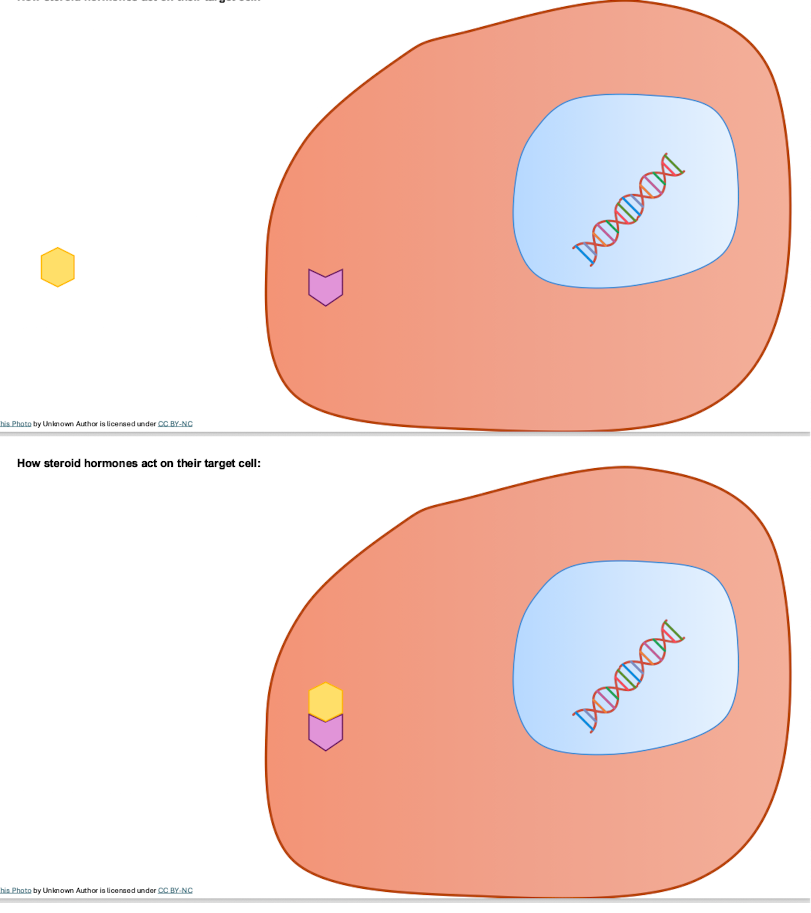
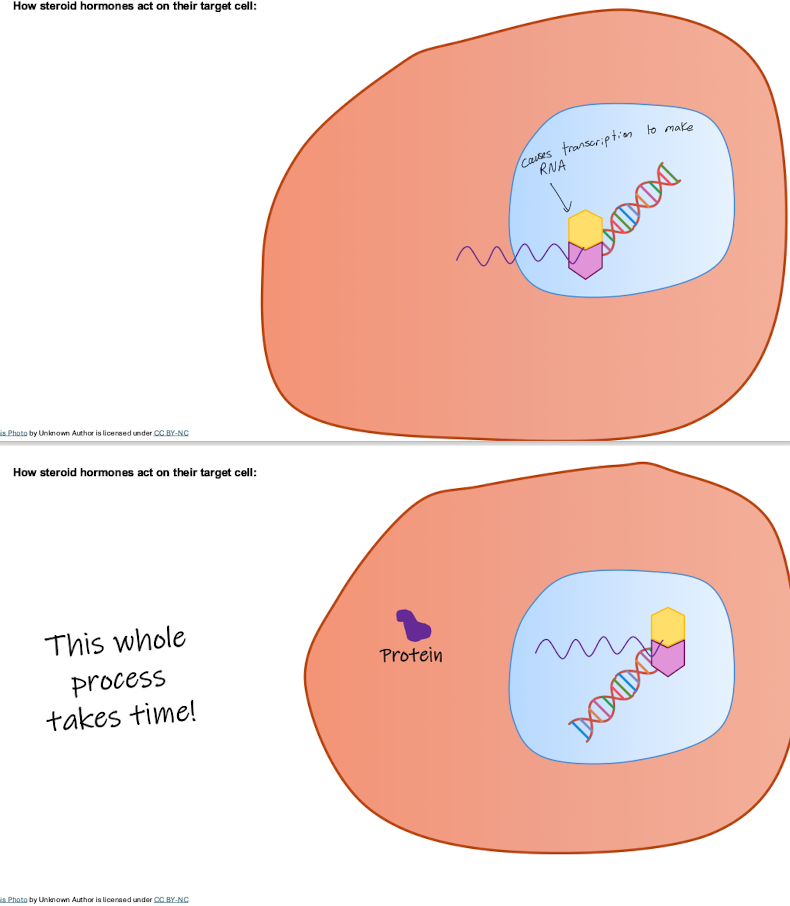
How do steriod hormones act on their target cell
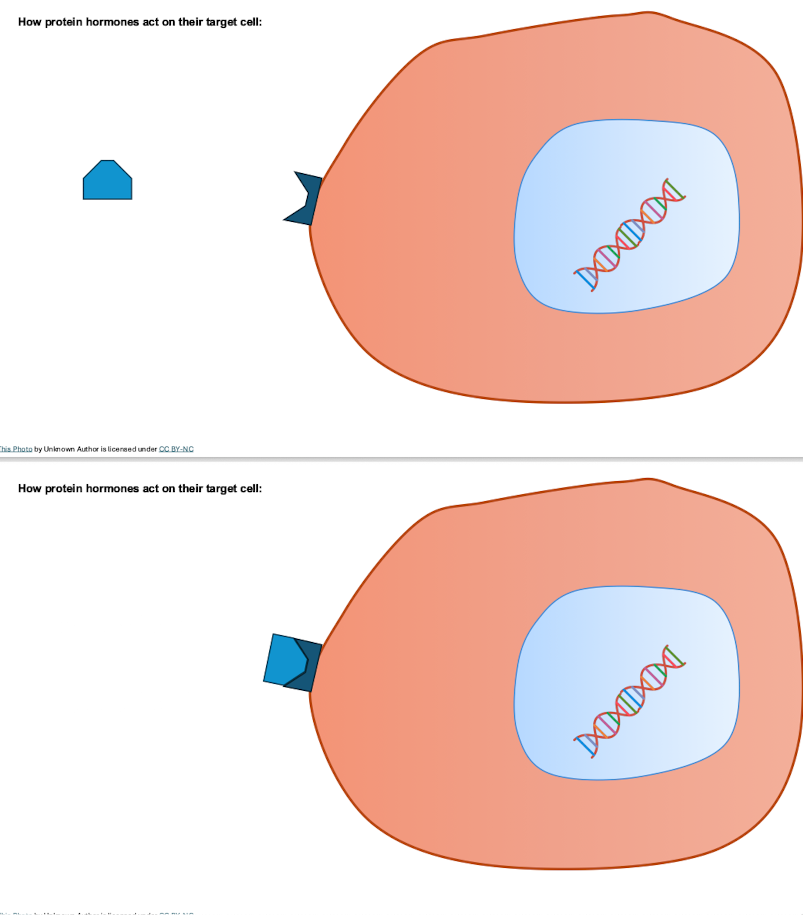
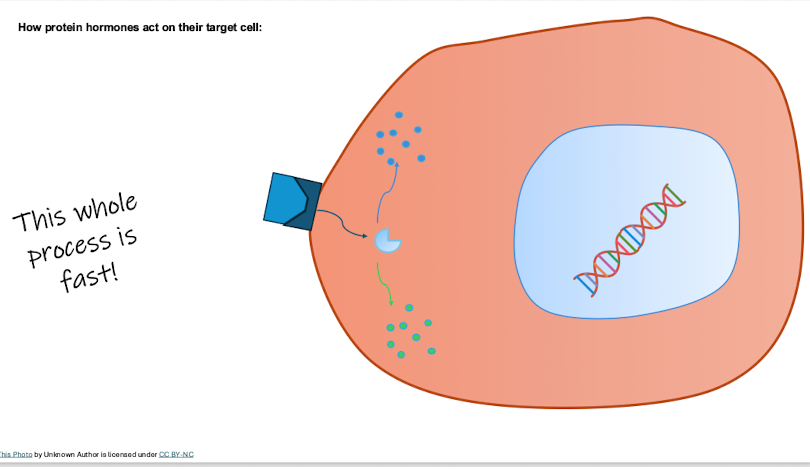
How do peptide hormones act on their target cell
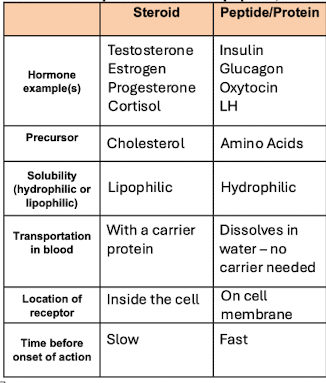
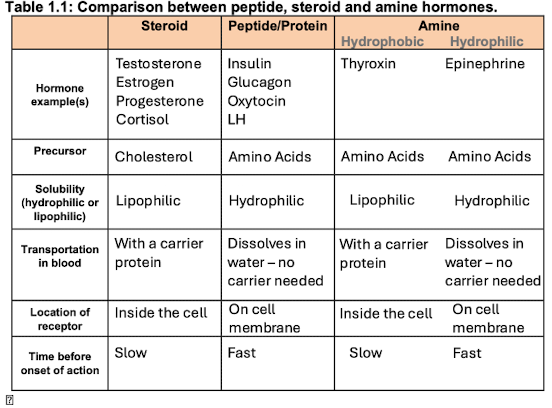
