lacrimal system IV: disorders of the orbit
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
what is the general aeitology of orbital diseases (6)
inflammatory
infectious
neoplastic - tumours/malignants
trauma - surgery
malformation
vascular
any abnormalities with the above categories that occur behind the globe/within the orbit can lead to orbital diseases
describe the general symptoms of orbital diseases (6)
•Eyelid swelling
•Bulging eye(s) - eyes pushed forward
•Double vision - as extraocular muscles effected and eyes do not work as well together
•Pain (sometimes ↑ on ocular movement)
•Blurring - as optic nerve is compressed
•Change in colour vision - due to effects on optic nerve
what are the general CRITICAL signs of orbital diseases (3:1:1)
Globe dystopia (abnormal displacement of the eyeball within the orbit):
•Proptosis/exophthalmos (linked to thyroid disease) - forward protrusion of the eyeball from the orbit
•Hyperglobus (upwards) & hypoglobus (downwards) - vertical displacement of the globe
Restricted ocular motility
if these signs occur = urgent referral

describe other/non-critical general signs of orbital disorders (3:3)
Soft tissue involvement:
Eyelid & periorbital oedema - swelling of eyelids and tissues around the orbit
ptosis - abnormal drooping of upper lid
Chemosis - conjunctival swelling
Fundus changes:
Optic disc swelling/atrophy
Collaterals - new blood vessels around optic disc - right at discs - tend not to leak/bleed
Choroidal folds - lines/streaks along the retina as seen in image below

explain the aeitology of thyroid eye disease - TED (2)
Systemic autoimmune disease/condition - increased or decreased thyroid production
Ocular effects - in soft tissue around the eyes - and ocular muscles
describe the early (5) and late (5) ocular symptoms of thyroid eye disease
Early/non speific ocular symptoms:
Non-specific FB sensation
Redness
Tearing
Photophobia - abnormal sensitivity/discomfort in bright light
Eyelid puffiness
Late ocular symptoms:
Persistent lid swelling
Chemosis - conjunctival oedema
Prominent eyes
Double vision (thickened muscles)
Loss of vision (optic nerve/corneal involvement
what are the signs of TED (8)
Eyelid retraction - eyelid lag on downgaze - lagophthalmos (inability to close eyelids properly - exposure keratopathy)
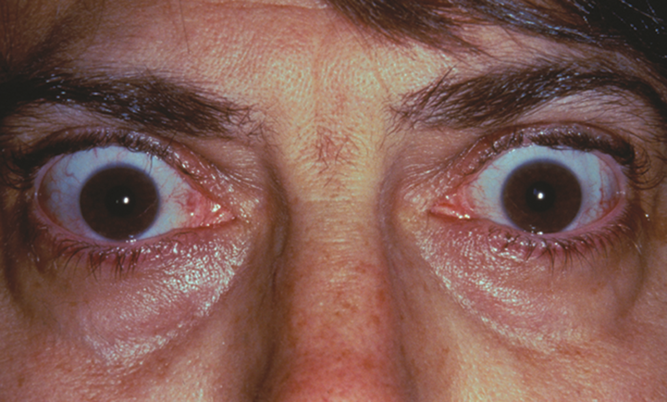
Uni or bilateral proptosis - 50% of patients - these px will often have choroidal folds
Variable ocular motility restriction - 40% of patients - due to EOM fibrosis and contracture
Higher IOP in up gaze
Conjunctival/lid hyperaemia/ oedema
Superior limbic keartoconjunctivits - kerato - involving cornwa
Optic nerve swelling/pallor
pupil abnormalities - RAPD & defective colour vision

