Weight loss and chronic colic
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
55 Terms
what are the mechanisms of weight loss?
reduced energy intake due to reduced access - e.g. inappropriate feeding, competition for feed, dental disorders, dysphagia
reduced digestion, absorption or assimilation of nutrients - e.g. dental disorders so less mechanical breakdown, malabsorption syndromes, liver disease
physiological increased energy demand - e.g. exercise, pregnancy, lactation, cold
pathological increased energy demand - e.g. neoplasia, infection, immune mediated, GI renal or effusion losses
additional mechanisms causing increased energy demand - e.g. chronic pain, stress, cachexia, primary muscle loss, aging (sarcopenia)
what are the most common causes of weight loss?
dental disorders
parasitism
inadequate diet
what is colic?
behavioural manifestation of visceral pain - usually intestinal pain e.g.
stretch
inflammation
ischaemia
muscle spasm
when is colic considered chronic?
if signs persist for more than 48 hours
when is colic considered recurrent?
if horse experiences shorter periods of colic pain which recur at variable intervals
what are the most common causes of recurrent colic?
colon displacement
impaction
adhesions
gastric ulceration
IBD
however most often the cause is not established
what is the most important history to take for recurrent colic cases?
diet esp if any recent changes
worming / FWEC (faecal worm egg count)
any dental problems or quidding
number and nature of previous colics
if regular 3 weekly colicing, what does this suggest?
ovulatory pain
if colic intervals are getting increasingly shorter, what does this suggest?
worsening of bowel condition
if investigating chronic weight loss, what would we look for in blood and faecal tests?
specific organ disease - liver enzymes, creatinine, etc
inflammatory processes - WCC, fibrinogen, globulins
protein loss - albumin
hypercalcaemia? - can be indicator of malignancy
faecal egg count
ELISA tests for cyathostominosis / tape worm
how should we interpret total protein for chronic weight loss?
often have a decrease in total protein, but may be masked by concurrent dehydration
how should we interpret hypoalbuminaemia for chronic weight loss?
may be due to loss - GI most common, or due to effusions
may be due to lack of production - malabsorption, liver disease
how should we interpret hypoglobulinaemia for chronic weight loss?
most commonly due to GI loss
how should we interpret hyperglobulinaemia for chronic weight loss?
suggests chronic inflammatory disease (incl. cyathostomosis)
how should we interpret fibrinogen / serum amyloid A for chronic weight loss?
acute phase proteins, SAA quicker up and down in response to infection
uses of abdominocentesis in chronic weight loss?
perform fluid analysis on peritoneal tap
nucleated cell count
protein
lactate
cytology

what does this peritoneal US show?
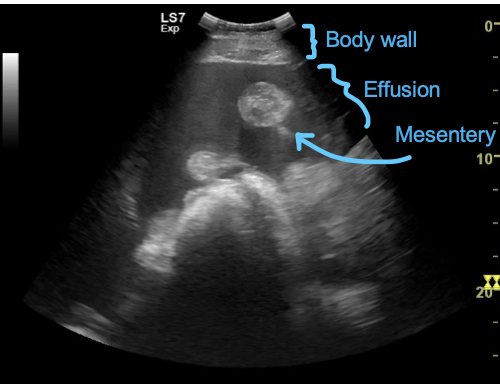
tadpole looking structure = intestine, normal to see the round part, but wouldnt usually see the mesentery (tail of tadpole)
what do we look for on abdominal US?
position of organs
intestinal wall thickness
intestinal lumen diameter
motility
any abnormal structures
signs of peritoneal effusion
what further tests (after blood and faecal tests and US) can be done to investigate chronic weight loss?
oral glucose absorption test - for small intestine only
rectal biopsy
gastroscopy
(duodenal biopsy) - can’t be done without ex lap
exploratory laparotomy / laparoscopy
how do you perform an oral glucose absorption test?
fast overnight
get baseline blood glucose level
give 1g glucose per kg BW as 20% solution by nasogastric tube
keep horse calm
measure blood glucose every 30 mins
what does oral glucose absorption test results show?
more than 85% increase in blood glucose = normal
15-85% increase in blood glucose = partial malabsorption
less than 15% increase in blood glucose = complete malabsorption
results indicate small intestinal absorption
how is a rectal biopsy performed?
use mare uterine biopsy instrument
20-30cm inside rectum
small piece of mucosa from floor at around 10 or 2 o’clock
submit for histology
give antibiotics and tetanus prophylaxis
what are some malabsorption and protein-losing enteropathy syndromes?
lymphocytic-plasmacytic enteritis
eosinophilic enteritis
granulomatous enteritis
inflammatory cells in intestinal wall leading to malabsorption and protein loss - diagnosis of exclusion
how do we treat IBD?
prednisolone
dexamethasone
highly digestible diet
see if responsive to anthelmintics
what are some multisystemic infiltrative bowel diseases?
multisystemic eosinophilic epitheliotropic disease (MEED)
systemic granulomatous disease
If IBD is steroid responsive, what are possible diagnoses?
eosinophilic enteritis
granulomatous enteritis
lymphocytic-plasmacytic enteritis
If IBD is non-steroid responsive, what are possible diagnoses?
eosinophilic enteritis
granulomatous enteritis
lymphocytic-plasmacytic enteritis
alimentary lymphoma
what are differential diagnosis for IBD?