Steriod vs peptides on hormone examples, precursor, solubility, transport in blood, location of receptor, and time befoe onset of action
Thyroxin and epinephrine
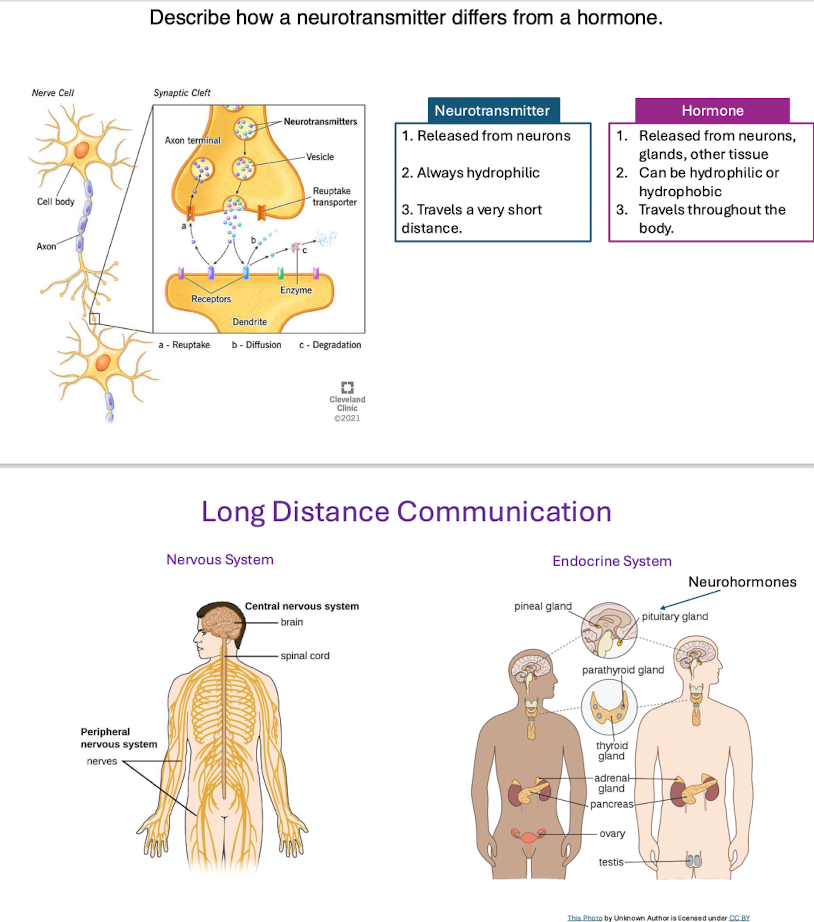
How do neurotransmitters differ from hormones
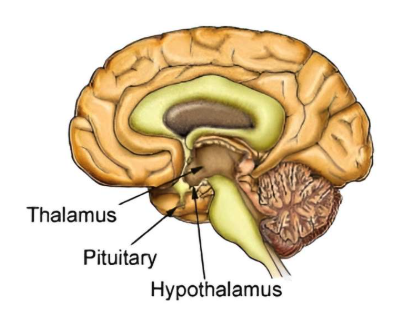
1) Where is the hypothalamus located, and what is its general structure?