what is the management of TED (4)
•Referral to GP or Ophthalmologist
•Steroids
•Radiotherapy
•Surgical decompression
state and briefly explain the 2 types of cellulitis (3
preseptal and orbital
cellulitis - inflammation of subcutaneous connective tissue
affects periorbital or orbital tissue (depending on type)
what is the aetiology of preseptal and orbital cellulitis (3)
caused by a bacterial infection
most commonly < 10 years old
severity varies form minor to life-threatening
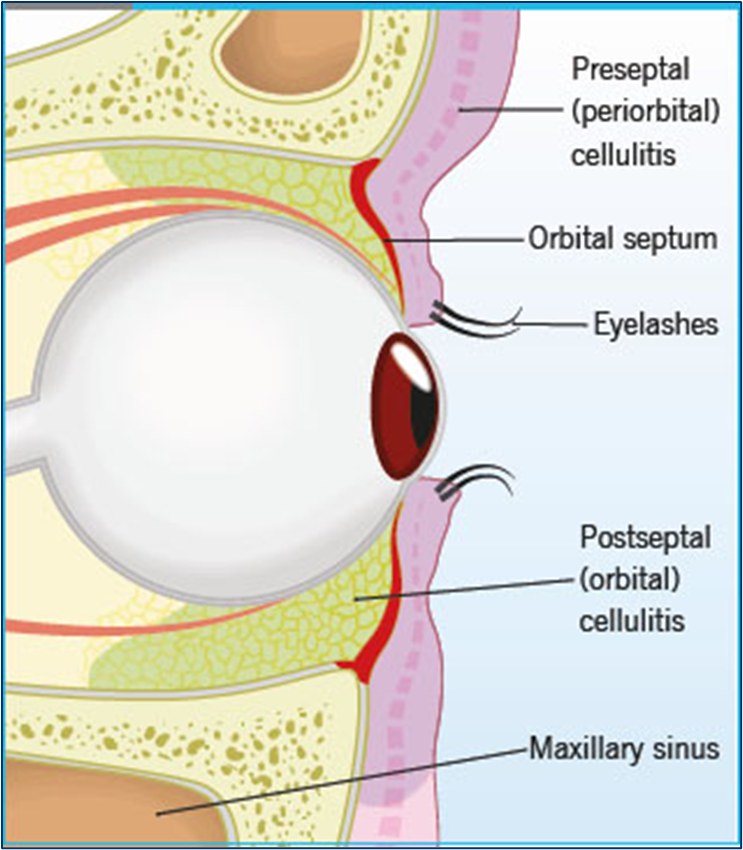
what is preseptal cellulitis (3)
affects tissues lying anterior to the orbital septum (periorbital tissue)
High risk of extension into the orbit in young children
mild condition compared to orbital cellulitis
what is orbital cellulitis (2)
Affects tissues lying posterior to the orbital septum (within the orbit) - orbital tissue
Severe sight and life-threatening emergency - needs prompt treatment and management
how do we clinically differentiate between preseptal and orbital cellulitis and what is the management for them (2)
difficult to clinically differentiate between preseptal or orbital - not job of optometrists to differentiate between them
same management for both types - same day emergency referral
what are the predisposing factors of both preseptal and orbital cellulitis (4)
fever/malaise/unwell - more severe in orbital cellulitis
infection - P: upper respiratory tract infection // O: acute sinusitis (ethmoid) dental abscess
ocular infection - P: dacryocystitis, hordeolum, impetigo // O: dacryocystitis, preseptal cellulitis
trauma - P: recent surgery // O: orbital fracture
describe the symptoms of preseptal cellulitis (4)
are acute/sudden onset
lid swelling
lid redness
lid tenderness
describe the symptoms of orbital cellulitis (8)
are acute/sudden onset
lid swelling
lid redness
lid tenderness
conjunctival swelling/oedema
pain on eye movements
blurred vision
double vision
compare the signs of preseptal and orbital cellulitis (5)

essentially if any of these signs occur - will be orbital cellulitis as they are not present in preseptal
what is the optometric management (1) and secondary care (5) of preseptal and orbital cellulitis
optometric management - emergency same day referral - both preseptal and orbital present in the same way so need to emergency refer for both - not take any risks - preseptal milder while orbital is much more severe and sight/life threatening
secondary care:
systemic antibiotics
hospital admission
blood tests
CT scan
co-management ENT
name 3 orbital disorders that are good to know
dermoid cysts
blow-out fracture
mucormycosis
explain what a dermoid/epidermoid cyst is (also known as choristoma) (4) and management (1)
mass of normal tissue in an abnormal location
thin walled, cystic lesion
may contain sweat glands, sebaceous glands, hair follicles
formed at birth but may not present until adulthood
management: refer routinely for removal - slow growing and can rupture

what are the 2 types of dermoid cysts and describe them (2)
superficial: painless slow growing nodule - often around the eyelid/brow
deep: presents in adolescence or adulthood - increasingly protruding eye, acute inflammation if ruptures
what is a blow-out fracture (3)
caused by blunt trauma - force/injuries (squash injury)
causes fracture of an orbital wall - typically the orbital floor or medial wall
tissue or muscle trapped

describe the signs (3) and management (1) of blow-out fractures
signs:
double vision - eye muscles tethered
bruising, tenderness and periorbital swelling
loss of sensation in cheek (infraorbital nerve trapped)
management:
same day referral - make it clear seen abnormal motility and double vision - needs to be seen to promptly
what is mucormycosis (4)
rare aggressive fungal infection
often fatal
typical affects patients with diabetic ketoacidosis or immunosuppression
Inhaled spores — upper respiratory tract infection — spreads to orbit and brain
what are the signs (3) and management (1) of mucormycosis
signs:
Gradual onset periorbital swelling
diplopia and loss of vision
appears similar to orbital cellulitis
management:
same day referral