cyathostomosis
mixed strongyle infection
idiopathic
infiltrative bowel disease
neoplasia
lawsonia (foals 3-11 months)
what are the types of equine lymphoma?
alimentary - generalised or solitary
cranial mesenteric
cutaneous
paraneoplastic syndromes:
hypercalcaemia
haemolytic anaemia
cachexia
what can we commonly see clinically with equine lymphoma?
fever
weight loss
peritonitis
pleural effusion
abdominal distension
intra-abdominal mass palpable per rectum
hypercalcaemia / haemolysis / cachexia of malignancy
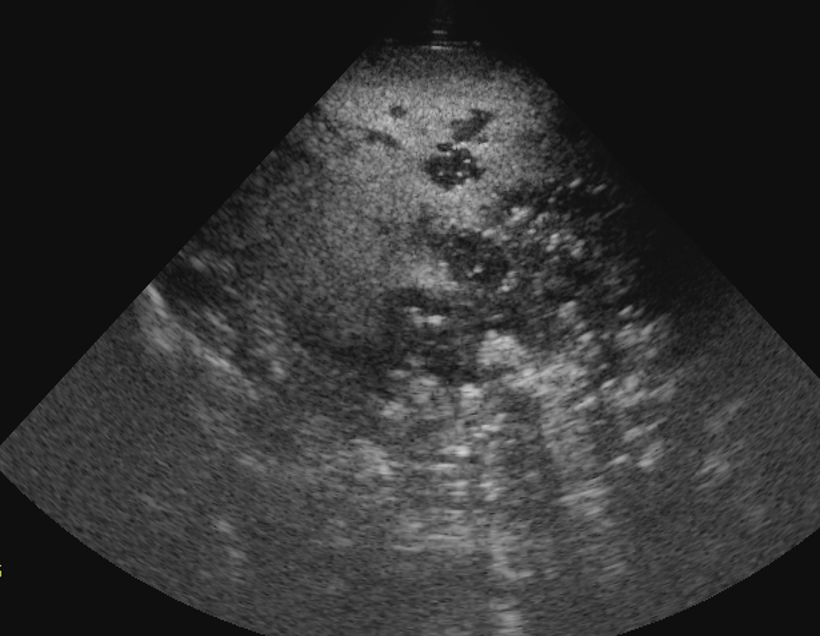
what does this US show?
islands of abnormal tissue in the spleen
can’t see distinct borders of spleen
—> possibly lymphoma
what neoplasms do we see in intestines?
lymphoma
leiomyoma
myxosarcoma
gastric or adenocarcinoma
melanoma
what bacteria are common causes of chronic intestinal disease?
Streptococcus equi
Rhodococcus equi
how to diagnose bacterial chronic infections in intestines?
inflammatory haemogram - neutrophilia, hyperfibrinogenaemia, anaemia
how to treat chronic bacterial intestinal infections?
long term antibiotics
what parasites do we see chronically?
large strongyle (S. vulgaris) —> verminous arteritis and thromboembolic colic
small strongyle (cyathostomins) —> submucosal inflammation
parascaris equorum
what are common haematological changes for parasitism?
neutrophilia
hypoalbuminaemia
hyperglobulinaemia
NOT eosinophilia
what can equine gastric ulcer syndrome be the cause of?
poor athletic performance
recurrent colic / poor behaviour
weight loss
bruxism (teeth grinding)
what horses is equine gastric ulcer syndrome common in?
horses in training (approx 70%)
highest incidence in thoroughbred race horses
what are the two branches of equine gastric ulcer syndrome (EGUS)?
equine squamous gastric disease
equine glandular gastric disease
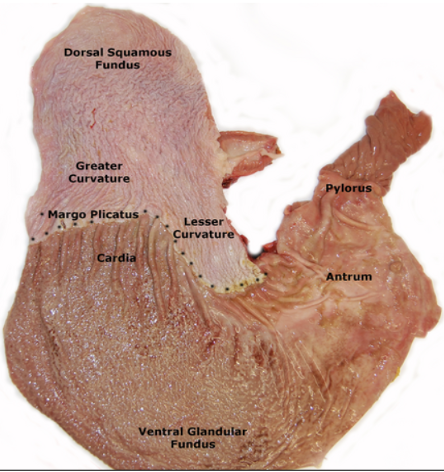
what part of the horse stomach do we see equine squamous gastric disease?
margo plicatus most common area
also dorsal squamous fundus, greater curvature and lesser curvature

what part of the horse stomach do we see equine glandular gastric disease?
ventral glandular fundus
what causes equine squamous gastric disease?
acid contact with squamous epithelium - pH is usually 5-7
primary - associated with management factors, rest of GI tract normal
secondary - due to delayed emptying of stomach after another problem with GI tract e.g. glandular disease
what are risk factors for equine squamous gastric disease?
performance horses
diet - high starch, intermittent fasting
increased stabling
stress, transport, etc.
what are risk factors for equine glandular gastric disease?
sports and leisure horses
exercise more than 4 days a week (but not intensity)
recently started training
inflammatory bowel disease
reduced blood supply to stomach
what medication can be used for gastric ulcers?
omeprazole
give on empty stomach, give 30-60 min before morning feed
4mg/kg for 4 weeks