The hypothalamus is located at the base of the brain just above the pituitary gland and below the thalamus. Because of its central location, it can receive information from all over the brain. It is composed of many regions made up of groups of nerve cell bodies, which are call nuclei. Several of these nuclei control the release of hormones from the pituitary gland.
2) How does the hypothalamus contribute to maintaining homeostasis in the body?
The hypothalamus is involved with some of the body's homeostatic mechanisms, including the regulation of body temperature, water balance, and energy production. It is also involved in regulating the behavioural drives of thirst, hunger, and sexual behaviour. In order to perform all of these complex and widespread function, the hypothalamus receives large amounts of information from all around the body, including metabolic, hormonal, temperature, and neural information.
3) What hormones are secreted by the hypothalamus?
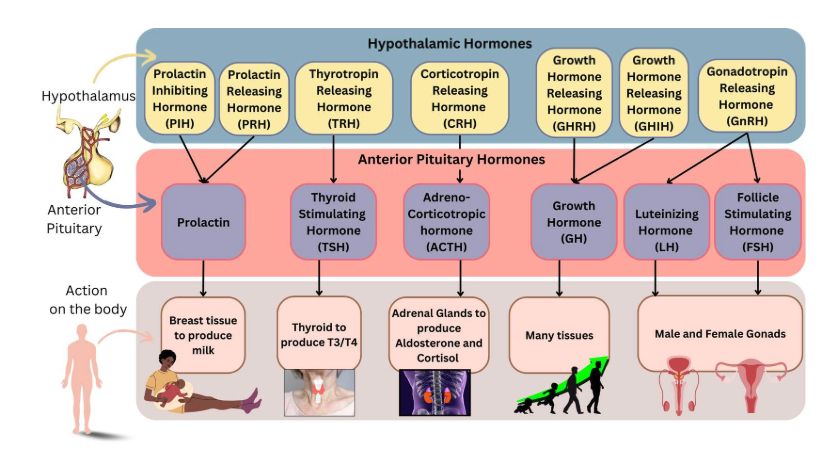
The hypothalamus secretes many types of hormones - sometimes called releasing or inhibiting hormones because they cause the release or inhibition of a hormones from the pituitary gland. The hormones in the list below are released by the hypothalamus and travel to the anterior pituitary. Click on each hormone below for more details on its function.
Prolactin releaseing hormone and prolactin inhibiting hormones
Prolactin releasing hormone (PRH) hormone is released after birth and continuously to help breastfeed a baby. It causes the release of prolactin from the anterior pituitary which then stimulates breast tissue to make milk.
When not breastfeeding, prolactin inhibiting hormone (PIH) is released from the hypothalamus and inhibits the release of prolactin, preventing the production of milk.
Thyrotropin releasing hormone
Thyrotropin releasing hormone (TRH) is released by the hypothalamus to the anterior pituitary, which will then release thyrotropin stimulating hormone, which will affect the thyroid. We will look more at the thyroid in the next section of this lesson. In this picture, we see a graphic of a thyroid gland, located in the neck.
Corticotropin releasing hormone
Corticotropin Releasing Hormone (CRH) is released by the hypothalamus and stimulates the anterior pituitary to release adrenocorticotropic hormone (ACTH). This in turn will stimulate the release of cortisol, involved in many actions throughout the body which we will see later in this lesson. The main reason for cortisol to be released is in response to stress. '
Growth hormone releasing hormone/ growth hormon inhibiing hormone
Growth Hormone Releasing Hormone (GHRH) will stimulate the anterior pituitary to release Growth Hormone (GH), while Growth Hormone Inhibiting Hormone (GHIH) has a slight inhibitory effect on GH release.
Gonadotropin releasing hormone
Gonadotropin Releasing Hormone (GnRH) is released from the hypothalamus and stimulate the anterior pituitary to release hormones that then affect the gonads.
4) How are the anterior and posterior sections of the pituitary gland related to the hypothalamus?
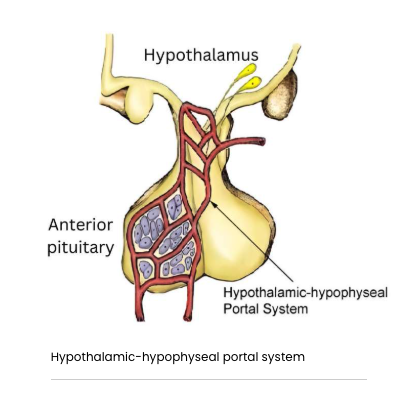
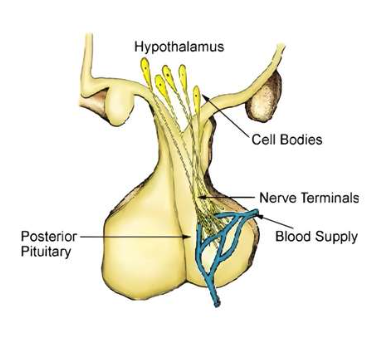
The pituitary gland is separated into two distinct regions - the anterior and the posterior pituitary. The anterior pituitary is formed during development from the tissue of the roof of the mouth. It is made up of endocrine tissue and is regulated by hormones. The hypothalamus sits above the pituitary gland and communicate with the pituitary through two different mechanisms, the hypothalamic-hypophyseal portal system and the hypothalamic-hypophyseal tract.
Hypothalamic-hypophyseal portal system
The hypothalamus communicates with the anterior pituitary by secreting the releasing or inhibiting hormones into the portal system. The portal system is made up of small blood vessels that link the hypothalamus directly to the anterior pituitary. The hormones from the hypothalamus then travel through the portal system to the anterior pituitary to either stimulate or inhibit the release of pituitary hormones.
posterior pituitary
The posterior pituitary develops from neural tissue at the base of the brain. It contains the axons and nerve terminal of neurons whose cell bodies lie in the hypothalamus. The tract of the neurons is sometimes referred to as the hypothalamic-hypophyseal tract. These neurons produce neurohormones in the hypothalamus that are secreted into the blood from the posterior pituitary in response to action potentials. We will look at these neurohormones a little later in the lesson.
The posterior pituitary releases two crucial hormones: oxytocin and antidiuretic hormone (ADH) also known as vasopressin. Unlike the anterior pituitary, the posterior pituitary does not produce its own hormones; instead, it stores and releases hormones produced by the hypothalamus. Each hormone is made in its own set of neurons, and is synthesized in the cell body of those neurons.
Axonal Transport: Once synthesized, oxytocin or ADH is packaged into vesicles (small membrane-bound sacs) and transported along the axons of the neurons to the posterior pituitary gland. These axons extend from the hypothalamus down into the posterior pituitary, where the hormone is stored.
Oxytocin or ADH is stored in the nerve endings (axon terminals) within the posterior pituitary until it is needed. The posterior pituitary is not a gland that synthesizes hormones itself but rather a storage and release site for hormones made in the hypothalamus, including oxytocin.
When the body requires oxytocin (e.g., during childbirth, breastfeeding, or in response to certain social and emotional stimuli), a signal is sent from the hypothalamus. This signal triggers an action potential that causes the release of oxytocin from the nerve endings in the posterior pituitary into the bloodstream.
The functions of the posterior pituitary are essential for fluid regulation, reproductive processes, and various aspects of social bonding and behaviour.
5) Why is the pituitary gland often referred to as the master gland of the body?
The anterior pituitary is a key endocrine gland that controls several critical bodily functions by releasing hormones into the bloodstream. It produces hormones such as growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), and gonadotropins (LH and FSH), which regulate growth, metabolism, stress response, and reproductive functions, respectively. The release of these hormones is regulated by the hypothalamus through the specific releasing and inhibiting hormones. Overall, the anterior pituitary plays a central role in maintaining homeostasis by coordinating various physiological processes. This chart shows where the different hormone are released from, what it affects on the anterior pituitary, and then how it affects the body. Please review it carefully.
Location in the body of adrenal glands
The adrenal glands are small, triangular-shaped endocrine glands situated on top of each kidney. They are part of the abdominal cavity, situated closer to the back, but protected by the ribs.
The adrenal glands are located bilaterally, with one gland resting on the top of each kidney.
They are positioned near major blood vessels:
The right adrenal gland is close to the inferior vena cava.
The left adrenal gland is near the aorta.
The glands receive a rich blood supply from the superior, middle, and inferior adrenal arteries, ensuring efficient delivery of hormones into the bloodstream.
Despite their small size, the adrenal glands are vital for producing hormones like cortisol, aldosterone, epinephrine, and norepinephrine, which regulate stress responses, metabolism, and electrolyte balance.
Organization of the adrenal glands
The gland has a distinct structure, divided into two main parts: the cortex (outer region) and the medulla (inner region). The adrenal cortex is further divided into three distinct zones, each responsible for producing specific hormones:

1. Zona Glomerulosa (Outer Zone):
Location: The outermost layer of the adrenal cortex.
Function: Produces mineralocorticoids, a class of steroid hormones that regulate minerals in the body. The most important of which is aldosterone.
Hormone Role:
Aldosterone regulates mineral balance by increasing sodium (Na⁺) reabsorption and potassium (K⁺) excretion in the kidneys.
This regulation helps maintain blood pressure and fluid balance.
Key Point: The zona glomerulosa is crucial for electrolyte and water balance in the body.
2. Zona Fasciculata (Middle Zone):
Location: The thickest layer of the adrenal cortex, located between the zona glomerulosa and zona reticularis.
Function: Produces glucocorticoids, a class of steroid hormones responsible for maintaining proper levels of glucose in the body. Most notable are cortisol and corticosterone.
Hormone Role:
Cortisol is involved in glucose metabolism, protein and fat breakdown, and the body's stress response.
It also suppresses the immune system, regulates inflammation, and aids in maintaining blood glucose levels during fasting or stress.
Key Point: This zone responds to ACTH (adrenocorticotropic hormone) released from the anterior pituitary, following stimulation by CRH (corticotropin-releasing hormone) from the hypothalamus. We will go over this pathway later in this lesson, and you can also review it by returning to the Endocrine Overview page(opens in a new tab).
3. Zona Reticularis (Inner Zone):
Location: The innermost layer of the adrenal cortex, adjacent to the adrenal medulla.
Function: Produces androgens, such as dehydroepiandrosterone (DHEA).
Hormone Role:
These hormones contribute to the development of secondary sexual characteristics during puberty.
In females, androgens can be converted into estrogen in peripheral tissues, particularly after menopause.
Androgens also stimulate hair growth in certain regions, such as the armpits.
Key Point: While the zona reticularis produces less androgen compared to gonads, its role is still significant in hormonal balance.
4. Adrenal Medulla (Inner Region):
Location: The central part of the adrenal gland, surrounded by the cortex.
Function: Produces catecholamines, primarily epinephrine (adrenaline) and norepinephrine (noradrenaline).
Hormone Role:
These hormones prepare the body for the fight-or-flight response by increasing heart rate, blood pressure, and glucose levels.
They also dilate airways in the lungs to improve oxygen delivery.
Key Point: The adrenal medulla functions as part of the sympathetic nervous system and is activated by stress or physical activity.

adrenal tissue layers and associated hormones
Overall Organization and Functionality:
Each layer of the adrenal gland has specialized roles to ensure the body's homeostasis and response to external and internal stimuli. From regulating mineral balance (zona glomerulosa) to managing energy and stress (zona fasciculata), influencing sexual characteristics (zona reticularis), and triggering rapid responses (adrenal medulla), the adrenal gland is indispensable for survival and adaptation.
Role of Cortisol
Cortisol is a glucocorticoid hormone produced by the adrenal cortex (specifically the zona fasciculata). It is often referred to as the "stress hormone" because it helps the body respond to stress and maintain homeostasis. Its effects are widespread, influencing metabolism, the immune system, and other physiological functions.
Metabolic Regulation
Glucose Metabolism: Increases blood glucose levels by stimulating gluconeogenesis (the production of glucose from non-carbohydrate sources) in the liver.
Protein Catabolism: Breaks down proteins in muscle tissue to provide amino acids for gluconeogenesis.
Fat Metabolism: Promotes lipolysis (breakdown of fats) in adipose tissue, releasing glycerol and free fatty acids for energy production.
Fat redistribution: Makes fat (important energy source) more accessible by redistributing it to the face and abdomen from the peripheral limbs.
Energy Mobilization: Ensures that the body has enough energy during fasting or stress by prioritizing glucose availability for the brain.
Cortisol regulation - and Steps in the Cortisol Regulation and Feedback Loop
Cortisol regulation is controlled through a finely tuned hypothalamic-pituitary-adrenal (HPA) axis, which ensures cortisol levels are maintained appropriately based on the body’s needs. The negative feedback loop is the central mechanism for preventing overproduction or underproduction of cortisol. We were first introduced to the hormones involved in this pathway in Endocrine Overview. Watch the video to see how cortisol is regulation by the HPA axis.
Activation:
When the body encounters stress (e.g., physical stress, low blood glucose, or psychological stress), the hypothalamus releases CRH into the bloodstream.
Pituitary Response:
CRH travels to the anterior pituitary gland, prompting it to release ACTH.
Adrenal Cortex Activation:
ACTH stimulates the adrenal cortex (specifically the zona fasciculata) to secrete cortisol into the bloodstream.
Effects of Cortisol:
Cortisol exerts widespread effects:
Increases blood glucose via gluconeogenesis.
Suppresses the immune response.
Affects mood and behavior.
Mobilizes energy by breaking down fats and proteins.
Negative Feedback:
Elevated cortisol levels inhibit further secretion of CRH from the hypothalamus and ACTH from the anterior pituitary.
This feedback loop prevents excessive cortisol production, maintaining balance.
Summary
Hypothalamus: Releases CRH → Stimulates Anterior Pituitary.
Anterior Pituitary: Releases ACTH → Stimulates Adrenal Cortex.
Adrenal Cortex: Releases Cortisol.
Cortisol: Provides negative feedback → Inhibits CRH and ACTH production.
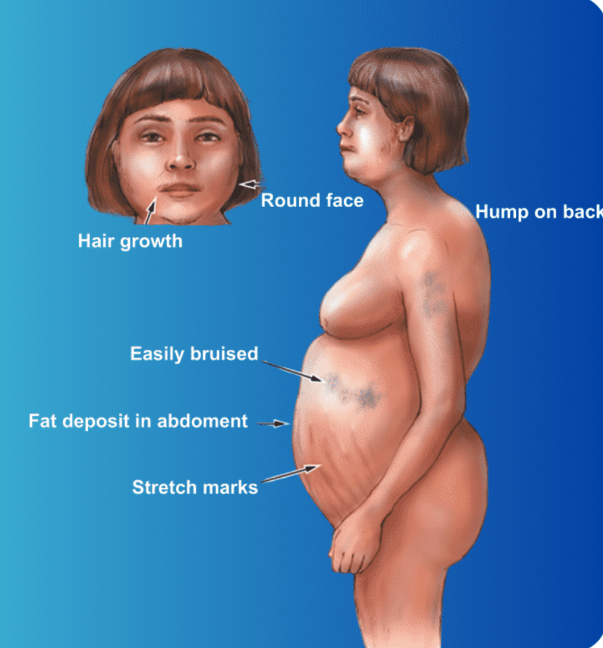
Cushing's Disease - Too much Cortisol
Cushing's syndrome is a disorder caused by prolonged exposure to high levels of cortisol. It can result from endogenous factors (overproduction by the body) or exogenous factors (prolonged use of corticosteroid medications). The condition affects multiple organ systems, leading to significant physical and metabolic changes.
The most common cause is by a tumor in the pituitary gland that secretes excess ACTH (adrenocorticotropic hormone), overstimulating the adrenal glands.
Cushing’s syndrome presents with a range of distinctive physical features and systemic effects due to prolonged exposure to high cortisol levels. Notable physical changes include a rounded, full face, often called "moon face," and a "buffalo hump," caused by fat accumulation on the back of the neck and upper back. Fat tends to concentrate in the abdomen, leading to central obesity with relatively thin limbs. Wide, purple or reddish stretch marks (striae) are commonly seen on the abdomen, thighs, or breasts. Additionally, the skin becomes thinner and more fragile, making it prone to bruising and slow wound healing. Women may experience excessive facial or body hair growth (hirsutism) due to hormonal imbalances.
Metabolic, cardiovascular, and immune system effects further compound the condition's severity. Hyperglycemia frequently occurs as cortisol promotes gluconeogenesis, and protein catabolism leads to muscle wasting and weakness. Bone loss, or osteoporosis, is a common complication, increasing the risk of fractures. Elevated cortisol also enhances vascular sensitivity to catecholamines, resulting in hypertension. Immune suppression leaves individuals more susceptible to infections, while the psychological impact includes mood swings, depression, anxiety, and cognitive impairments, all contributing to the disorder's complex presentation.
Epinephrine: Overview and Function
Epinephrine, also known as adrenaline, is a hormone and neurotransmitter produced primarily by the adrenal medulla, the inner region of the adrenal glands. It plays a crucial role in the body’s response to stress, particularly during the "fight-or-flight" reaction. It is a amine hormone, like T3 /T4 however, this hormone is hydrophilic. It is released into the blood stream, does not require a carrier protein to transport it, will have its receptor on the cell membrane of its target tissue, and will cause a rapid response. Let's see what the rapid response is so important!A Bear Encounter and the Power of Epinephrine
Jack was hiking in the woods when he turned a corner and saw a big bear on the path. Jack’s heart started pounding fast, and his breathing sped up.
This sudden reaction happened because Jack’s brain sent an emergency signal to his adrenal glands. The glands released epinephrine into his blood causing his heart to pump blood faster, his lungs to open up to take in more air, and his senses to became sharp and alert.
The bear eventually wandered off, and Jack felt his pounding heart start to slow down while his body relaxed.
Functions of Epinephrine
Epinephrine is short lived in the body, heightening the body's response to help you get away from danger. It is not regulated by negative feedback mechanisms or by hormones, but instead, is stimulated when the sympathetic pathway is activated by danger or acute stress. It has many effects on the body, but only acts for a short period of time to help you get away or fight your way out of danger. The following are some effects epinephrine has on other bodily systems. These effects are sometimes also felt before taking an exam. As you go through each one ask yourself how this would help you survive a dangerous situation or to help you get ready for a stressful event.
Cardiovascular Effects:
Increases heart rate and force of contraction, improving blood flow to vital organs and muscles.
Constricts blood vessels in less essential areas (like the skin), raising blood pressure.
Dilates blood vessels in skeletal muscles and the lungs, enhancing oxygen delivery.
Metabolic Effects:
Stimulates glycogenolysis (breakdown of glycogen into glucose) in the liver and muscles, rapidly increasing blood glucose levels.
Promotes lipolysis in adipose tissue, releasing fatty acids for energy use.
Respiratory Effects:
Relaxes smooth muscles in the airways, leading to bronchodilation, which increases airflow to the lungs.
Other Effects:
Increases pupil dilation to enhance vision during stress.
Heightens mental alertness and prepares the body for rapid action.
How Epinephrine is Released
Signal Pathway:
The hypothalamus signals the sympathetic nervous system, which stimulates the adrenal medulla at the centre of the adrenal gland.
Cells in the adrenal medulla release epinephrine into the bloodstream. Since epinephrine is hydrophilic, it quickly dissolves into the blood stream and is distributed to the body.
Trigger:
Stressful stimuli, such as physical exertion, fear, low blood sugar, or injury, activate the sympathetic nervous system.
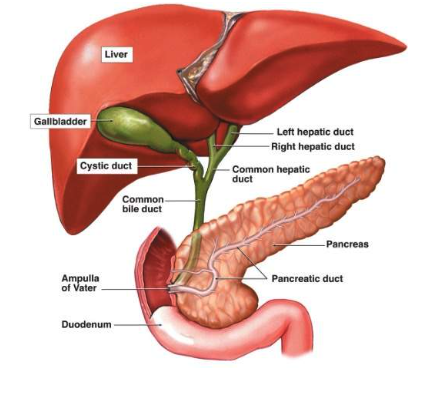
1) What is the structure and function of the pancreas?
The pancreas plays a vital role in the endocrine system by producing and secreting hormones that regulate blood sugar levels. The two main hormones are insulin and glucagon. Insulin lowers blood sugar levels by promoting the uptake of glucose into cells, where it can be used for energy or stored as glycogen. On the other hand, glucagon raises blood sugar levels by signalling the liver to release stored glucose into the bloodstream.
This delicate balance between insulin and glucagon ensures that the body maintains stable blood sugar levels, which is crucial for overall health. Any disruption in this balance can lead to conditions such as diabetes. In type 1 diabetes, the pancreas fails to produce enough insulin, while in type 2 diabetes, the body’s cells become resistant to insulin. Therefore, the endocrine function of the pancreas is essential for metabolic regulation and energy management.The pancreas lies parallel to and beneath the stomach. It contains both endocrine tissue, secreting hormones into the blood, and exocrine tissue, secreting chemicals through a duct into the digestive tract. The endocrine portion consists of 1 million to 2 million pancreatic islets, each about 0.3 mm in diameter. These islets, which surround small capillaries, contain three principal types of cells : alpha cells make up to 25% of the islets and secrete glucagon; beta cells make up 60% of the islets and secrete insulin and amylin; and delta cells make up 10% of the islets and secrete somatostatin. The exocrine portion, which we will look at in a later lessons, consists of pancreatic acinar cells and ducts.
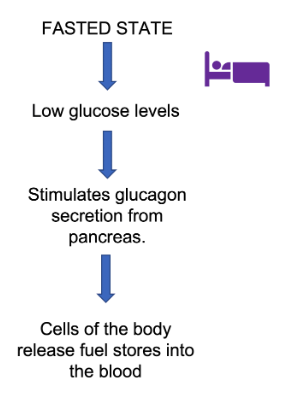
Glucagon
Glucagon is a hormone that is release by the alpha cells in the pancreas in response to low blood glucose, or a fasted state. A fasted state can occur when food has not been consumed for a while, like after sleeping at night. Glucagon acts on tissues in the body to stimulate the production and release of glucose from storage. In muscle cell, glucagon causes glycogen, a glucose storing molecule, to break down, and glucose to be released. In the liver, it stimulates the production of new glucose molecules through gluconeogenesis, an enzymatic process that the liver has to make glucose. Glucagon is a peptide hormone.
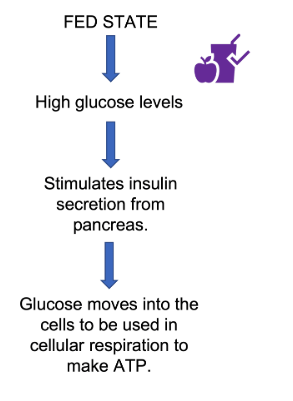
Insulin
Insulin is released by the pancreatic beta cells in response to high blood glucose levels, or a fed state. A fed state will occur after food has been consumed, like after a meal. Insulin is secreted by the pancreas and released into the blood stream. It acts on target tissue to help promoted the movement of glucose from the blood to inside the target tissue cell. There, glucose can be metabolized into ATP, which provides energy for the cell. Insulin also promotes the storage of glucose into glycogen within muscles cells. Insulin is a peptide hormone.
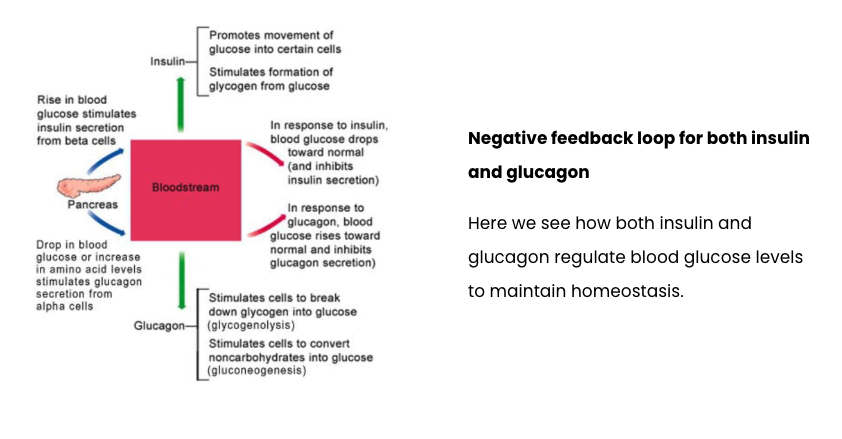
Negative feedback loops for glucagon and insulin
Both glucagon and insulin regulate blood glucose levels, and work in tandem to keep blood glucose levels with a homeostatic range. The following video shows the negative feedback loop for insulin. Note which aspects of the negative feedback loop are the effector and variable.
Diabetes Mellitus
Diabetes Mellitus is a disease that results in either the inability of the pancreas to produce insulin (Type I) or an inability of target cells to properly respond to insulin (Type II). In either scenario, the ultimate issue is that the uptake of glucose into the cell is severely decreased, causing blood glucose levels to be high and remain high. This can have serious deleterious effects throughout the body.
The term "melitus" comes from the Latin word mel, which means "honey." In the context of diabetes, "melitus" refers to the sweet-smelling urine that was historically observed in people with the condition. The term "diabetes" itself is derived from the Greek word siphon, referring to the frequent urination associated with the disease.
So, "diabetes mellitus" essentially means "honey-sweet diabetes," reflecting the high levels of glucose in the urine that give it a sweet odor.
Type 1 Diabetes
This involves the damage of insulin producing beta cells in the pancreas, and as it usually occurs around that age 14, it is ofter referred to as juvenile diabetes. What triggers the damage to beta cells is still largely not understood and a strong area of research.
Type 2 Diabetes
Type II diabetes usually has its onset later in life, around 45 years of age, however, younger and younger people are presenting with type II diabetes according to the centre for disease control (CDC). Type II diabetes can occur due to a variety of factors, such as diet, lifestyle, and genetic heritability. In type II diabetes, the target cells no longer properly respond to insulin, as if they have become tolerant to insulin, and therefore, the effects of insulin are diminished. This can then result in exhaustion of the pancreatic beta cells, and less and less insulin is produced.
Physiological explanation for diabetes symptoms
polyuria
Polyuria, (or having to 'wee' a lot as the video said), is increased frequency in urination. This is due to the high levels of glucose in the blood that then results in a high level of glucose in the fluid that will become the urine. In the kidneys, glucose is reabsorbed out of the fluid prior to the fluid becoming urine. Glucose first has to be reabsorbed to create an osmotic gradient that then allows water to be reabsorbed. In diabetes, there is SO MUCH glucose that it cannot all be reabsorbed, and thus less water is reabsorbed. This causes an increased volume of urine, resulting in frequent urination.
Thirst
Due to the decrease in water reabsorption in the kidneys, the body becomes regularly dehydrated. Under normal circumstances, the kidneys would be able to reabsorb water from the fluid prior to it becoming urine. But due to the high concentration of glucose (a solute) in the fluid, there isn't enough tonicity across the kidney to cause the movement of water out of the fluid and back into the blood circulation. We will see this in more detail once we reach the renal section of the course.
Blood vessels
Increased blood glucose levels can lead to damage to blood vessels, which can subsequently lead to damage to other tissues and organs. This can also lead to damage to vision, and could possible lead to strokes or heart attacks as well.
Metabolic Acidosis
Metabolic Acidosis is primarily associated with Type 1 diabetes and is also known as Diabetic Ketoacidosis. Since the body cannot use glucose properly, it will instead start to deplete other energy stores, like fat and proteins. This is what causes the sudden weight loss. The breakdown of fats leads to the release of ketones into the blood, which decreases the pH of the body, making it more acidic. This can then affect enzyme, protein, and cell function throughout the body. In severe cases this can lead to coma or death.
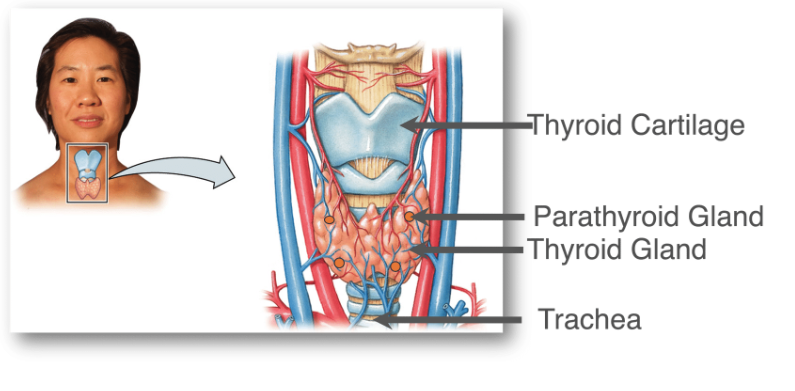
1) Where the thyroid is located
The thyroid is a butterfly like structure located in the neck. On the thyroid are four small glands which make up the parathyroid.
2) How thyroid hormone is regulated
At this point, you have seen the Hypothalamic Pituitary Thyroid axis before in the overview of endocrinology. Below, is a video showing how these hormones relate to one another.
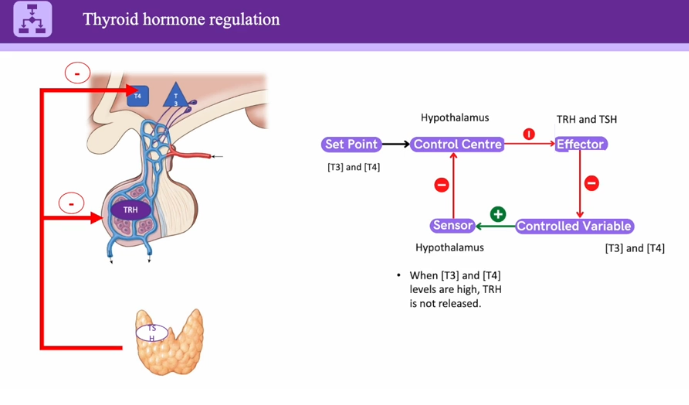
Step-by-Step Process of Thyroid Hormone Production and Regulation
The thyroid hormone system is regulated by the Hypothalamic-Pituitary-Thyroid (HPT) Axis and is crucial for metabolism, growth, and energy balance. The thyroid produces two major hormones:
Thyroxine (T4) – The inactive form, converted into T3 when needed.
Triiodothyronine (T3) – The active form that regulates metabolism.
Here’s how thyroid hormone is produced, released, and regulated in the body:
Step 1: Hypothalamus Releases TRH (Thyrotropin-Releasing Hormone)
The hypothalamus detects low thyroid hormone levels or increased energy demands.
It releases thyrotropin-releasing hormone (TRH) into the bloodstream.
TRH travels to the anterior pituitary gland.
Step 2: Pituitary Gland Releases TSH (Thyroid-Stimulating Hormone)
TRH stimulates the anterior pituitary to release thyroid-stimulating hormone (TSH).
TSH enters the bloodstream and travels to the thyroid gland.
TSH tells the thyroid to produce and release thyroid hormones (T3 and T4).
Step 3: Thyroid Gland Produces and Releases T3 & T4
The thyroid gland absorbs iodine (from food) and combines it with the amino acid tyrosine.
It forms thyroxine (T4) and a smaller amount of triiodothyronine (T3).
Most of the thyroid hormone released is T4, which is later converted into the active form, T3, in tissues.
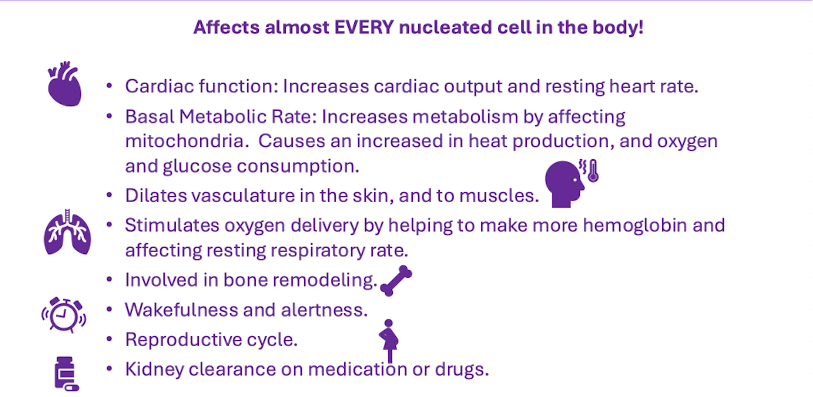
Step 4: T3 and T4 Regulate Metabolism
T3 (active hormone) enters cells and binds to receptors, influencing:
Metabolism – Increases oxygen use and energy production.
Heart rate – Increases cardiac output.
Temperature regulation – Generates heat.
Brain function – Supports cognitive function.
T4 (inactive form) circulates in the blood and is converted into T3 when needed.
Step 5: Negative Feedback Regulation
When T3 and T4 levels rise, they signal the hypothalamus and pituitary to reduce TRH and TSH secretion.
This prevents excessive thyroid hormone production, maintaining balance.
If T3 and T4 levels drop, the process restarts, increasing hormone release.
What does thyroid hormone do
Thyroid anatomy
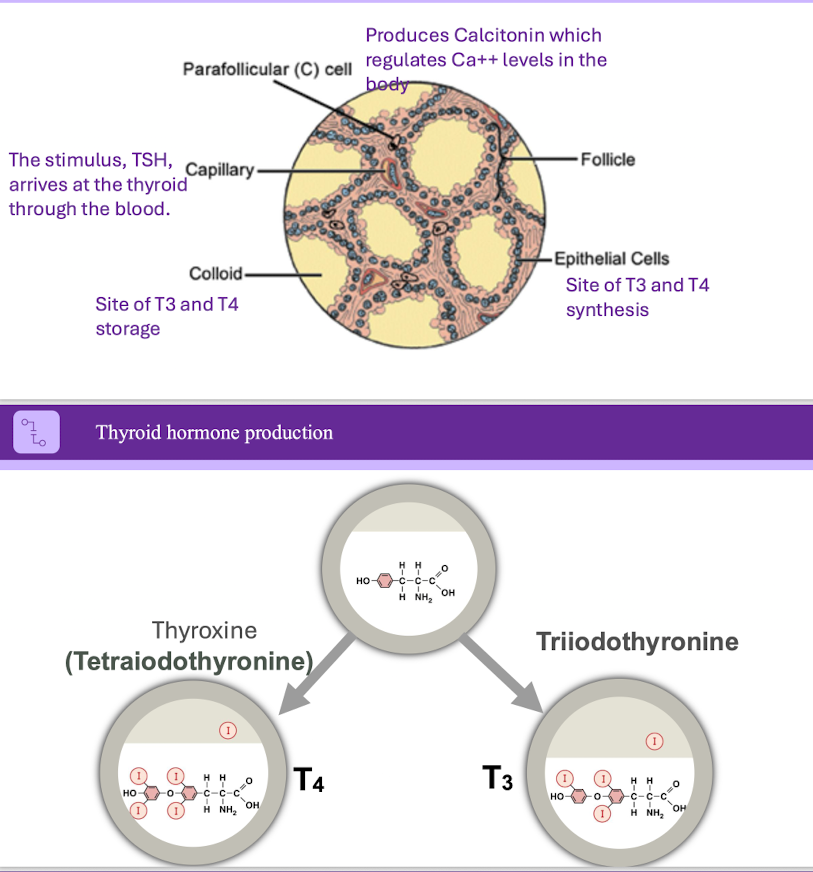
How Parafollicular Cells Regulate Calcium with Calcitonin
Parafollicular cells (also called C cells) are specialized cells in the thyroid gland that produce and release calcitonin, a hormone involved in calcium homeostasis. These cells are located outside the thyroid follicles and play a role in lowering blood calcium levels when they become too high.
Sensing High Blood Calcium Levels
When blood calcium (Ca²⁺) levels rise above normal, parafollicular cells detect this increase.
Releasing Calcitonin
In response, parafollicular cells secrete calcitonin into the bloodstream.
Calcitonin Lowers Blood Calcium by Acting on Three Targets:
Bones – Inhibits osteoclast activity, preventing bone breakdown (resorption), which reduces calcium release into the blood.
Kidneys – Enhances calcium excretion in urine by reducing calcium reabsorption in the renal tubules.
Intestines – Decreases calcium absorption from food, helping to prevent further increases in blood calcium levels.
Effect: Blood Calcium Levels Drop
With less calcium released from bones, more excreted in urine, and less absorbed from food, blood calcium levels return to normal.
7) Parathyroid Gland and Its Role in Calcium Regulation
The parathyroid glands, located behind the thyroid, produce parathyroid hormone (PTH), which raises blood calcium levels when they drop too low. PTH acts on three main targets:
Bones – Stimulates osteoclasts to break down bone and release calcium into the bloodstream.
Kidneys – Reduces calcium excretion and increases calcitriol (active vitamin D) production.
Intestines – Enhances calcium absorption from food via calcitriol.
PTH works opposite to calcitonin, ensuring calcium levels remain balanced for nerve signalling, muscle function, and bone health.
Calcitonin vs. Parathyroid Hormone (PTH)
Calcitonin (from the thyroid) lowers blood calcium.
Parathyroid Hormone (PTH) (from the parathyroid glands) raises blood calcium.
These two hormones work in opposition to maintain calcium homeostasis.